Abstract
The prevalence of type 2 diabetes mellitus is high among the elderly population. Treatment of elderly patients with type 2 diabetes presents challenges because of co-morbidities and the potential increase in the risk of adverse effects. Hyperlipidaemia is also common in the elderly population. Glucose-and lipid-lowering treatment in elderly patients should be individualized on the basis of the patient’s life expectancy, health status and cardiovascular risk factors, and evidence-based guideline recommendations. Because elderly patients often have impaired renal and hepatic function, careful considerations must be made when selecting appropriate glucose- and lipid-lowering therapy. There are a number of potential safety issues associated with various glucose- and lipid-lowering therapies that are relevant to elderly patients, including increased risk of heart failure exacerbations, weight loss, increased risk of hypoglycaemia, increased risk of myopathy, and contraindications of some agents in patients with hepatic or renal impairment. The bile acid sequestrant colesevelam HCl is unique compared with other glucose- and lipid-lowering therapies because it is the only product approved by the US Food and Drug Administration, as an adjunct to diet and exercise, to lower both glucose and low-density lipoprotein cholesterol (LDL-C) in adults with type 2 diabetes and primary hyperlipidaemia, respectively. Furthermore, colesevelam has been shown to have similar glucose- and lipid-lowering efficacy in patients aged <65 years and those aged ≥65 years. Colesevelam was not associated with weight gain, was associated with a low incidence of hypoglycaemia, and can be safely combined with a broad range of glucose-lowering agents (metformin, sulfonylureas and insulin) and lipid-lowering statins. Currently, colesevelam is available in tablet form and as a powder for oral suspension formulation; the latter may be of benefit to elderly patients with swallowing difficulties. As colesevelam has both glucose- and lipid-lowering effects, its use may reduce the drug burden in elderly patients receiving multiple agents for glucose and lipid lowering. Colesevelam may be a valuable treatment option as an add-on to existing glucose- and/or lipid-lowering therapy to help improve haemoglobin A1c and to lower LDL-C levels in elderly patients with type 2 diabetes and primary hyperlipidaemia.
Similar content being viewed by others
1. Introduction
Diabetes mellitus is a chronic disease characterized by persistent hyperglycaemia, which is associated with increased morbidity and mortality.[1] Globally, the age-standardized prevalence of diabetes in adults aged 20–79 years has been estimated at 8.3% in 2011, and is projected to increase to 9.9% by 2030.[2] The majority of individuals with diabetes (90%) have type 2 diabetes mellitus,[3] a progressive disease characterized by pancreatic β-cell dysfunction and increased insulin resistance.[1] Epidemiological data on diabetes by age group are limited, but US data indicate that the prevalence of diabetes is high among the elderly. In the US, the prevalence of diabetes increased by 62% from 1994 to 2003 among individuals >65 years of age.[4] It was estimated that 10.9 million individuals (26.9%) aged ≥65 years within the US had diabetes in 2010.[5]
Hyperlipidaemia is a major risk factor for cardiovascular complications in patients with type 2 diabetes, regardless of age.[6,7] Hyperlipidaemia in patients with type 2 diabetes is associated with high atherogenic risk and is characterized by elevated triglyceride levels, low high-density lipoprotein cholesterol (HDL-C) levels, and a shift towards small, dense, low-density lipoprotein particles.[6,8–10] Although low-density lipoprotein cholesterol (LDL-C) levels in patients with diabetes are generally similar to those in the general population,[8] patients with diabetes can benefit from LDL-C reduction, even in the absence of elevated LDL-C levels.[11] In addition, data from the Framingham Heart Study indicate that hyperlipidaemia, obesity and cardiovascular disease often precede the development of type 2 diabetes in older patients.[12] The overall prevalence of hyperlipidaemia (defined as an LDL-C level above that recommended by the National Cholesterol Education Program [NCEP] Adult Treatment Panel III [ATP III] {i.e. <160 mg/dL for patients with 0–1 risk factor, <130 mg/dL for those with multiple risk factors, and <100 mg/dL for those with coronary heart disease and coronary heart disease risk equivalents[13]} or treatment with a lipid-lowering agent) has been reported to be as high as 60.3% in patients aged ≥65 years.[14]
Although many treatments exist for control of glucose and lipid levels in patients with type 2 diabetes, some are contraindicated in the presence of conditions that may be prevalent in the elderly. In addition, some treatments are associated with an increased risk of adverse effects in the general population and, to a greater degree, in elderly patients. It is important to tailor treatment to the needs of individual patients with type 2 diabetes, especially those who are elderly, in order to improve outcomes.[15] The bile acid sequestrant colesevelam HCl is an established treatment for lowering LDL-C levels in adults with primary hyperlipidaemia, but is not considered first-line lipid-lowering therapy in adults with diabetes, since statins are recommended first.[1] Colesevelam is approved in the US for use in combination with a statin, and could be used in patients with diabetes who require LDL-C lowering beyond that achieved with a statin. Colesevelam is also approved in Canada, the EU, Iceland and Norway for the treatment of hypercholesterolaemia. In January 2008, colesevelam was also approved by the US Food and Drug Administration (FDA) for improving glycaemic control in adults with type 2 diabetes.[16] In this review, the challenges associated with controlling hyperglycaemia and hyperlipidaemia in elderly patients are discussed, with a focus on colesevelam in the context of targeting appropriate glycaemic and lipid-lowering goals in the elderly population. This non-systematic review of the treatment of elderly patients with type 2 diabetes is based on manual literature searches.
