Abstract
Bronchoalveolar lavage (BAL) is a minimally invasive procedure and plays an important role in the diagnostic evaluation of interstitial lung disease, pulmonary infiltrates, and some infectious diseases. The decision to perform bronchoscopy and BAL should be guided by clinical presentation and the patient’s status as well as local technical expertise, both in performing the procedure and in interpreting the results. An important problem with interpreting BAL results is the variability between centers, which highlights the importance of following standard protocols. There is a need for a consensus statement among experts to provide guidelines for the utility of BAL cellular analyses in clinical practice. A number of specific conditions, such as some rare diseases, malignancy, and infections, can be diagnosed by BAL analyses. In such cases, more invasive procedures can be avoided. Even when nondiagnostic, BAL cellular analysis usually adds valuable information to the clinical and radiological data and helps to narrow the differential diagnosis. On the other hand, the diagnostic usefulness of BAL in interstitial lung disease, especially idiopathic pulmonary fibrosis (IPF), is limited. An important issue of BAL in this setting is exclusion of other diseases as sarcoidosis or hypersensitivity pneumonitis. BAL is an invaluable research tool for ILD, providing information regarding immune effector cells that accumulate in the alveoli and their noncellular products. With the increasing availability of proteomics, the importance of biomarkers of ILD will hopefully become clear in the near future. It is essential that BAL findings be interpreted by experts in the context of clinical and radiological data.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
Keywords
- Idiopathic Pulmonary Fibrosis
- Interstitial Lung Disease
- Hypersensitivity Pneumonitis
- Usual Interstitial Pneumonia
- Idiopathic Pulmonary Fibrosis Patient
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Introduction
Bronchoalveolar lavage (BAL) is a low-risk tool, which is very popular, commonly used to get diagnostic information. On the other hand, it may provide prognostic information too.
Among diagnostic tests, BAL has a specific value for the diagnosis of certain interstitial lung diseases (ILDs), such as alveolar hemorrhage, alveolar proteinosis, bronchoalveolar carcinoma, Langerhans’ cell histiocytosis, and Pneumocystis pneumonia, allowing surgical lung biopsy to be avoided. In other ILDs, BAL findings may support, in combination with clinical and high-resolution computer tomography (HRCT) findings, a suspected diagnosis or make it unlikely. This method is also a valid support for research. Genetic and molecular biomarkers, with different diagnostic/prognostic significance, can be detected in BAL. It has a role in diagnostic of infectious diseases such as bacterial pneumonia, tuberculosis, mycoses, or virus infections of the lung.
BAL Technique
The idea of BAL is to obtain cells, inhaled particles, infectious organisms, and solutes from the lower respiratory tract and from the alveolar spaces of the lung. A sufficient volume of lavage fluid has to be instilled. The minimum is considered about 100 mL of lavage fluid in adults. The recommendations reach from 100 to 300 mL for BAL.
BAL is a minimally invasive technique, which is usually performed during bronchoscopy under local anesthesia and moderate sedation. Local anesthesia is required to avoid cough, but can interfere with the fluid obtained during the process of BAL, and can cause coughing too. The ideal conditions might be under general anesthesia and through the rigid bronchoscope or through an endotracheal tube, but this is far from daily routine. It can be carried out in ventilated patients too.
There have been different guidelines published previously. Though the volume of saline instilled to retrieve cells from the pulmonary parenchyma, the positioning of the patient, the suction applied, and the processing of the BAL fluid for cellular analyses have not been standardized totally, something may contribute to the varying results from different laboratories and centers.
BAL must be distinguished from other lavage techniques. The widely used technique of bronchial washing or bronchial lavage during routine bronchoscopy is different from BAL. It samples material from large airways as trachea and smaller airways down to the level of segmental or subsegmental bronchi for diagnostic purpose as bacteriological or tumor cytology studies. The amount of fluid instilled is comparatively small, around 20 mL. On the other hand, there are therapeutic purposes for lavage techniques too. Often amounts of some aliquots of 20 mL are needed to remove tenacious secretions under bronchoscopy in patients suffering from chronic bronchitis, asthma, or bronchiectasis. This is sometimes necessary and the most simple therapeutic lavage technique. The most invasive lavage technique is whole lung lavage, a therapeutic procedure for pulmonary alveolar proteinosis. It is performed under general anesthesia and double-lumen intubation. Repeated instillations of 1,000 mL are used up to 20 or more liters.
Where to Perform BAL?
The middle lobe or the lingula (or one of its segments or subsegments, if thinner bronchoscopes are used) is recommended as standard site for BAL, if diffuse lung disease is present. From these lobes, about 20% more fluid and cells are recovered than from the lower lobes. Alternatively, one of the anterior segments or subsegments of the upper or lower lobes of both lungs may be used, if it is impossible or difficult to carry it out at the standard site. If diffuse lung disease is the indication for BAL, a good interlobar correlation was found concerning lavage cell differentials, lymphocyte subpopulations, and asbestos body counts. While a single-site BAL cellular profile is assumed to be representative of the lung as a whole in interstitial lung disease (ILD), some evidence suggests that this diagnostic procedure might be more useful if it was targeted to one of the pulmonary segments most affected, as identified by chest high-resolution computed tomography (HRCT). In patients with marked radiographic heterogeneity or with localized lesions, such as inflammatory infiltrates, malignant lesions, or from other cause, it is recommended that the area of greatest abnormality, as seen on the chest radiograph or CT, should be chosen as the preferred site for BAL. Some follow the concept of BAL at two or three different sites to reach higher representation.
Instillation and Recovery
The most commonly used instillate is sterile isotonic saline solution (0.9% NaCl). Warming of the instillate to body temperature may prevent coughing and increase cellular yield. The most widespread technique is to instill the fluid directly through the biopsy channel of the fiber bronchoscope. Optimal recovery is accomplished by occluding the bronchial lumen with the bronchoscope. The tip of the bronchoscope is therefore advanced into a bronchial segment (or subsegment) until a wedge position is reached. Alternatively, a suction catheter through the working channel can be used. The catheter is placed more peripherally to subsegmental or subsubsegmental bronchi. Local anesthesia fluid should be removed prior to instillation of the lavage fluid, since it may influence cell viability. The fluid is instilled with syringes using a standard number of input aliquots. Commonly 20-mL syringes are used (alternatively 60-mL) and four to five aliquots are recommended up to a total volume of 100–300 mL. Smaller instilled volumes carry the risk of contamination by the bronchial spaces. Then a more “bronchial” washing component may dominate the cellular picture.
