Summary
Abstract
Insulin glargine is a human insulin analogue prepared by recombinant DNA technology. Modification of the human insulin molecule at position A21 and at the C-terminus of the B-chain results in the formation of a stable compound that is soluble at pH 4.0, but forms amorphous microprecipitates in subcutaneous tissue from which small amounts of insulin glargine are gradually released. The plasma concentration versus time profile of insulin glargine is therefore relatively constant in relation to conventional human insulins, with no pronounced peak over 24 hours. This allows once-daily administration as basal therapy.
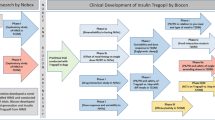
Early randomised trials with insulin glargine generally showed greater reductions in fasting blood or plasma glucose levels and a reduced frequency of nocturnal hypoglycaemia relative to neutral protamine Hagedorn (NPH) insulin in patients with type 1 diabetes mellitus. In addition to this basal therapy, patients continued to use the regular mealtime insulin regimen to which they were accustomed. More recent data with insulin glargine have included evidence of improved glycaemic control, with improvements in satisfaction with treatment over NPH insulin. Furthermore, the time of day at which insulin glargine is injected has no clinically relevant effect on glycaemic control in these patients. There are also data from small, nonblind studies to suggest comparable glycaemic control with insulin glargine and continuous subcutaneous insulin infusion.
Results from comparative studies and meta-analyses in individuals with type 2 diabetes show lower incidences of nocturnal hypoglycaemia with insulin glargine than with NPH insulin, with two studies showing a significantly greater improvement in glycosylated haemoglobin levels with insulin glargine than with NPH. Insulin glargine is well tolerated, and is not associated with greater immunogenicity or increases in bodyweight than NPH insulin. Long-term data show maintenance of glycaemic control with insulin glargine for up to 39 months in adults and children with type 1 and adults with type 2 diabetes.
In conclusion, insulin glargine is an effective and well tolerated basal insulin therapy when given as a single daily subcutaneous injection to patients with diabetes, with benefits in terms of glycaemic control and reduced frequency of hypoglycaemia over regimens based on conventional basal insulins. Accumulating data and official recommendations show the suitability of insulin glargine for first-line use in selected patients with type 2 diabetes who require insulin treatment, as well as in patients with type 1 disease, and confirm its use in children and adolescents.
Pharmacodynamic Properties
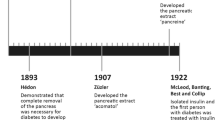
Insulin glargine is a long-acting recombinant human insulin analogue made by modifying human insulin using recombinant DNA technology. These changes at position 21 of the A-chain and at the C-terminus of the B-chain enable insulin glargine to remain soluble in the acidic environment of the vial, but form amorphous microprecipitates in the neutral pH of subcutaneous tissue after injection. Insulin glargine is slowly released from these microprecipitates to provide basal insulin supplementation over its once-daily dosage interval. Isoglycaemic and euglycaemic clamp studies in patients with diabetes mellitus and healthy volunteers have been conducted to evaluate the glucose-lowering effects of insulin glargine. Results show a time profile of pharmacodynamic activity characterised by a slower onset but longer duration of activity than neutral protamine Hagedorn (NPH) insulin. Unlike NPH or ultralente insulin, insulin glargine has no peak effect and has almost constant glucose-lowering activity lasting 24 hours.
In general, at clinically relevant concentrations, insulin receptor binding kinetics of insulin glargine are similar to those of regular human insulin, and blood glucose levels are lowered by stimulation of peripheral glucose uptake and inhibition of hepatic glucose production. Physiological and biochemical responses to hypoglycaemia induced by insulin glargine in patients with type 1 diabetes mellitus and healthy volunteers were similar to those induced by regular human insulin. Mitogenic effects of insulin are thought to be primarily mediated via the insulin-like growth factor-1 (IGF-1) receptor, and insulin glargine appears to have a generally higher affinity for the IGF-1 receptor than regular human insulin in vitro . However, the clinical relevance of this is probably limited since the affinity of insulin glargine for the IGF-1 receptor is <0.5% that of IGF-1 in human skeletal muscle cells. Moreover, in most cell types tested in vitro, mitogenic activity was similar between insulin glargine and regular human insulin.
Pharmacokinetic Properties
The rate of absorption of insulin glargine appears to provide a basal insulin level that remains constant for at least 24 hours. Following subcutaneous injection, the absorption of insulin glargine (containing zinc 15 or 80 μg/mL) was significantly slower than that of NPH insulin in healthy volunteers, in terms of the time to disappearance of 25% radioactivity (8.8 and 11.0 vs 3.2h; p < 0.0001). Importantly, in healthy volunteers, absorption of the drug was similar irrespective of the site (arm, leg or abdomen) of administration of insulin glargine containing zinc 30 μg/ mL (standard formulation).
No accumulation of insulin glargine occurred with daily subcutaneous injections in patients with type 1 diabetes. On days 1, 4 and 11, the maximum free serum insulin concentration (Cmax) ranged from 192–250 pmol/L, trough free serum insulin concentrations ranged from 77–86 pmol/L and the time to Cmax ranged from 2.8–4.1 hours. Steady-state insulin glargine concentrations are achieved 2–4 days after the first dose.
Insulin glargine is partially degraded in the subcutaneous tissues to two active metabolites. Both unchanged drug and metabolites are present in the plasma.