2. Managing Hyperglycaemia and Hyperlipidaemia in the Elderly
Treatment of diabetes (type 1 or type 2) is often suboptimal, particularly in those aged ≥65 years.[14,17] Data from the National Health and Nutrition Examination Survey from 1999 to 2004 indicate that 50.9% of elderly patients with diabetes (type 1 or type 2) are treated pharmacologically; however, only 50.4% of treated patients achieve glycaemic control (defined as haemoglobin A1c [HbA1c] <7.0%).[14] Recent clinical trials in the type 2 diabetes patient population have been unable to show reduced cardiovascular events with aggressive HbA1c targets.[18] The low percentage of elderly patients who received pharmacological treatment may be due to a range of issues relating to perceived vulnerability, co-morbidity, tolerability, polypharmacy, less aggressive glycaemic targets and psychosocial issues.[14,15,19] Similarly, only 64.9% of elderly patients who received treatment to manage their hyperlipidaemia achieved the NCEP ATP III-recommended target LDL-C level.[14]
2.1 Hyperglycaemia
The American Diabetes Association (ADA), the American Association of Clinical Endocrinologists (AACE) and the International Diabetes Federation (IDF) recommend HbA1c targets of <7.0%, ≤6.5% and <6.5%, respectively, in all non-pregnant adults with diabetes, although the ADA recommends that the goals be individualized on the basis of a number of factors, including age/life expectancy.[1,20,21] Less intensive glycaemic targets (e.g. HbA1c <8.0%) are recommended in older adults with limited life expectancy, advanced diabetes complications and/or cardiovascular disease.[18,22] Alternatively, a significant minority of elderly patients with longer life expectancy might benefit from intensive management of hyperglycaemia with a target HbA1c of <7.0%.[1,18,23] A study evaluating the implementation of American Geriatrics Society guidelines recommending an HbA1c target of <8.0% in frail older adults (aged ≥55 years) found that patients had fewer hyperglycaemic episodes, lower HbA1c values and greater use of glucose-lowering agents, but also found that there was a significant increase in the incidence of severe hypoglycaemia during the early implementation period.[24]
2.2 Hyperlipidaemia
Although primary hyperlipidaemia has specific typical characteristics, studies suggest that the benefit derived from lipid-lowering therapy with an HMG-CoA reductase inhibitor (statin) in terms of cardiovascular outcomes is comparable in patients with and without diabetes (type 1 or type 2).[8] The HPS (Heart Protection Study) and the CARDS (Collaborative Atorvastatin Diabetes Study) demonstrated that treatment with simvastatin or atorvastatin, respectively, significantly reduced the risk of cardiovascular events in patients with diabetes (type 1 or type 2 in the HPS and type 2 in the CARDS).[25,26] Furthermore, results from the HPS indicated that the reduction in risk of cardiovascular events reported with statin therapy was similar in patients with and without diabetes (type 1 or type 2).[25] A meta-analysis of clinical studies evaluating statin therapy showed that patients with diabetes who were aged ≤65 and >65 years benefited to a similar extent from LDL-C lowering regardless of baseline lipid profile.[27]
Lipid-lowering targets for patients with type 2 diabetes or at cardiometabolic risk are shown in table I.[1,20,21,28] Slight variation exists among targets advocated by the ADA, NCEP, AACE and IDF for patients with type 2 diabetes,[1,20,21] and those recommended by the ADA/American College of Cardiology Foundation (ACCF) for patients at cardiometabolic risk.[28] Treatment guidelines often do not provide separate recommendations for elderly patients; however, treatment in elderly patients should be individualized on the basis of physiological/functional age.[30] The ADA recommends statin treatment in all patients with diabetes who have established cardiovascular disease, or those without cardiovascular disease and at least one cardiovascular risk factor who are >40 years of age, irrespective of baseline lipid values.[1]
The American Diabetes Association (ADA), the National Cholesterol Education Program (NCEP), the American Association of Clinical Endocrinologists (AACE) and the International Diabetes Federation (IDF) lipid targets in patients with type 2 diabetes mellitus, and the ADA/American College of Cardiology Foundation (ACCF) lipid and lipoprotein targets in patients at cardiometabolic risk[1,20,21,28,29]
Although the association between hyperlipidaemia and cardiovascular risk weakens with age, older patients have a higher baseline risk because of other risk factors, and may benefit more from lipid-lowering treatment.[31] Therefore, those expected to survive >1 year should be strongly considered for primary and secondary prevention efforts as recommended by the NCEP and ADA.[1,13]
3. Safety/Adherence Concerns in Elderly Patients with Type 2 Diabetes
The risk of hypoglycaemia with glucose-lowering agents is higher in elderly patients with type 2 diabetes because of altered pharmacokinetics, impaired metabolism, co-morbid conditions that can mask hypoglycaemia, impaired perception or isolation preventing early identification and treatment of hypoglycaemia, poor nutrition, polypharmacy, and/or cognitive impairment leading to non-adherence (e.g. reduced dose interval or increased dose taken in error).[19,32]
Reduced renal and hepatic function can be present in elderly patients,[33] and therefore, pharmacological agents must be selected carefully on the basis of where they are metabolized or excreted from the body. Decreased renal function slows the drug metabolized through the kidneys, which can decrease drug clearance, resulting in increased plasma concentrations, which can potentially lead to adverse effects.[19] Consequently, doses of pharmacological agents may need to be adjusted in elderly patients. Congestive heart failure (CHF) is most common in the elderly, and diabetes is an independent predictor for CHF in the elderly.[34–36] In addition, elderly patients with type 2 diabetes often have other co-morbid conditions, including hypertension, coronary artery disease and hyperlipidaemia. The use of polypharmacy may lead to drug-drug interactions, altered drug pharmacokinetics and adherence issues.[19] Furthermore, difficulty swallowing, frailty and reduced manual dexterity may make some drugs more difficult to take.
