Abstract
Concerning viral infection of the respiratory system, a single virus can cause a variety of clinical symptoms and the same set of symptoms can be caused by different viruses. Moreover, infection is often caused by a combination of viruses acting at the same time. The present study demonstrates, using multiplex RT-PCR and real-time qRT-PCR, that in the 2015/2016 influenza season, co-infections were confirmed in patients aged 1 month to 90 years. We found 73 co-infections involving influenza viruses, 17 involving influenza viruses and influenza-like viruses, and six involving influenza-like viruses. The first type of co-infections above mentioned was the most common, amounting to 51 cases, with type A and B viruses occurring simultaneously. There also were four cases of co-infections with influenza virus A/H1N1/pdm09 and A/H1N1/ subtypes and two cases with A/H1N1/pdm09 and A/H3N2/ subtypes. The 2015/2016 epidemic season was characterized by a higher number of confirmed co-infections compared with the previous seasons. Infections by more than one respiratory virus were most often found in children and in individuals aged over 65.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Respiratory infections constitute a major public health problem due to a high incidence rate, mortality, and well-documented healthcare and economic burden (Brydak and Nitsch-Osuch 2014; Stefańska et al. 2013). Fifty to eighty percent of acute respiratory infections are viral ones (Nitsch-Osuch et al. 2015).
The multiplex RT-PCR method is a highly sensitive alternative to other diagnostic procedures (Templeton et al. 2004). It saves time and reagents necessary to test samples for the presence of genetic material of respiratory viruses, which also expedites the introduction of proper treatment (Stefańska et al. 2012). The methods enables to detect several co-infecting contagions during a single test. The most common respiratory viruses are influenza virus type A and B, respiratory syncytial virus, parainfluenza viruses type 1, 2, 3, and human rhinovirus, human metapneumovirus, adenovirus, and human coronavirus (Do et al. 2011).
Influenza is a disease which, due to its constant evolution, causes persistent epidemics and less frequently pandemics (Brydak 2014). Co-infections with influenza viruses may induce re-assortment between the viruses, leading to a more pathogenic subtype (Liu et al. 2010). In particular, co-infections with different subtypes of influenza A virus constitute a likely source of reassortants that can acquire unpredictable properties (Pajak et al. 2011). A sectional structure of the influenza virus genome brings about the variation of genotype and phenotype of the virus. When the host cell is infected with more than one strain, viruses equipped with a new set of genes may appear. Considering the essential role of co-infections in spread and severity of the disease, the goal of this study was to determine the frequency and a crisscross pattern of co-infections with influenza and influenza-like viruses.
2 Methods
2.1 Material
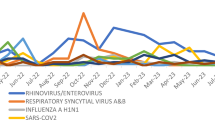
The study protocol was approved by an institutional Ethics Committee. In total, during the influenza season 2015/2016 in Poland 8542 samples from patients of all ages were tested. Swabs from the nose and throat and the washings from the bronchial tree (BALF) were taken. Specimens were tested in the Department of Influenza Research of the National Influenza Center in the National Institute of Public Health – National Institute of Hygiene and Voivodeship Sanitary Epidemiological Station in Poland. The samples prior to analysis were stored at −80 °C. Clinical specimens were collected from week 40 week of 2015 to week 34 of 2016 (October 1, 2015 – August 28, 2016).
2.2 Isolation of Viral RNA
RNA of respiratory viruses from clinical specimens were isolated using Maxwell 16 Viral Total Nucleic Acid Purification Kit (Promega Corporation, Madison, WI) in 200 μL sample suspended in PBS, according to the manufacturer’s instructions. RNA was suspended in 50 μL RNase-free water.