There is a lack of data concerning the pharmacokinetics of insulin glargine in special patient populations, including paediatric patients and those with renal or hepatic impairment.
Numerous drugs may affect glucose metabolism resulting in the need for adjustment of the insulin glargine dosage.
Therapeutic Efficacy
Type 1 diabetes: Six previously reviewed randomised trials, each involving more than 250 adults (aged 18–70 years) with type 1 diabetes, compared insulin glargine given once daily at bedtime with NPH insulin once or twice daily over 4–28 weeks. In all these studies patients continued to use the regular mealtime insulin regimen to which they were accustomed, and dosages of basal insulin (glargine or NPH) were based on fasting blood glucose (FBG) targets ranging from around 4–7 mmol/L. In these studies, patients receiving insulin glargine showed greater reductions in mean FBG levels at study endpoint than NPH insulin recipients, with significant (p < 0.05) reductions from baseline in insulin glargine groups (but not the NPH insulin group) in one of the trials. Mean glycosylated haemoglobin (HbA1c) levels were reduced to a similar extent with both insulin types in all 16- and 28-week trials. The incidence of symptomatic hypoglycaemia was greater (p < 0.05) with NPH than with insulin glargine in two 28-week studies. Percentages of patients reporting at least one episode of nocturnal hypoglycaemia were higher with NPH than with insulin glargine in most trials, and significantly (p < 0.05) higher in two.
Since the last review in Drugs, data have become available from several further randomised comparisons of insulin glargine with NPH insulin in patients with type 1 diabetes. Study durations ranged from 28 weeks to 1 year, and all findings are currently available as abstracts. One trial recruited 585 patients whereas the others randomised approximately 50–120 patients each. Findings were broadly similar to those of the earlier comparisons, although smaller studies showed statistically significantly greater improvements in glycaemic control as shown by FBG and/or HbA1c levels with insulin glargine than with NPH insulin. Frequencies of moderate or severe episodes of nocturnal hypoglycaemia were reduced with insulin glargine relative to NPH insulin in one trial and the other reported statistically significant reductions with insulin glargine in incidences of overall and nocturnal hypoglycaemia. Additional German data from 378 patients have shown no effect on glycaemic control of the timing of the daily injection of insulin glargine (breakfast, dinner or bedtime). Long-term findings demonstrate maintenance of glycaemic control, with minimal effects on bodyweight, with insulin glargine for up to 3 years in patients with type 1 diabetes.
A 28-week analysis in 517 patients has shown improved levels of satisfaction with treatment according to the Diabetes Treatment Satisfaction Questionnaire and Well-Being Questionnaire with insulin glargine relative to NPH insulin treatment. Preliminary 1-year results from a further study in 121 Italian patients support these findings. Basal therapy with insulin glargine has also been compared with continuous subcutaneous insulin infusion (CSII) in three small studies. Results are currently inconclusive, although one parallel-group comparison in 32 patients has shown insulin glargine therapy and CSII to offer equivalent glycaemic control together with reductions in frequency of hypoglycaemia relative to previously used conventional multiple-dose insulin regimens.
Randomised comparisons in children and adolescents (one large 28-week parallel-group study and one small crossover trial with 16-week treatment periods) have shown greater antihyperglycaemic efficacy of insulin glargine than NPH insulin in terms of FBG but not HbA1c levels, with less nocturnal hypoglycaemia with insulin glargine. Maintenance of glycaemic control for up to 3 years has been reported in a long-term extension study in 129 children and adolescents. Recent nonrandomised trials and noncomparative investigations in which series of patients were switched to treatment with insulin glargine show results broadly concordant with the randomised studies.
Type 2 diabetes: Previously reviewed studies, each in over 100 patients with type 2 diabetes, were of up to 1 year’s duration and showed similar improvements in glycaemic control with either insulin glargine or NPH insulin. Lower incidences of nocturnal hypoglycaemia were found in most trials with insulin glargine relative to NPH insulin (ranges of 10–31.3% vs 24–40.2%). Two further large, randomised trials that compared insulin glargine with NPH insulin (with concurrent oral antihyperglycaemic therapy) have shown statistically significant (p < 0.05 all comparisons) reductions in risk of nocturnal hypoglycaemia with insulin glargine therapy. One study has also demonstrated a statistically significantly (p < 0.01) greater decrease from baseline in mean HbA1c level with insulin glargine given at breakfast time (reduction of 1.24%) than with NPH insulin (0.84%). In another similarly designed trial, there were no differences in the mean reduction in HbA1c levels or in the incidence of nocturnal, all symptomatic or severe hypoglycaemia with morning versus evening administration of insulin glargine.
Notably, two large (n = 2304 and 1786) meta-analyses of phase III and IV clinical trials indicated that there was a significantly (p ≤ 0.01 all comparisons) lower risk of all confirmed symptomatic or nocturnal hypoglycaemia with insulin glargine when compared with NPH insulin treatment. Poisson regression analysis showed that when the incidence of confirmed symptomatic hypoglycaemia or confirmed nocturnal hypoglycaemia was made equivalent in the two treatment groups, there was a clinically relevant and statistically significant reduction in HbA1c with insulin glargine versus NPH insulin.