4. Agents Used for the Treatment of Type 2 Diabetes in the Elderly
4.1 Agents Used for Managing Hyperglycaemia
Current treatment options for glucose control in type 2 diabetes are shown in table II. Oral glucose-lowering agents are widely used for the treatment of type 2 diabetes to control blood glucose levels. These agents include insulin secretagogues, including sulfonylureas (glipizide, glyburide and glimepiride) and meglitinides (repaglinide and nateglinide); biguanides (metformin); thiazolidinediones (rosiglitazone and pioglitazone); α-glucosidase inhibitors (acarbose); dipeptidyl peptidase-IV (DPP-IV) inhibitors (linagliptin, saxagliptin and sitagliptin); and bile acid sequestrants (colesevelam). Injectable glucose-lowering agents include glucagon-like peptide-1 (GLP-1) analogues (exenatide and liraglutide) and insulin (short and long acting). Traditionally, insulin is initiated when elevated blood glucose levels persist despite oral glucose-lowering therapy (generally starting with basal insulin and then transitioning to bolus insulin with meals) or when a patient presents with HbA1c >9.0% and symptomatic hyperglycaemia, regardless of whether they are on treatment or are treatment-naive.[20]
4.1.1 Limitations of Glucose-Lowering Agents Used in the Treatment of Elderly Patients with Type 2 Diabetes
There are a number of potential safety issues associated with the use of various glucose-lowering agents that are relevant to elderly patients, which are summarized in table II.[19,23,37–39]
Chronic use of thiazolidinediones may cause bone loss, which can increase the risk of fractures, especially in older women.[43–45] Both thiazolidinediones and meglitinides can be used in patients with impaired renal function since these agents are not metabolized via the kidney; however, both classes of glucose-lowering agents require monitoring of liver function, and should be used with caution in patients with hepatic impairment.[19] Rosiglitazone may increase the risk of myocardial infarction.[46] In addition, thiazolidinediones can cause or exacerbate CHF in some patients; thus, monitoring for heart failure is required after initiating these drugs, and they are contraindicated in patients with established New York Heart Association functional class III or IV heart failure.[40,46,47] Based on the potential for rosiglitazone to increase cardiovascular risk, the marketing authorization for rosiglitazone-based medications in the EU has been suspended,[48] and, in the US, the FDA has created a Risk Evaluation and Mitigation Strategy (REMS) programme to restrict access and distribution and monitor patients taking the medication.[49] Recently, the FDA warned that use of pioglitazone for >1 year may be associated with an increased risk of bladder cancer, and therefore it should not be used in patients with active bladder cancer and should be used with caution in those with a history of bladder cancer.[50]
Metformin is contraindicated in patients with renal disease or dysfunction (serum creatinine levels of ≥1.5 mg/dL in males or ≥1.4 mg/dL in females),[41] and may not be suitable in elderly patients who are underweight or frail, those with hepatic impairment or those with CHF.[37,51] Recent recommendations on the use of metformin in patients with compromised renal function has suggested their safe use down to an estimated glomerular filtration rate of 30 mL/min/1.73 m2.[52] Gastrointestinal effects may occur with metformin (metallic taste, anorexia, nausea, abdominal pain and diarrhoea), acarbose (abdominal discomfort, increased formation of intestinal gas and diarrhoea) and colesevelam (primarily constipation).[53] The gastrointestinal issues associated with metformin can be minimized by a slow initial titration as suggested by the ADA.[42]
The risk of hypoglycaemia with sulfonylureas and meglitinides is increased in the elderly, particularly in patients with renal impairment.[37] Although data are limited regarding the use of DPP-IV inhibitors in the elderly, DPP-IV inhibitors appear to have benign tolerability profiles and a low risk of hypoglycaemia; however, for those agents that are renally excreted, dose adjustments are necessary in patients with renal impairment.[37,54]
In the general adult diabetes population, α-glucosidase inhibitor use is uncommon, and this holds true in the elderly population, possibly as a result of its minimal effectiveness compared with other available glucose-lowering agents. In addition, α-glucosidase inhibitors are associated with gastrointestinal effects (flatulence and diarrhoea), should be avoided in patients with renal impairment, and may increase the risk of hypoglycaemia when combined with prandial insulin.[37]
Insulin use is complex and has a high risk of hypoglycaemia if taken inappropriately; therefore, if glycaemic control is achievable without it, insulin use should be avoided in elderly patients who have reduced cognitive function or poor manual dexterity.[37]
Some glucose-lowering agents affect weight. Sulfonylureas and thiazolidinediones are both associated with weight gain.[55] The DPP-IV inhibitors are generally weight neutral, but the GLP-1 analogues are associated with significant weight loss,[56,57] which, although useful in overweight or obese elderly patients, might potentially be less beneficial in frail elderly patients or patients with a low body mass index at baseline.
4.2 Agents Used for Managing Primary Hyperlipidaemia
Pharmacotherapy for the treatment of primary hyperlipidaemia across various co-morbidities focuses on statin therapy as first-line treatment, but allows for the addition of other lipid-lowering therapies depending on patient cholesterol values and co-morbidities, and avoidance of drug-drug interactions. Current treatment options for managing the lipid profile in adults with type 2 diabetes are summarized in table III. These options include statins, niacin, fibrates (gemfibrozil and fenofibrate), bile acid sequestrants (colesevelam, cholestyramine and colestipol), and cholesterol absorption inhibitors (ezetimibe). Statins are the first-line treatment for LDL-C lowering for all patients, including those with type 2 diabetes; however, their use may be restricted or contraindicated in some patients (e.g. because of drug-drug interactions).[1,8]
4.2.1 Limitations of Lipid-Lowering Agents Used in the Treatment of Elderly Patients with Type 2 Diabetes
The limitations of lipid-lowering agents in elderly patients with type 2 diabetes are summarized in table III.[30,38,58,59] Primary and secondary prevention trials have demonstrated the efficacy and tolerability of lipid-lowering therapy in elderly patients with hyperlipidaemia[60,61] and in patients with type 2 diabetes,[6,10] but data in elderly patients with type 2 diabetes are limited.
