Abstract
Perioperative management of chronically anticoagulated patients and/or patients treated with antiplatelet therapy is a complex medical problem. This review considers the pharmacokinetic and pharmacodynamic properties of commonly used antiplatelet and anticoagulant drugs with special emphasis on loss of effects after discontinuation and possible counteracting (or antidote) strategies. These drugs are aspirin (acetylsalicylic acid), ticlopidine/clopidogrel, abciximab, tirofiban and eptifibatide, heparin (unfractionated and low-molecular-weight), warfarin and direct thrombin inhibitors. Since the pharmacological mechanisms of some of these drugs are based on irreversible or slowly reversible effects, their pharmacokinetic profiles are not necessarily predictive for their pharmacodynamic profiles. A close and direct relationship between plasma concentrations and effects is seen only for the glycoprotein (GP) IIb/IIIa inhibitors tirofiban and eptifibatide with a fast off-rate for dissociation from the GPIIb/IIIa receptor, and for direct thrombin inhibitors (hirudin and argatroban). For other compounds, drug concentrations in plasma and pharmacodynamic effects are not closely correlated because of, for example, irreversible binding to their target (aspirin, Clopidogrel and abciximab), inhibition of the generation of a subset of clotting factors with differing regeneration and degradation rates (coumarins) or sustained binding to the vascular wall (heparins).
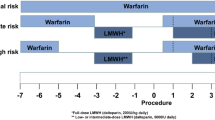
Surgery in patients on anticoagulant and/or antiplatelet therapy may be categorised as: (i) elective versus urgent; and (ii) cardiopulmonary bypass (CPB) versus non-CPB. Monotherapy with Clopidogrel or aspirin need not be discontinued in elective non-CPB surgery, and temporary discontinuation of warfarin should be accompanied by preoperative intravenous heparin only in selected high-risk patients. Vitamin K as an antidote for warfarin should only be used subcutaneously and solely in urgent/emergency surgery. In elective surgery requiring CPB (coronary artery bypass grafting), it is recommended to discontinue aspirin 7 days preoperatively in patients with a low risk profile. Patients requiring urgent CPB surgery (e.g. after failure of a percutaneous coronary angioplasty with or without coronary stent deployment) are usually pretreated with several antiplatelet agents (e.g. aspirin and Clopidogrel, together with a GPIIb/IIIa inhibitor) together with unfractionated or low-molecular-weight heparin. With judicious planning, urgent/emergency cardiac surgery can be safely performed on these patients. Delaying surgery (e.g. for 12 hours in patients treated with abciximab) should be considered if possible. Standard heparin doses should be given to achieve optimal anticoagulation for CPB. Prophylactic use of aprotinin (intraand/or postoperatively), aminocaproic acid or tranexamic acid should be considered. Early (in the operating theatre prior to chest closure) and judicious use of replacement blood products (platelets) should be commenced when clinically indicated.