2.3 Real-Time qRT-PCR
The tests were performed using quantitative polymerase chain reaction RT-PCR. The analysis was carried out in the Roche Light Cycler 2.0 system. The qRT-PCR reactions were performed in capillary tubes of 20 μL volume with 0.5 μM primers and 0.2 μM probe for each reaction. The probes and primers were obtained from the Influenza Reagent Resources (IRR) program operated by the Centers for Disease Control and Prevention (CDC 2016). The reaction mixture contained MgSO4, reaction buffer, BSA, RNase free water, Super Script®III/platinum Taq mix, with the addition of 5 μL of RNA for each sample. A positive control consisted of RNA strains being components of the influenza vaccine for the season 2015/2016: A/California/7/2009 (H1N1pdm09), A/Switzerland/9715293/2013 (H3N2), B/Phuket/3073/2013, and a negative control was provided by RNase-free water. Before the start of amplification, viral RNA was rewritten to cDNA, using the reverse transcriptase enzyme at 50 °C for 30 min. Then, samples were analyzed according to the following scheme: initialization at 95 °C for 2 min and 45 cycles of amplification: denaturation at 95 °C for 15 s, annealing at 55 °C for 30 s, and extension at 72 °C for 2 min.
2.4 Conventional Multiplex RT-PCR
Samples were tested using an RV12 ACE Detection Kit (Seegene; Seoul, South Korea) that enables to detect such respiratory viruses as influenza type A and B, adenovirus (AdV), human respiratory syncytial virus A and B (RSV A and B), human coronavirus OC43 (hCoV OC43), human metapneumovirus (hMPV), rhinovirus A/B (RVA/B), human coronavirus 229/NL63 (hCoV 229/NL63), and parainfluenza type 1, 2 and 3 (PIV-1, PIV-2, PIV-3). Random hexamer-primed cDNA synthesis products were generated using the first strand cDNA synthesis kit (Fermentas; York, UK), according to the manufacturer’s instructions. Each cDNA preparation was subjected to the RV12 PCR procedure according to the manufacturer’s instructions (Seegene; Seoul, South Korea). The reaction products were detected using agarose gel electrophoresis.
3 Results
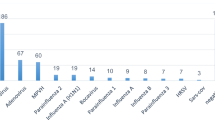
In the influenza season 2015/2016 73, co-infections with influenza viruses were reported, as shown in Table 1.
The following types of co-infections were confirmed: subtype A/H1N1/pdm09 with subtype A/H1N1/ (4 cases), subtype A/H1N1/pdm09 and subtype A/H3N2/ (2 cases), subtype A/H1N1/ and influenza virus B type (1 case), subtype A/H1N1/pdm09 and influenza type B (15 cases), and co-infection of unsubtyped type A with type B virus (51 cases).
Co-infections were reported in people of all ages, from month 1 to 90 years of age. Most co-infections caused by influenza viruses were reported among children up to 4 years of age (22 cases), in the other age-groups the number of co-infections was lower: 5–9 years – 18 cases, 10–14 years – 5 cases, 15–25 years – 3 cases, 26–44 years – 3 cases, 45–64 years – 9 cases, and ≥ 65 years of age – 13 cases (Table 1).
In the epidemic season 2015/2016 co-infections between influenza viruses and influenza-like viruses and among influenza-like viruses were noted, as shown in Table 2. Seventeen cases co-infections with influenza and influenza-like viruses were recorded. The following types of co-infections were confirmed: subtype A/H1N1/pdm09 and RSV (5 cases), A/H1N1/pdm09 and RSV and RV A/B (3 cases), A/H1N1/pdm09 with influenza type B virus and RSV (1 case), A/H1N1/pdm09 and hCoV OC43 (2 cases), A/H1N1/pdm09 and influenza type B virus and hCoV OC43 (1 case), A/H1N1/pdm09 and influenza type B virus, hMPV and RSV (1 case), influenza virus type A and RSV (2 cases), influenza virus type A and hCoV OC43 (1 case), and influenza virus type A with RV A/B (1 case). Furthermore, six co-infections of influenza-like viruses were confirmed: RSV and hCoV 229/NL63 (2 cases), RSV and RVA/B (1 case), RSV and PIV-1 (1 case), AdV and hCoV 229/NL63 (1 case), hCoV 229/NL63, and RSV and PIV-2 (1 case) (Table 2).