After instillation of each aliquot, the fluid is recovered either by aspirating manually using the attached syringe or by wall suction into a fluid trap. Suction can cause airway collapse and traumatization of the airway mucosa, which may reduce recovery volume and change the fluid profile by adding blood. The optimal effect can be driven by the bronchoscopist by visual control. We prefer the use of 20-mL syringes and instillate the fluid directly through the biopsy channel. A recovery of 40–70% of the instilled volume is normal. The first aspirate may be the smallest one. Reasons for small recovery rates are emphysema, obstructive airway disease, smoking, or a higher age of the patient. Another important reason is a poor wedge position, which leads to leakage and coughing during BAL. Some reject the first “bronchial” aliquot to avoid changes of the following “alveolar” aliquots. Siliconized or plastic containers are recommended to avoid loss of cells through adhesion to glass surfaces.
Safety of BAL
BAL is a minimally invasive technique associated with a low complication rate (0–2.3%) without mortality. Most of the reported side effects are closely related to endoscopic technique, location and extent of lavaged lung area, and the volume and temperature of instilled fluid. Supplemental oxygen delivery throughout the entire procedure, oximetry, and ECG monitoring has been recommended.
The most frequent complications of BAL are transient fever and decrease of lung function parameters. Fever due to resorption of the fluid occurs in up to 30% of the patients. Typically, it occurs some hours after bronchoscopy and is self-limited, resolving within 24 h. Usually there is no need for additional therapy. It depends on the amount of the instilled fluid volume. A transient change of lung function parameters as a decrease of vital capacity, FEV1, and oxygen tension has been reported. Other side effects are transient alveolar infiltrations. Clinically, wheezing or bronchospasm may be seen after BAL.
Major complications can be seen in patients with severe lung or heart disease. Risk factors for major complications are extensive pulmonary infiltrates, pO2 < 8.0 kPa (<60 mmHg), SO2 < 90%, FEV1 < 1.0 L, bleeding disorders (prothrombin time <50 s, platelet counts <20,000 platelets/mL), significant comorbidity, and bronchial hyperreactivity. Absolute contraindications for BAL do not differ from those for bronchoscopy.
At the Laboratory
It is essential that the transfer of the materials to the laboratory is performed as quickly as possible, best within 1 h. The next steps recommended are (1) filtration through cotton gauze or nylon mesh, which reduces the mucus and a preferential loss of bronchial epithelial cells without a significant effect on the total cell count and cell differentials, (2) pooling into a single container and measurement of the total volume, (3) centrifugation for 10 min at 500 g, and (4) the supernatant can be stored frozen for subsequent analysis of soluble components.
Routine processing of BAL fluid cellular analyses for patients with ILD includes total and differential cell counts (e.g., counted in a hemocytometer) and the determination of lymphocyte subsets as well as the morphological appearances of cells, besides cultures and special stains for infection in the appropriate clinical setting.
The total count of cells can be performed in a sample of the pooled native fluid or in a resuspension of the cells after the first centrifugation. Washing procedures result in a loss of total cells but lead to an increase in cell viability of the remaining cells. The total cell count is usually expressed as the total number of cells recovered per lavage but also as the concentration of cells per milliliter of recovered fluid. Cell viability is assessed by trypan blue exclusion and should range from 80% to 95%.
For the enumeration of cell differentials, at least 600 cells are counted on cytocentrifuge or cell smear preparations after staining with May-Grünwald–Giemsa. This number of cells is needed to achieve sufficient reproducibility and low variability in the differential cell counts. The Diff-Quick stain should not be used because it does not stain mast cells. Ciliated or squamous epithelial cells should be noted but not included in the differential cell count. A high percentage of epithelial cells (>5%) is indicative of contamination of the alveolar samples by bronchial cells. Such BAL probes may not be representative for the diagnosis of diffuse parenchymal lung disease. At least three unstained slides should be stored to have the possibility for special staining (iron, periodic acid–Schiff (PAS), silver, toluidine blue, fat, or Ziehl–Neelsen) if clinically indicated or if specific observations arise from the May-Grünwald–Giemsa slides.
If clinically indicated, routine investigations could be expanded by an additional workup. If malignant disease is suspected, the Papanicolaou stain should be added. In case of infection, a complete microbiological assessment, including cultures, should be performed. Lymphocyte subpopulations can be identified by immunocytochemical methods, immunofluorescence, or flow cytometry using monoclonal antibody techniques. The crucial point for flow cytometry is that ≥1 × 106 cells are required to perform an adequate test. These investigations are not recommended as routine procedures for BAL specimens. They are especially indicated in patients with high lymphocyte counts, such as hypersensitivity pneumonitis (HP), or if Langerhans’ cell histiocytosis is suspected. CD1a and Langerin are very specific markers for Langerhans’ cell histiocytosis. Flow cytometry can be helpful in detecting markers of malignant lymphoma.
In addition, for research purposes, functional studies of viable BAL cells can be performed. The cells can be cultivated in appropriate culture medium, and the release of mediators can be determined along with the mechanisms that appear to regulate the mediator release. It is possible to study cell–cell interactions with co-cultures of two different types of cells. Cells can also be assessed with molecular biology tools to investigate gene activation and intracellular signaling pathways.
As for the measurement of acellular components, a reasonable pragmatic approach was taken by the European Respiratory Society (ERS) Task Force. These components should be expressed as amounts per mL of recovered BAL fluid, in order to facilitate comparison of data from different workers until a reliable external marker can be defined. The report of the ERS Task Force also provides detailed information on the measurement of soluble components.
What Is Normal in BAL?
The BAL fluid obtained from healthy, nonsmoking adults without underlying lung disease is dominated by alveolar macrophages (>80%). Normal in BAL may be 80–90% alveolar macrophages (AMs), 5–15% lymphocytes, 1–3% polymorphonuclear neutrophils, 1% eosinophils, and <1% mast cells.