There are a number of potential safety issues associated with lipid-lowering therapy that are relevant to elderly patients with type 2 diabetes. In general, statins are well tolerated.[62,63] However, statin therapy has been associated with muscle injury and hepatotoxicity. According to information in the product labelling from controlled studies, 1–5% of patients receiving statins may develop myalgia, although the incidence of this is not significantly different to that in patients given placebo.[62] A review of a drug safety database, Qscan-FDA (DrugLogic, Inc., Reston, VA, USA), from January 1990 through to March 2002 identified 3339 cases of statin-associated rhabdomyolysis.[62] A subsequent analysis of data from November 1997 to March 2000 identified 612 cases of rhabdomyolysis, with one-half of the reported cases occurring in patients aged 51–75 years.[62] Concomitant use of gemfibrozil and niacin were found to increase the risk of statin-associated myopathy (primarily associated with statins that have a drug-drug interaction with gemfibrozil, including lovastatin, simvastatin and rosuvastatin).[62,64] In June 2011, the FDA initiated label changes for products containing simvastatin to include restrictions on the use of a simvastatin dose of 80 mg/day, because of an elevated risk of myopathy at this dosage.[65] The FDA recommends that simvastatin 80 mg/day should only be used in patients who have already taken this dose for ≥12 months without evidence of myopathy. Combination therapy may be a safer alternative to help patients achieve LDL-C goals without requiring high statin dosages such as these. Elevated liver enzyme levels during statin treatment are not uncommon, but studies have suggested that the incidence of aminotransferase levels of >3 times the upper limit of normal is approximately 1–3%, and is not significantly different to that in patients given placebo.[66–70] The FDA recently updated statin labels to recommend performing liver enzyme tests before initiation of therapy and as clinically indicated thereafter (as opposed to routine periodic monitoring as was previously recommended).[71] Importantly, there does not appear to be an association between increased age and risk of significant liver injury.[63] The updated statin labels also include a warning regarding reports of cognitive impairment associated with statin use, which may be of particular concern in elderly patients.[71]
Niacin has the potential to worsen glycaemic control,[59] although studies have shown that immediate-release niacin, as well as low doses of extended-release niacin, can be used safely in patients with type 2 diabetes.[72–74] There are also data suggesting that some statins may worsen glycaemic control or increase the risk of new-onset type 2 diabetes, as illustrated by findings with atorvastatin.[75–77] Bile acid sequestrants (colesevelam, cholestyramine and colestipol) are associated with gastrointestinal effects, primarily constipation.[78] Finally, the use of fibrates may be limited in some elderly patients because they are contraindicated in patients with hepatic or severe renal impairment.[79,80]
4.3 Role of Colesevelam in Managing Lipid and Glucose Levels
Bile acid sequestrants were initially approved for reducing LDL-C levels. However, cholestyramine and colesevelam have also been shown to exert significant glucose-lowering effects in patients with type 2 diabetes.[81–85] In 2008, colesevelam received approval from the FDA for improving glycaemic control in adults with type 2 diabetes.[16] In addition to a tablet formulation, colesevelam may be taken as an oral suspension, which may be beneficial for elderly patients who may have swallowing difficulties, and could facilitate patient adherence to treatment.
4.3.1 Efficacy
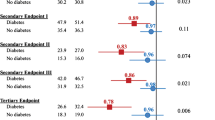
In three randomized, double-blind, placebo-controlled studies, colesevelam significantly lowered mean HbA1c (treatment difference vs placebo: −0.50% to −0.54%; p < 0.001 for all) and LDL-C levels (−12.8% to −16.7%; p < 0.001 for all) in adults with type 2 diabetes when added to stable metformin-, insulin- or sulfonylurea-based therapy.[83–85] A post hoc analysis on pooled data from the three above-mentioned double-blind, placebo-controlled studies (n = 1018) showed that colesevelam significantly reduced the levels of mean HbA1c, LDL-C, non–HDL-C and total cholesterol compared with placebo in both the <65 and ≥65 years of age subpopulations.[86,87] The effect of colesevelam on cardiovascular morbidity and mortality has not been established.
In addition, colesevelam has shown a dose-sparing effect on statin therapy when used in combination, but a statin dose potent enough to achieve a 30–40% reduction in LDL-C levels should be targeted.[88–90] Therefore, combining colesevelam with a moderate dose of a statin may be appropriate for adults who have not achieved lipid targets with higher statin doses, or for adults who may be susceptible to adverse effects when receiving a high dose of a statin.[59] However, adults who require substantial LDL-C lowering may still need to receive a high-potency statin dose, either alone or in combination with additional LDL-C-lowering agents.