Similar content being viewed by others
References
Takahashi T, Kawamata T, Namiki A. A case of postoperative acute myocardial infarction due to the interruption of anticoagulant therapy. Masui 2002; 51: 280–2
Schanbacher CF, Bennett RG. Postoperative stroke after stopping warfarin for cutaneous surgery. Dermatol Surg 2000; 26: 785–9
Palareti G, Legnani C. Warfarin withdrawal: pharmacokineticpharmacodynamic considerations. Clin Pharmacokinet 1996; 30: 300–13
Ferraris VA, Gildengorin V. Predictors of excessive blood use after coronary artery bypass grafting: a multivariate analysis. J Thorac Cardiovasc Surg 1989; 98: 492–7
Ferraris VA, Ferraris SP, Joseph O, et al. Aspirin and postoperative bleeding after coronary artery bypass grafting. Ann Surg 2002; 235: 820–7
Yende S, Wunderink RG. Effect of Clopidogrel on bleeding after coronary artery bypass surgery. Crit Care Med 2001; 29: 2271–4
Gammie JS, Zenati M, Kormos RL, et al. Abciximab and excessive bleeding in patients undergoing emergency cardiac operations. Ann Thorac Surg 1998; 65: 465–9
Juergens CP, Yeung AC, Oesterle SN. Routine platelet transfusion in patients undergoing emergency coronary bypass surgery after receiving abciximab. Am J Cardiol 1997; 80: 74–5
Arjomand H, Mascarenhas DA, Morgan RJ. Abciximab and the risk of bleeding during emergency cardiac operations. Ann Thorac Surg 1999; 67: 292–3
Silvestry SC, Smith PK. Current status of cardiac surgery in the abciximab-treated patient. Ann Thorac Surg 2000; 70 (2Suppl.): S12–9
Alvarez JM. Emergency coronary bypass grafting for failed percutaneous coronary artery stenting: increased costs and platelet transfusion requirements after the use of abciximab. J Thorac Cardiovasc Surg 1998; 115: 472–3
Alvarez JM. Coronary stenting and use of abciximab. Lancet 1998; 17: 1311–2
Singh M, Nuttall GA, Ballman KV, et al. Effect of abciximab on the outcome of emergency coronary artery bypass grafting after failed percutaneous coronary intervention. Mayo Clin Proc 2001; 76: 784–8
Vahl CF, Kayhan N, Thomas G, et al. Myocardial revascularization after pretreatment with the GPIIb/IIIa receptor blocker abciximab. Z Kardiol 2001; 90: 889–97
Bizzarri F, Scolletta S, Tucci E, et al. Perioperative use of tirofiban hydrochloride (Aggrastat) does not increase surgical bleeding after emergency or urgent coronary artery bypass grafting. J Thorac Cardiovasc Surg 2001; 122: 1181–5
Dyke CM, Bhatia D, Lorenz TJ, et al. Immediate coronary artery bypass surgery after platelet inhibition with eptifibatide: results from PURSUIT (Platelet Glycoprotein IIb/IIIa in Unstable Angina: Receptor Suppression Using Integrelin Therapy). Ann Thorac Surg 2000; 70: 866–71
Horlocker TT. Low molecular weight heparin and neuraxial anesthesia. Thromb Res 2001; 101: V141–54
Horlocker TT, Wedel DJ, Schroeder DR, et al. Preoperative antiplatelet therapy does not increase the risk of spinal hematoma associated with regional anesthesia. Anesth Analg 1995; 80: 303–9
Urmey WF, Rowlingson J. Do antiplatelet agents contribute to the development of perioperative spinal hematoma? Reg Anesth Pain Med 1998; 23 Suppl. 2: 146–51
Neilipovitz DT, Bryson GL, Nichol G. The effect of perioperative aspirin therapy in peripheral vascular surgery: a decision analysis. Anesth Analg 2001; 93: 573–80
Kearon C, Hirsh J. Management of anticoagulation before and after elective surgery. N Engl J Med 1997; 336: 1506–11
Wahl MJ. Dental surgery in anticoagulated patients. Arch Intern Med 1998; 158: 1610–6
Hull RD, Raskob GE, Hirsh J, et al. Continuous intravenous heparin compared with intermittent subcutaneous heparin in the initial treatment of proximal-vein thrombosis. N Engl J Med 1986; 315: 1109–14