Concerning the regional distribution of co-infections, most of those caused by another influenza virus were observed in the provinces of Mazovia (39 cases) and Lesser-Poland (25 cases), co-infections with more than one influenza virus were noted in Sub-Carpathian (3 cases), Lower-Silesia (2 cases), and single cases in Kuyavian-Pomeranian, Silesia, and Lublin provinces (Table 3).
Co-infections of subtype A/H1N1/pdm09 with A/H1N1/, subtype A/H1N1/pdm09 with A/H3N2/, and A/H1N1/ with influenza B virus were confirmed only in the province of Mazovia (4, 2, 1 cases, respectively). Co-infections of subtype A/H1N1/pdm09 with influenza B virus were reported in Mazovia (8 cases), Sub-Carpathian, Lesser-Poland (in 2 cases), Lower-Silesia, Kuyavian-Pomeranian, and Lublin provinces (1 case each). The most frequently confirmed co-infection was a combination of infection with influenza virus type A and B, with the most cases reported in Mazovia (25) and Lesser-Poland Province (23). Moreover, in Sub-Carpathian, Silesia and Lower-Silesia Provinces one case was confirmed per each region (Table 3).
4 Discussion
The 2015/2016 epidemic season was dominated by co-infections of unsubtyped influenza A and B virus (51 cases), reported among people from 1 to 84 years of age. There were also 15 cases of subtype A/H1N1/pdm09 and influenza virus type B co-infections. Moreover, there were detected single cases of co-infections of subtype A/H1N1/ with influenza virus type B (65 years of age) and of subtype A/H1N1/pdm09 with A/H3N2/ (63 and 5 years of age). There also were four confirmed cases of co-infections between subtypes A/H1N1/pdm09 and A/H1N1/ among children up to 4 years of age and adults above 46 years of age.
Co-infections of influenza viruses with influenza-like viruses and co-infections among influenza-like viruses were reported only in children up to 11 years of age. Here, the following co-infection were detected: subtype A/H1N1/pdm09 with influenza type B virus, hMPV, and RSV (1.5 years of age). There were also four cases of co-infections with three respiratory viruses: three cases of co-infections with subtype A/H1N1/pdm09 and RSV and RV A/B, and one case of co-infection with subtype A/H1N1/pdm09, influenza type B virus and hCoV OC43 (Table 2).
In the 2015/2016 epidemic season, there was a higher number of confirmed co-infections with influenza and respiratory influenza-like viruses, compared with previous seasons. In the 2012/2013 season, co-infections were as follows: ten of subtype A/H1N1/pdm09 with A/H3N2/ and 8 of A/H3N2/ with type B virus (Czarkowski et al. 2014). In the 2013/2014 season, co-infections were as follows: two of subtype A/H1N1/pdm09 with A/H3N2/, seven of influenza with influenza-like viruses (two of influenza type A virus, RSV A virus, and RV A/B virus in one-day old and one-month-old children each), and three of influenza-like viruses (Bednarska et al. 2015). In the 2014/2015 season, in a framework of the I-MOVE (Influenza Monitoring of Vaccine Effectiveness) program, the following co-infections were detected: seven of subtype A/H1N1/pdm09 with type B virus and eight of subtype A/H3N2/ with type B virus. In that last season, in addition, one co-infection of influenza viruses and four of influenza viruses with influenza-like viruses were noted in children under 14 years of age (Hallmann-Szelińska et al. 2016). A significant increase in the number of infections with more than one respiratory virus in the 2015/2016 season could be associated with a higher number of samples tested (8542 samples) compared with the two preceding seasons (2479 and 2416 samples, respectively) (Bednarska et al. 2016; Bednarska et al. 2015). Nonetheless, influenza viruses constantly evolve, undergoing antigenic changes, which provides them the ability to elude the host immune response system (Webster et al. 2013).
