Abstract
Study objectives
To compare the efficacy and safety of oral azithromycin 500mg once daily for 3 days with those of oral clarithromycin 500mg twice daily for 10 days.
Design
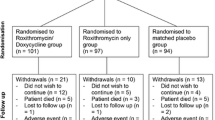
Randomized, double-blind, double-dummy, multicenter study.
Setting
Seventy-six study centers in eight countries (Argentina, Brazil, Canada, Chile, Costa Rica, India, South Africa, and USA).
Patients
Three hundred and twenty-two adult outpatients with acute exacerbation of chronic bronchitis (AECB) as documented by increased cough or sputum production, worsening dyspnea, and purulent sputum production.
Interventions
Randomization 1: 1 to azithromycin 500mg once daily for 3 days or clarithromycin 500mg twice daily for 10 days.
Results
The primary efficacy endpoint was clinical response at day 21–24, or test of cure (TOC) visit in the modified intent-to-treat (MITT) analysis (n = 318 patients). The TOC clinical cure rates in the MITT population were equivalent in the two treatment groups at 85% with azithromycin and 82% with clarithromycin (95% CI–5.9%, 12.0%). Clinical success rates on day 10–12 were also equivalent at 93% with azithromycin and 94% with clarithromycin (95% CI–7.9%, 4.4%). Clinical cure rates at TOC by pathogen were equivalent for the two treatment groups for Haemophilus influenzae (azithromycin, 85.7%; clarithromycin, 87.5%), Moraxella catarrhalis (91.7% and 80.0%, respectively) and Streptococcus pneumoniae (90.6% and 77.8%, respectively). Bacteriologic success rates were also equivalent between the azithromycin and clarithromycin treatment groups at TOC for S. pneumoniae (90.6% and 85.2%, respectively), H. influenzae (71.4% and 81.3%, respectively) and M. catarrhalis (100% and 86.7%, respectively). The overall incidence of treatment-related adverse events was similar in the azithromycin and clarithromycin groups (20.9% and 26.8%, respectively), with the most common being abdominal pain (6.3% and 6.1%, respectively), diarrhea (4.4% and 5.5%, respectively), and nausea (4.4% and 3.7%, respectively).
Conclusions
Three-day treatment with azithromycin 500mg once daily is equivalent to a 10-day treatment with clarithromycin 500mg twice daily in adult patients with AECB.










Similar content being viewed by others
References
Stoller JK. Acute exacerbations of chronic obstructive pulmonary disease. N Engl J Med 2002; 346: 988–94
Pauwels RA, Buist AS, Calverley PMA, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: NHLBI/WHO Global Initiative for Chronic Obstructive Lung Disease (GOLD) Workshop summary. Am J Respir Crit Care Med 2001; 163: 1256–76
Celli BR. Chronic obstructive pulmonary disease. In: Khan MG, Lynch JP, editors. Pulmonary disease diagnosis and therapy. Baltimore (MD): Williams and Wilkins, 1997: 199–236
World Health Organization. The World Health Report 1999: making a difference. Geneva: World Health Organization, 1999; 1: 2
Deaths/mortality US 1998. Hyattsville (MD): National Center for Health Statistics, 1998
American Thoracic Society. Standards for the diagnosis and care of patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med 1995; 152 (5 Pt 2 Suppl.): 77–121
Balter MS, Hyland RH, Low D, et al. Recommendations on the management of chronic bronchitis: a practical guide for Canadian physicians. CMAJ 1994; 10 Suppl.: 5–23
Ball P. Epidemiology and treatment of chronic bronchitis and its exacerbations. Chest 1995; 108(2 Suppl.): 43S–52S
Saint S, Bent S, Vittinghoff E, et al. Antibiotics in chronic obstructive pulmonary disease exacerbations: a meta-analysis. JAMA 1995; 273: 957–60
Anthonisen N, Manfreda J, Warren C, et al. Antibiotic therapy in exacerbations of chronic obstructive pulmonary disease. Ann Intern Med 1987; 106: 196–204
Gotfried MH. Diagnosis and management of acute exacerbation of chronic bronchitis. Hosp Med 1997; 33 Suppl.: 2–4
Sethi S, Evans N, Grant BJ, et al. New strains of bacteria and exacerbations of chronic obstructive pulmonary disease. N Engl J Med 2002; 347: 465–71
