Oral Presentations
Risk Management Plans
OP01. Training on Risk Management Planning
E. Brown
Elliot Brown Consulting Ltd, Primevigilance Ltd, UK
Risk management planning for medicines has assumed increasing importance in recent years[1–3] but associated training needs may not have been clearly defined. There are several groups for whom training may be valuable in the context of Risk Management Plans (RMPs). These include: top management who are responsible for overall strategy, allocation of resources, planning and budgets in pharmaceutical companies; department heads in pharmaceutical companies who commission RMPs; individuals or groups (in pharmaceutical companies or contract organisations) who contribute to, write or update RMPs; company personnel who review or approve RMPs; regulators who assess the RMPs.
There are various subjects for the training, depending on who is being trained: understanding concepts of risk management and how these apply to medicines; knowledge of why risk management is needed and circumstances under which RMPs are required; awareness of the regulatory framework, depending on geographical region; knowledge of guidelines; understanding of organisational and logistical issues, such as setting up multidisciplinary teams, time/cost in preparing RMPs; ability to assess the need for additional pharmacovigilance or risk minimisation activities according to the medicines and the risks concerned; knowledge of methods for identifying, quantifying and characterising risk, including conventional pharmacovigilance, interventional and non-interventional studies; understanding of methods available for risk minimisation and for evaluating their effectiveness; awareness of sources of information needed to prepare the RMP and of internal and external resources that may be needed for implementation; understanding of the need for pragmatism, considering factors such as acceptability of uncertainty of risk, magnitude and severity of risks, costs and options for risk measurement and risk minimisation, the seriousness of disease being treated and the commercial viability of the product.
Concepts of risk management in relation to medicines are evolving, as are regulatory requirements. In addition to the practicalities associated with preparing and updating risk management plans there should be awareness of scientific and regulatory developments and this also is an element that needs to be included in training. Recently introduced concepts of benefit-risk management will require deployment of additional understanding and skills even for those with significant experience and expertise to date in writing and implementing risk management plans.
In this paper, we consider these points, who should be trained on what and by whom; how the training can be imparted; and what might be done to measure its effectiveness.
OP02. The Use of Internet Surveys to Measure the Effectiveness of Educational Materials for Use as Risk Minimisation Tools: What to Consider?
C.R. Knight
TranScrip Partners LLP, UK
Introduction: Risk Management Plans (RMPs) and Risk Evaluation and Mitigation Strategies (REMS) are a regulatory requirement for newly-licensed medicines.[1,2] In addition, other tools, such as product monographs and patient educational materials, are also used as risk-minimisation tools. Follow-up assessment on the effectiveness of these risk minimisation tools is now expected from regulatory authorities. It is important that companies consider which evaluation methods to adopt at a very early stage of the regulatory approval process, so that these planned risk minimisation activities can be communicated to regulatory authorities as part of the overall submission.
Discussion: When assessing the effectiveness of educational materials, several evaluation methods are applied, including questionnaires, telephone interviews and surveys. The first step for organisations is to develop close working relationships with all the relevant in-house departments. This will ensure that there is an integrated approach to risk communications and also agreement on which method of evaluation are considered optimal.[3]
Should the Internet survey approach be agreed upon, then the following items should also be considered in the planning:
-
• Deciding on the data elements for collection and how this data will then be analysed and presented to regulatory authorities
-
• Producing an in-house survey tool, and deciding what resource will be necessary for this development and by when
-
• Deciding to outsource the development of an Internet survey tool and conducting appropriate evaluations of any potential third-party providers
Finally, it is important to consider the mix of survey respondents providing this feedback. If there is potentially a high proportion of non-Internet users amongst those groups that need to be included within the evaluation process, then possibly some other parallel evaluation activities may need considering. These may include additional telephone interview surveys or paper based questionnaires. It is important that any evaluation is not considered biased due to either the unavailability of the Internet by individual responder groups.
Conclusion: Internet surveys provide an effective method in collecting follow-up information on the effectiveness of educational materials. Planning for these evaluations must happen well ahead of the launch of the newly-licensed medicine. The balance between collecting high quality feedback must also be considered against the need to maintain high levels of internet security and data privacy. Healthcare companies also need to be aware of the extent of Internet usage when considering Internet surveys as an evaluation tool for risk-minimisation measures, and make appropriate alternative arrangements as necessary.