Patients with type 2 diabetes showed improved treatment satisfaction during a 1-year randomised, multicentre trial in both the insulin glargine and NPH insulin groups. At weeks 36, the improvement was greater in the insulin glargine group than in the NPH insulin group.
Long-term data from a multicentre, nonblind, extension study in 239 patients with type 2 diabetes who received insulin glargine in combination with oral antidiabetic agents showed that he mean HbA1c level was reduced from 9.44% at baseline to 8.42% over a period of up to 39 months. Only two severely symptomatic episodes of hypoglycaemia were reported during this period.
Significant (p < 0.05 all comparisons) reductions from baseline in mean HbA1c levels after starting insulin glargine treatment have also been reported in patients with type 2 diabetes in several nonrandomised studies and in a small (n = 20; 16 with type 2 diabetes) retrospective analysis of patients with end-stage renal disease.
Effect on bodyweight: Bodyweight gains were no greater with insulin glargine than with NPH insulin in comparative studies in patients with type 2 diabetes, with one previously reviewed trial showing less weight gain with insulin glargine and another showing similar increases with either type of insulin. Although more recently reported trials have not yet reported details of effects on bodyweight of randomised treatment, several prospective case series have shown no clinically relevant increases in mean bodyweight in patients with type 2 disease receiving insulin glargine for up to 9 months, despite significant improvements in glycaemic control relative to baseline. Data collected over up to 36 months in patients with type 1 diabetes receiving insulin glargine during long-term follow-up have shown a minimal increase in mean bodyweight with insulin glargine treatment.
Tolerability
The incidence of adverse events with insulin glargine has been generally similar to that with NPH insulin in randomised clinical studies. Injection site reactions, most of which are minor, are the most common adverse events with insulin glargine, and are seen in around 3–4% of patients. Observations in 239 patients with type 2 diabetes who participated in a recent long-term extension study revealed no injection site reactions with insulin glargine for up to 39 months.
Evidence to date shows that insulin glargine is no more immunogenic than NPH insulin, and there have been no clinically relevant increases in levels of antibodies to Escherichia coli reported in clinical trials. There have also been no indications of any increases in risk of progression of diabetic retinopathy related to the generally higher affinity of insulin glargine than regular human insulin for IGF-1 receptors. Recent data from patients with end-stage renal disease who received insulin glargine have shown no specific tolerability concerns, and animal studies have indicated no effect of insulin glargine on fetal or postnatal development, and no evidence of carcinogenicity linked to interaction with IGF-1 receptors.
Dosage and Administration
Once-daily, self-administered, subcutaneous injections of insulin glargine provide basal insulin levels for the treatment of adults or children (aged >6 years) with type 1 diabetes and adults with type 2 diabetes. Insulin glargine should not be diluted or mixed with any other insulin or solution as this could alter its time-action profile because of the acidic nature of its formulation.
The dosage of insulin glargine is determined individually for each patient and adjustments to dosage are made according to blood glucose levels. In clinical trials, insulin-naive patients were started with a dose of 10 IU once daily and were maintained at dosages ranging from 2–100 IU once daily. In patients receiving once-daily NPH or ultralente insulin, the initial dose of insulin glargine was usually matched in terms of the number of international units administered, whereas the initial dose was reduced by approximately 20% for the first week and then adjusted according to blood glucose levels in patients previously treated with twice-daily NPH insulin. Paediatric patients should be managed in the same way. The dosage and timing of additional short-acting insulin or oral antidiabetic agents may need to be adjusted with the initiation of insulin glargine.











Similar content being viewed by others

Notes
Use of tradename is for identification purposes only and does not imply endorsement.
References
International Diabetes Federation. Diabetes Prevalence [online]. Available from URL: http://www.idf.org [Accessed 2003 Apr 24]
American Diabetes Association. Basic diabetes information: facts and figures [online]. Available from URL: http://www.diabetes.org [Accessed 2003 Apr 24]
Mandrup-Poulsen T. Diabetes. BMJ 1998 Apr 18; 316: 1221–5
American Diabetes Association. Implications of the Diabetes Control and Complications Trial. Diabetes Care 2003; 26 Suppl. 1: S25–7
