Abstract
Background: Use of the ergot-derived dopamine receptor agonists (cabergoline and pergolide) is associated with an increased risk of cardiac valvulopathy. Pergolide was withdrawn from the US market in 2007 because of the risk of valvular heart disease, while the European Medicines Agency (EMA) required a reduction in the maximum daily dosage of cabergoline and pergolide from 6mg/day to 3 mg/day in 2008. In Japan, the package inserts of both drugs were revised in April 2007 to request that physicians conduct periodic ultrasonic cardiography (UCG) examinations for patients taking cabergoline or pergolide. Also, through face-to-face communication with medical representatives of drug companies, physicians were informed that use of cabergoline and pergolide has increased the risk of valvulopathy. However, cabergoline and pergolide have remained in wide use, even following the regulatory actions.
Objective: The objective of this study was to assess the impact of actions, including the package insert revision in April 2007, to encourage periodic UCG.
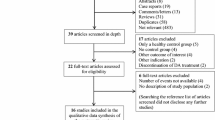
Methods: Data on monthly claims (January 2005-October 2008) covering 330 000 patients were obtained from a Japanese database vendor. We selected patients ≥40 years of age with Parkinson’s disease. The impact of the regulatory action on the proportion of patients with Parkinson’s disease prescribed cabergoline or pergolide was assessed by segmented regression analysis and by a statistical model of the rates of UCG examination in patients taking/ not taking cabergoline or pergolide before and after the action. We also compared the use of cabergoline and pergolide before and after the action with that of other antiparkinson drugs.
Results: Of 574 patients with Parkinson’s disease, the proportion of patients prescribed cabergoline or pergolide did not decrease but rather tended to increase after the action when analysed by segmented regression analysis (p = 0.13). Similarly, the proportion of the prevalent and incident users of cabergoline or pergolide did not change between two 19-month periods before and after the action. The adjusted rates of UCG examination per personyear before and after the action were both 0.02 in those not prescribed cabergoline or pergolide, but 0.02 before the action and 0.09 after the action in those taking either drug. The excess UCG examination rate of cabergoline or pergolide attributable to the action was 0.08 per person-year (95% CI 0.03, 0.11). While 1 of 49 (2%) patients taking cabergoline or pergolide had a UCG up to 19 months before the action, 9 of 36 (25%) patients taking cabergoline or pergolide had a UCG up to 19 months after the action. Annual sales from 2004 to 2008 were 195, 195, 170, 110 and 75 billion yen, respectively, and the number of valvulopathy events, including incompetence of aortic/mitral/ tricuspid valves and cardiac valve disease, per annual sales from 2004 to 2008 were estimated at 0.23, 0.03, 0.08, 0.25 and 0.19 per billion yen, respectively.
Conclusions: Following the actions in April 2007, no decrease in the use of cabergoline or pergolide occurred, although more patients administered the drug underwent a UCG. However, those undergoing a UCG represented onequarter of the total number prescribed cabergoline or pergolide. To mitigate the risk, additional risk management tools such as patient registration may be needed to secure careful clinical examination (including UCG examination, if necessary) for cardiac function.




Similar content being viewed by others
References
Muangpaisan W, Hori H, Brayne C. Systematic review of the prevalence and incidence of parkinson’s disease in Asia. J Epidemiol 2009; 19: 281–93
von Campenhausen S, Bornschein B, Wick R, et al. Prevalence and incidence of parkinson’s disease in Europe. Eur Neuropsychopharmacol 2005; 15: 473–90
Morikawa F, Tashiro K, Itoh K, et al. Prevalence of parkinson’s disease in Hokkaido, the northernmost island of Japan. Intern Med 1996; 35: 276–9
MHLW. Statistics of specific diseases [in Japanese; online]. Available from URL: http://www.mhlw.go.jp/toukei/saikin/hw/eisei/08/dl/data_007.pdf [Accessed 2010 Jun 26]
Olanow CW, Watts RL, Koller WC. An algorithm (decision tree) for the management of parkinson’s disease (2001): treatment guideline. Neurology 2001; 56: 1–88