OP03. Measuring REMS Effectiveness: Time for a Program Overhaul?
M. Mease
Quintiles
It is time for concrete progress toward the ultimate risk management goal of predicting and avoiding adverse events linked to biopharmaceuticals. Four years after Congress passed the FDA Amendments Act (FDAAA), challenges continue to surround Risk Evaluation and Mitigation Strategies (REMS).[1] As of February 2011, the FDA had approved 166 REMS, and some 780 drugs currently have an FDA safety-related requirement.[2] Yet around three-quarters of healthcare stakeholders believe that the REMS program needs a major overhaul, according to a recent survey by the Tufts Center for the Study of Drug Development (CSDD).[3] According to most survey respondents, “it is virtually impossible to measure the benefits of a REMS, compared to its burdens on patient access and cost of health care delivery, for a newly approved drug, and that even for an already-approved drug, it would likely require two years or more to effectively conduct such an assessment.” The issue of continuing adverse events was highlighted in June 2011 by the Safer Medicines Trust in a open letter to The Lancet,[4] quoting a European Commission estimate that adverse drug reactions kill 197 000 EU citizens per year, incurring €79 billion in costs. If implemented properly, REMS could integrate all healthcare providers, treatment strategies and patient data into a single, comprehensive and patient-centric process. To achieve this, all stakeholders must have input into REMS development to ensure that they provide effective and measurable results.[5] For an objective assessment of the effectiveness of each REMS, there is a need for evaluation methods and tools to evolve. As input to this process, FDA should share the results of its analyses of existing REMS with industry. In the meantime, REMS have potential to create an obstacle to access, and to expose patients to more serious safety effects from alternatives.
This presentation will examine the REMS approved to date, compare the REMS objectives with their content and activities, and assess whether the objectives are met. We will also describe the changes to FDA’s February 2011 draft Guidance on Medication Guide-only REMS requirements. An FDA public meeting heard that medication guides sometimes do not reach patients as intended, may need improvements in comprehensibility and ease of understanding, and that many pharmacists are not familiar with these tools. In this context, we will discuss whether Medication Guides should be required given their questionable content and distribution.
Signal Detection
OP04. An Empirical Study of Exclusion Criteria for Disproportionality Analysis
J. Hopstadius,1 M. Hauben 12 and G.N. Norén 3
1 Uppsala Monitoring Centre, Uppsala, Sweden; 2 Pfizer Inc., New York, NY, USA; New York University School of Medicine, New York, NY, USA; New York Medical College, Valhalla, NY, USA; Brunel University, West London, UK; 3 Uppsala Monitoring Centre, Uppsala, Sweden; Stockholm University, Stockholm, Sweden
Background: Individual case safety reports vary substantially in nature and origin. Many organisations rely on computerized methods for first-pass adverse drug reaction (ADR) surveillance in which the reporting patterns for specific drugs are compared against the generality of the database. An open question is what reports to include in such analyses.
Objective: To determine the overall impact on disproportionality analysis of a range of exclusion criteria restricting the analysis to a subset of the available reports.
Methods: We analysed the WHO global individual case safety reports database, VigiBase, as of 2010-02-15. Values of the Information Component (IC) measure of disproportionality based on the database as a whole were compared against IC values under the exclusion of, in turn: suspected duplicates, reports from lawyers, literature reports, direct patient reports, reports from clinical trials, reports from special studies, reports with multiple suspected drugs, reports with at least 10 drugs and 10 ADRs, reports on vaccines, reports before 1990, and reports before 2000. Differences between the crude IC and the IC under different exclusion criteria were visualized in box plots. The number of drug-ADR pairs with Statistics of Disproportionate Reporting (SDR) shifting to non-SDRs, and vice versa were identified. All proposed exclusion criteria were compared against random removal of a similar number of reports.
Results: Exclusion of reports had considerable effect on disproportionality analysis, and the more reports excluded, the greater the impact. The greatest impact was seen under exclusion of reports with multiple suspected drugs, reports before 2000, direct patient reports, and vaccine reports. However, most of the variation is explicable by the sheer number of reports removed under different criteria. That is, similar effects are seen also under removal of randomly selected reports. More substantial changes in the measure of disproportionality proved more likely to reflect real patterns in data, but were on the other hand limited to a narrow range of drugs and ADRs for each criterion.