De Swart CAM, Nijmeyer B, Roelofs JMM, et al. Kinetics of intravenously administered heparin in normal humans. Blood 1982; 60: 1251–8
Hirsh J, Warkentin TE, Shaughnessy SG, et al. Heparin and low-molecular-weight heparin: mechanisms of action, pharmacokinetics, dosing, monitoring, efficacy, and safety. Chest 2001; 119: 64–94S
Levine MN, Hirsh J, Kelton JG. Heparin induced bleeding. In: Lane DA, Lindahl U, editors. Heparin: chemical and biological properties, clinical applications. London: Edward Arnold, 1989: 517–32
Morabia A. Heparin doses and major bleedings. Lancet 1986; I: 1278–9
Levy JH. Pharmacologic preservation of the hemostatic system during cardiac surgery. Ann Thorac Surg 2001; 72: 1814–20
Young E, Wells P, Holloway S, et al. Ex-vivo and in-vitro evidence that low molecular weight heparins exhibit less binding to plasma proteins than unfractionated heparin. Thromb Haemostasis 1994; 71: 300–4
Kessler CM, Esparraguera IM, Jacobs HM, et al. Monitoring the anticoagulant effects of a low molecular weight heparin preparation: correlation of assays in orthopedic surgery patients receiving ardeparin sodium for prophylaxis of deep venous thrombosis. Am J Clin Pathol 1995; 103: 642–8
Kronemann H, Eikelboom BC, Knot EA, et al. Pharmacokinetics of low-molecular-weight heparin and unfractionated heparin during elective aortobifemoral bypass grafting. J Vasc Surg 1991; 14: 208–14
Holst J, Lindblad B, Bergqvist D, et al. Protamine neutralization of intravenous and subcutaneous low-molecular-weight heparin (tinzaparin): an experimental investigation in healthy volunteers. Blood Coagul Fibrinolysis 1994; 5: 795–803
Bauer KA. Fondaparinux sodium: a selective inhibitor of factor Xa. Am J Health Syst Pharm 2001; 58 Suppl. 2: S14–7
Bijsterveld NR, Moons AH, Boekhold SM, et al. Ability of recombinant factor VIIa to reverse the anticoagulant effect of the pentasaccharide fondaparinux in healthy volunteers. Circulation 2002; 106: 2550–4
Keam SJ, Goa KL. Fondaparinux sodium. Drugs 2002; 62: 1673–85
Weitz JI, Leslie B, Hudoba M. Thrombin binds to soluble fibrin degradation products where it is protected from inhibition by heparin-antithrombin but susceptible to inactivation by antithrombin-independent inhibitors. Circulation 1998; 97: 544–52
Weitz JI, Harry RB. Direct thrombin inhibitors in acute coronary syndromes: present and future. Circulation 2002; 105: 1004–11
Stringer KA, Lindenfeld J. Hirudins: antithrombin anticoagulants. Ann Pharmacother 1992; 26: 1535–40
Zoldhelyi P, Webster MW, Fuster V, et al. Recombinant hirudin in patients with chronic, stable coronary artery disease: safety, half-life, and effect on coagulation parameters. Circulation 1993; 88: 2015–22
Robson R, White H, Aylward P, et al. Bivalirudin pharmacokinetics and pharmacodynamics: effect of renal function, dose, and gender. Clin Pharmacol Ther 2002; 71: 433–9
Fitzgerald D, Murphy N. Argatroban: a synthetic thrombin inhibitor of low relative molecular mass. Coron Artery Dis 1996; 7: 455–8
McKeage K, Plosker GL. Argatroban. Drugs 2001; 61: 515–22
Gustafsson D, Elg M. The pharmacodynamics and pharmacokinetics of the oral direct thrombin inhibitor ximelagatran and its active metabolite melagatran: a mini-review. Thromb Res 2003; 109 Suppl. 1: S9–15
Harder S, Graff J, Klinkhardt U, et al. Transition from argatroban to oral anticoagulation with phenprocoumon or acenocoumarol: effects on Prothrombin time, activated partial thromboplastin time, and Ecarin clotting time. Thromb Haemost 2004; 91: 1137–45
Hirsh J, Dalen JE, Anderson DR, et al. Oral anticoagulants: mechanism of action, clinical effectiveness, and optimal therapeutic range. Chest 2001; 119: 8–21