American Diabetes Association. Implications of the United Kingdom Prospective Diabetes Study. Diabetes Care 2003; 26 Suppl. 1: S28–32
National Institute for Clinical Excellence. Guidance on the use of long-acting insulin analogues for the treatment of diabetes: insulin glargine. Technology Appraisal Guidance 2002 Dec, No. 53
Vajo Z, Fawcett J, Duckworth WC. Recombinant DNA technology in the treatment of diabetes: insulin analogs. Endocr Rev 2001 Oct; 22(5): 706–17
McKeage K, Goa KL. Insulin glargine: a review of its therapeutic use as a long-acting agent for the management of type 1 and 2 diabetes mellitus. Drugs 2001; 61(11): 1599–624
Aventis Pharmaceuticals Inc. Lantus® (insulin glargine [rDNA origin] injection) prescribing information [online]. Available from URL: http://www.aventis.com [Accessed 2003 Apr 9]
Scholtz HE, van Niekerk N, Meyer BH, et al. An assessment of the variability in the pharmacodynamics (glucose lowering effect) of HOE901 compared to NPH and ultralente human insulins using the euglycaemic clamp technique [abstract no. 882]. Diabetologia 1999; 49 Suppl. 1: 999–1005
Ciaraldi TP, Carter L, Scipke G, et al. Effects of the long-acting insulin analog insulin glargine on cultured human skeletal muscle cells: comparisons to insulin and IGF-I. J Clin Endocrinol Metab 2001 Dec; 86(12): 5838–47
Berti L, Kellerer M, Bossenmaier B, et al. The long acting human insulin analog HOE 901: characteristics of insulin signalling in comparison to Asp(B10) and regular insulin. Horm Metab Res 1998; 30: 123–9
European Agency for the Evaluation of Medicinal Products. Insulin glargine: summary of product characteristics [online]. Available from URL: http://www.emea.eu.int [Accessed 2003 Apr 9]
Kurtzhalas P, Schaffer L, Sorensen A, et al. Correlations of receptor binding and metabolic and mitogenic potencies of insulin analogs designed for clinical use. Diabetes 2000; 49: 999–1005
Lepore M, Pampanelli S, Fanelli C, et al. Pharmacokinetics and pharmacodynamics of subcutaneous injection of long-acting human insulin analog glargine, NPH insulin, and ultralente human insulin and continuous subcutaneous infusion of insulin lispro. Diabetes 2000 Dec; 49: 2142–8
Soon PC, Matthews DR, Rosskamp R, et al. 24h profile of action of biosynthetic long-acting insulin (HOE901) tested in normal volunteers by glucose clamp methodology [abstract no. 0621]. Diabetes 1997; 46 Suppl. 1: 161A
Heinemann L, Linkeschova T, Rave K, et al. Time-action profile of the long-acting insulin analog insulin glargine (HOE901) in comparison with those of NPH insulin and placebo. Diabetes Care 2000 May; 23(5): 644–9
Fanelli CG, Pampanelli S, Porcellati F, et al. Pharmacodynamics of subcutaneous injection of insulin glargine after the first as compared to seventh day of its once daily administration in patients with T1 DM [abstract no. 802]. Diabetologia 2002 Aug; 45 Suppl. 2: A258
Meyer BH, Scholtz HE, Pretorius SG, et al. A comparison of the pharmacodynamics (glucose lowering effect) of intravenous HOE901 and regular insulin using the euglycaemic clamp technique [abstract no. PII-34]. Clin Pharmacol Ther 2000; 67(2): 123
Mudaliar S, Mohideen P, Deutsch R, et al. Intravenous glargine and regular insulin have similar effects on endogenous glucose output and peripheral activation/deactivation kinetic profiles. Diabetes Care 2002 Sep; 25(9): 1597–602
King AB, Armstrong D. A comparison of basal insulin delivery: continuous subcutaneous insulin infusion versus glargine [letter]. Diabetes Care 2003 Apr; 26(4): 1322
Dagogo-Jack S, Askari H, Lehner LL. Effect of glargine on glucose disposal and lipolysis in healthy and diabetic subjects [abstract no. 1737]. Diabetes 2000; 49 Suppl. 1: 213
Dagogo-Jack S, Askari H, Morrill B, et al. Physiological responses during hypoglycaemia induced by regular human insulin or a novel human analogue, insulin glargine. Diabetes, Obes Metab 2000; 2: 373–83
Sandow J, Scipke G. In vitro pharmacology studies with insulin glargine and human insulin: IGF-1 receptor binding and thymidine incorporation [abstract no. 1787-PO]. Diabetes 2001; 50 Suppl. 2: 429
Bähr M, Kolter T, Scipke G, et al. Growth promoting and metabolic activity of the human insulin analogue [GlyA21,ArgB31,ArgB32] insulin (HOE901) in muscle cells. Eur J Pharmacol 1997; 320: 259–65
Slawik M, Petersen KG. Effects of basal insulin treatment on IGF-I: glargine vs. NPH-insulin [abstract no. 1202-P]. Diabetes 2002; 51 Suppl. 2: A296
Stammberger I, Bube A, Durchfeld-Meyer B, et al. Evaluation of the carcinogenic potential of insulin glargine (LANTUS) in rats and mice. Int J Toxicol 2002 May-2002 30; 21(3): 171–9
Scipke G, Berchthold H, Geisen K, et al. HOE901: a new insulin with prolonged action [abstract]. Eur J Endocrinol 1995; 132 Suppl. 1: 25
Vehkavaara S, Yki-Järvinen H. 3.5 Years of insulin therapy with insulin glargine at bedtime markedly improves in vivo endothelial function in type 2 diabetes [abstract no. 699-P]. Diabetes 2002; 51 Suppl. 2: A173