Conclusions: Separate treatment of different types of reports, time periods, and reports with one or several suspected drugs requires care but can be valuable in highlighting a limited number of reporting patterns that would otherwise be missed. Stratification would typically be preferred over report exclusion.
OP05. A Reference Standard for Evaluating Methods for Drug Safety Signal Detection using Electronic Healthcare Record (EHR) Databases
P.M. Coloma,1 P. Avillach,2 M.J. Schuemie,1 C. Ferrajolo,1 A. Pariente,3 A. Fourrier Reglat,3 A. Ottosson,4 J. van der Lei,1 M. Sturkenboom 1 and G. Trifirò 5
1 Department of Medical Informatics, Erasmus Medical Center, Rotterdam, The Netherlands; 2 LERTIM, Faculté de Médecine, Université Aix Marseille 2, Marseille, France; 3 Inserm U657, Pharmacology Department, Bordeaux, France; 4 AstraZeneca, Lund, Sweden; 5 Department of Clinical and Experimental Medicine and Pharmacology, Section of Pharmacology, University of Messina, Messina, Italy
Background: The growing interest in the utility of electronic healthcare records (EHR) databases for drug safety surveillance has spurred development of new methodologies for signal detection. There is, however, no definitive list of known adverse drug reactions and which drugs can cause them.[1] As there is no true gold standard, most of the methods used in drug safety signal detection have not been prospectively evaluated.
Objectives: Within the context of methods development and evaluation in the EU-ADR project, we propose a reference standard of drug-adverse event pairs acknowledged to be associated (i.e., ‘true positive’) and drug-event pairs where there is currently no ‘known proof’ of such association (i.e., ‘true negative’).
Methods: The reference standard was constructed for ten top-ranked events judged as important in pharmacovigilance based on the following criteria: (1) ‘trigger for drug withdrawal’; (2) ‘trigger for black box warning’; (3) ‘leading to emergency department visit or hospitalization’; (4) ‘probability of event to be drug-related’; and (5) ‘likelihood of death’. A stepwise approach was employed to identify which, among a list of drug-event associations, are previously well-known (true positive associations) or highly unlikely (true negative associations) based on published scientific literature, drug product labels, spontaneous reports made to pharmacovigilance database systems, and expert opinion. Only drugs with adequate exposure in EU-ADR to allow detection of an association were considered. Manual verification of ‘true positive’ and ‘true negative’ associations was independently performed by two researchers with expertise in clinical medicine, pharmacoepidemiology, and pharmacovigilance. A third expert arbitrated in case of disagreement between evaluators.
Results: 95 drug-event combinations comprised the reference standard, which included 45 ‘true positive’ associations and 50 ‘true negative’ associations for 10 events of interest: bullous eruptions; acute renal failure; anaphylactic shock; acute myocardial infarction; rhabdomyolysis; aplastic anemia; neutropenia; cardiac valve fibrosis; acute liver injury; and upper gastrointestinal bleeding. For cardiac valve fibrosis, there was no drug with adequate exposure in the database network to permit detection of a ‘true positive’ association.
Conclusions: Proper evaluation of new signal detection methodologies calls for the creation of a reference standard, the purpose of which is to better define the predictive value of such methodologies and their added value to the current pharmacovigilance armamentarium. The reference standard is by no means definitive, however, and should be seen as dynamic. As knowledge on drug safety evolves and new issues in drug safety arise, this reference standard will need to be re-evaluated.
Periodic Safety Update Reports
OP06. The Outcome of PSUR Assessments of Biopharmaceuticals
H.C. Ebbers,1 A.K. Mantel Teeuwisse,1 F.A. Sayed Tabatabaei,2 E.H. Moors,3 H. Schellekens 4 and H.G. Leufkens 1
1 Division of Pharmacoepidemiology and Pharmacotherapy, Utrecht Institute for Pharmaceutical Sciences (UIPS), Utrecht University, Utrecht, the Netherlands; 2 Medicines Evaluation Board, The Hague, the Netherlands; 3 Copernicus Institute/Department of Innovation and Environmental Studies, Utrecht University, Utrecht, the Netherlands; 4 Department of Pharmaceutics, Utrecht Institute for Pharmaceutical Sciences (UIPS), Faculty of Science, Utrecht, the Netherlands
Background: Recent changes introduced to European legislation amend the requirements for the submission of periodic safety update reports (PSURs). However, information on the outcome of PSUR assessment is lacking.