Cigarette smoking leads to significant effects on BAL samples. The alveolar macrophages from smokers are larger than those in nonsmokers (three- to fivefold increase) and show a characteristic morphology. They contain smoker’s inclusion bodies, which are cytoplasmic inclusion bodies consisting of tar products, lipids, lipofuscin, and other substances.
BAL in Different Situations
BAL plays a role in the daily clinical routine in very different situations, as:
-
In the diagnosis of diffuse parenchymal lung disease
-
In the diagnosis of infiltrations, infectious disease, malignant disease
-
An adjunct to diagnosis in different situations
-
Assessment of disease activity and prognosis, especially in ILDs
Additionally, it plays a role in research and development of new drugs.
BAL in the Diagnosis of Diffuse Parenchymal Lung Disease
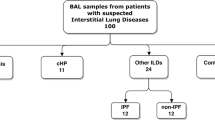
ILDs represent a very broad and heterogeneous group of acute and chronic lung disorders with variable degrees of inflammation and fibrosis. They predominantly affect the distal pulmonary parenchyma including the confined interstitial space bounded by the epithelial and endothelial basement membranes of the alveolar wall. Because of these similarities, they are grouped under ILDs. However, there are significant differences between different ILDs. The etiology, the findings on HRCT and histology differ, as do the clinical course, prognosis, treatment modalities, and response to treatment. Idiopathic interstitial pneumonias (IIPs) are a specific subgroup of ILDs of unknown etiology, with distinct histological features. The initial diagnostic approach includes a full medical history (with occupational and environmental exposures or drug reactions), physical examination, laboratory tests, pulmonary function tests, and imaging (chest x-ray and HRCT). If these noninvasive techniques do not lead to diagnosis, more invasive techniques as bronchoscopy including BAL, transbronchial lung biopsy, and surgical lung biopsy have to be considered. Among these procedures, bronchoscopy is the least invasive technique. It is generally well tolerated with very low overall morbidity and mortality [19], but there is a discussion, if bronchoscopy is needed.
BAL plays an important role in the diagnosis of patients suffering from pulmonary infiltrates and shadowing and some diffuse interstitial lung disease, so this indication is widely accepted. In most situations, in which diffuse lung disease caused by infectious, immunological, or malignant disease is suspected, BAL should not be considered as the only diagnostic test but in addition to clinical, radiographical, and laboratory tests. The findings of HRCT play a more and more important role. In ILD, the differential cell counts and specific BAL lavage features can be variable, nonspecific, and insensitive. But often, BAL cellular profiles may help to narrow the differential diagnoses of ILDs and to guide further specific diagnostic interventions. However, some BAL findings may be very specific and lead directly to a diagnosis and can in such situations replace biopsy.
Cellular Patterns of BAL
There are different BAL profiles, which are common in the clinical routine. A lymphocytic cellular pattern, a neutrophilic cellular pattern, an eosinophilic cellular pattern, and other inflammatory patterns have different implications (Table 16.1).
A lymphocytic BAL pattern is commonly seen in granulomatous lung diseases, such as sarcoidosis and hypersensitivity pneumonitis (Fig. 16.1a, b), and in the context of immune reactions of the lung to some drugs. However, the number of lymphocytes and the CD4/CD8 ratio can be variable in sarcoidosis. The majority of sarcoidosis cases display an isolated BAL lymphocytosis, while a raised neutrophil count appears to correlate with more severe disease and need for therapy. In hypersensitivity pneumonitis, not only the number of lymphocytes but also the absolute neutrophil and eosinophil counts may be significantly increased. BAL lymphocytosis >50% generally raises a suspicion for the diagnosis of hypersensitivity pneumonitis, and patients with hypersensitivity pneumonitis may exhibit either decreased, normal, or increased CD4/CD8 ratio. BAL lymphocytosis may be present in methotrexate and amiodarone pneumonitis, as well as in beryllium disease. BAL lymphocytosis appears to be common in the cellular variant of nonspecific interstitial pneumonia (NSIP) too. Finally, a subclinical lymphocytic cellular pattern in BAL has been reported in Wegener’s granulomatosis, Crohn’s disease, and primary biliary cirrhosis.
(a) Lymphocytic pattern and foamy cytoplasm of alveolar macrophages with vacuoles in hypersensitivity pneumonitis (HP) (Courtesy of Dr. Henry Budihardjo Welim, Institute of Pathology Hemer). (b) Vacuoles in alveolar macrophages (Courtesy of Dr. Henry Budihardjo Welim, Institute of Pathology Hemer and Dr. Thomas Beyer, Lung Clinic Ballenstedt)
A neutrophilic cellular pattern can be found in idiopathic pulmonary fibrosis (IPF), asbestosis, acute respiratory distress syndrome (ARDS), aspiration pneumonia, subacute hypersensitivity pneumonitis, and cryptogenic organizing pneumonia (COP), as well as in pulmonary infections. An increased neutrophil count may be unspecific but in the appropriate clinical setting is observed in the BAL of 70–90% of patients with IPF. The nonspecific nature of a BAL neutrophilia is illustrated by the difficult diagnostic problem of fibrotic nonspecific interstitial pneumonia (NSIP) too.
An eosinophilic cellular pattern of BAL is in the absence of asthma and parasitic infections highly suggestive of eosinophilic pneumonia. Differential diagnosis may be Churg–Strauss syndrome, allergic pulmonary aspergillosis, drug-induced lung disease, or Langerhans’ cell histiocytosis. The diagnosis of Langerhans’ cell histiocytosis can be made by the presence of more than 5% Langerhans’ cells in BAL, identified by monoclonal antibodies directed against the CD1a antigen or Langerin. Though, it can be an unspecific finding too, as in some cases of IPF, HP, and collagen vascular disease-associated pulmonary fibrosis. If eosinophilia exceeds 25%, eosinophilic pneumonia has to be considered.
Plasma cells are not present in normal BAL. If found, together with foamy macrophages and increased lymphocyte count, HP or drug-induced lung disease has to be suggested. Differential diagnoses are cryptogenic organizing pneumonia and chronic eosinophilic pneumonia. Mast cells appear in the process of lung inflammation and fibrosis. An increased number is sometimes observed in sarcoidosis, associated with advanced or progressive disease.
