Abstract
For years, osteoporosis and cardiovascular disease were thought to be two independent consequences of aging; however, mounting evidence supports an association between these diseases. Recently, a widespread class of cholesterol-lowering drugs known as statins have demonstrated (in rodents and cell cultures) the ability to induce bone formation. This finding is significant since current therapies are limited to the prevention or slowing down of bone loss rather than (enhancing/improving) bone formation. In humans, the ability of statins to generate new bone has not been consistent; however, several investigations have demonstrated a dramatic decrease in fracture risk. Although it has been proposed that statins induce new bone via increased bone morphogenetic protein-2, other conditions affected by statins such as dyslipidaemia, vascular calcification, endothelial dysfunction and impaired nitric oxide expression, may also contribute to the cardiovascular and bone health paradigm. Furthermore, the role of physical activity and its influence on cardiovascular and bone health, especially in postmenopausal women, may contribute to the discrepancy of findings in human data. In summary, it remains to be determined if statins contribute to bone health via improvements in vascular health or by pleiotropic properties unique to their pharmacology. This review provides information on our current understanding of the bone and cardiovascular association, as well as on novel areas of research to further our current understanding of these conditions.










Similar content being viewed by others
References
Celermajer DS, Sorensen KE, Gooch VM, et al. Non-invasive detection of endothelial dysfunction in children and adults at risk of atherosclerosis. Lancet 1992; 340(8828): 1111–5
O’Driscoll G, Green D, Taylor RR. Simvastatin an HMG-coenzyme A reductase inhibitor, improves endothelial function within 1 month. Circulation 1997; 95(5): 1126–31
Wilson SH, Simari R, Best P, et al. Simvastatin preserves coronary endothelial function in hypercholesterolemia in the absence of lipid lowering. Arteriocler Thromb Vasc Biol 2001; 21: 122–8
Anderson T, Elstein E, Haber H, et al. Comparative study of ACE-inhibition, angiotensin II antagonism, and calcium channel blockade on flow-mediated vasodilation in patients with coronary disease (BANFF study). J Am Coll Cardiol 2000; 35(1): 67–70
Mancini G, Henry G, Macaya C, et al. Angiotensin-converting enzyme inhibition with quinapril improves endothelial vasomotor dysfunction in patients with coronary artery disease: the TREND (Trial on Reversing ENdothelial Dysfuncton) study. Circulation 1996; 94(3): 258–65
Hornig B, Arakawa N, Haussmann D, et al. Differential effects of quinaprilat and enalaprilat on endothelial function of conduit arteries in patients with chronic heart failure. Circulation 1998; 98(25): 2842–8
Celermajer D, Sorenson K, Spiegelhalter D, et al. Aging is associated with endothelial dysfunction in healthy men years before the age-related decline in women. J Am Coll Cardiol 1994; 24(2): 471–6
Clarkson P, Montgomery H, Mullen M, et al. Exercise training enhances endothelial function in young men. J Am Coll Cardiol 1999; 33(5): 1379–85
Takemoto M, Liao JK. Pleiotropic effects of 3-hydroxy-3-methylglutaryl coenzyme A reductase inhibitors. Arterioscler Thromb Vasc Biol 2001; 21(11): 1712–9
Scandinavian Simvastatin Survival Study Group. Randomised trial of cholesterol lowering in 4444 patients with coronary heart disease: The Scandinavian Simvastatin Survival Study (4S). Lancet 1994; 344(19): 1383–9
Shepherd J, Cobbe SM, Ford I, et al. Prevention of coronary heart disease with pravastatin in men with hypercholesterolemia. N Engl J Med 1995; 333(20): 1301–7
Sacks FM, Pfefferr MA, Move LA, et al. The effect of pravastatin on coronary events after myocardial infarction in patients with average cholesterol levels. N Engl J Med 1996; 335(14): 1001–9
LIPID Study Group. Prevention of cardiovascular events and death with pravastatin in patients with coronary heart disease and a broad range of initial cholesterol levels. N Engl J Med 1998; 339(19): 1349–57