Aim: To describe the outcomes of PSUR assessments.
Methods: A cross sectional analysis was performed of all PSURs and PSUR assessment reports (AR) issued between July 1st 2008 and June 30th 2010 for all biopharmaceuticals centrally approved in the European Union. PSURs and PSUR ARs were obtained from the repository of the Dutch Medicines Evaluation Board, CBG-MEB.
Results: PSURs and PSUR ARs were collected for 70 products. Most products in the sample belonged to the ATC group of antineoplastic and immunomodulating agents (n = 26, 37.1%). Of the 70 PSURs included in the sample 26 (37%) covered a period of 6 months, 24 (34%) a period of 1 year and 20 (29%) a period of more than 1 year.
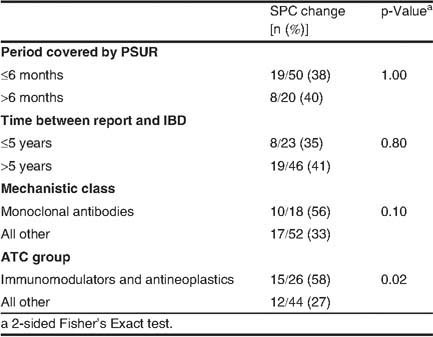
The most common outcome of PSUR assessment was monitoring a possible safety issue, which was requested in 55 (79%) of all ARs. Of these, 23 (42%) included new safety concerns not identified before. New safety concerns were identified in 35% of the PSURs that were issued within 5 years of the international birth date (IBD) of the product, and in 40% of the PSURs submitted after 5 years of the IBD (p = 0.795). Cumulative reviews of data relating to a possible safety issue were requested in 31 (44%) of the PSUR assessments and 27 (39%) of the assessments resulted in proposals and/or requests to change the Summary of Product Characteristics (SPC). The proportion of assessments resulting in SPC changes in various subgroups is presented in table I.
Conclusions: PSUR assessments are an important tool in the dialogue between regulators and marketing authorization holders. PSUR assessments are involved in the safety management of both new and well established products. New safety concerns occur throughout the life-cycle of biopharmaceuticals and may occur more often for products in different therapeutic and mechanistic classes.
Vaccine Pharmacovigilance
OP07. The Italian Surveillance of HPV Vaccination
S. Spila Alegiani, R. Da Cas, C. Giambi, R. Raschetti and S. Salmaso
National Institute of Health, Centre of Epidemiology, Rome, Italy
Objectives: To carry out an active surveillance of common events on 9-to 26-year-old women receiving human papillomavirus vaccine (HPV) in Italy. The surveillance of HPV vaccination is included in the Pharmacovigilance Multiregional Programs funded by AIFA (Italian Medicines Agency).
Methods: There are two human papillomavirus vaccines, Gardasil and Cervarix, available in Italy since 2008. The HPV vaccine is offered free of charge by Local Health Units (LHU) and an active programme is aimed at immunizing all female adolescents in the twelfth year of life. Some Regions have extended the HPV vaccine offer to other cohorts, either free of charge or with a limited co-payment. The study population is represented by all the women who received the HPV in a LHU and gave their consent to participation. Common adverse events occurring in two weeks following each dose administration were collected by vaccinated woman using a structured diary. An ad hoc web platform was available to enter data at regional level.
Results: The surveillance involves 33 LHUs in 9 Italian Regions. From July 2009 to June 2011, 10785 immunised women (8332 receiving Cervarix and 2453 Gardasil), were included in the surveillance for a total of 23740 administered doses. 38% of women concluded the vaccination cycle, 66% with Gardasil and 30% with Cervarix. Out of 14732 doses 9061 adverse events were reported. The vast majority consisted of swelling at the injection site, headache, nausea, fainting and pain. The vaccination cycle was interrupted by 33 women (0.1%): 16 for refusing, 3 for changing residence, and 11 for adverse reactions (3 of whom required the hospitalization).