4.3.2 Safety and Tolerability
Colesevelam is not systemically absorbed; therefore, the potential for systemic adverse events is low, and patients receiving colesevelam do not require routine monitoring of liver function. In clinical studies, the overall incidence of adverse events with colesevelam was similar to placebo.[83–85] Colesevelam has also been shown to be weight neutral and have a low risk of hypoglycaemia.[83–85] The most common adverse event reported with colesevelam is constipation; clinical studies have shown that the incidence of constipation was higher with colesevelam compared with placebo.[83–85] Constipation could be more problematic for the elderly than for the general population.[91]
However, colesevelam increased triglyceride levels compared with placebo treatment (p < 0.001 when added to insulin- or sulfonylurea-based therapy).[83–85] Similarly, in the age-based subgroup analysis, triglyceride levels were significantly increased with colesevelam treatment in both age subgroups (colesevelam vs placebo treatment difference: <65 years, +14.7% [p < 0.0001]; ≥65 years, +14.2% [p = 0.0036]).[87] A number of studies have suggested an association between triglyceride levels and cardiovascular risk; however, this is controversial, with the effect size typically modest compared with other cardiovascular risk factors (including other lipid parameters).[92] In addition, although triglyceride levels are closely associated with type 2 diabetes, studies evaluating the association between triglycerides and cardiovascular risk often do not include type 2 diabetes as a confounding factor.[92] Because colesevelam increases triglyceride levels, it is contraindicated in patients with triglyceride levels of >500 mg/dL.[16]
5. Conclusions
The prevalence of type 2 diabetes is increasing among elderly individuals in the US and worldwide. Elderly patients with type 2 diabetes can be difficult to treat because of co-morbidities and an increased risk of adverse effects with pharmacological treatments. In addition, hyperlipidaemia represents a particular health concern among elderly patients with diabetes. The proven efficacy, once- or twice-daily dosing, and dual formulations of the bile acid sequestrant colesevelam make it a treatment option as an add-on to existing glucose-lowering therapy or lipid-lowering statins for control of primary hyperlipidaemia and hyperglycaemia in elderly patients with type 2 diabetes not achieving treatment targets. However, the effect of colesevelam on cardiovascular morbidity and mortality has not been established.
References
American Diabetes Association. Standards of medical care in diabetes-2011. Diabetes Care 2011 Jan; 34 (Suppl. 1): S11–61
Whiting DR, Guariguata L, Weil C, et al. IDF Diabetes Atlas: global estimates of the prevalence of diabetes for 2011 and 2030. Diabetes Res Clin Pract. Epub 2011 Nov 11
Chen L, Magliano DJ, Zimmet PZ. The worldwide epidemiology of type 2 diabetes mellitus-present and future perspectives. Nat Rev Endocrinol. Epub 2011 Nov 8
Sloan FA, Bethel MA, Ruiz Jr D, et al. The growing burden of diabetes mellitus in the US elderly population. Arch Intern Med 2008 Jan 28; 168 (2): 192–9
Centers for Disease Control and Prevention. National diabetes fact sheet: national estimates and general information on diabetes and prediabetes in the United States, 2011. Atlanta (GA): U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, 2011 [online]. Available from URL: http://www.cdc.gov/diabetes/pubs/pdf/ndfs_2011.pdf [Accessed 2012 Feb 23]
Farmer JA. Diabetic dyslipidemia and atherosclerosis: evidence from clinical trials. Curr Diab Rep 2008 Feb; 8 (1): 71–7
Turner RC, Millns H, Neil HA, et al. Risk factors for coronary artery disease in non-insulin dependent diabetes mellitus: United Kingdom Prospective Diabetes Study (UKPDS: 23). BMJ 1998 Mar 14; 316 (7134): 823–8
Solano MP, Goldberg RB. Management of dyslipidemia in diabetes. Cardiol Rev 2006 May–Jun; 14 (3): 125–35
Adiels M, Olofsson SO, Taskinen MR, et al. Overproduction of very low-density lipoproteins is the hallmark of the dyslipidemia in the metabolic syndrome. Arterioscler Thromb Vasc Biol 2008 Jul; 28 (7): 1225–36
Brunzell JD, Ayyobi AF. Dyslipidemia in the metabolic syndrome and type 2 diabetes mellitus. Am J Med 2003 Dec 8; 115 (Suppl. 8A): 24S–8S
Howard BV, Robbins DC, Sievers ML, et al. LDL cholesterol as a strong predictor of coronary heart disease in diabetic individuals with insulin resistance and low LDL: the Strong Heart Study. Arterioscler Thromb Vasc Biol 2000 Mar; 20 (3): 830–5
Wilson PW, Anderson KM, Kannel WB. Epidemiology of diabetes mellitus in the elderly. The Framingham Study. Am J Med 1986 May 16; 80 (5A): 3–9
Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive Summary of the Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). JAMA 2001 May 16; 285 (19): 2486–97
McDonald M, Hertz RP, Unger AN, et al. Prevalence, awareness, and management of hypertension, dyslipidemia, and diabetes among United States adults aged 65 and older. J Gerontol A Biol Sci Med Sci 2009 Feb; 64 (2): 256–63