References
Bednarska K, Hallmann-Szelińska E, Kondratiuk K, Brydak LB (2015) Evaluation of the activity of influenza and influenza-like viruses in the epidemic season 2013/2014. Adv Exp Med Biol 857:1–7
Bednarska K, Hallmann-Szelińska E, Brydak LB (2016) Antigenic drift of A/H3N2/ virus and circulation of influenza-like viruses during the 2014/2015 influenza season in Poland. Adv Exp Med Biol 905:33–38
Brydak LB (2008) A flu pandemic, myth or real threat? Rytm, Warsaw (Article in Polish)
Brydak LB (2014) Influenza – the greatest master of metamorphosis – constant puzzle. JHPOR 2:4–11
Brydak LB, Nitsch-Osuch A (2014) Prevention of influenza infection – a Polish perspective. Postepy Hig Med Dosw (Online) 68:137–144 (Article in Polish)
CDC (2016) http://www.cdc.gov/flu/pdf/international/program/irr.pdf. Accessed on 30 Oct 2016
Czarkowski MP, Hallmann-Szelińska E, Staszewska E, Bednarska K, Kondratiuk K, Brydak LB (2014) Influenza in Poland in 2011-2012 and in 2011/2012 and 2012/2013 epidemic seasons. Przegl Epidemiol 68:455–463
Do AH, van Doorn HR, Nghiem MN et al (2011) Viral etiologies of acute respiratory infections among hospitalized Vietnamese children in Ho Chi Minh City, 2004–2008. PLoS One 6(3):e18176
Hallmann-Szelińska E, Bednarska K, Kondratiuk K, Rabczenko D, Brydak LB (2016) Viral infections in children in the 2014/2015 epidemic season in Poland. Adv Exp Med Biol 912:51–56
Liu W, Li ZD, Tang F, Wei MT et al (2010) Mixed infections of pandemic H1N1 and seasonal H3N2 viruses in 1 outbreak. Clin Infect Dis 50(10):1359–1365
Nitsch-Osuch A, Kuchar E, Topczewska-Cabanek A, Wardyn K, Życińska K, Brydak LB (2015) Incidence and clinical course of respiratory viral coinfections in children aged 0–59 months. Adv Exp Med Biol 905:17–23
Pajak B, Stefanska I, Lepek K, Donevski S, Romanowska M, Szeliga M, Brydak LB, Szewczyk B, Kucharczyk K (2011) Rapid differentiation of mixed influenza A/H1N1/ virus infections with seasonal and pandemic variants by multitemperature single-stranded conformational polymorphism analysis. J Clin Microbiol 49(6):2216–2221
Stefańska I, Romanowska M, Brydak LB (2012) Methods of detection of selected respiratory viruses. Postepy Hig Med Dosw (Online) 66:452–460 (Article in Polish)
Stefańska I, Romanowska M, Donevski S, Gawryluk D, Brydak LB (2013) Coinfections with influenza and other respiratory viruses. Adv Exp Med Biol 756:291–301
Templeton KE, Scheltinga SA, Beersma MF, Kroes AC, Claas EC (2004) Rapid and sensitive method using multiplex real-time PCR for diagnosis of infections by influenza A and influenza B viruses, respiratory syncytial virus, and parainfluenza viruses 1, 2, 3 and 4. J Clin Microbiol 42(4):1564–1569
Webster RG, Monto AS, Braciale TJ, Lamb RA (2013) Textbook of influenza. Blackwell, London
Acknowledgements
Funded by NIPH-NIH 5/EM.1.
Conflicts of Interests
The authors declare no conflict of interests in relation to this article.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Szymański, K., Cieślak, K., Kowalczyk, D., Brydak, L. (2017). Co-infection with Influenza Viruses and Influenza-Like Virus During the 2015/2016 Epidemic Season. In: Pokorski, M. (eds) Influenza and Respiratory Care. Advances in Experimental Medicine and Biology(), vol 968. Springer, Cham. https://doi.org/10.1007/5584_2016_182
Download citation
DOI: https://doi.org/10.1007/5584_2016_182
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-51711-7
Online ISBN: 978-3-319-51712-4
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)