In addition, if mixed cellular patterns are present, the predominant cellular pattern might offer a hint to the diagnosis, although in these circumstances, invasive procedures such as lung biopsy (bronchoscopic transbronchial or surgical) may be required to make a specific diagnosis.
Specific BAL Findings
In some rare diseases, in the appropriate clinical setting, BAL findings can be diagnostic per se. BAL has a high diagnostic value in these cases (Table 16.2).
In pulmonary alveolar proteinosis, the BAL fluid looks milky or turbid. Under bronchoscopy, this may cast suspicion on the specific disease. Under light microscopy, the characteristic acellular oval bodies (surfactant-derived lipoproteins) are basophilic on May-Grünwald–Giemsa staining and positive with PAS staining. The background is filled by large amounts of amorphous debris showing weak PAS staining and few foamy macrophages (Fig. 16.2).
The combination of grossly milky BAL fluid, PAS-positive acellular oval bodies, and foamy macrophages under light microscopy is virtually pathognomonic of the disease and obviates the need for transbronchial or surgical lung biopsy.
Pulmonary Langerhans’ cell histiocytosis is strongly associated with cigarette smoking, and the BAL differential cytology shows a typical smoker constellation with increased total cell counts and macrophages with smoker’s inclusions. The specific finding is an increase in Langerhans’ cells to >5% of the total BAL cell count (Fig. 16.3). The sensitivity is low because in late cases of the disease the number of Langerhans’ cells decreases in the tissue. Low proportions of Langerhans’ cells in the range of 2–4% can be seen in other conditions, such as in healthy smokers, respiratory bronchiolitis/interstitial lung disease (RB/ILD), other ILDs, and bronchoalveolar carcinoma. Staining by monoclonal antibodies for CD1a or Langerin enables identification of Langerhans’ cells in BAL (Fig. 16.4). The reaction with the polyclonal antibody S100 is less specific. In cases with characteristic BAL findings, electronic microscopy is not needed.
Multiple causes may lead to diffuse alveolar hemorrhage (DAH). It is a clinical syndrome characterized by severe hemoptysis because of bleeding into the alveolar space. BAL analysis may help to diagnose alveolar hemorrhage syndromes, including Goodpasture’s syndrome, Wegener’s granulomatosis, systemic lupus erythematosus and other vasculitides, idiopathic pulmonary hemosiderosis, pulmonary capillaritis, and collagen vascular disease. The characteristic findings in BAL are numerous hemosiderin-laden macrophages. If coagulopathy is excluded, BAL is pivotal in excluding or confirming diffuse alveolar hemorrhage in patients with unexplained pulmonary infiltrates. In extensive diffuse alveolar hemorrhage, hemoptysis is often minimal or absent, and HRCT findings are nonspecific.
Fresh bleeding leads to free red blood cells in the BAL fluid. Fragments of ingested red blood cells within the cytoplasm of macrophages are pathognomonic. The color of the BAL fluid is bloody or something between pink and brown, depending on the interval and intensity to bleeding. The recovered fluid stains more intensely from fraction to fraction, which is characteristic for alveolar hemorrhage. It can be distinguished from aspirated blood from the bronchi by the fact that then the first fraction is the bloodiest one.
To assess the severity of bleeding, the percentage of siderophages can be counted. This is more practical than the time-consuming application of the Golde score, which also takes into account the intensity of staining of each macrophage. It has been shown that a percentage of siderophages ≥20% is sufficient for the diagnosis of DAH. Hemosiderin-laden macrophages do not appear earlier than 48 h after bleeding. Thus, very early bleeding shows only numerous red blood cells.
It is important to highlight that many syndromes belong to this group of disorders; therefore, other clinical and laboratory findings must be considered to establish the cause of bleeding. In the clinical setting, chronic left heart failure with pulmonary congestion is one of the most frequent underlying conditions for the finding of DAH in BAL fluid examination.
BAL is not as sensitive for solid tumors as biopsy or other cytology techniques. But diffuse malignant infiltrates can be reliably diagnosed in 60–90% of cases. Malignancies like primary bronchoalveolar carcinoma or lymphangitis carcinomatosis due to adenocarcinoma have the highest yield in BAL. BAL can also provide diagnostic cytological material in hematological malignancies of the lung, including lymphoma, leukemia, and others.
Different pneumoconioses lead to changes which can be detected through the use of BAL. Dust particles in alveolar macrophages can confirm exposure, but no close correlation exists between the extent of disease and the quantity of inhaled dust. Dust particles and birefringent material within the alveolar macrophages or elevated asbestos body counts suggest occupational exposure.
In asbestos-related disease, asbestos bodies can be detected in smears or cytocentrifuged preparations of BAL fluid. More sensitive, however, is the quantification of asbestos bodies by a specific millipore filtration technique (Figs. 16.5 and 16.6). It shows a good correlation with the asbestos body count in lung tissue analysis. A negative BAL asbestos body count does not exclude asbestos-related disease, as 10–15% of subjects with known occupational asbestos exposure do not have detectable asbestos bodies in their BAL fluid.
Chronic beryllium disease is clinically, radiologically, and histologically identical to sarcoidosis. Even BAL lymphocytosis and an increase of CD4/CD8 ratio are identical. Diagnosis can be confirmed by an in vitro lymphocyte transformation test because the antigen is known. The transformation test in BAL is more sensitive and specific than the blood test.
Eosinophilic lung diseases can be diagnosed when there are ≥25% eosinophils in BAL of the radiologically affected segment. In both acute and chronic eosinophilic pneumonia, the fraction of BAL eosinophils ranges from 20% to 90% and is higher than the neutrophils fraction. In addition, a mild-to-moderate increase in lymphocyte count with a decrease in CD4/CD8 ratio can be observed. Sometimes plasma cells can also be detected. Churg–Strauss syndrome shows similar findings. The diagnostic significance of a milder eosinophilia (<20%) is limited since it may be present in ILD or asthma too. In combination with clinical and HRCT findings, eosinophilic lung diseases can be appropriately diagnosed by BAL even without open lung biopsy.