Downs J, Clearfield M, Weis S, et al. Primary prevention of acute coronary events with lovastatin in men and women with average cholesterol levels: results of AFCAPS/TexCAPS. JAMA 1998; 279(20): 1615–22
Expert Panel on Detection Evaluation and Treatment of High Blood Cholesterol in Adults. Executive Summary of the Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). JAMA 2001; 285(19): 2486–97
Kannel WB, Castelli WP, Gordon T, et al. Serum cholesterol, lipoproteins and the risk of coronary heart disease: the Framingham Study. Ann Intern Med 1971; 74(1): 1–12
Pitt B, Waters D, Brown WV, et al. Aggressive lipid-lowering therapy compared with angioplasty in stable coronary artery disease. N Engl J Med 1999; 341(2): 70–6
Packard CJ. Influence of pravastatin and plasma lipids on clinical events in the West of Scotland Coronary Prevention Study (WOSCOPS). Circulation 1998; 97(15): 1440–5
Massy ZA, Keane WF, Kasiske BL. Inhibition of the mevalonate pathway: benefits beyond cholesterol reduction? Lancet 1996; 347(8994): 102–3
Panza J, Cannon III R. Endothelium, nitric oxide, and atherosclerosis: from basic mechanisms to clinical implications. 1st ed. Armonk (NY): Futura Publishing Company Inc., 1999
Vita J, Treasure C, Nabel E, et al. Coronary vasomotor response to acetylcholine relates to risk factors for coronary artery disease. Circulation 1990; 81(2): 491–7
Zeiher A, Drexler H, Saurbier B, et al. Endothelium-mediated coronary blood flow modulation in humans: effects of age, atherosclerosis, hypercholesterolemia, and hypertension. J Clin Investig 1993; 92(2): 652–62
Cooke JP, Tsao P. Is NO an endogenous antiatherogenic molecule? Arteriocler Thromb 1994; 14(5): 653–5
Gibbons G, Dzau V. The emerging concept of vascular remodeling. N Engl J Med 1994; 330(20): 1431–8
Adams M, Jessup W, Hailstones D, et al. L-Arginine reduces monocyte adhesion to vascular endothelium and endothelial expression of cell adhesion molecules. Circulation 1997; 95(3): 662–8
Wang PS, Solomon DH, Mogun H, et al. HMG-CoA reductase inhibitors and the risk of hip fractures in elderly patients. JAMA 2000; 283(24): 3211–6
Sugiyama M, Kodama T, Konishi K, et al. Compactin and simvastatin, but not pravastatin, induce bone morphogenetic protein-2 in human osteosarcoma cells. Biochem Biophys Res Commun 2000; 271(3): 688–92
Oxlund H, Dalstra M, Andreassen TT. Statin given perorally to adult rats increases cancellous bone mass and compressive strength. Calcif Tissue Int 2001; 69(5): 299–304
Ohnaka K, Shimoda S, Nawata J, et al. Pitavastatin enhanced BMP-2 and osteocalcin expression by inhibition of Rho-associated kinase in human osteoblasts. Biochem Biophys Res Commun 2001; 287(2): 337–42
Mundy G, Garrett R, Harris S, et al. Stimulation of bone formation in vitro and in rodents by statins. Science 1999; 286(5446): 1946–55
Meier CR, Schlienger RG, Kraenzlin ME, et al. HMG-CoA reductase inhibitors and the risk of fractures. JAMA 2000; 283(24): 3205–10
Maritz FJ, Conradie MM, Hulley PA, et al. Effect of statins on bone mineral density and bone histomorphometry in rodents. Arterioscler Thromb Vasc Biol 2001; 21(10): 1636–41
Maeda T, Matsunuma A, Kawane T, et al. Simvastatin promotes osteoblast differentiation and mineralization in MC3T3-E1 cells. Biochem Biophys Res Commun 2001; 280(3): 874–7
Edwards C, Hart D, Spector T. Oral statins and increased bone-mineral density in postmenopausal women. Lancet 2000; 355(9222): 2218–9
Chung Y-S, Lee M-D, Lee S-K, et al. HMG-CoA reductase inhibitors increase BMD in type 2 diabetes mellitus patients. J Clin Endocrinol Metab 2000; 85(3): 1137–42
Chan KA, Andrade SE, Boles M, et al. Inhibitors of hydroxymethylglutaryl-coenzyme A reductase and risk of fracture among older women. Lancet 2000; 355(9222): 2185–8
Bjarnason N, Riis B, Christiansen C. The effect of fluvastatin on parameters of bone remodeling. Osteoporos Int 2001; 12(5): 380–4
Watanabe S, Fukumoto S, Takeuchi Y, et al. Effects of 1-year treatment with fluvastatin or pravastatin on bone. Am J Med 2001; 110(7): 584–7
