Abstract
Objectives
To search for optimal markers in the exhaled breath condensate (EBC), plasma and urine that would reflect the activity/severity of occupational asthma (OA) after the withdrawal from the exposure to the allergen.
Material and Methods
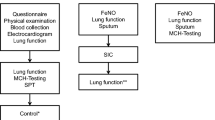
Markers of oxidative stress: 8-iso-prostaglandin {ie206-1} (8-isoprostane, 8-ISO), malondialdehyde (MDA), 4-hydroxy-trans-2-nonenale (HNE), cysteinyl leukotrienes (LT) and LTB4 were determined using liquid chromatography and mass spectrometry in 43 subjects with immunological OA (49.3±11.8 years), removed from the exposure to the sensitizing agent 10.5±6.5 years ago; and in 20 healthy subjects (49.0±14.9 years). EBC was harvested both before and after the methacholine challenge test. In parallel, identical markers were collected in plasma and urine. The results were analyzed together with forced expiratory volume in one second (FEV1), blood eosinophils, immunoglobulin E (IgE) and eosinophilic cationic protein (ECP) and statistically evaluated (Spearman rank correlation rS, two- or one-sample t tests and alternatively Kruskal Wallis or pair Wilcoxon tests).
Results
Several parameters of lung functions were lower in the patients (FEV1% predicted, MEF25% and MEF50%, Rtot%, p < 0.001). Shorter time interval since the removal from the allergen exposure correlated with higher ECP (rS = 0.375) and lower FEV1%, MEF25% and MEF50% after methacholine challenge (rS = −0.404, −0.425 and −0.532, respectively). In the patients, IgE (p < 0.001) and ECP (p = 0.009) was increased compared to controls. In EBC, 8-ISO and cysteinyl LTs were elevated in the asthmatics initially and after the challenge. Initial 8-ISO in plasma correlated negatively with FEV1 (rS = −0.409) and with methacholine PD20 (rS = −0.474). 8-ISO in plasma after the challenge correlated with IgE (rS = 0.396).
Conclusions
The improvement in OA is very slow and objective impairments persist years after removal from the exposure. Cysteinyl LTs and 8-ISO in EBC and 8-ISO in plasma might enrich the spectrum of useful objective tests for the follow-up of OA.
Similar content being viewed by others
References
Fenclová Z, Urban P, Pelclová D, Voriskova M, Havlová D. [Occupational diseases reported in the Czech Republic in 2012]. Prakt Lék. 2013;93(3):93–99. Czech.
Klusáčková P, Lebedová J, Pelclová D, Šalandová J, Šenholdová Z, Navrátil T. Occupational asthma and rhinitis in workers from a lasamide production line. Scand J Work Environ Health. 2007;33(1):74–78.
Talini D, Novelli F, Melosini L, Bacci E, Bartoli ML, Cianchetti S, et al. May the reduction of exposure to specific sensitizers be an alternative to work cessation in occupational asthma? Results from a follow-up study. Int Arch Allergy Immunol. 2012;157(2):186–193, http://dx.doi.org/10.1159/000327550.
Klusáčková P, Pelclová D, Lebedová J, Marečková H, Brabec M. Occupational asthma after withdrawal from the occupational allergen exposure. Ind Health. 2006;44(4):629–638, http://dx.doi.org/10.2486/indhealth.44.629.
Krakowiak A, Walusiak J, Krawczyk P, Wiszniewska M, Dudek W, Wittczak T, et al. IL-18 levels in nasal lavage after inhalatory challenge test with flour in bakers diagnosed with occupational asthma. Int J Occup Med Environ Health. 2008;21(2):165–172, http://dx.doi.org/10.2478/v10001-008-0015-y.
Świerczyńska-Machura D, Krakowiak A, Wiszniewska M, Dudek W, Walusiak J, Pałczyński C. Exhaled nitric oxide levels after specific inahalatory challenge test in subjects with diagnosed occupational asthma. Int J Occup Med Environ Health. 2008;21(3):219–225, http://dx.doi.org/10.2478/v10001-008-0024-x.