Meneilly GS, Tessier D. Diabetes in elderly adults. J Gerontol A Biol Sci Med Sci 2001 Jan; 56 (1): M5–13
Welchol® (colesevelam hydrochloride) tablets: US prescribing information. Parsippany (NJ): Daiichi Sankyo, Inc., 2010
Saydah SH, Fradkin J, Cowie CC. Poor control of risk factors for vascular disease among adults with previously diagnosed diabetes. JAMA 2004 Jan 21; 291 (3): 335–42
Ismail-Beigi F, Moghissi E, Tiktin M, et al. Individualizing glycemic targets in type 2 diabetes mellitus: implications of recent clinical trials. Ann Intern Med 2011 Apr 19; 154 (8): 554–9
Rosenstock J. Management of type 2 diabetes mellitus in the elderly: special considerations. Drugs Aging 2001; 18 (1): 31–44
Handelsman Y, Mechanick JI, Blonde L, et al. American Association of Clinical Endocrinologists Medical Guidelines for Clinical Practice for developing a diabetes mellitus comprehensive care plan. Endocr Pract 2011 Mar–Apr; 17 (Suppl. 2): 1–53
IDF Clinical Guidelines Task Force. Global guideline for type 2 diabetes. Brussels: International Diabetes Federation, 2005
Selvin E, Steffes MW, Zhu H, et al. Glycated hemoglobin, diabetes, and cardiovascular risk in nondiabetic adults. N Engl J Med 2010 Mar 4; 362 (9): 800–11
Cayea D, Boyd C, Durso SC. Individualising therapy for older adults with diabetes mellitus. Drugs Aging 2007; 24 (10): 851–63
Lee SJ, Boscardin WJ, Stijacic Cenzer I, et al. The risks and benefits of implementing glycemic control guidelines in frail older adults with diabetes mellitus. J Am Geriatr Soc 2011 Apr; 59 (4): 666–72
Collins R, Armitage J, Parish S, et al. MRC/BHF Heart Protection Study of cholesterol-lowering with simvastatin in 5963 people with diabetes: a randomised placebo-controlled trial. Lancet 2003 Jun 14; 361 (9374): 2005–16
Colhoun HM, Betteridge DJ, Durrington PN, et al. Primary prevention of cardiovascular disease with atorvastatin in type 2 diabetes in the Collaborative Atorvastatin Diabetes Study (CARDS): multicentre randomised placebo-controlled trial. Lancet 2004 Aug 21–27; 364 (9435): 685–96
Kearney PM, Blackwell L, Collins R, et al. Efficacy of cholesterol-lowering therapy in 18,686 people with diabetes in 14 randomised trials of statins: a meta-analysis. Lancet 2008 Jan 12; 371 (9607): 117–25
Brunzell JD, Davidson M, Furberg CD, et al. Lipoprotein management in patients with cardiometabolic risk: consensus statement from the American Diabetes Association and the American College of Cardiology Foundation. Diabetes Care 2008 Apr; 31 (4): 811–22
Grundy SM, Cleeman JI, Merz CN, et al. Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III guidelines. Circulation 2004 Jul 13; 110 (2): 227–39
Jellinger PS, Dickey RA, Ganda OP, et al. AACE medical guidelines for clinical practice for the diagnosis and treatment of dyslipidemia and prevention of atherogenesis. Endocr Pract 2000 Mar–Apr; 6 (2): 162–213
Lewis SJ, Moye LA, Sacks FM, et al. Effect of pravastatin on cardiovascular events in older patients with myocardial infarction and cholesterol levels in the average range. Results of the Cholesterol and Recurrent Events (CARE) trial. Ann Intern Med 1998 Nov 1; 129 (9): 681–9
Wallace JI. Management of diabetes in the elderly. Clin Diabetes 1999; 17: 19–25
Mangoni AA, Jackson SH. Age-related changes in pharmacokinetics and pharmacodynamics: basic principles and practical applications. Br J Clin Pharmacol 2004 Jan; 57 (1): 6–14
Gottdiener JS, Arnold AM, Aurigemma GP, et al. Predictors of congestive heart failure in the elderly: the Cardiovascular Health Study. J Am Coll Cardiol 2000 May; 35 (6): 1628–37
Rich MW. Epidemiology, pathophysiology, and etiology of congestive heart failure in older adults. J Am Geriatr Soc 1997 Aug; 45 (8): 968–74
Schocken DD, Arrieta MI, Leaverton PE, et al. Prevalence and mortality rate of congestive heart failure in the United States. J Am Coll Cardiol 1992 Aug; 20 (2): 301–6
Neumiller JJ, Setter SM. Pharmacologic management of the older patient with type 2 diabetes mellitus. Am J Geriatr Pharmacother 2009 Dec; 7 (6): 324–42
Reasner CA. Reducing cardiovascular complications of type 2 diabetes by targeting multiple risk factors. J Cardiovasc Pharmacol 2008 Aug; 52 (2): 136–44
Inzucchi SE, McGuire DK. New drugs for the treatment of diabetes: part II. Incretin-based therapy and beyond. Circulation 2008 Jan 29; 117 (4): 574–84
Nesto RW, Bell D, Bonow RO, et al. Thiazolidinedione use, fluid retention, and congestive heart failure: a consensus statement from the American Heart Association and American Diabetes Association. October 7, 2003. Circulation 2003 Dec 9; 108 (23): 2941–8
Glucophage® (metformin hydrochloride) tablets; Glucophage® XR (metformin hydrochloride) extended-release tablets: US prescribing information. Princeton (NJ): Bristol-Myers Squibb Company, 2009
Nathan DM, Buse JB, Davidson MB, et al. Medical management of hyperglycemia in type 2 diabetes: a consensus algorithm for the initiation and adjustment of therapy: a consensus statement of the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care 2009 Jan; 32 (1): 193–203
Schwartz AV, Sellmeyer DE, Vittinghoff E, et al. Thiazolidinedione use and bone loss in older diabetic adults. J Clin Endocrinol Metab 2006 Sep; 91 (9): 3349–54