Breckenridge AM. Oral anticoagulant drugs: pharmacokinetic aspects. Semin Hematol 1978; 15: 19–26
O’Reilly RA. Warfarin metabolism and drug-drug interactions. In: Wessler S, Becker CG, Nemerson Y, editors. The new dimensions of warfarin prophylaxis: advances in experimental medicine and biology. New York: Plenum, 1986: 205–12
Mannucci PM. Genetic control of anticoagulation. Lancet 1999; 353: 688–9
Harder S, Thurmann P. Clinically important drug interactions with anticoagulants: an update. Clin Pharmacokinet 1996; 30: 416–44
White RH, McKittrick T, Hutchinson R, et al. Temporary discontinuation of warfarin therapy: changes in the international normalized ratio. Ann Intern Med 1995; 122: 40–2
Patrono C. Aspirin as an antiplatelet drug. N Engl J Med 1994; 330: 1287–9
Schroder H, Schror K. Clinical pharmacology of acetylsalicylic acid. Z Kardiol 1992; 81: 171–5
Cryer B, Feldman M. Cyclooxygenase-1 and cyclooxygenase-2 selectivity of widely used nonsteroidal anti-inflammatory drugs. Am J Med 1998; 104: 413–21
Antiplatelet Trialists’ Collaboration. Collaborative overview of randomised trials of antiplatelet therapy: I: prevention of death, myocardial infarction, and stroke by prolonged antiplatelet therapy in various categories of patients. BMJ 1994; 308: 81–106
Benedek IH, Joshi AS, Pieniaszek HJ, et al. Variability in the pharmacokinetics and pharmacodynamics of low dose aspirin in healthy male volunteers. J Clin Pharmacol 1995; 35: 1181–6
Feldman M, Shewmake K, Cryer B. Time course inhibition of gastric and platelet COX activity by acetylsalicylic acid in humans. Am J Physiol Gastrointest Liver Physiol 2000; 279: 1113–20
Quinn MJ, Fitzgerald DJ. Ticlopidine and Clopidogrel. Circulation 1999; 100: 1667–72
Savi P, Combalbert J, Gaich C, et al. The antiaggregating activity of Clopidogrel is due to a metabolic activation by the hepatic cytochrome P450-1A. Thromb Haemost 1994; 26: 347–55
Savi P, Pereillo JM, Uzabiaga MF, et al. Identification and biological activity of the active metabolite of Clopidogrel. Thromb Haemost 2000; 84: 891–6
Klinkhardt U, Kirchmaier CM, Westrup D, et al. Ex vivo-in vitro interaction between aspirin, Clopidogrel, and the glycoprotein IIb/IIIa inhibitors abciximab and SR121566A. Clin Pharmacol Ther 2000; 67: 305–13
Heptinstall S, May JA, Glenn JR, et al. Effects of ticlopidine administered to healthy volunteers on platelet function in whole blood. Thromb Haemost 1995; 74: 1310–5
Cattaneo M, Akkawat B, Lecchi A, et al. Ticlopidine selectively inhibits human platelet responses to adenosine diphosphate. Thromb Haemost 1991; 66: 694–9
Weber AA, Braun M, Hohfeld T, et al. Recovery of platelet function after discontinuation of Clopidogrel treatment in healthy volunteers. Br J Clin Pharmacol 2001; 52: 333–6
Yusuf S, Zhao F, Mehta SR, et al. Effects of Clopidogrel in addition to aspirin in patients with acute coronary syndromes without ST-segment elevation. N Engl J Med 2001; 345: 494–502
Kleiman NS. Pharmacokinetics and pharmacodynamics of glycoprotein IIb-IIIa inhibitors. Am Heart J 1999; 138: 263–75
Klinkhardt U, Graff J, Westrup D, et al. Pharmacodynamic characterization of the interaction between abciximab or tirofiban with unfractionated or a low molecular weight heparin in healthy subjects. Br J Clin Pharmacol 2000; 52: 297–305
Faulds D, Sorkin EM. Abciximab (c7E3 Fab): a review of its pharmacology and therapeutic potential in ischaemic heart disease. Drugs 1994; 48: 583–98
Tcheng JE, Ellis SG, George BS, et al. Pharmacodynamics of chimeric glycoprotein IIb/IIIa integrin antiplatelet antibody Fab 7E3 in high-risk coronary angioplasty. Circulation 1994; 90: 1757–64