Horstink M, Tolosa E, Bonuccelli U, et al. Review of the therapeutic management of parkinson’s disease. Report of a joint task force of the European Federation of Neurological Societies and the Movement Disorder Society-European Section. Part I: early (uncomplicated) parkinson’s disease. Eur J Neurol 2006; 13: 1170–85
Pritchett AM, Morrison JF, Edwards WD, et al. Valvular heart disease in patients taking pergolide. Mayo Clin Proc 2002; 77: 1280–6
Zanettini R, Antonini A, Gatto G, et al. Valvular heart disease and the use of dopamine agonists for parkinson’s disease. N Engl J Med 2007; 356: 39–46
Corvol JC, Anzouan-Kacou JB, Fauveau E, et al. Heart valve regurgitation, pergolide use, and parkinson disease. Arch Neurol 2007; 64: 1721–6
Yamamoto M, Uesugi T, Nakayama T. Dopamine agonists and cardiac valvulopathy in parkinson disease: a casecontrol study. Neurology 2006; 67: 1225–9
Yamashiro K, Komine-Kobayashi M, Hatano T, et al. The frequency of cardiac valvular regurgitation in Parkinson’s disease. Mov Disord 2008; 23: 935–41
Schade R, Andersohn F, Suissa S, et al. Dopamine agonists and the risk of cardiac-valve regurgitation. N Engl J Med 2007; 356: 29–38
Bhattacharyya S, Schapira AH, Mikhailidis DP, et al. Drug-induced fibrotic valvular heart disease. Lancet 2009; 374: 577–85
Millan MJ, Maiofiss L, Cussac D, et al. Differential actions of antiparkinson agents at multiple classes of monoamin-ergic receptor: I. A multivariate analysis of the binding profiles of 14 drugs at 21 native and cloned human receptor subtypes. J Pharmacol Exp Ther 2002; 303: 791–804
Jähnichen S, Horowski R, Pertz HH. Agonism at 5-HT2B receptors is not a class effect of the ergolines. Eur J Pharmacol 2005; 513: 225–8
US FDA. Withdrawal of parkinson’s treatment: pergolide [online]. Available from URL: http://www.fda.gov/ForConsumers/ConsumerUpdates/ucm048819.htm [Accessed 2010 Jun 26]
EMEA. Questions and answers on the review of ergotderived dopamine agonists [online]. Available from URL: http://www.ema.europa.eu/docs/en_GB/document_library/Referrals_document/Ergot_derived_dopamine_agonists_31/WC500011445.pdf [Accessed 2011 Jan 12]
PMDA. Revision of label [in Japanese; online]. Available from URL: http://www.info.pmda.go.jp/kaitei/kaitei20070419.html#1 [Accessed 2010 Jun 26]
Anonymous. Yakuji handbook 2006 [in Japanese]. Tokyo: Jiho, 2006
Anonymous. Yakuji handbook 2010 [in Japanese]. Tokyo: Jiho, 2010
Kimura S, Sato T, Ikeda S, et al. Development of a database of health insurance claims: standardization of disease classifications and anonymous record linkage. J Epidemiol 2010; 20: 413–9
Wagner AK, Soumerai SB, Zhang F, et al. Segmented regression analysis of interrupted time series studies in medication use research. J Clin Pharm Ther 2002; 27: 299–309
PMDA. On the data of spontaneous reports [in Japanese; online]. Available from URL: http://www.info.pmda.go.jp/fsearchnew/jsp/menu_fukusayou_base.jsp [Accessed 2010 Jun 26]
Smalley W, Shatin D, Wysowski DK, et al. Contraindicated use of cisapride: impact of Food and Drug Administration regulatory action. JAMA 2000; 284: 3036–9
Guo JJ, Curkendall S, Jones JK, et al. Impact of cisapride label changes on codispensing of contraindicated medications. Pharmacoepidemiol Drug Saf 2003; 12: 295–301
Lung B, Gohlke-Bärwolf C, Tornos P, et al. Recommendations on the management of the asymptomatic patient with valvular heart disease. Eur Heart J 2002; 23: 1253–66
Kim JY, Chung EJ, Park SW, et al. Valvular heart disease in parkinson’s disease treated with ergot derivative dopamine agonists. Mov Disord 2006; 213: 1261–4
Waller EA, Kaplan J, Heckman MG. Valvular heart disease in patients taking pergolide. Mayo Clin Proc 2005; 80: 1016–20
Hazell L, Shakir SAW. Under-reporting of adverse drug reactions. Drug Saf 2006; 29: 385–96
Zanettini R, Antonini A, Gatto G, et al. Regression of cardiac valvulopathy related to ergot-derived dopamine agonists. Cardiovasc Ther. Epub 2010 Jun 11
Acknowledgements
No sources of funding were used to prepare this manuscript or conduct this study. The authors have no conflicts of interest to declare that are directly relevant to the content of this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ooba, N., Yamaguchi, T. & Kubota, K. The Impact in Japan of Regulatory Action on Prescribing of Dopamine Receptor Agonists. Drug-Safety 34, 329–338 (2011). https://doi.org/10.2165/11588230-000000000-00000
Published:
Issue Date:
DOI: https://doi.org/10.2165/11588230-000000000-00000