Lecka-Czernik B. Bone loss in diabetes: use of antidiabetic thiazolidinediones and secondary osteoporosis. Curr Osteoporos Rep 2010 Dec; 8 (4): 178–84
Kahn SE, Zinman B, Lachin JM, et al. Rosiglitazone-associated fractures in type 2 diabetes: an analysis from A Diabetes Outcome Progression Trial (ADOPT). Diabetes Care 2008 May; 31 (5): 845–51
Avandia® (rosiglitazone maleate) tablets: US prescribing information. Research Triangle Park (NC): GlaxoSmith-Kline, 2011
Actos (pioglitazone) tablets: US prescribing information. Deerfield (IL): Takeda Pharmaceuticals America Inc., 2011
European Medicines Agency. Questions and answers on the suspension of rosiglitazone-containing medicines (Avandia, Avandamet and Avaglim) [online]. Available from URL: http://www.ema.europa.eu/docs/en_GB/document_library/Medicine_QA/2010/09/WC500097003.pdf [Accessed 2011 Oct 27]
US Food and Drug Administration. Avandia (rosiglitazone): REMS — risk of cardiovascular events [online]. Available from URL: http://www.fda.gov/Safety/MedWatch/SafetyInformation/SafetyAlertsforHumanMedicalProducts/ucm226994.htm [Accessed 2011 Oct 27]
US Food and Drug Administration. FDA Drug Safety Communication: update to ongoing safety review of Actos (pioglitazone) and increased risk of bladder cancer [online]. Available from URL: http://www.fda.gov/Drugs/DrugSafety/ucm259150.htm [Accessed 2011 Jul 25]
Choy CK, Rodgers JE, Nappi JM, et al. Type 2 diabetes mellitus and heart failure. Pharmacotherapy 2008 Feb; 28 (2): 170–92
Lipska KJ, Bailey CJ, Inzucchi SE. Use of metformin in the setting of mild-to-moderate renal insufficiency. Diabetes Care 2011 Jun; 34 (6): 1431–7
Rodbard HW, Jellinger PS, Davidson JA, et al. Statement by an American Association of Clinical Endocrinologists/American College of Endocrinology consensus panel on type 2 diabetes mellitus: an algorithm for glycemic control. Endocr Pract 2009 Sep–Oct; 15 (6): 540–59
Abbatecola AM, Maggi S, Paolisso G. New approaches to treating type 2 diabetes mellitus in the elderly: role of incretin therapies. Drugs Aging 2008; 25 (11): 913–25
Rajagopalan R, Xu Y, Abbadessa M. The effect of pioglitazone on glycemic and lipid parameters and adverse events in elderly patients with type 2 diabetes mellitus: a post hoc analysis of four randomized trials. Am J Geriatr Pharmacother 2006 Jun; 4 (2): 123–33
Amori RE, Lau J, Pittas AG. Efficacy and safety of incretin therapy in type 2 diabetes: systematic review and meta-analysis. JAMA 2007 Jul 11; 298 (2): 194–206
Phung OJ, Scholle JM, Talwar M, et al. Effect of noninsulin antidiabetic drugs added to metformin therapy on glycemic control, weight gain, and hypoglycemia in type 2 diabetes. JAMA 2010 Apr 14; 303 (14): 1410–8
Moon YS, Kashyap ML. Pharmacologic treatment of type 2 diabetic dyslipidemia. Pharmacotherapy 2004 Dec; 24 (12): 1692–713
National Cholesterol Education Program Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Third report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation 2002 Dec 17; 106 (25): 3143–421
Grundy SM, Cleeman JI, Rifkind BM, et al. Cholesterol lowering in the elderly population. Coordinating Committee of the National Cholesterol Education Program. Arch Intern Med 1999 Aug 9–23; 159 (15): 1670–8
Jacobson TA. Overcoming ‘ageism’ bias in the treatment of hypercholesterolaemia: a review of safety issues with statins in the elderly. Drug Saf 2006; 29 (5): 421–48
Thompson PD, Clarkson P, Karas RH. Statin-associated myopathy. JAMA 2003 Apr 2; 289 (13): 1681–90
Parra JL, Reddy KR. Hepatotoxicity of hypolipidemic drugs. Clin Liver Dis 2003 May; 7 (2): 415–33
Shepherd J. Fibrates and statins in the treatment of hyperlipidaemia: an appraisal of their efficacy and safety. Eur Heart J 1995 Jan; 16 (1): 5–13
US Food and Drug Administration. FDA Drug Safety Communication: new restrictions, contraindications, and dose limitations for Zocor (simvastatin) to reduce the risk of muscle injury [online]. Available from URL: http://www.fda.gov/Drugs/DrugSafety/ucm256581.htm [Accessed 2011 Jul 19]
Scandinavian Simvastatin Survival Study Group. Randomised trial of cholesterol lowering in 4444 patients with coronary heart disease: the Scandinavian Simvastatin Survival Study (4S). Lancet 1994 Nov 19; 344 (8934): 1383–9
The Long-Term Intervention with Pravastatin in Ischaemic Disease (LIPID) Study Group. Prevention of cardiovascular events and death with pravastatin in patients with coronary heart disease and a broad range of initial cholesterol levels. N Engl J Med 1998 Nov 5; 339 (19): 1349–57
Downs JR, Clearfield M, Weis S, et al. Primary prevention of acute coronary events with lovastatin in men and women with average cholesterol levels: results of AFCAPS/Tex CAPS. Air Force/Texas Coronary Atherosclerosis Prevention Study. JAMA 1998 May 27; 279 (20): 1615–22
Sacks FM, Pfeffer MA, Moye LA, et al., Cholesterol and Recurrent Events Trial Investigators. The effect of pravastatin on coronary events after myocardial infarction in patients with average cholesterol levels. N Engl J Med 1996 Oct 3; 335 (14): 1001–9