Harder S, Kirchmaier CM, Krzywanek HJ, et al. Pharmacokinetics and pharmacodynamic effects of a new antibody glycoprotein IIb/IIIa inhibitor (YM337) in healthy subjects. Circulation 1999; 100: 1175–81
Lefkovits J, Topol EJ. Platelet glycoprotein IIb/IIIa receptor antagonists in coronary artery disease. Eur Heart J 1996; 17: 9–18
Tcheng JE, Talley JD, O’shea JC, et al. Clinical pharmacology of higher dose eptifibatide in percutaneous coronary intervention (the PRIDE study). Am J Cardiol 2001; 88: 1097–102
Theroux P, White H, David D, et al. A heparin-controlled study of MK-383 in unstable angina [abstract]. Circulation 1994; 90 Suppl. 1: I–231
Barrett JS, Murphy G, Peerlinck K, et al. Pharmacokinetics and pharmacodynamics of MK-383, a selective non-peptide platelet glycoprotein-IIb/IIIa receptor antagonist, in healthy men. Clin Pharmacol Ther 1994; 56: 377–88
Thompson CM, Steinhubl SR. Monitoring of platelet function in the setting of glycoprotein IIb/IIIa inhibitor therapy. J Interv Cardiol 2002; 15: 61–70
Poullis M, Manning R, Haskard D, et al. Reopro removal during cardiopulmonary bypass using a hemoconcentrator. J Thorac Cardiovasc Surg 1999; 117: 1032–4
Lemmer Jr JH. Abciximab (ReoPro) removal with a hemoconcentrator during cardiopulmonary bypass. J Thorac Cardiovasc Surg 1999; 118: 980–1
Steinhubl SR, Moore SA, Lincoff AM. Abciximab (ReoPro) removal during cardiopulmonary bypass with a hemoconcentrator. J Thorac Cardiovasc Surg 2000; 119: 401–2
Poullis M. Abciximab (ReoPro) removal during cardiopulmonary bypass with a hemoconcentrator. J Thorac Cardiovasc Surg 2000; 119: 401–2
Royston D. Aprotinin versus lysine analogues: the debate continues. Ann Thorac Surg 1998; 65: S9–19
Jacobs LG, Nusbaum N. Perioperative management and reversal of antithrombotic therapy. Clin Geriatr Med 2001; 17: 189–202
Sindet-Pedersen S, Ramstrom G, Bernvil S, et al. Hemostatic effect of tranexamic acid mouthwash in anticoagulant-treated patients undergoing oral surgery. N Engl J Med 1989; 320: 840–3
Douketis JD. Perioperative anticoagulation management in patients who are receiving oral anticoagulant therapy: a practical guide for clinicians. Thromb Res 2002; 108: 3–13
Eagle KA, Guyton RA, Davidoff R, et al. ACC/AHA guidelines for coronary artery bypass graft surgery: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Revise the 1991 Guidelines for Coronary Artery Bypass Graft Surgery). J Am Coll Cardiol 1999; 34: 1262–347
Mangano DT, the Multicenter Study of Perioperative Ischemia Research Group. Aspirin and mortality from coronary bypass surgery. N Engl J Med 2002; 347: 1309–17
Alvarez JM, Chen L, Sinclair IN. Acute stent thrombosis following off pump coronary bypass surgery: a new and avoidable complication? J Thorac Cardiovasc Surg 2003; 125: 1544–6
Alvarez JM, Harper RW, Peverill RE. Emergency coronary artery bypass grafting (CABG) after failed coronary artery intervention: caution regarding the combined use of aspirin, ticlopidine and abciximab. Aust N Z J Med 1998; 28: 463–4
Alvarez JM, Jackson LR, Chatwin C, et al. Low dose postoperative aprotinin reduces mediastinal drainage and blood transfusion requirements in primary CABG patients on aspirin: a prospective, double-blind, placebo-controlled trial. J Thorac Cardiovasc Surg 2001; 112: 457–63
Christenson JT, Maurice J, Simonet F, et al. Open chest and delayed sternal closure after cardiac surgery. Eur J Cardiothorac Surg 1996; 10: 305–11
Bouboulis N, Rivas LF, Kuo J, et al. Packing the chest: a useful technique for intractable bleeding after open heart operation. Ann Thorac Surg 1994; 57: 856–60
O’Regan DJ, Giannopoulos N, Mediretta N, et al. Topical aprotinin in cardiac operations. Ann Thorac Surg 1994; 58: 778–81