Čáp P, Chládek J, Pehal F, Malý M, Petrů V, Barnes PJ, et al. Gas chromatography/mass spectrometry analysis of exhaled leukotrienes in asthmatic patients. Thorax. 2004;59(6):465–470, http://dx.doi.org/10.1136/thx.2003.011866.
Al-Samri MT, Benedetti A, Préfontaine D, Olivenstein R, Lemière C, Nair P, et al. Variability of sputum inflammatory cells in asthmatic patients receiving corticosteroid therapy: A prospective study using multiple samples. J Allergy Clin Immunol. 2010;125(5):1161–1163, http://dx.doi.org/10.1016/j.jaci.2010.02.005.
Lemiere C, Chaboillez S, Welman M, Maghni K. Outcome of occupational asthma after removal from exposure: A follow-up study. Can Respir J. 2010:17(2):61–66.
Kharitonov SA, Barnes PJ. Exhaled markers of pulmonary disease. Am J Respir Crit Care Med. 2001;163(7):1693–1722.
Horvath I, Hunt J, Barnes PJ. Exhaled breath condensate: methodological recommendations and unresolved questions. Eur Res J. 2005;26(3):523–548, http://dx.doi.org/10.1183/09031936.05.00029705.
Antczak A, Górski P. Markers of pulmonary diseases in exhaled breath condensate. Int J Occup Med Environ Health. 2002;15(4):317–323.
Holgate ST, Peter-Golden M, Panettieri RA, Henderson WR. Roles of cysteinyl leukotrienes in airway inflammation, smooth muscle function, and remodeling. J Allergy Clin Immunol. 2003;111(Suppl):S18–S36.
Carpagnano GE, Kharitonov SA, Foschino-Barbaro MP, Resta O, Gramiccioni E, Barnes PJ. Increased inflammatory markers in the exhaled breath condensate of cigarette smokers. Eur Respir J. 2003;21(4):589–593, http://dx.doi.org/10.1183/09031936.03.00022203.
Montuschi P. Exhaled breath condensate: 8-isoprostane and eicosanoids. In: Horvath I, de Jongste JC, editors. Exhaled Biomarkers. Eur Respir Soc Monogr. 2010;49:196–206, http://dx.doi.org/10.1183/1025448x.00011210.
Baraldi E, Ghiro L, Piovan V, Carraro S, Ciabattoni G, Barnes PJ, et al. Increased exhaled 8-isoprostane in childhood asthma. Chest. 2003;124(1):25–31, http://dx.doi.org/10.1378/chest.124.1.25.
Klusáčková P, Lebedová J, Kačer P, Kuzma M, Brabec M, Pelclová D, et al. Leukotrienes and 8-isoprostane in exhaled breath condensate in bronchoprovocation tests with occupational allergens. Prostaglandins Leukot Essent Fatty Acids. 2008;78(4–5):281–292, http://dx.doi.org/10.1016/j.plefa.2008.03.006.
Battaglia S, den Hertog H, Timmers MC, Lazeroms SPG, Vignola AM, Rabe KF, et al. Small airways function and molecular markers in exhaled air in mild asthma. Thorax. 2005;60(8):639–644, http://dx.doi.org/10.1136/thx.2004.035279.
Bousquet J, Heinzerling L, Bachert C, Papadopoulos NG, Bousquet PJ, Burney PG, et al. Global Allergy and Asthma European Network; Allergic Rhinitis and its Impact on Asthma. Practical guide to skin prick tests in allergy to aeroallergens. Allergy. 2012;67(1):18–24, http://dx.doi.org/10.1111/j.1398-9995.2011.02728.x.