Aspiration has to be considered in the differential diagnosis of recurrent pneumonia or atypical diffuse pulmonary infiltrates. BAL analysis shows usually large numbers of lipid-laden macrophages with marked vacuolization of their cytoplasm. These finding is highly suggestive for lipoid pneumonia caused by chronic aspiration. Other differential diagnoses are hypersensitivity pneumonia and drug-induced pneumonia.
In immunocompromised patients with pulmonary infiltrates, opportunistic infections are common. In this setting, BAL is one of the most important tools. The sensitivity of BAL ranges from 60% to 90% in the diagnosis of bacterial infections; 70–80% in mycobacterial, fungal, and most viral infections; and 90–95% in Pneumocystis jivorecii pneumonia. If Pneumocystis infection is suspected, the BAL fluid should not be filtered through gauze, as Pneumocystis is commonly found in mucous material. The characteristic cysts of Pneumocystis can be detected on May-Grünwald–Giemsa or Grocott stained slides. The cysts are foamy vacuoles within an accumulation of slightly basophilic amorphous material. Staining with modified toluidine blue or silver methamine visualizes the cyst wall. There is a high sensitivity of PCR (>90%) for Pneumocystis jivorecii in BAL. A positive PCR for Pneumocystis should be confirmed by staining methods to differentiate between colonization and infection. In cytomegalovirus pneumonia, the characteristic cytomegalic-transformed cell (the owl eye cell) with typical nuclear or cytoplasmic inclusions is highly specific and can be seen on light microscopy in 30–50% of cases.
BAL as an Adjunct to Diagnosis
Most BAL findings in ILDs are unspecific. However, BAL and cellular analysis may help clearing up a diagnosis. Very important is the context of clinical and especially radiological HRCT findings. BAL cellular patterns can generally differentiate the fibrosing conditions (characterized by neutrophilia and eosinophilia) from granulomatous diseases (lymphocytosis with or without granulocytosis). For further specification, the CD4/CD8 ratio may be helpful. In some centers, CD4/CD8 ratios are considered to be diagnostically useful, with an increased CD4/CD8 ratio favoring a diagnosis of sarcoidosis, whereas a low CD4/CD8 ratio is more usual in HP. But it is clear that there are too many exceptions to these observations. This BAL distinction is not definitive in isolation.
In most of the patients suffering from sarcoidosis, BAL shows a typical pattern, demonstrating lymphocytic alveolitis (>90%) independent of the stage of disease. If there is active sarcoidosis, the lymphocyte counts tend to be higher, but the range is wide. In the more advanced stages, neutrophils and mast cells may also be increased. Even if imaging findings are normal, BAL findings may be typical in sarcoidosis patients.
The CD4/CD8 ratio is characterized by a high variability in sarcoidosis, so it has been debated controversially. At the time of diagnosis, not every patient has an increased CD4/CD8 ratio. Most probably it is increased if acute sarcoidosis or Löfgren’s syndrome is present. On the other hand, even 15% of patients show a decreased CD4/CD8 ratio. The sensitivity for diagnosis of sarcoidosis is low around only 55%, but the specificity is high around 95%, higher than the specificity of transbronchial biopsy. Increased neutrophils in BAL of patients with newly diagnosed sarcoidosis may indicate unfavorable prognosis.
The disease showing the highest total cell count and the highest lymphocyte count is extrinsic allergic alveolitis or hypersensitivity pneumonitis (HP). The proportion of lymphocytes exceeds often 50%. The number of activated T cells is also increased. The CD4/CD8 ratio can be decreased, which was a general belief, but it can be normal or increased too. A higher ratio is more probably found in chronic disease.
The alveolar macrophages are heterogeneous and often show a foamy cytoplasm. Plasma cells can be seen in patients with recent antigen exposure. In contrast to sarcoidosis, an increase of neutrophils, eosinophils, and mast cells can also be observed. To complicate matters further, the BAL profile of HP is also heavily influenced by the time that has elapsed from antigen inhalation and the intensity of exposure. Following an acute episode of HP, the neutrophil count may increase transiently. Exclusions for HP are a normal cell appearance and an isolated increase in neutrophil or eosinophil count.
A large number of different drugs may cause drug-induced pneumonitis. The mechanisms are either toxic or immunological. BAL findings are very different. Lymphocytosis, granulocytosis, cytotoxic reactions, and diffuse alveolar hemorrhage can be found, partly combined. The most frequent finding is lymphocytic alveolitis with a dominance of CD8+ T cells. Most important are an increase of CD4+ cells in methotrexate-induced pneumonitis and the presence of alveolar macrophages with a finely vacuolated foamy cytoplasm in amiodarone-induced pneumonitis. If no foamy macrophages are found, amiodarone-induced pneumonitis may be excluded. But these findings are not specific, so diagnosis cannot be made on this only.
Idiopathic pulmonary fibrosis (IPF) is a progressive and often fatal fibro-proliferative lung disorder of unknown etiology characterized by the histopathological and HRCT pattern of usual interstitial pneumonia (UIP). The existing American Thoracic Society (ATS)/European Respiratory Society (ERS) consensus statement suggests major criteria (exclusion of known causes of interstitial lung disease, abnormal pulmonary function with restriction and/or decreased gas transfer, bibasal reticular abnormalities on HRCT scans or chest radiograph, BAL or transbronchial lung biopsy not suggesting any other disease) and minor criteria (age >50 years, insidious onset of otherwise unexplained dyspnea, duration of illness >3 months, bibasal inspiratory crackles on auscultation) for the clinical diagnosis of IPF. The role of surgical lung biopsy is debated controversially. If a diagnosis cannot be made on the basis of these simple criteria, surgical lung biopsy may be necessary for a confident diagnosis [18]. However, if classical features in HRCT images, which are associated with a UIP histopathological pattern, are present, there will be no need for lung biopsy. In the moment, there is no consensus on the role of BAL and biopsy. Awaited new evidence-based guidelines for managing IPF will clarify the diagnostic process of IPF.