Woo J-T, Kasai S, Stern P, et al. Compactin suppresses bone resorption by inhibiting the fusion of prefusion osteoclasts and disrupting the actin ring in osteoclasts. J Bone Miner Res 2000; 15(4): 650–62
Chan M, Mak T, Chiu R, et al. Simvastatin increases serum osteocalcin concentration in patients treated for hypercholesterolaemia. J Clin Endocrinol Metab 2001; 86(9): 4556–9
Reid IR, Hague W, Emberson J, et al. Effect of pravastatin on frequency of fracture in the LIPID study: secondary analyses of a randomised controlled trial. Lancet 2001; 337(9255): 509–12
Pasco J, Kotowicz M, Henry M, et al. Statin use, bone mineral density, and fracture risk. Arch Intern Med 2002; 162(5): 537–40
Sirola J, Honkanen R, Kroger H, et al. Relation of statin use and bone loss: a prospective population-based cohort study in early postmenopausal women. Osteoporos Int 2002; 13(7): 537–41
Stein E, Farnier M, Waldstreicher J, et al. Effects of statins on biomarkers of bone metabolism: a randomised trial. Nutr Metab Cardiovasc Dis 2001; 11(2): 84–7
Looker A, Bauer D, Chesnut III C, et al. Clinical use of biochemical markers of bone remodeling: current status and future directions. Osteoporos Int 2000; 11(6): 467–80
van Staa T-P, Wegman S, de Vries F, et al. Use of statins and risk of fractures. JAMA 2001; 285(14): 1850–5
Safeer R, Lacivita C. Choosing drug therapy for patients with hyperlipidemia. Am Fam Physician 2000; 61(11): 3371–82
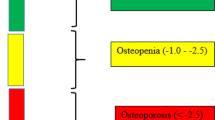
Marcus R, Feldman D, Kelsey J. Osteoporosis. San Diego (CA): Academic Press, 1996
Callister TQ, Raggi P, Cooil B, et al. Effect of HMG-CoA reductase inhibitors on coronary artery disease as assessed by electron-beam computed tomography. N Engl J Med 1998; 339(27): 1972–8
Parhami F, Morrow A, Balucan J, et al. Lipid oxidation products have opposite effects on calcifying vascular cell and bone cell differentiation: a possible explanation for the paradox of arterial calcification in osteoporotic patients. Arterioscler Thromb Vasc Biol 1997; 17(4): 680–7
Parhami F, Jackson S, Tintut Y, et al. Atherogenic diet and minimally oxidized low density lipoprotein inhibit osteogenic and promote adipogenic differentiation of marrow stromal cells. J Bone Miner Res 1999; 14(12): 2067–78
Parhami F, Tintut Y, Beamer W, et al. Atherogenic high-fat diet reduces bone mineralization in mice. J Bone Miner Res 2001; 16(1): 182–8
Aoyagi K, Ross P, Orloff J, et al. Low bone density is not associated with aortic calcification. Calcif Tissue Int 2001; 69(1): 20–4
Vogt M, Valentin R, Forrest K, et al. Bone mineral density and aortic calcification: the Study of Osteoporotic Fractures. J Am Geriatr Soc 1997; 45(2): 140–5
Yamaguchi T, Sugimoto T, Yano S, et al. Plasma lipids and osteoporosis in postmenopausal women. Endocr J 2002; 49(2): 211–7
Uyama O, Yoshimoto Y, Yamamoto Y, et al. Bone changes and carotid atherosclerosis in postmenopausal women. Stroke 1997; 28(9): 1730–2
Barengolts E, Berman M, Kukreja S, et al. Osteoporosis and coronary atherosclerosis in asymptomatic postmenopausal women. Calcif Tissue Int 1998; 62(3): 209–13
Browner W, Seeley D. Non-trauma mortality in elderly women with low bone mineral density. Lancet 1991; 338(8763): 355–8
Vogt M, Cauley J, Kuller L, et al. Bone mineral density and blood flow to the lower extremities: the study of osteoporotic fractures. J Bone Miner Res 1997; 12(2): 283–9
von der Recke P, Hansen M, Hassager C. The association between low bone mass at the menopause and cardiovascular mortality. Am J Med 1999; 106(3): 273–8
Hak A, Pols H, van Hemert A, et al. Progression of aortic calcification is associated with metacarpal bone loss during menopause: a population-based longitudinal study. Arterioscler Thromb Vasc Biol 2000; 20(8): 1926–31
Kado D, Browner W, Blackwell T, et al. Rate of bone loss is associated with mortality in older women: a prospective study. J Bone Miner Res 2000; 15(10): 1974–80
Kiel D, Kauppila L, Cupples L, et al. Bone loss and the progression of abdominal aortic calcification over a 25 year period: the Framingham Heart Study. Calcif Tissue Int 2001; 68(5): 271–6
Helfrich M, Evans D, Grabowski P, et al. Expression of nitric oxide synthase isoforms in bone and bone cell cultures. J Bone Miner Res 1997; 12(7): 1108–15
