Abstract
Context: The US FDA has issued an advisory warning of a possible link between antidepressant treatment for paediatric patients with major depressive disorder (MDD) and an increased risk of suicidal behaviour. A large database of paid health insurance claims for adolescents with MDD provided the opportunity to examine this possible relationship.
Objective: To examine the potential empirical link between antidepressant treatment and suicide attempts among adolescents aged 12–18 years using a community sample of managed care enrollees across the US.
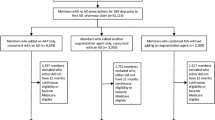
Design: A retrospective longitudinal cohort using paid insurance claims for all healthcare and prescription fills for adolescents who were newly diagnosed with MDD and had at least 6 months of follow-up data. A multivariate Cox proportional hazards regression analysis was used to test the hypothesis that antidepressant use increased the risk of suicide attempt, adjusting for propensity for allocation to each treatment group and for demographic and clinical characteristics.
Setting: Managed care plans including both commercial and Medicaid plans in the east, midwest, south and western regions of the US from January 1997 to March 2003.
Participants: All adolescent insurance members aged 12–18 years at first diagnosis of MDD.
Main outcome measures: Suicide attempts as indicated by medical utilisation with International Classification of Diseases (9th edition) [ICD-9] or 10th edition (ICD-10) codes in any healthcare setting or by any covered provider.
Results: 24 119 adolescents met inclusion criteria (63% female). Crude suicide attempt rates ranged from 0.0-2.3% by index treatment group. Treatment with SSRIs (hazard ratio) [HR] = 1.59; CI 0.89, 2.82), other antidepressants (HR = 1.03; CI 0.43, 2.44), or multiple antidepressants (HR = 1.43; CI 0.70, 2.89) after index MDD diagnosis resulted in no statistically increased risk of suicide attempt. Treatment with antidepressant medication for at least 180 days (6 months) reduced the likelihood of suicide attempt compared with antidepressant treatment for <55 days (8 weeks) [HR = 0.34; CI 0.21, 0.55]. Other variables that were independently associated with greater risk of suicide attempts included female gender, severity of illness indicators, younger age at time of MDD diagnosis, and living in the midwest or west.
Conclusions: Antidepressant medication use had no statistically significant effect on the likelihood of suicide attempt in a large cohort of adolescents across the US after propensity adjustment for treatment allocation and controlling for other factors. The relationship between suicidal behaviour and antidepressant medication use is complex and requires further investigation.






Similar content being viewed by others
References
Mitka M. FDA alert on antidepressants for youth. JAMA 2003; 290(19): 2534
Abbott A. British panel bans use of antidepressant to treat children. Nature 2003; 423: 792
Food and Drug Administration. FDA public health advisory: suicidality in children and adolescents being treated with anti-depressant medications [online]. 2004 Oct15. Available from URL: http://www.fda.gov/cder/drug/antidepressants/SS-RIPHA200410.htm [Accessed 2004 Oct 29]
Kessler RC, Berglund P, Dernier O, et al. The epidemiology of major depressive disorder: results from the national comorbidity survey replication (NCS-R). JAMA 2003; 289(23): 3095–105
Birmaher B, Ryan ND, Williamson D, et al. Childhood and adolescent depression: a review of the past 10 years. Part I. J Am Acad Child Adolesc Psychiatry 1996; 35(11): 1427–39
Birmaher B, Arbelaez C, Brent D. Course and outcome of child and adolescent major depressive disorder. Child Adolesc Psychiatr Clin N Am 2002; 11(3): 619–37
Voelker R. Researchers probe depression in children. JAMA 2003; 289(23): 3078–9
Weissman M, Wolk S, Wickramaratne P, et al. Children with prepubertal-onset major depressive disorder and anxiety grown up. Arch Gen Psychiatry. 1999; 56: 794–801
Weissman M, Wolk S, Goldstein R, et al. Depressed adolescents grown up. JAMA 1999; 281: 1707–13
Berndt E, Koran L, Finkelstein S, et al. Lost human capital from early-onset chronic depression. Am J Psychiatry 2000; 157: 940–7
Birmaher B, Brent DA, Benson RS. Practice parameters for the assessment and treatment of children and adolescents with depressive disorders. J Am Acad Child Adolesc Psychiatry 1998; 37(10): 63S–83S