Reynolds HY. Chronic bronchitis and acute infectious exacerbations. In: Mandell GL, Bennett JE, Dollin R, editors. X: principles and practices of infectious diseases. 4th ed. New York: Churchill Livingstone, 1995: 608–12
Niederman MS. Antibiotic therapy of exacerbations of chronic bronchitis. Semin Respir Infect 2000; 15: 59–70
Doern GV, Jones RN, Pfaller MA, et al. Haemophilus influenzae and Moraxella catarrhalis from patients with community-acquired respiratory tract infections: antimicrobial susceptibility patterns from the SENTRY Antimicrobial Surveillance Program (United States and Canada, 1997). Antimicrob Agents Chemother 1999; 43: 385–9
Thornsberry C, Oigilvue PT, Holley Jr HP, et al. Survey of susceptibilities of Haemophilus influenzae and Moraxella catarrhalis isolates to 26 antimicrobial agents: a prospective U.S. study. Antimicrob Agents Chemother 1999; 43: 2612–23
Amsden GW, Nafziger AN, Foulds G. Pharmacokinetics in serum and leukocyte exposures of oral azithromycin, 1500 milligrams, given over a 3- or 5-day period in healthy subjects. Antimicrob Agents Chemother 1999; 43: 163–5
Myberg J, Nagel GJ, Petschel E. The efficacy and tolerance of a three-day course of azithromycin in the treatment of community-acquired pneumonia. J Antimicrob Chemother 1993; 31Suppl. E: 163–9
McPhee SJ, Schroeder SA. General approach to the patient. In: Tierney LM, McPhee SJ, Papadakis MA, editors. Current medical diagnosis & treatment. 36th ed. Stamford (CT): Appleton Publishers, 1997: 1–2
Woods GL, Washington JA. The clinician and the microbiology laboratory. In: Mandell GL, Douglas Jr RG, Bennett JE, editors. Principles and practice of infectious diseases. 4th ed. New York: Churchill Livingstone, 1995: 169–99
National Committee for Clinical Laboratory Standards. Methods for dilution antimicrobial disk susceptibility tests. 5th ed; approved standard. NCCLS Document M2-A5, 1993, 13(24)
National Committee for Clinical Laboratory Standards. Performance standards for antimicrobial disk susceptibility tests. 5th ed; approved standard. NCCLS Document M2-A5, 1993, 13(24)
Amsden GW, Baird IM, Simon S, et al. Efficacy and safety of azithromycin versus levofloxacin in the outpatient treatment of acute bacterial exacerbations of chronic bronchitis. Chest 2003; 123(3): 772–7
DeAbate CA, Mathew CP, Warner JH, et al. The safety and efficacy of short course (5-day) moxifloxacin vs azithromycin in the treatment of patients with acute exacerbation of chronic bronchitis. Respir Med 2000; 94: 1029–37
Sclar DA, Tartaglione TA, Fine MJ. Overview of issues related to medical compliance with implications for the outpatient management of infectious diseases. Infect Agents Dis 1994; 3: 266–73
Grossman RF. The value of antibiotics and the outcomes of antibiotic therapy in exacerbations of COPD. Chest 1998; 113(4 Suppl.): 249S–55S
Doern GV, Brueggemann A, Holley HP, et al. Antimicrobial resistance of Streptococcus pneumoniae recovered from outpatients in the United States during the winter months of 1994 and 1995: results of a 30-center national surveillance study. Antimicrob Agents Chemother 1996; 40: 1208–13
Acknowledgment
This study was supported by Pfizer Inc. Drs Swanson and Dunne are both employees of the sponsor, Pfizer Inc. Drs Lainez-Ventosilla and De Salvo have both been Pfizer investigators and received research monies from Pfizer Inc. Dr Amsden is a consultant, researcher and speaker for Pfizer Inc. and Pliva dd and is/has conducted antimicrobial research for Abbott, Bayer, Bristol-Myers Squibb, and GlaxoSmithKline.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Swanson, R.N., Lainez-Ventosilla, A., De Salvo, M.C. et al. Once-Daily Azithromycin for 3 Days Compared with Clarithromycin for 10 Days for Acute Exacerbation of Chronic Bronchitis. Treat Respir Med 4, 31–39 (2005). https://doi.org/10.2165/00151829-200504010-00004
Published:
Issue Date:
DOI: https://doi.org/10.2165/00151829-200504010-00004