Fox S, Chow J. Nitric oxide and synthase expression in bone cells. Bone 1998; 23(1): 1–6
Klein-Nulend J, Helfrich M, Sterck J, et al. Nitric oxide response to shear stress by human bone cell cultures is endothelial nitric oxide synthase dependent. Biochem Biophys Res Commun 1998; 250(1): 108–14
Mancini L, Moradi-Bidhendi N, Becherini L, et al. The biphasic effects of nitric oxide in primary rat osteoblasts are cGMP dependent. Biochem Biophys Res Commun 2000; 274(2): 477–81
MacIntyre I, Zaidi M, Alam A, et al. Osteoclastic inhibition: an action of nitric oxide not mediated by cyclic GMP. Proc Natl Acad Sci U S A 1991; 88(7): 2936–40
Holliday L, Dean A, Lin R, et al. Low NO concentrations inhibito osteoclast formation in mouse marrow cultures by cGMP-dependent mechanism. Am J Physiol 1997; 272 (3 Pt 2): F283–91
Wimalawansa S, De Marco G, Gangula P, et al. Nitric oxide donor alleviates ovariectomy-induced bone loss. Bone 1996; 18(4): 301–4
Turner C, Owan I, Jacob D, et al. Effects of nitric oxide synthase inhibitors on bone formation in rats. Bone 1997; 26(6): 487–90
Jamal S, Browner W, Bauer D, et al. Intermittent use of nitrates increases bone mineral density: the study of osteoporotic fractures. J Bone Miner Res 1998; 13(11): 1755–9
Armour K, Van’t Hof R, Grabowski P, et al. Evidence for a pathogenic role of nitric oxide in inflammation-induced osteoporosis. J Bone Miner Res 1999; 14(12): 2137–42
MacPherson H, Noble B, Ralston S. Expression and functional role of nitric oxide synthase isoforms in human osteoblast-like cells. Bone 1999; 24(3): 179–85
Zaman G, Pitsillides A, Rawlinson S, et al. Mechanical strain stimulates nitric oxide production by rapid activation of endothelial nitric oxide synthase in osteocytes. J Bone Miner Res 1999; 14(7): 1123–31
McAllister T, Du T, Frangos J. Fluid shear stress stimulates prostaglandin and nitric oxide release in bone marrow-derived preosteoclast-like cells. Biochem Biophys Res Commun 2000; 270(2): 643–8
O’Shaughnessy M, Polak J, Afzal F, et al. Nitric oxide mediates 17β-estradiol-stimulated human and rodent osteoblast proliferation and differentiation. Biochem Biophys Res Commun 2000; 277(3): 604–10
Wimalawansa S. Restoration of ovariectomy-induced osteopenia by nitroglycerin. Calcif Tissue Int 2000; 66(1): 56–60
Aguirre J, Buttery L, O’Shaughnessy M, et al. Endothelial nitric oxide synthase gene-deficient mice demonstrate marked retardation in postnatal bone formation, reduced bone volume, and defects in osteoblast maturation and activity. Am J Pathol 2001; 158(1): 247–57
Armour K, Armour K, Gallagher M, et al. Defective bone formation and anabolic response to exogenous estrogen in mice with targeted disruption of endothelial nitric oxide synthase. Endocrinology 2001; 142(2): 760–6
Samuels A, Perry M, Gibson R, et al. Role of endothelial nitric oxide synthase in estrogen-induced osteogenesis. Bone 2001; 29(1): 24–9
Watanuki M, Sakai A, Sakata T, et al. Role of inducible nitric oxide synthase in skeletal adaptation to acute increases in mechanical loading. J Bone Miner Res 2002; 17(6): 1015–25
Riancho J, Salas E, Zarrabeitia M, et al. Expression and functional role of nitric oxide synthase in osteoblast-like cells. J Bone Miner Res 1995; 10(3): 439–46
Turner C, Takano Y, Owan I, et al. Nitric oxide inhibitor LNAME suppresses mechanically induced bone formation in rats. Am J Physiol 1996; 270 (4 Pt 1): E634–9
Fox S, Chambers T, Chow J. Nitric oxide is an early mediator of the increase in bone formation by mechanical stimulation. Am J Physiol 1996; 270 (6 Pt 1): E955–60
Kasten T, Collin-Osdoby P, Patel N, et al. Potentiation of osteoclast bone-resorption activity by inhibition of nitric oxide synthase. Proc Natl Acad Sci U S A 1994; 91(9): 3569–73
Rich G, Mudge G, Laffel G, et al. Cyclosporine A and prednisone-associated osteoporosis in heart transplant recipients. J Heart Lung Transplant 1992; 11(5): 950–8
Berguer D, Krieg M-A, Thiebaud D, et al. Osteoporosis in heart transplant recipients: a longitudinal study. Transplant Proc 1994; 26(5): 2649–51