One of the problems with IPF is that the disease has no pathognomonic clinical, biochemical, BAL cellular, or pathological features. The role of BAL in IPF is controversial. In early published case series, the diagnostic value of BAL findings was considered in isolation in groups of patients, without reference to a priori probabilities of individual diagnoses (based on the relative prevalence of individual disorders), the clinical presentation, or findings of other tests. For this reason, these studies failed to quantify the true added diagnostic value of BAL in diffuse parenchymal lung disease. BAL may be useful in individual patients, in altering the balance of diagnostic probability, but is rarely diagnostic itself. A diagnostic likelihood of only 30–70% means major uncertainty. The same reservation applied to the predictive value of CD4/CD8 ratios. The prevailing problem is that no study exists in which BAL data are integrated with the pretest probability of disease, based not only on disease prevalence but also on age, sex, smoking history, mode of presentation, observed disease behavior, observed previous responsiveness to treatment, clinical evaluation, and the results of other tests. The problem has been compounded by the advent of HRCT, which has transformed the diagnostic landscape. The definition of pre-BAL diagnostic probabilities has been refined radically in the HRCT era, and thus, the landmark BAL series of the 1980s are now out of date. A second problem, common to all clinical diagnostic studies, is the issue of an appropriate reference standard.
Although BAL findings are nonspecific to IPF, they differ distinctly from differential cell counts in sarcoidosis or HP. Typically there is a moderately increased neutrophil count (10–30% of the total cells). Eosinophils may slightly be increased too, but neutrophils are usually twice of eosinophils. Seventy to ninety percent show an increased neutrophil count, and 40–60% show an additionally increased eosinophil count. A minority of patients have a moderately increased lymphocyte count too. Conversely, a lone BAL lymphocytosis is an uncommon finding in IPF and, when present, should raise the suspicion of alternative diagnoses, such as granulomatous infectious diseases, sarcoidosis, HP, COP, NSIP, or lymphocytic interstitial pneumonia (LIP). If a marked increase of lymphocytes is found, such diseases have to be excluded. An increase in the BAL lymphocyte count, which has been associated with a positive clinical response to steroid treatment and better outcome, is found in 10–20% of patients with IPF. However, because these latter data come from historical studies, some of these patients most probably had NSIP, a more benign form of idiopathic interstitial pneumonia, which more recently has been conceived as a separate entity.
Conversely, distinguishing IPF from the fibrotic variant of NSIP solely based on the BAL cellular profile is far more difficult. Recently, the role of BAL in separating NSIP from UIP in a large patient population retrospectively was evaluated. It was found that UIP is characterized by a higher neutrophil count (7%) and lower lymphocyte count (5%) than NSIP (3% and 29%, respectively).
A BAL lymphocytosis with a mild increase in the neutrophil and eosinophil count may be seen in nonspecific interstitial pneumonia (NSIP). Cellular NSIP is more frequently characterized by BAL lymphocytosis than fibrotic NSIP. The BAL findings in cellular NSIP may be similar to those of cryptogenic organizing pneumonia (COP). These results are in contrast with other published data, demonstrating that BAL had neither a diagnostic role nor prognostic value in a smaller cohort of patients with either IPF or idiopathic NSIP. When diagnosis of IPF is based on HRCT, pulmonary function, and clinical findings, in the presence of a predominantly lymphocytic BAL, alternative diagnoses should be suggested. A retrospective analysis on IPF patients data showed that none of them had >30% lymphocytosis, with three patients (7%) displaying only mild lymphocytosis (range 14–17%), far below a discussed 30% cutoff. This data are consistent with previous data showing that an increase in BAL lymphocytes alone may be present in up to 10% of IPF patients only.
First, the clinical entity of NSIP was termed as “provisional.” It subsequently became apparent that the term NSIP, as applied over the past decade, covered distinct diverse clinicoradiological profiles, including profiles suggestive of COP, HP, and even IPF. Among these disorders, cryptogenic organizing pneumonia (COP) was described in the mid-1980s, but typical BAL profiles were not at first recognized, and thus, the presence of COP was not considered in the differential diagnosis of a lymphocytic profile. This omission had important implications with regard to reports of the diagnostic and prognostic utility of BAL. The BAL profile of COP, evaluated in a number of studies, includes a lymphocytosis in the great majority of cases, but other cell types (neutrophils, eosinophils, and mast cells) are commonly (although not always strikingly) increased. The eosinophil counts are not as high as in patients with chronic eosinophilic pneumonia, usually less than 25%. The combination of typical clinical symptoms and patchy infiltrates, a BAL cell profile of >20% lymphocytes, eosinophils between 2% and 25%, and a CD4/CD8 ratio <1.0 are highly suggestive for COP if infection or malignancy is excluded. Based on this, a corticosteroid therapy is well founded.
Nonetheless, the early series drew important broad diagnostic distinctions between granulomatous lung disease and IPF. Only a BAL neutrophilia, often associated with an eosinophilia, in IPF and a BAL lymphocytosis, with a variable BAL neutrophil content and, in HP, an occasional BAL eosinophilia, has stood the test of time. However, the use of BAL to make more refined diagnostic subdivisions among the more prevalent diseases has proved disappointing.
The BAL fluid in acute interstitial pneumonia is often bloody and rich in albumin, indicating increased alveolar capillary permeability. The typical cellular BAL finding is a marked increase in neutrophils and an occasional increase in lymphocytes. Atypical pneumocytes mimicking adenocarcinoma and fragmented hyaline membranes may also be observed.
Desquamative interstitial pneumonia (DIP) and RB/ILD are smoking-related ILDs. The typical BAL finding in desquamative interstitial pneumonia and RB/ILD is an increase in macrophages with black pigmented inclusions. An increase in neutrophils, eosinophils, and occasionally, lymphocytes may also be seen.
In collagen vascular disease, pulmonary involvement is frequent and associated with different histological patterns. It may reach from patterns like usual interstitial pneumonia to patterns like nonspecific interstitial pneumonia. The HRCT pattern may show this variability too. The BAL findings vary too and are different to IPF. The general pattern is increased neutrophils, may be together with increased eosinophils, and more likely together with increased lymphocytes, and in different combinations. The NSIP pattern is the more prevalent. Increased BAL neutrophils may be associated with more extensive changes on HRCT. But BAL cell profiles do not seem to be useful to predict survival, progression, or treatment response in systemic sclerosis-associated interstitial lung disease. In general, the BAL profile is nonspecific. BAL plays a greater role in clinical routine of these patients by managing drug-induced pulmonary disease, infection, hemorrhage, and malignancy.