Bolli GB, Owens DR. Insulin glargine. Lancet 2000; 356: 443–5
Hofmann T, Horstmann G, Stammberger I. Evaluation of the reproductive toxicity and embryotoxicity of insulin glargine (LANTUS) in rats and rabbits. Int J Toxicol 2002; 21(3): 181–9
Owens DR, Coates PA, Luzio SD, et al. Pharmacokinetics of 125I-labeled insulin glargine (HOE 901) in healthy men. Diabetes Care 2000 Jun; 23(6): 813–9
Gerich J, Bolli G, Becker R, et al. Fluctuation of serum insulin levels following single and multiple dosing of insulin glargine [abstract]. Proceedings of the 63rd Annual Scientific Sessions of the American Diabetes Association; 2003 Jun 13–17; New Orleans, Louisiana
Luzio SD, Owens D, Evans M, et al. Comparison of the sc absorption of HOE 901 and NPH human insulin type 2 diabetic subjects [abstract no. 0480]. Diabetes 1999 May; 48 Suppl. 1: A111
Heise T, Bott S, Rave K, et al. No evidence for accumulation of insulin glargine (LANTUS): a multiple injection study in patients with type 1 diabetes. Diabet Med 2002 Jun; 19(6): 490–5
Kuerzel GU, Shukla U, Scholtz HE, et al. Biotransformation of insulin glargine after subcutaneous injection in healthy subjects. Curr Med Res Opin 2003; 19(1): 34–40
Sandow J, Scipke G, Kuerzel GU, et al. Pharmacokinetics and metabolism of insulin glargine [abstract no. Pl-358]. 82nd Annual Meeting of the Endocrine Society; 2001 Jun 20–23; Denver, Colorado
American Diabetes Association. Standards of medical care for patients with diabetes mellitus. Diabetes Care 2003; 26 Suppl. 1: S33–50
Sacks DB, Brans DE, Goldstein DE, et al. Guidelines and recommendations for laboratory analysis in the diagnosis and management of diabetes mellitus. Clin Chem 2002; 48: 436–72
Schoenle E. Insulin glargine (HOE 901) lowers fasting blood glucose in children with type I diabetes mellitus without increasing the risk of hypoglycaemia [abstract no. 883]. HOE 901/3033 Study Group. Diabetologia 1999; 42 Suppl. 1: A235
Hershon K, Blevins T, Donley D, et al. Lower fasting blood glucose (FBG) and less symptomatic hypoglycemia with QD insulin glargine (Lantus) compared to BID NPH in subjects with type 1 diabetes [abstract no. 466-P]. Diabetes 2001; 50 Suppl. 2: 116–7
Pieber TR, Eugene-Jolchine I, Derobert E, et al. Efficacy and safety of HOE 901 versus NPH insulin in patients with type I diabetes mellitus. Diabetes Care 2000; 23: 157–62
Rosenstock J, Park G, Zimmerman J, et al. Basal insulin glargine (HOE 901) versus NPH insulin in patients with type 1 diabetes on multiple daily insulin regimens. Diabetes Care 2000; 23: 1137–42
Raskin P, Klaff L, Bergenstal R, et al. A 16-week comparison of the novel insulin analog insulin glargine (HOE 901) and NPH human insulin used with insulin lispro in patients with type 1 diabetes. Diabetes Care 2000; 23: 1666–71
Ratner RE, Hirsch IB, Neifing JL, et al. Less hypoglycemia with insulin glargine in intensive insulin therapy for type 1 diabetes. Diabetes Care 2000; 23: 639–43
Home P. A randomized, multicentre trial of insulin glargine versus NPH insulin in people with type 1 diabetes [abstract no. 800]. European Insulin Glargine Study Group. Diabetologia 2002 Aug; 45 Suppl. 2: A258
Standl E. Results of an international, multicentered, randomised 28-week study for the comparison of glargine insulin (HOE 901) and NPH insulin in the intensified treatment (ICT) of type 1 diabetes [abstract no. pFr107] [in German]. Exp Clin Endocrinol Diabetes 2000; 108 Suppl. 1: 159
Ashwell S, Amiel S, Bilous R, et al. Improvement in HbA1c with insulin glargine + insulin lispro in comparison with NPH insulin + unmodified human insulin in people with type 1 diabetes [abstract]. Proceedings of the 63rd Annual Scientific Sessions of the American Diabetes Association; 2003 Jun 13–17; New Orleans, Louisiana
Fulcher G, Yue D, Gilbert R, et al. Insulin glargine vs. NPH insulin in patients with type 1 diabetes: the effects of intensive insulin therapy on glycaemic control, hypoglycaemia and quality of life [abstract]. Diabetologia 2002 Aug; 45 Suppl. 2: A258
Porcellati F, Rossetti P, Fanelli CG, et al. Glargine vs NPH as basal insulin in intensive treatment of TIDM given lispro at meals: one year comparison [abstract no. 145]. Diabetologia 2002 Aug; 45 Suppl. 2: A51
Rossetti P, Costa E, Pampanelli S, et al. Intensive replacement of basal insulin in patients with type 1 diabetes given rapid-acting insulin analog at mealtime. Diabetes Care 2003; 26(5): 1490–6
Witthaus E, Stewart J, Bradley C. Treatment satisfaction and psychological well-being with insulin glargine compared with NPH in patients with type 1 diabetes. Diabet Med 2001 Aug; 18(8): 619–25
Bradley C. The Diabetes Treatment Satisfaction Questionnaire: DTSQ. Handbook of psychology and diabetes: a guide to psychological measurement in diabetes research and practice. Chur: Harwood Academic Publishers, 1994: 111–32
Bradley C. The Well-being Questionnaire. Handbook of psychology and diabetes: a guide to psychological measurement in diabetes research and practice. Chur: Harwood Academic Publishers, 1994: 89–109