Braith R, Howard C, Fricker F, et al. Glucocoritcoid-induced osteopenia in adolescent heart transplant recipients. J Heart Lung Transplant 2000; 19(9): 840–5
Ip J, Fuster V, Badimon L, et al. Syndromes of acelerated arterosclerosis: role of vascular injury and smooth muscle cell proliferation. J Am Coll Cardiol 1990; 15(7): 1667–87
Leidig-Bruckner G, Hosch S, Dodidou P, et al. Frequency and predictors of osteoporotic fractures after cardiac or liver transportation: a follow-up study. Lancet 2001; 357(9253): 342–7
Becker D, Chamberlain B, Swank R, et al. Relationship between corticosteroid exposure and plasma lipid levels in heart transplant recipients. Am J Med 1988; 85(5): 632–8
Stamler J, Vaughan D, Rudd M, et al. Frequency of hypercholesterolemia after cardiac transplantation. Am J Cardiol 1988; 62(17): 1268–72
Holvoet P, Van Cleemput J, Collen D, et al. Oxidized low density lipoprotein is a prognostic marker of transplant-associated coronary artery disease. Arterioscler Thromb Vasc Biol 2000; 20(3): 698–702
Holvoet P, Stassen J, Cleemput J, et al. Oxidized low density lipoproteins in patients with transplant-associated coronary artery disease. Arterioscler Thromb Vasc Biol 1998; 18(1): 100–7
Hinkleman L, Nieman D. The effects of a walking program on body composition and serum lipids and lipoproteins in overweight women. J Sports Med Phys Fitness 1993; 33(1): 49–58
Lokey E, Tran Z. Effects of exercise training on serum lipid and lipoprotein concentrations in women: a meta-analyses. Int J Sports Med 1989; 10(6): 424–9
Nieman D, Warren B, O’Donnell K, et al. Physical activity and serum lipids and lipoproteins in elderly women. J Am Geriatr Assoc 1993; 41(12): 1339–44
Leon A, Sanchez O. Response of blood lipids to exercise training alone or combined with dietary intervention. Med Sci Sports Exerc 2001; 33 (6 Suppl.): S502–15
King A, Haskell W, Taylor C, et al. Group- vs home-based exercise training in healthy older men and women: a community-based clinical trial. JAMA 1991; 266(11): 1535–42
Cauley J, Kriska A, LaPorte R, et al. A two year randomized exercise trial in older women: effects on HDL-cholesterol. Atherosclerosis 1987; 66(3): 247–58
Seip R, Moulin P, Cocke T, et al. Exercise training decreases plasma cholesterol ester transfer protein. Arterioscler Thromb 1993; 13(9): 1359–67
Lindheim S, Notelovitz M, Feldman E, et al. The independent effects of exercise and estrogen on lipids and lipoproteins in postmenopausal women. Obstet Gynecol 1994; 83(2): 167–72
King A, Haskell W, Young D, et al. Long-term effects of varying intensities and formats of physical activity on participation rates, fitness, and lipoproteins in men and women aged 50 to 65 years. Circulation 1995; 91(10): 2596–604
Motoyama M, Sunami Y, Kinoshita F, et al. The effects of long-term low intensity aerobic training and detraining on serum lipid and lipoprotein concentrations in elderly men and women. Eur J Appl Physiol 1995; 70(2): 126–31
Ready A, Drinkwater D, Ducas J, et al. Walking program reduces elevated cholesterol in women postmenopause. Can J Cardiol 1995; 11(10): 905–12
Ready A, Maimark B, Ducas J, et al. Influence of walking volume on health benefits in women post-menopause. Med Sci Sports Exerc 1996; 28(9): 1097–105
Binder E, Birge S, Kohrt W. Effects of endurance exercise and hormone replacement therapy on serum lipids in older women. J Am Geriatr Soc 1996; 4(3): 231–6
Fox A, Thompson J, Butterfield G, et al. Effects of diet and exercise on common cardiovascular disease risk factors in moderately obese older women. Am J Clin Nutr 1996; 63(2): 225–33
Heikkinen J, Kyllonen E, Kurttila-Matero E, et al. HRT and exercise: effects on bone density, muscle strength and lipid metabolism: a placebo controlled 2-year prospective trial on two estrogen-progestin regimens in healthy postmenopausal women. Maturitas 1997; 26(2): 139–49
Schuit A, Schouten E, Miles T, et al. The effect of six months training on weight, body fatness and serum lipids in apparently healthy elderly dutch men and women. Int J Obes Relat Metab Disord 1998; 22(9): 847–53