Emslie G, Rush A, Weinberg W, et al. A double-blind, randomized, placebo-controlled trial of fluoxetine in children and adolescents with depression. Arch Gen Psychiatry 1997; 54: 1031–7
Wagner KD, Ambrosini P, Rynn M, et al. Efficacy of sertraline in the treatment of children and adolescents with major depressive disorder: two randomized clinical Trials. JAMA 2003; 290(8): 1033–93
Emslie G, Heiligenstein J, Wagner K, et al. Fluoxetine for acute treatment of depression in children and adolescents: a placebo-controlled, randomized clinical trial. J Am Acad Child Adolesc Psychiatry 2002; 41: 1205–15
Keller M, Ryan N, Strober M, et al. Efficacy of paroxetine in the treatment of adolescent major depression: a randomized, controlled trial. J Am Acad Child Adolesc Psychiatry 2001; 40: 762–72
Varley C. Psychopharmocological treatment of major depressive disorder in children and adolescents. JAMA 2003; 290(8): 1091–3
Brent D, Birmaher B. British warning on SSRIs questioned. J Am Acad Child Adolesc Psychiatry 2004; 43(4): 379–80
Hazell P, O’Connell D, Heathcote D, et al. Efficacy of tricyclic drugs in treating child and adolescent depression: a meta-analysis. BMJ 1995; 310: 897–901
Shireman T, Olson BM, Dewan NA. Patterns of antidepressant use among children and adolescents. Psychiatr Serv (Chic) 2002; 53(11): 1444–50
McCombs JS, Nichol MB, Stimmel GL, et al. The cost of antidepressant drug therapy failure: a study of antidepressant use patterns in a Medicaid population. J Clin Psychiatry 1990; 51 Suppl.: 60–9
McCombs JS, Nichol MB, Stimmel GL. The role of SSRI antidepressants for treating depressed patients in the California Medicaid (Medi-Cal) program. Value Health 1999; 2(4): 269–80
Hoagwood K, Burns BJ, Kiser L, et al. Evidence-based practice in child and adolescent mental health services. Psychiatr Serv (Chic) 2001; 52(9): 1179–89
New Freedom Commission on Mental Health. Achieving the promise: transforming mental health care in America. Final report. Rockville, MD: DHHS; 2003. Pub. No. SMA-03-3832
Horesh N, Orbach I, Gothelf D, et al. Comparison of the suicidal behavior of adolescent inpatients with borderline personality disorder and major depression. J Nerv Ment Dis 2003; 191(9): 582–8
Zametkin AJ, Atler MR, Yemeni T. Suicide in teenagers: assessment, management, and prevention. JAMA 2001; 286(24): 3120–5
Keith CR. Adolescent suicide. JAMA 2001; 286(24): 3126–7
Anderson R. Deaths: leading causes for 2000. National Vital Statistics Report. 2002; 50: 1–85
Hall WD, Mant A, Mitchell PB, et al. Association between antidepressant prescribing and suicide in Australia, 1991–2000: trend analysis. BMJ 2003; 326: 1–5
Olfson M, Shaffer D, Marcus SC, et al. Relationship between antidepressant medication treatment and suicide in adolescents. Arch Gen Psychiatry 2003; 60: 978–82
Jick H, Kaye J, Jick S. Antidepressants and the risk of suicidal behaviors. JAMA 2004; 292(3): 338–43
Russell M, Taylor D, Cummins G, et al. Use of managed care claims data in the risk assessment of venous thromboembolism in outpatients. Am J Manag Care 2002; 8(1 Suppl.): S3–9
Valuck R. Treatment of depression with citalopram, fluoxetine, paroxetine, sertraline, and venlafaxine in managed care. Part 1: drug selection, dosing, and utilization. Drug Benefit Trends 2002; 14(7): 23–30
Valuck R. Treatment of depression with citalopram, fluoxetine, paroxetine, sertraline, and venlafaxine in managed care. Part 2: patient comorbidities and coprescribed therapies. Drug Benefit Trends 2002; 14(8): 33–40
World Health Organization. ICD-9: international statistical classification of diseases and relation health problems. 9th rev. Geneva: World Health Organization, 1978
World Health Organization. ICD-10: international statistical classification of diseases and relation health problems. 10th rev. Geneva: World Health Organization, 1994
O’Carroll PW, Potter LB. Suicide contagion and the reporting of suicide: recommendations from a national workshop. Morb Mortal Wkly Rep 1994; 43(RR-6): 9–18
American Psychiatric Association. Diagnostic and statistical manual of mental disorders (DSM-IV). 4th ed. Washington, DC: American Psychiatric Association, 1994
Martin A, Van Hoof T, Stubbe D, et al. Multiple psychotropic pharmacotherapy among child and adolescent enrollees in Connecticut Medicaid managed care. Psychiatric Services 2003; 54(1): 72–7
Malone D, Billups S, Valuck R, et al. Development of a chronic disease indicator score using a Veterans Affairs Medical Center medication database. J Clin Epidemiol 1999; 52: 551–7