Hamann A, Matthaei S, Rosak C, et al. A randomized clinical trial comparing breakfast, dinner, or bedtime administration of insulin glargine in patients with type 1 diabetes. Diabetes Care 2003; 26(6): 1738–44
Silvestre L, Bradley C, Witthaus E, et al. Improved treatment satisfaction and perceived metabolic control with insulin glargine, regardless of whether injected before breakfast, dinner or bedtime in patients with type 1 diabetes [abstract]. Proceedings of the 63rd Annual Scientific Sessions of the American Diabetes Association; 2003 Jun 13–17; New Orleans, Louisiana
Dreyer M. Glycemic control with insulin glargine in patients with type 1 diabetes is maintained in long-term exposure [abstract]. Diabetes 2002 Jun; 51 Suppl. 2: A129
Garg SK, Izuora KE, Hisatomi ME, et al. Impact of insulin glargine on glycemic control and severe hypoglycemie episodes in adults with type 1 diabetes [abstract no. 1936-PO]. Proceedings of the 63rd Annual Scientific Sessions of the American Diabetes Association; 2003 Jun 13–17; New Orleans, Louisiana
Kelly JL, Hirsch IB, Trence DL. Rapid decrease in clinically significant hypoglycemia with insulin glargine [abstract]. Diabetes 2002 Jun; 51 Suppl. 2: A123
Armstrong DU, King AB. Basal insulin: continuous glucose monitoring reveals less over-night hypoglycemia with continuous subcutaneous insulin infusion than with glargine [abstract]. Diabetes 2002 Jun; 51 Suppl. 2: A92
Wolpert HA, Porter SH. Partial basal replacement with glargine reduces ketosis after interruption of continuous subcutaneous insulin infusion [abstract no. 548-P]. Diabetes 2002 Jun; 51 Suppl. 2: A136
Lepore G, Dodesini AR, Nosari I, et al. Both continuous subcutaneous insulin infusion and a multiple daily insulin injection regimen with glargine as basal insulin are equally better than traditional multiple daily insulin injection treatment [letter]. Diabetes Care 2003 Apr; 26(4): 1321–2
Bode W, Hirsch IB, Hu P, et al. Type 1 diabetes patients can temporarily switch from continuous subcutaneous insulin infusion with insulin aspart to basal bolus therapy with insulin aspart and insulin glargine [abstract no. 438-P]. Proceedings of the 63rd Annual Scientific Sessions of the American Diabetes Association; 2003 Jun 13–17; New Orleans, Louisiana
Bode B, Schleusener D, Strange P, et al. Switch from continuous subcutaneous insulin (CSII) with insulin lispro [Humalog®] to multiple daily injections (MDI) with insulin glargine and insulin lispro [abstract]. Proceedings of the 63rd Annual Scientific Sessions of the American Diabetes Association; 2003 Jun 13–17; New Orleans, Louisiana
Schober E, Schoenle E, Van Dyk J, et al. Comparative trial between insulin glargine and NPH insulin in children and adolescents with type 1 diabetes mellitus. J Pediatr Endocrinol Metab 2002 Apr; 15(4): 369–76
Murphy NP, Keane SM, Ong KK, et al. Randomized cross-over trial of insulin glargine plus lispro or NPH insulin plus regular human insulin in adolescents with type 1 diabetes on intensive insulin regimens. Diabetes Care 2003 Mar; 26(3): 799–804
Dunger DB, Edge JA, Skvor J. Insulin glargine provides long-term effective glycemic control in children and adolescents with type 1 diabetes [abstract]. Diabetes 2002 Jun; 51 Suppl. 2: A426
Herwig J, Scholl-Schilling G, Böhles H. Experience with insulin glargine in children, juveniles, and adolescents with type 1 diabetes: a prospective study [abstract no. 8712]. Diabetologia 2002 Aug; 45 Suppl. 2: A281–2
Dixon BF, Chase HP, Fiallo-Scharer RH, et al. The addition of insulin glargine to lower hypoglycemic events and A1C levels in children and adolescents with type 1 diabetes [abstract no. 1736-P]. Proceedings of the 63rd Annual Scientific Sessions of the American Diabetes Association; 2003 Jun 13–17; New Orleans, Louisiana
Pearson J, Chase HP, Wightman C, et al. Reduction of severe hypoglycemic episodes in children and adolescents with type 1 diabetes using insulin-glargine therapy [abstract]. Diabetes 2002 Jun; 51 Suppl. 2: A425
Kordonouri O, Deiss D, Hopfen-Mueller W, et al. Treatment with insulin glargine (Lantus®) reduces asymptomatic nightly hypoglycemia detected by continuous subcutaneous glucose monitoring in children and adolescents with type 1 diabetes [abstract]. Diabetes 2002 Jun; 51 Suppl. 2: 427
Barnett AH. Basal insulin: answers from analogues? Pract Diabetes Int 2002; 19(7): 213–6
Siegmund T, Born T, Weber S, et al. Basal insulin therapy in type 2 diabetes: a prospective 18 month comparison of insulin glargine and NPH insulin in patients with a multiple injection regimen [abstract no. 1976-PO]. Proceedings of the 63rd Annual Scientific Sessions of the American Diabetes Association; 2003 13–16 Jun; New Orleans, Louisiana
Fonseca V, Bell D, Mecca T. Less symptomatic hypoglycemia with bedtime insulin glargine (Lantus) compared to bedtime NPH insulin in patients with type 2 diabetes [abstract no. 449-P]. Diabetes 2001; 50 Suppl. 2: 112–3