It is debatable in IPF, whether BAL adds diagnostic value to a thorough and very careful history and clinical and laboratory findings, thus highlighting the importance of excluding known causes of interstitial pneumonia at the beginning of the diagnostic process. The diagnostic gold standard of IPF is therefore an integrated clinical–radiological–pathological evaluation.
Assessing the Activity of Disease and Prognosis
The difficulties in relating historical BAL data to diagnosis apply equally to the use of BAL in the definition of prognosis. It is unclear whether BAL cellularity is useful for assessing the activity of disease processes with respect to obtaining prognostic information.
In sarcoidosis, differences were observed for several BAL parameters between clinically active and inactive patient groups, but without predicting long-term outcome in individual patients. In patients with IPF, a BAL lymphocytosis was found to denote a more favorable course, including a higher likelihood of a response to treatment. In contrast, a BAL neutrophilia or eosinophilia was associated with a poor outcome. A recent analysis of 156 patients showed that an increased BAL neutrophil percentage was an independent predictor of early mortality. It is increasingly accepted that in diffuse lung disease, “diagnosis is prognosis”. Thus, it is unclear whether the prognostic value of a BAL lymphocytosis relates solely to its diagnostic value or whether it carries a separate prognostic advantage in patients with IPF, diagnosed using recent criteria. However, after adjustment for underlying disease severity (using pulmonary function tests and HRCT data in separate multivariate models), BAL neutrophil content does not differ between different diseases, which makes it difficult to argue for a tight link between a BAL neutrophilia and the intrinsic progressiveness of disease.
In pulmonary fibrosis due to pulmonary involvement in systemic sclerosis, neutrophilia is the most prevalent BAL abnormality. It is associated with a worse outcome if other data are not considered. However, there is ample evidence that in systemic sclerosis, neutrophilia is linked to more extensive pulmonary fibrosis on HRCT and greater pulmonary function impairment. In one recent study, the presence of a BAL neutrophilia had no independent prognostic significance in a large cohort of systemic sclerosis patients, after adjustment for disease severity. Thus, it appears that in systemic sclerosis, a BAL neutrophilia is no more than a marker of disease severity and the same may also apply to other diffuse lung diseases.
It is not proven that BAL or serial BAL is helping to guide therapy or to predict treatment response. At present, BAL cannot be routinely recommended for this purpose. In general, it appears that the presence of a BAL lymphocytosis or neutrophilia is much less influential in prognostic evaluation than accurate diagnosis and the accurate staging of disease severity, respectively.
BAL in the Diagnosis of Infections
BAL may help to detect infections of the lower respiratory tract. But the role of BAL in this context is debatable too. The material should be processed as soon as possible, thus avoiding further contamination or missing such agents as anaerobic bacteria. BAL fluid should be worked up for bacterial, fungal, opportunistic, and viral infections. In addition, the material should be examined by a cytopathologist. BAL fluid should be stained and cultured quantitatively for bacteria using appropriate media, stained and cultured for mycobacteria (including mycobacteria other than M. tuberculosis) and for fungi.
In most clinical situations, there is no advantage for those invasive techniques over less invasive procedures as sputum diagnostic or blind aspirations of the trachea in bacterial pneumonia. In the management of severe community-acquired pneumonia, it could not yet be shown that etiological diagnosis with or without bronchoscopy has a prognostic impact. Semiquantitative counting of bacteria helps to differentiate between colonization and infection. As a less invasive procedure, a mini-BAL technique has been described. The diagnosis of ventilator-associated pneumonia is very difficult. It is made by the combination of clinical, radiological, and laboratory criteria (new infiltration, fever or hypothermia, leukocytosis or leukopenia, putrid tracheal secretions) and quantitative culture of tracheal aspirations or BAL. The cutoff of ≥105 resp. ≥104 CFU/mL is accepted as an indicator for ventilator-associated pneumonia.
Legionella infections can be detected either by direct immunofluorescence technique or by bacterial culture. Viral infections should be excluded using antibodies, viral cultures, and DNA-/RNA-probe analysis. To differentiate between acute, latent, or chronic persistent infection, the virus load must be measured by the number of genome equivalents, preferably in induced sputum or BAL. Electron microscopy can be used too.
Role of BAL in Research and Development of New Drugs
The discovery of new biomarkers and new signal pathways between cells and the application of proteomics, gene arrays, and metabolomics have contributed many important insights into the pathogenesis of respiratory tract diseases. BAL has been profiled as a pivotal method to obtaining alveolar space and airway specimens for research, and this could lead to more precise longitudinal monitoring of ILD in the future. For example, KL-6, a high molecular weight glycoprotein predominantly expressed on the surface of alveolar type II cells, is a promising biomarker in the field of ILD. Increased levels of KL-6 in BAL fluid and plasma correlate with the severity of alveolar inflammation and poor survival in acute respiratory distress syndrome. Increased levels of KL-6 in both BAL fluid and blood, with a strong correlation between BAL and blood, also reflect disease severity in patients with idiopathic pulmonary alveolar proteinosis.
BAL is suitable to study the cellular and biological changes induced by drugs. In this regard, BAL can be used for proof-of-concept studies in the clinical development of new drugs.
Conclusions
Since the early 1980s, BAL has been used to diagnose diffuse parenchymal lung disease. In addition, prognostic evaluation of ILD was made by BAL. It plays a crucial role in diagnosing rare disorders and in diagnosing or excluding opportunistic infection. In the most centers, BAL is an important tool for the diagnostic approach and management of more common diseases as sarcoidosis, HP, or IPF. But this use of BAL is recently discussed controversially as there were important changes in disease classification. Most published studies fail to integrate BAL data with other clinical and radiological information. Further studies to assess the additional value of BAL are required.
Suggested Reading
Allen JN, Davis WB. Eosinophilic lung diseases. Am J Respir Crit Care Med. 1994;150:1423–38.
American Thoracic Society/European Respiratory Society. ATS/ERS international multidisciplinary consensus classification of the idiopathic interstitial pneumonias. Am J Respir Crit Care Med. 2002;165:277–304.