Valuck R, Williams S, MacArthur M, et al. A retrospective cohort study of correlates of response to pharmacologic therapy for hyperlipidemia in members of a managed care organization. Clin Ther 2003; 25: 2936–57
Rey M, Schulz P, Costa C, et al. Guidelines for the dosage of neuroleptics: I. Chloropromazine equivalents of orally administered neuroleptics. Int Clin Psychiatry 1989; 4: 95–104
Rijcken C, Monster T, Brouwers J, et al. Chlorpromazine equivalents versus defined daily doses: how to compare anti-psychotic drug doses? J Clin Psychopharmacology 2003; 23(6): 657–9
Foley K. The treatment of cancer pain. N Engl J Med 1985; 313(2): 84–95
Asburn M, Lipman A. Management of pain in the cancer patient. Anesth Analg 1994; 79(3): 612–4
Steiner J, Prochazka A. The assessment of refill compliance using pharmacy records: methods, validity, and applications. J Clin Epidemiol 1997; 50: 105–16
Current Procedural Terminology. 4th ed. Chicago (IL): American Medical Association, 2000
Wang J, Donnan P. Propensity score methods in drug safety studies: practice, strengths, and limitations. Pharmacoepidemiol Drug Saf 2001; 10: 341–4
Cox DR. Regression models and life tables. J R Stat Soc 1972; 34: 187–202
Crown W, Treglia M, Meneades L, et al. Long-term costs of treatment for depression: impact of drug selection and guideline adherence. Value Health 2001; 4(4): 295–307
SAS Language [computer program]. Version 8.1. Cary (NC): SAS Institute, 2000
Wong I, Besag F, Santosh P, et al. Use of selective serotonin reuptake inhibitors in children and adolescents. Drug Saf 2004; 27(13): 991–1000
Cook TD, Campbell DT. Quasi-experimentation: design and analysis issues for field settings. Chicago (IL): Rand McNally, 1979
Vorstman J, Lahuis B, Buitelaar JK. SSRIs associated with behavioral activation and suicidal ideation. J Am Acad Child Adolesc Psychiatry 2001; 40(12): 1364–5
American Psychiatric Association, et al. Practice guideline for the treatment of patients with major depressive disorder (revision). Am J Psychiatry 2000; 157(4): 1–45
Goldstein B, Goodnick P. Selective serotonin reuptake inhibitors in the treatment of affective disorders: III. Tolerability, safety and pharmacoeconomics. J Psychopharmacol 1998; 12Suppl. B: S57A
Aguglia E, Casacchia M, Cassano G, et al. Double-blind study of the efficacy and safety of sertraline versus fluoxetine in major depression. Int Clin Psychopharmacol 1993; 8(3): 197–202
Montgomery SA, Huusom AK. Escitalopram is at least as effective as venlafaxine XR in the treatment of depression and is better tolerated [poster]. 15th Congress of the European College of Neuropsychopharmacology; 2002 Oct 5–9; Barcelona
Bielski R, Ventura D, Chang C. A double-blind comparison of escitalopram with venlafaxine XR in the treatment of major depressive disorder [poster]. 16th Congress of the European College of Neuropsychopharmacology; 2003 Sep 20–24; Prague
Valuck R. Selective serotonin reuptake inhibitors: a class review. Pharmacy and Therapeutics. 2004; 29(4): 234–43
Schlesselman J. Sample size requirements in cohort and case-control studies of disease. Am J Epidemiol 1974; 99: 381–4
Spettell C, Wall T, Allison J, et al. Identifying physician-recognized depression from administrative data: consequences for quality measurement. Health Serv Res 2003; 38(4): 1081–102
Rost K, Smith R, Matthews D, et al. The deliberate misdiagnosis of major depression in primary care. Arch Fam Med 1994; 3(4): 333–7
Hirschfeld R, Keller M, Panico S, et al. The National Depressive and Manic-Depressive Association consensus statement on the undertreatment of depression. JAMA 1997; 277(4): 333–40
Lemelin J, Hotz S, Swensen R, et al. Depression in primary care: why do we miss the diagnosis? Can Fam Physician 1994; 40: 104–8
Acknowledgements
The research presented in this manuscript was unfunded and investigator-initiated. Dr Valuck has received other research funding and served as an advisor to Forest Laboratories, Pfizer and Janssen. Dr Libby was supported by William T. Grant Foundation Scholars Award; Dr Sills was supported by Health Resources and Services Administration Faculty Development in Primary Care Fellowship D14HP00153.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Valuck, R.J., Libby, A.M., Sills, M.R. et al. Antidepressant Treatment and Risk of Suicide Attempt by Adolescents with Major Depressive Disorder. CNS Drugs 18, 1119–1132 (2004). https://doi.org/10.2165/00023210-200418150-00006
Published:
Issue Date:
DOI: https://doi.org/10.2165/00023210-200418150-00006