Le Moual N, Siroux V, Pin I, Kauffmann F, Kennedy SM. Epidemiological study on the genetics and environment of asthma. Asthma severity and exposure to occupational asthmogens. Am J Respir Crit Care Med. 2005;172(4):440–445.
Quanjer PH, Tammeling GJ, Cotes JE, Pedersen OF, Peslin R, Yernault JC. Lung volumes and forced ventilatory flows. Report working party. Standardization of Lung Function Tests. European Community for Steel and Coal. Official Statement of the European Respiratory Society. Eur Respir J. 1993;6(Suppl 16):5–40.
Cockcroft DW, Killian DN, Mellon JJ, Hargreave FE. Bronchial reactivity to histamine: A method and clinical survey. Clin Allergy. 1977;7(3):235–243, http://dx.doi.org/10.1111/j.1365-2222.1977.b01448.x.
Sterk PJ, Fabbri LM, Quanjer PhH, Cockcroft DW, O’Byrne PM, Anderson SD, et al. Airway Responsiveness. Standardized challenge testing with pharmacological, physical and sensitizing stimuli in adults. Report Working Party. Standardization of Lung Function Tests. European Community for Steel and Coal. Official Statement of the European Respiratory Society. Eur Respir J. 1993;6(Suppl 16):53–83.
APS Instruction manual 1986, version 2, Art. No. 780092, Erich Jaeger GmbH&Co Höchberg.
Syslová K, Kačer P, Kuzma M, Pankrácová A, Fenclová Z, Vlčková S, et al. LC-ESI-MS/MS method for oxidative stress multimarker screening in the exhaled breath condensate of asbestosis/silicosis patients. J Breath Res. 2010;4(1):017104, http://dx.doi.org/10.1088/1752-7155/4/1/017104.
Syslová K, Kačer P, Vilhanová B, Kuzma M, Lipovová P, Fenclová Z, et al. Determination of cysteinyl leukotrienes in exhaled breath condensate: method combining immunoseparation with LC-ESI-MS/MS. J Chromatogr B. 2011;879(23):2220–2228, http://dx.doi.org/10.1016/j.jchromb.2011.06.004.
Syslová K, Kačer P, Kuzma M, Lebedová J, Klusáčková P, Fenclová Z, et al. Determination of 8-iso-prostaglandin F2a in exhaled breath condensate by method combining immunoseparation with LC-ESI-MS. J Chromatogr B. 2008;867(1):8–14, http://dx.doi.org/10.1016/j.jchromb.2008.02.019.
Syslová K, Kačer P, Kuzma M, Najmanová V, Fenclová Z, Vlčková S, et al. Rapid and easy method for monitoring oxidative stress markers in body fluids of patients with asbestos or silica-induced lung diseases. J Chromatogr B. 2009;877(24):2477–2486, http://dx.doi.org/10.1016/j.jchromb.2009.06.008.
Ono E, Mita H, Taniguchi M, Higashi N, Tsuburai T, Hasegawa M, et al. Increase in inflammatory mediator concentrations in exhaled breath condensate after allergen inhalation. J Allergy Clin Immunol. 2008;122(4):768–773, http://dx.doi.org/10.1016/j.jaci.2008.06.009.
Author information
Authors and Affiliations
Corresponding author
Additional information
Study support was provided by the Research Project of the Charles University in Prague P28/LF/6 and EU Project “Material-technical Research Base for the Diagnostics and Treatment of Environmentally-caused and Oncological Disorders and their Risks, in the General University Hospital in Prague” (reg. No. CZ.2.16/3.1.00/24012) from OP Prague Competitiveness. Manager of project: Jan Malík, Professor, MD, PhD.
About this article
Cite this article
Pelclová, D., Fenclová, Z., Vlčková, Š. et al. Occupational asthma follow-up — which markers are elevated in exhaled breath condensate and plasma?. IJOMEH 27, 206–215 (2014). https://doi.org/10.2478/s13382-014-0243-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.2478/s13382-014-0243-2