Grandjean P, Crouse S, O’Brien B, et al. The effects of menopausal status and exercise training on serum lipids and the activities of intravascular enzymes related to lipid transport. Metabolism 1998; 47(4): 337–83
Klebanoff R, Miller V, Fernhall B. Effects of exercise and estrogen therapy on lipid profiles of postmenopausal women. Med Sci Sports Exerc 1998; 30(7): 1028–34
Stefanick M, Mackey S, Sheehan M, et al. Effects of diet and exercise in men and postmenopausal women with low levels of HDL cholesterol and high levels of LDL cholesterol. N Engl J Med 1998; 339(1): 12–20
Sunami Y, Motoyama M, Kinoshita F, et al. Effects of low-intensity aerobic training on the high-density lipoprotein cholesterol concentration in healthy elderly subjects. Metabolism 1999; 48(8): 984–8
Kraus W, Houmard J, Duscha B, et al. Effects of the amount and intensity of exercise on plasma lipoproteins. N Engl J Med 2002; 347(19): 1483–92
American Heart Association. Heart and stroke statistical update. Dallas (TX): American Heart Association, 2002
Schrott H, Bittner V, Vittinghoff E, et al. Adherence to national cholesterol education program treatment goals in postmenopausal women with heart disease: The Heart and Estrogen/Progestin Replacement Study (HERS): the HERS Research Group. JAMA 1997; 277(16): 1281–6
Health United States. With socioeconomic status and health Chartbook. Hyattsville (MD): National Center for Health Statistics, 1998
Leung W, Lau C, Wong C. Beneficial effect of cholesterol-lowering therapy on coronary endothelium-dependent relaxation in hypercholesterolemia patients. Lancet 1993; 341(8859): 1496–500
Williams S, Cusco J, Roddy M, et al. Impaired nitric-oxide mediated vasodilation in patients with non-insulin-dependent diabetes mellitus. J Am Coll Cardiol 1996; 27(3): 567–74
Celermajer D, Sorensen K, Georgakopoulos D, et al. Cigarette smoking is associated with dose-related and potentially reversible impairment of endothelium-dependent dilation in healthy adults. Circulation 1993; 88 (5 Pt 1): 2149–55
Taddei S, Virdis A, Mattei P, et al. Hypertension causes premature aging of endothelial function in humans. Hypertension 1997; 29(3): 736–43
Gokce N, Vita J, Bader D, et al. Effect of exercise on upper and lower extremity endothelial function in patients with coronary artery disease. Am J Cardiol 2002; 90(2): 124–7
Hambrecht R, Wolf A, Gielen S, et al. Effects of exercise on coronary endothelial function in patients with coronary artery disease. N Engl J Med 2000; 342(7): 454–60
Hornig B, Maier V, Drexler H. Physical training improves endothelial function in patients with chronic heart failure. Circulation 1996; 93(2): 210–4
Maiorana A, O’Driscoll G, Cheetham C, et al. The effect of combined aerobic and resistance exercise training on vascular function in type 2 diabetes. J Am Coll Cardiol 2001; 38(3): 860–6
Stampfer M, Colditz G, Willett W, et al. Postmenopausal estrogen therapy and cardiovascular disease: ten-year follow-up from the Nurses’ Health Study. N Engl J Med 1991; 325(11): 756–62
Hashimoto M, Akishita M, Eto M, et al. Modulation of endothelium-dependent flow-mediated dilation of the brachial artery by sex and menstrual cycle. Circulation 1995; 92(12): 3431–5
McKechnie R, Rubenfire M, Mosca L. Association between self-reported physical activity and vascular reactivity in postmenopausal women. Atherosclerosis 2001; 159(2): 483–90
Taddei S, Galetta F, Agostino V, et al. Physical activity prevents age-related impairment in nitric oxide availability in elderly athletes. Circulation 2000; 101(25): 2896–901
Gielen S, Erbs S, Linke A, et al. Home-based versus hospital-based exercise programs in patients with coronary artery disease: effects on coronary vasomotion. Am Heart J 2003; 145(1): J1–7
Maiorana A, O’Driscoll G, Dembo L, et al. Effect of aerobic and resistant exercise training on vascular function in heart failure. Am J Physiol Heart Circ Physiol 2000; 279(4): H1999–2005
Katz S, Yuen J, Bijou R, et al. Training improves endothelium-dependent vasodilation in resistance vessels of patients with heart failure. J Appl Physiol 1997; 82(5): 1488–92