Baughman RP, Raghu G. Bronchoalveolar cellular analysis in scleroderma lung disease: does Sutton’s law hold? Am J Respir Med. 2008;177:2–3.
Bonella F, Ohshimo S, Bauer P, Guzman J, Costabel U. Bronchoalveolar lavage. In: Strausz J, Bolliger CT, editors. Interventional pulmonology. Eur Respir Monogr. 2010;48: 59–72.
Costabel U, editor. Atlas der bronchoalveolären Lavage. Stuttgart: Thieme; 1994.
Costabel U, Guzman J, Bonella F, Oshimo S. Bronchoalveolar lavage in other interstitial lung diseases. Semin Respir Crit Care Med. 2007;28:514–24.
Costabel U. CD4:CD8 ratios in bronchoalveolar lavage fluid: of value for diagnosing sarcoidosis? Eur Respir J. 1997;10:2699–700.
Drent M, Baughman RP, Meyer KC. Bronchoalveolar lavage. In: Costabel U, du Bois RM, Egan JJ, editors. Diffuse parenchymal lung disease. Prog Respir Res. 2007;36:58–67.
Drent M, Mansour K, Linssen C. Bronchoalveolar lavage in sarcoidosis. Semin Respir Crit Care Med. 2007;28:486–95.
Flaherty KR, King TE, Raghu G, Lynch JP, Colby TV, Travis WD, Gross BH, Kazerooni EA, Toews GB, Long Q, Murray S, Lama VN, Gay SE, Martinez FJ. Idiopathic interstitial pneumonia: what is the effect of a multidisciplinary approach to diagnosis? Am J Respir Crit Care Med. 2004;170:904–10.
Haslam PL, Baughman RP. Report of ERS Task Force: guidelines for measurement of acellular components and standardization of BAL. Eur Respir J. 1999;14:245–8.
Höffken G, Lorenz J, Kern W, Welte T, Bauer T, Dalhoff K, Dietrich E, Ewig S, Gastmeier P, Grabein B, Halle E, Kolditz M, Marre R, Sitter H. Guidelines of the Paul-Ehrlich-Society of Chemotherapy, the German Respiratory Diseases Society, the German Infectious Diseases Society and of the Competence Network CAPNETZ for the management of lower respiratory tract infections and community-acquired pneumonia summary of the update 2009. Pneumologie. 2010;64:149–54.
Kinder BW, Brown KK, Schwarz MI, Ix JH, Kevitsky A, King TE. Baseline BAL neutrophilia predicts early mortality in idiopathic pulmonary fibrosis. Chest. 2008;133:226–32.
Klech H, Hutter C. Clinical guidelines and indications for bronchoalveolar lavage (BAL): report of the European Society of Pneumology Task Force on BAL. Eur Respir J. 1990;3:937–74.
Klech H, Pohl W. Technical recommendations and guidelines for bronchoalveolar lavage (BAL). Report of the European Society of Pneumology Task Group. Eur Respir J. 1989;2:561–85.
Meyer KC. The role of bronchoalveolar lavage in interstitial lung disease. Clin Chest Med. 2004;25:637–49.
Ohshimo S, Bonella F, Cui A, Beume M, Kohno N, Guzman J, Costabel U. Significance of bronchoalveolar lavage for the diagnosis of idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 2009;179:1043–7.
Ryu YJ, Chung MP, Han J, Kim TS, Lee KS, Chun EM, Kyung SY, Jeong SH, Colby TV, Kim H, Kwon OJ. Bronchoalveolar lavage in fibrotic idiopathic interstitial pneumonias. Respir Med. 2007;101:655–60.
Spagnolo P, Luppi F, Rossi G, Richeldi L. To BAL or not to BAL: is this a problem in diagnosing IPF? Am J Respir Crit Care Med. 2009;180:379–80.
Spagnolo P, Richeldi L, Raghu G. The role of bronchoalveolar lavage cellular analysis in the diagnosis of interstitial lung diseases. Eur Respir Monogr. 2009;46:36–46.
Tazi A. Adult pulmonary Langerhans’ cell histiocytosis. Eur Respir J. 2006;27:1272–85.
The BAL Cooperative Group Steering Committee. Bronchoalveolar lavage constituents in healthy individuals, idiopathic pulmonary fibrosis, and selected comparison groups. Am Rev Respir Dis. 1990;141:S169–202.
Travis WD, Hunninghake G, King TE, Lynch DA, Colby TV, Galvin JR, Brown KK, Chung MP, Cordier JF, du Bois RM, Flaherty KR, Franks TJ, Hansell DM, Hartman TE, Kazerooni EA, Kim DS, Kitaichi M, Koyama T, Martinez FJ, Nagai S, Midthun DE, Müller NL, Nicholson AG, Raghu G, Selman M, Wells A. Idiopathic nonspecific interstitial pneumonia: report of an American Thoracic Society project. Am J Respir Crit Care Med. 2008;177:1338–47.
Wells AU. Cryptogenic organizing pneumonia. Semin Respir Crit Care Med. 2001;22:449–50.
Wells AU. The clinical utility of bronchoalveolar lavage in diffuse parenchymal lung disease. Eur Respir Rev. 2010;19:237–41.
Ye Q, Nakamura S, Sarria R, Costabel U, Guzman J. Interleukin 12, interleukin 18, and tumor necrosis factor alpha release by alveolar macrophages: acute and chronic hypersensitivity pneumonitis. Ann Allergy Asthma Immunol. 2009;102:149–54.
Ziegenhagen MW, Rothe ME, Schlaak M, Müller-Quernheim J. Bronchoalveolar and serological parameters reflecting the severity of sarcoidosis. Eur Respir J. 2003;21:407–13.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2013 Springer Science+Business Media New York
About this chapter
Cite this chapter
Stanzel, F. (2013). Bronchoalveolar Lavage. In: Ernst, A., Herth, F. (eds) Principles and Practice of Interventional Pulmonology. Springer, New York, NY. https://doi.org/10.1007/978-1-4614-4292-9_16
Download citation
DOI: https://doi.org/10.1007/978-1-4614-4292-9_16
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4614-4291-2
Online ISBN: 978-1-4614-4292-9
eBook Packages: MedicineMedicine (R0)