Shepherd J, Cobbe SM, Ford I, et al., West of Scotland Coronary Prevention Study Group. Prevention of coronary heart disease with pravastatin in men with hypercholesterolemia. N Engl J Med 1995 Nov 16; 333 (20): 1301–7
US Food and Drug Administration. FDA Drug Safety Communication: Important safety label changes to cholesterol-lowering statin drugs [online]. Available from URL: http://www.fda.gov/Drugs/DrugSafety/ucm293101.htm [Accessed 2012 Mar 9]
Elam MB, Hunninghake DB, Davis KB, et al. Effect of niacin on lipid and lipoprotein levels and glycemic control in patients with diabetes and peripheral arterial disease: the ADMIT study: a randomized trial. Arterial Disease Multiple Intervention Trial. JAMA 2000 Sep 13; 284 (10): 1263–70
Kane MP, Hamilton RA, Addesse E, et al. Cholesterol and glycemic effects of Niaspan in patients with type 2 diabetes. Pharmacotherapy 2001 Dec; 21 (12): 1473–8
Grundy SM, Vega GL, McGovern ME, et al. Efficacy, safety, and tolerability of once-daily niacin for the treatment of dyslipidemia associated with type 2 diabetes: results of the assessment of diabetes control and evaluation of the efficacy of niaspan trial. Arch Intern Med 2002 Jul 22; 162 (14): 1568–76
Yamakawa T, Takano T, Tanaka S, et al. Influence of pitavastatin on glucose tolerance in patients with type 2 diabetes mellitus. J Atheroscler Thromb 2008 Oct; 15 (5): 269–75
Waters DD, Ho JE, DeMicco DA, et al. Predictors of new-onset diabetes in patients treated with atorvastatin: results from 3 large randomized clinical trials. J Am Coll Cardiol 2011 Apr 5; 57 (14): 1535–45
Sabatine MS, Wiviott SD, Morrow DA, et al. High-dose atorvastatin associated with worse glycemic control: a PROVE-IT TIMI 22 substudy [abstract]. Circulation 2004; 110 (17 Suppl. 1): S834
Bays HE, Goldberg RB. The ‘forgotten’ bile acid sequestrants: is now a good time to remember? Am J Ther 2007 Nov–Dec; 14 (6): 567–80
Tricor® (fenofibrate) tablets: US prescribing information. North Chicago (IL): Abbott Laboratories, 2010
Lopid® (gemfibrozil tablets, USP): US prescribing information. New York (NY): Pfizer, Inc., 2010
Garg A, Grundy SM. Cholestyramine therapy for dyslipidemia in non-insulin-dependent diabetes mellitus: a short-term, double-blind, crossover trial. Ann Intern Med 1994 Sep 15; 121 (6): 416–22
Lipid Research Clinics Program. The Lipid Research Clinics Coronary Primary Prevention Trial results: I. Reduction in incidence of coronary heart disease. JAMA 1984 Jan 20; 251 (3): 351–64
Fonseca VA, Rosenstock J, Wang AC, et al. Colesevelam HCl improves glycemic control and reduces LDL cholesterol in patients with inadequately controlled type 2 diabetes on sulfonylurea-based therapy. Diabetes Care 2008 Aug; 31 (8): 1479–84
Goldberg RB, Fonseca VA, Truitt KE, et al. Efficacy and safety of colesevelam in patients with type 2 diabetes mellitus and inadequate glycemic control receiving insulin-based therapy. Arch Intern Med 2008 Jul 28; 168 (14): 1531–40
Bays HE, Goldberg RB, Truitt KE, et al. Colesevelam hydrochloride therapy in patients with type 2 diabetes mellitus treated with metformin: glucose and lipid effects. Arch Intern Med 2008 Oct 13; 168 (18): 1975–83
Jialal I, Abby SL, Misir S, et al. Concomitant reduction in low-density lipoprotein cholesterol and glycated hemoglobin with colesevelam hydrochloride in patients with type 2 diabetes: a pooled analysis. Metab Syndr Relat Disord 2009 Jun; 7 (3): 255–8
Jones MR, Rosenstock J, Abby SL, et al. Colesevelam HCl in type 2 diabetes reduces A1C and LDL-C consistently across age, gender, and race. J Clin Lipidol 2008 June; 2 (3): 229–30
Davidson MH, Toth P, Weiss S, et al. Low-dose combination therapy with colesevelam hydrochloride and lovastatin effectively decreases low-density lipoprotein cholesterol in patients with primary hypercholesterolemia. Clin Cardiol 2001 Jun; 24 (6): 467–74
Knapp HH, Schrott H, Ma P, et al. Efficacy and safety of combination simvastatin and colesevelam in patients with primary hypercholesterolemia. Am J Med 2001 Apr 1; 110 (5): 352–60
Hunninghake D, Insull Jr W, Toth P, et al. Coadministration of colesevelam hydrochloride with atorvastatin lowers LDL cholesterol additively. Atherosclerosis 2001 Oct; 158 (2): 407–16
Ginsberg DA, Phillips SE, Wallace J, et al. Evaluating and managing constipation in the elderly. Urol Nurs 2007 Jun; 27 (3): 191–200, 12
Miller M, Stone NJ, Ballantyne C, et al. Triglycerides and cardiovascular disease: a scientific statement from the American Heart Association. Circulation 2011 May 24; 123 (20): 2292–333
Acknowledgements
The editorial assistance provided by Mary Hines, Anna Mett and Lucy Whitehouse of inScience Communications was funded by Daiichi Sankyo, Inc. Joel C. Marrs declares no potential conflicts of interest, and did not receive funding for writing this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Marrs, J.C. Glucose and Low-Density Lipoprotein Cholesterol Lowering in Elderly Patients with Type 2 Diabetes. Drugs Aging 29, e1–e12 (2012). https://doi.org/10.2165/11599290-000000000-00000
Published:
Issue Date:
DOI: https://doi.org/10.2165/11599290-000000000-00000