Hambrecht R, Fiehn E, Weigl C, et al. Regular physical exercise corrects endothelial dysfunction and improves exercise capacity in patients with chronic heart failure. Circulation 1998; 98(24): 2709–15
Bergholm R, Makimattila S, Valkonen M, et al. Intense physical training decreases circulating antioxidants and endothelium-dependent vasodilatation in vivo. Atherosclerosis 1999; 145(2): 341–9
Higashi Y, Sasaki S, Sasaki N, et al. Daily aerobic exercise improves reactive hyperemia in patients with essential hypertension. Hypertension 1999; 33 (1 Pt 2): 591–7
Higashi Y, Sasaki S, Kurisu S, et al. Regular aerobic exercise augments endothelium-dependent vascular relaxation in normotensive as well as hypertensive subjects: role of endothelium-derived nitric oxide. Circulation 1999; 100(11): 1194–202
Clarkson P, Montgomery H, Mullen M, et al. Exercise training enhances endothelial function in young men. J Am Coll Cardiol 1999; 33(5): 1379–85
DeSouza CA, Shapiro LF, Clevenger CM, et al. Regular aerobic exercise prevents and restores age-related declines in endothelium-dependent vasodilation in healthy men. Circulation 2000; 102(12): 1351–7
Lavrencic A, Salobir BG, Keber I. Physical training improves flow-mediated dilation in patients with the polymetabolic syndrome. Arterioscler Thromb Vasc Biol 2000; 20(2): 551–5
Brendle DC, Joseph LJ, Corrett MC, et al. Effects of exercise rehabilitation on endothelial reactivity in older patients with peripheral arterial disease. Am J Cardiol 2001; 87(3): 324–9
Linke A, Schoene N, Gielen S, et al. Endothelial dysfunction in patients with chronic heart failure: systemic effects of lower-limb exercise training. J Am Coll Cardio 2001; 37(2): 392–7
Maiorana A, O’Driscoll G, Cheetham C, et al. The effect of combined aerobic and resistance exercise training on vascular function in type 2 diabetes. J Am Coll Cardiol 2001; 38(3): 860–6
Fuchsjager-Mayrl G, Pleiner J, Wiesinger GF, et al. Exercise training improves vascular endothelial function in patients with type 1 diabetes. Diabetes Care 2002; 25(10): 1795–801
Schmidt A, Pleiner J, Bayerle-Eder M, et al. Regular physical exercise improves endothelial function in heart transplant recipients. Clin Transplant 2002; 16(2): 137–43
Green DJ, Walsh JH, Maiorana A, et al. Exercise-induced improvement in endothelial dysfunction is not mediated by changes in CV risk factors: pooled analysis of diverse patient populations. Am J Physiol Heart Circ Physiol 2003; 285(6): H2679–87
Goto C, Higash Y, Kimura M, et al. Effect of different intensities of exercise on endothelium-dependent vasodilation in humans: role of endothelium-dependent nitric oxide and oxidative stress. Circulation 2003; 108(5): 530–5
Walsh JH, Bilsborough W, Maiorana A, et al. Exercise training improves conduit vessel function in patients with coronary artery disease. J Appl Physiol 2003; 95(1): 20–5
Kobayashi N, Tsuruya Y, Iwasawa T, et al. Exercise training in patients with chronic heart failure improves endothelial function predominantly in the trained extremities. Circ J 2003; 67(6): 505–10
Edwards D, Schofield R, Lennon S, et al. Effect of exercise training on endothelial function in men with coronary artery disease. Am J Cardiol 2004; 93(5): 617–20
Vona M, Rossi A, Capodaglio P, et al. Impact of physical training and detraining on endothelium-dependent vasodilation in patients with recent acute myocardial infarction. Am Heart J 2004; 147(6): 1039–46
Maiorana A, O’Driscoll G, Dembo L, et al. Exercise training, vascular function, and functional capacity in middle-aged subjects. Med Sci Sport Exerc 2001; 33(12): 2022–8
Kubo S, Rector T, Bank A. Effects of cardiac transplantation on endothelium dependent dilation of the peripheral vasculature in congestive heart failure. Am J Cardiol 1993; 71(1): 88–93
Cavero P, Sudhir K, Galli F, et al. Effect of orthotopic cardiac transplantation on peripheral vascular function in congestive heart failure: influence of cyclosporine therapy. Am Heart J 1994; 127(6): 1581–7
Berkenboom G, Crasset V, Giot C, et al. Endothelial function of internal mammary artery in patients with coronary artery disease and in transplant recipients. Am Heart J 1998; 135(5): 488–94