Peters DC, Noble S. Aprotinin: an update of its pharmacology and therapeutic use in open heart surgery and coronary artery bypass surgery. Drugs 1999; 57: 233–60
Munoz JJ, Birkemeyer NJ, Birkemeyer JD, et al. Is epsilonaminocaproic acid as effective as aprotinin in reducing bleeding with cardiac surgery?. A meta analysis. Circulation 1999; 99: 81–9
Laupacis A, Fergusson D. Drugs to minimize perioperative blood loss in cardiac surgery: meta-analyses using perioperative blood transfusion as the outcome. The International Study of Peri-operative Transfusion (ISPOT) investigators. Anesth Analg 1997; 85: 1258–67
Levi M, Cromheecke ME, de Jonge E, et al. Pharmacological strategies to decrease excessive blood loss in cardiac surgery: a meta-analysis of clinically relevant endpoints. Lancet 1999; 345: 1940–7
Alvarez JM, Quiney NF, McMillan D, et al. The use of ultralow-dose aprotinin to reduce blood loss in cardiac surgery. J Cardiothorac Vasc Anesth 1995 Feb; 9(1): 29–33
Westaby S. Aprotinin in perspective. Ann Thorac Surg 1993; 44: 1033–41
Ciçek S, Demirkiliç U, Özal E, et al. Postoperative use of aprotinin in cardiac operations: an alternative to its prophylactic use. J Thorac Cardiovasc Surg 1996; 112: 1462–7
Ciçek S, Demirkiliç U, Özal E, et al. Postoperative aprotinin: effect on blood loss and transfusion requirements in cardiac operations. Ann Thorac Surg 1996; 61: 1372–6
Forestier F, B’elisle S, Robitaille D, et al. Low-dose aprotinin is ineffective to treat excessive bleeding after cardiopulmonary bypass. Ann Thorac Surg 2000; 69: 452–6
Alvarez JM, Goldstein J, Mezzatesta J, et al. Fatal intraoperative pulmonary thrombosis after graft replacement of an aneurysm of the arch and descending aorta in association with deep hypothermic circulatory arrest and aprotinin therapy. J Thorac Cardiovasc Surg 1998; 115: 723–4
Alvarez JM, Chandraratna H, Newman MA. Intraoperative coronary thrombosis in association with low-dose aprotinin therapy. J Cardiothorac Vasc Anesth 1999; 13: 623–8
Alderman EL, Levy JH, Rich JB, et al. Analyses of coronary graft patency after aprotinin use: results from the International Multicenter Aprotinin Graft Patency Experience (IMAGE) trial. J Thorac Cardiovasc Surg 1998; 116: 716–30
Hébert PC, Wells G, Blajchman MA, et al. The Transfusion Requirements in Critical Care Investigators for the Canadian Critical Care Trials Group: a multicenter, randomized, controlled clinical trial of transfusion requirements in critical care. N Engl J Med 1999; 340: 409–17
Weightman WM, Gibbs NM, Weidmann CR, et al. The effect of preoperative aspirin-free interval on red blood cell transfusion requirements in cardiac surgical patients. J Cardiothorac Vasc Anesth 2002; 16: 54–8
Hedner U. NovoSeven as a universal haemostatic agent. Blood Coagul Fibrinolysis 2000; 11 Suppl. 1: S107–11
Al Douri M, Shafi T, Al Khudairi D, et al. Effect of the administration of recombinant activated factor VII (rFVIIa; NovoSeven) in the management of severe uncontrolled bleeding in patients undergoing heart valve replacement surgery. Blood Coagul Fibrinolysis 2000; 11 Suppl. 1: S121–7
Acknowledgements
The authors have provided no information on sources of funding or on conflicts of interest directly relevant to the content of this review.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Harder, S., Klinkhardt, U. & Alvarez, J.M. Avoidance of Bleeding During Surgery in Patients Receiving Anticoagulant and/or Antiplatelet Therapy. Clin Pharmacokinet 43, 963–981 (2004). https://doi.org/10.2165/00003088-200443140-00002
Published:
Issue Date:
DOI: https://doi.org/10.2165/00003088-200443140-00002