Fritsche A, Schweitzer MA, Häring H-U, et al. Glimepiride combined with morning insulin glargine, bedtime neutral protamine hagedorn insulin, or bedtime insulin glargine in patients with type 2 diabetes; a randomized, controlled trial. Ann Intern Med 2003; 138: 952–9
Massi Benedetti M, Humburg E, Dressier A, et al. A one-year, randomised, multicentre trial comparing insulin glargine with NPH insulin in combination with oral agents in patients with type 2 diabetes. Horm Metab Res 2003 Mar; 35(3): 189–96
Safety and efficacy of insulin glargine (HOE 901) versus NPH insulin in combination with oral treatment in type 2 diabetic patients. HOE 901/2004 Study Investigators Group. Diabetic Med 2003; 20: 545–51
Raskin P, Park G, Zimmermann J. The effect of HOE 901 on glycaemic control in type 2 diabetes [abstract]. Diabetes 1998; 47 Suppl. 1: A103
Riddle M, Rosenstock J. Treatment to target in type 2 diabetes: successful glycemic control with less nocturnal hypoglycaemia with insulin glargine versus NPH insulin added to oral therapy [abstract no. 150]. Diabetologia 2002 Aug; 45 Suppl. 2: A52
Rosenstock J, Schwartz SL, Clark CM, et al. Basal insulin therapy in type 2 diabetes: 28-week comparison of insulin glargine (HOE 901) and NPH insulin. Diabetes Care 2001; 24: 631–6
Yki-Järvinen H, Dressier A, Ziemen M, et al. Less nocturnal hypoglycemia and better post-dinner glucose control with bedtime insulin glargine compared with bedtime NPH insulin during insulin combination therapy in type 2 diabetes. Diabetes Care 2000; 23: 1130–6
Witthaus E, Stewart J, Bradley C. Improved psychological outcomes after initiation of insulin treatment in patients with type II diabetes [abstract no. 787]. Diabetologia 2000; 43 Suppl. 1: A205
Standl E, Maxeiner S, Schweitzer MA, et al. Morning versus bedtime insulin glargine in combination with glimepiride: no differences in incidence of nocturnal hypoglycemia in patients with type 2 diabetes [abstract]. Proceedings of the 63rd Annual Scientific Sessions of the American Diabetes Association; 2003 Jun 13–17; New Orleans, Louisiana
Rosenstock J, Benedetti MM, Häring H-U, et al. Confirmed lower risk of hypoglycemia with insulin glargine versus NPH insulin: a meta-analysis of 2304 patients with type 2 diabetes [abstract]. Proceedings of the 63rd Annual Scientific Sessions of the American Diabetes Association; 2003 Jun 13–17; New Orleans, Louisiana
Yki-Järvinen H, Häring H-U, Johnson E, et al. The relationship between glycemic control and hypoglycemia using insulin glargine versus NPH insulin: a meta-regression analysis in type 2 diabetes [abstract]. Proceedings of the 63rd Annual Scientific Sessions of the American Diabetes Association; 2003 Jun 13–17; New Orleans, Louisiana
Karacovsky-Bielesc G, Hirtz R. Glycemic control with insulin glargine in patients with type 2 diabetes is safely maintained in long-term exposure [abstract no. 1191-P]. Diabetes 2002 Jun; 51 Suppl. 2: A293
Fritsche A, Häring H-U, Togel E, et al. Treat-to-target with addon basal insulin: can insulin glargine reduce the barrier to target attainment? [abstract]. Proceedings of the 63rd Annual Scientific Sessions of the American Diabetes Association; 2003 Jun 13–17; New Orleans, Louisiana
Fischer JS, Dirani RG, Schwartz SL, et al. Impact of use of insulin, glargine, on Hbg Alc and BMI in a speciality (endocrine) practice population [abstract no. 393-P]. Diabetes 2002 Jun; 51 Suppl. 2: A97
Schreiber S, Russmann A. Improved metabolic control in patients with type 1 and type 2 diabetes following the initiation/ switching to insulin glargine in clinical practice [abstract no. 465-P]. Diabetes 2002 Jun; 51 Suppl. 2: A114–5
Pscherer S, Schreyer-Zell G, Gottsmann M. Experience with insulin glargine in patients with end-stage renal disease [abstract no. 216-OR]. Diabetes 2002 Jun; 51 Suppl. 2: A53
Schreiber SA, Russmann A. Long-term administration of insulin glargine (Lantus®): metabolic and weight benefits in patients with type 2 diabetes in clinical practice [abstract]. Proceedings of the 63rd Annual Scientific Sessions of the American Diabetes Association; 2003 Jun 13–17; New Orleans, Louisiana
Schreiber SA, Russmann A. Improved metabolic control with a favorable weight profile in patients with type 2 diabetes treated with insulin glargine in clinical practice [abstract no. 464-P]. Diabetes 2002 Jun; 51 Suppl. 2: A114
Stryjek-Kaminska D, Plininger I, Jaursch-Hancke C. Combined insulin glargine and metformin therapy for obese patients with type 2 diabetes mellitus [abstract no. 2531-P]. Diabetes 2002 Jun; 51 Suppl. 2: A423–4
Schiel R, Schweitzer MA, Müller U. Patients with type 2 diabetes on long-term insulin therapy can be switched to a single dose of insulin glargine plus oral hypoglycemic agents [abstract]. Proceedings of the 63rd Annual Scientific Sessions of the American Diabetes Association; 2003 Jun 13–17; New Orleans, Louisiana