Patel A, Kuvin J, DeNofrio D, et al. Peripheral vascular endothelial function correlates with exercise capacity in cardiac transplant recipients. Am J Cardiol 2003; 9(1): 897–9
Khan K, McKay H, Kannus P, et al. Physical activity and bone health. Champaign (IL): Human Kinetics, 2001
Bassey E, Ramsdale S. Increase in femoral bone density in young women following high-impact exercise. Osteoporos Int 1994; 4(2): 72–5
Heinonen A, Oja P, Kannus P, et al. Bone mineral density in female athletes representing sports with different loading characteristics of the skeleton. Bone 1995; 17(3): 197–203
Lohman T, Going S, Pamenter R, et al. Effects of resistance training on regional and total bone mineral density in premenopausal women: a randomized prospective study. J Bone Miner Res 1995; 10(7): 1015–24
Hatori M, Hasegawa A, Adachi H, et al. The effects of walking at the anaerobic threshold level on vertebral bone loss in postmenopausal women. Calcif Tissue Int 1993; 52(6): 411–4
Kohrt W, Ehsani A, Birge Jr S. Effects of exercise involving predominantly either joint-reaction or ground-reaction forces on bone mineral density in older women. J Bone Miner Res 1997; 12(8): 1253–61
Welsh L, Rutherford O. Hip bone mineral density is improved by high-impact aerobic exercise in postmenopausal women and men over 50 years. Eur J Appl Physiol Occup Physiol 1996; 74(6): 511–7
Smidt G, Lin S, O’Dwyer K, et al. The effect of high-intensity trunk exercise on bone mineral density of postmenopausal women. Spine 1992; 17(2): 280–5
Kerr D, Morton A, Dick I, et al. Exercise effects on bone mass in postmenopausal women are site-specific and load-dependent. J Bone Miner Res 1996; 11(2): 218–25
Berard A, Bravo G, Gauthier P. Meta-analysis of the effectiveness of physical activity for the prevention of bone loss in postmenopausal women. Osteoporos Int 1997; 7(4): 331–7
Kelley G. Exercise and regional bone mineral density in postmenopausal women. Am J Phys Med Rehabil 1998; 77(1): 76–87
Kelley G. Aerobic exercise and lumbar spine bone mineral density in postmenopausal women: a meta-analyses. J Am Geriatr Soc 1998; 46(2): 143–52
Wallace B, Cumming R. Systematic review of randomized trials of the effect of exercise on bone mass in pre- and postmenopausal women. Calcif Tissue Int 2000; 67(1): 10–8
Wolff I, van Croonenborg J, Kemper H, et al. The effect of exercise training programs on bone mass: a meta-analyses of published controlled trials in pre- and postmenopausal women. Osteoporos Int 1999; 9(1): 1–12
Bonaiuti D, Shea B, Iovine R, et al. Exercise for preventing and treating osteoporosis in postmenopausal women (Cochrane Review). Available in The Cochrane Library; issue 3, 2004. Chichester: John Wiley & Sons, 2004: CD000333
Beck T, Ruff C, Mourtada F, et al. Dual-energy X-ray absorptiometry derived structural geometry for stress fracture prediction in male US Marine Corps recruits. J Bone Miner Res 1996; 11(5): 645–53
Beck T, Looker A, Ruff C, et al. Structural trends in the aging femoral neck and proximal shaft: analysis of the third national health and nutrition examination survey dual-energy X-rays absorptiometry data. J Bone Miner Res 2000; 15(12): 2297–304
Beck T, Oreskovic T, Stone KL, et al. Structural adaptation to changing skeletal load in progression toward hip fragility: the Study of Osteoporotic Fractures. J Bone Miner Res 2001; 16(6): 1108–19
Adami S, Gatil D, Braga V, et al. Site-specific effects of strength training on bone structure and geometry of ultradistal radius in postmenopausal women. J Bone Miner Res 1999; 14(1): 120–4
Acknowledgements
The authors wish to acknowledge financial support from the Canada Foundation for Innovation, the BC Knowledge Development Fund, and the Michael Smith Foundation for Health Research. The authors have no conflicts of interest directly relevant to the content of this review.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Whitney, C., Warburton, D.E.R., Frohlich, J. et al. Are Cardiovascular Disease and Osteoporosis Directly Linked?. Sports Med 34, 779–807 (2004). https://doi.org/10.2165/00007256-200434120-00001
Published:
Issue Date:
DOI: https://doi.org/10.2165/00007256-200434120-00001