MarburyT, Schwartz S, Rosenberg MA, et al. Evaluation of the safety, efficacy and tolerability of insulin glargine in subjects with impaired fasting glucose, impaired glucose tolerance or new-onset type 2 diabetes [abstract]. Proceedings of the 63rd Annual Scientific Sessions of the American Diabetes Association; 2003 Jun 13–17; New Orleans, Louisiana
Brange J, Volund A. Insulin analogs with improved pharmacokinetic profiles. Adv Drug Deliv Rev 1999; 35: 307–35
Forjanic-Klapproth J, Home P. Progression of retinopathy with insulin glargine or NPH insulin: a multi-trial analysis [abstract no. 1103]. Diabetologia 2001; 44 Suppl. 1: A287
Berkowitz K. Lantus? Or Lente? Am J Nurs 2002 Aug; 102(8): 55
Harmel AL, Somma L. Not all long-acting insulins are the same [letter]. Diabetes Care 2002 Sep; 25(9): 1666–7
Phillips W, Lando H. Insulin confusion: an observation [letter]. Diabetes Care 2002 Jun; 25(6): 1103–4
Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications Research Group. Retinopathy and nephropathy in patients with type 1 diabetes four years after a trial of intensive therapy. N Eng J Med 2000; 342: 381–9
Diabetes Control and Complications Trial Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Eng J Med 1993; 329: 977–86
Stratton IM, Adler AI, Neil HA, et al. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. BMJ 2000; 321: 405–12
UK Prospective Diabetes Study Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet 1998; 352: 837–53
UK Prospective Diabetes Study (UKPDS) Group. Effect of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes (UKPDS 34). Lancet 1998; 352: 854–65
Lawson ML, Gerstein HC, Tsui E, et al. Effect of intensive therapy on early macrovascular disease in young individuals with type 1 diabetes: a systematic review and meta-analysis. Diabetes Care 1999; 22 Suppl. 2: B35–9
Lindholm A. New insulins in the treatment of diabetes mellitus. Best Pract Res Clin Gastroenterol 2002 Jun; 16(3): 475–92
DeWitt DE, Hirsch IB. Outpatient insulin therapy in type 1 and type 2 diabetes mellitus: scientific review. JAMA 2003 May 7; 289(17): 2254–64
Lindström T, Olsson PO, Arnqvist HJ. The use of human ultralente is limited by great intraindividual variability in overnight plasma insulin profiles. Scand J Clin Lab Invest 2000; 60: 341–7
Aventis. Lantus® receives European approval for flexible administration: also receives positive opinion for pediatrie use from the European Committee for Proprietary Medicinal Products. Media Rel Available from URL: http://www.emea.eu.int [Accessed 2003 Jul 16]
Aventis (US). Lantus® (insulin glargine [rDNA origin] injection) receives FDA approval for flexible administration [online]. Available from URL: http://www.aventis.com [Accessed 2003 May 27]
Author information
Authors and Affiliations
Corresponding author
Additional information
Various sections of the manuscript reviewed by: R.K. Campbell, College of Pharmacy, Washington State University, Pullman, Washington, USA; L. Heinemann, Profil Institute for Metabolic Research, Neuss, Germany; T. Heise, Department of Metabolic Diseases and Nutrition, Heinrich Heine University, WHO Collaborating Center for Diabetes, Dusseldorf, Germany; T.L. Levien, College of Pharmacy, Washington State University Spokane, Spokane, Washington, USA; S.D. Luzio, Diabetes Research Unit, University Hospital of Wales and Llandough Hospital, Penarth, South Glamorgan, Wales; D.R. Owens, Diabetes Research Unit, University Hospital of Wales and Llandough Hospital, Penarth, South Glamorgan, Wales.
Data Selection
Sources: Medical literature published in any language since 2001 on insulin glargine, identified using Medline and EMBASE, supplemented by AdisBase (a proprietary database of Adis International). Additional references were identified from the reference lists of published articles. Bibliographical information, including contributory unpublished data, was also requested from the company developing the drug.
Search strategy: Medline search terms were ‘insulin glargine’ or ‘glargine’ or ‘HOE-901’. EMBASE search terms were ‘insulin glargine’ or ‘glargine’ or ‘HOE-901’. AdisBase search terms were ‘insulin-glargine’ or ‘glargine’ or ‘HOE 901’. Searches were last updated 12 Jul 2003.
Selection: Studies in patients with type 1 diabetes mellitus or type 2 diabetes who received insulin glargine. Inclusion of studies was based mainly on the methods section of the trials. When available, large, well-controlled trials with appropriate statistical methodology were preferred. Relevant pharmacodynamic and pharmacokinetic data are also included.
Index terms: Insulin glargine, type 1 diabetes mellitus, type 2 diabetes mellitus, pharmacodynamics, pharmacokinetics, therapeutic use.
Rights and permissions
About this article
Cite this article
Dunn, C.J., Plosker, G.L., Keating, G.M. et al. Insulin Glargine. Drugs 63, 1743–1778 (2003). https://doi.org/10.2165/00003495-200363160-00007
Published:
Issue Date:
DOI: https://doi.org/10.2165/00003495-200363160-00007