Conclusions: The surveillance is still ongoing and final results will be available by the end of 2011. The high proportion of adverse events reported is mainly due to the design of the study; however the majority of the events were mild and transient.[1] The low number of vaccinated women included in the study could be partly explained by the voluntary participation of the Regions. As for all vaccines, and in particular for newly marketed ones, the surveillance of adverse events represents an essential step in the evaluation of a vaccination programme.[2]
OP08. Adverse Events of Special Interest and Pneumococcal Vaccination
C. Santuccio,1 F. Menniti Ippolito,2 L.Tartaglia,1 R. Da Cas,2 F. Trotta 1 and G. Traversa 2
1 Italian Medicines Agency, Pharmacovigilance Unit, Rome, Italy; 2 National Institute of Health, Pharmacoepidemiology Unit, Rome, Italy
Background: In Italy the childhood immunization programs include the pneumococcal vaccination, commonly co-administered with other vaccines. The vaccine mostly used was the pneumococcal 7-valent vaccine, that has been replaced in 2010 by the pneumococcal 13-valent.[1,2] Since 1999 an active surveillance focusing on the role of drugs and vaccines in the occurrence of specific clinical conditions responsible for the hospitalisation of paediatric patients has been conducted in Italy.
Objective: To estimate the risks of occurrence of adverse events of special interest (AESI) in children who received pneumococcal vaccination.
Methods: The study population consisted of all children admitted through the Emergency Departments of nine clinical centres regardless of drug and vaccine use, for the following conditions: endoscopically confirmed gastroduodenal lesions; neurological disorders; non infectious muco-cutaneous diseases and vasculitis; thrombocytopenia. Data were collected through an interview to the parents using a structured questionnaire during hospital admission of the child. For the assessment of safety, drug (or vaccine) exposure, in a time period of three (or twelve) weeks prior to the onset of symptoms that had caused the hospital admission was collected. A case-control analysis was conducted to estimate the risk of occurrence of AESI in children vaccinated with pneumococcal vaccine (with and without the concomitant administration of other vaccines). Hospitalizations for AESI represented the case series and gastrointestinal lesions the control group.
Results: From November 2009 to April 2011 we included in the study 1057 children (mean age 5 years). Among these, 61 (6%) were vaccinated with pneumococcal vaccine (mean age 8 months). In only 5 children (8%) no other vaccines had been administered, whereas a concomitant administration of either a hexavalent vaccine, or of other vaccines, was respectively reported in 42 (69%) and 14 (23%) children. In 19 children an episode of AESI occurred in a compatible time window at risk. In particular, we observed 5 disturbances of vigilance and consciousness (e.g., numbness, somnolence, lipothymia), 3 afebrile convulsions, 2 episodes of Apparent Life Threatening Events, 2 thrombocytopenia, 1 vasculitis and 1 encephalitis.
The OR of AESI associated with concomitant administration of pneumococcal and hexavalent vaccines was 2.5 (0.7–9.2). The OR of AESI among children who only received the hexavalent vaccine was 1.6 (0.7–3.7).
Conclusions: The estimated risk of AESI (especially neurological ones) associated with pneumococcal vaccination, when co-administered with hexavalent products, was higher than that estimated for hexavalent vaccine alone. Other evidence needs to be collected to confirm the results.
OP09. Pilot Swine Flu Vaccination Active Surveillance Study: Final Results
D. Layton,1 M. Dryburgh,2 T.M. MacDonald,2 S.A. Shakir 1 and I.S. MacKenzie 2
1 Drug Safety Research Unit, Southampton, UK; School of Pharmacy and Biomedical Sciences, University of Portsmouth, Portsmouth, UK; 2 Medicines Monitoring Unit, University of Dundee, Dundee, UK
Background: Immediately following start of the H1N1 influenza A (swine flu) UK vaccination programme (21/10/2009), a pilot study based in Scotland was initiated to examine the feasibility of using modern technology (email, text, online forms) to capture vaccine utilisation and patient self-reported events and sequelae over 12 month period for purposes of near ‘real-time’ post-marketing systematic active surveillance of eligible H1N1 influenza A (swine flu) vaccinees.
Objectives: To examine study participation rates, patient characteristics and types of events reported in this pilot study.
Methods: A prospective observational cohort study (start date 2/11/2009). Voluntary enrolment was generated via adverts in vaccination centres and a bespoke website; consent allowed follow-up and investigation of serious adverse events (SAEs) requiring emergency treatment or resulting in hospitalization (primary outcome). Modern technology collected exposure, outcome and covariate data. Descriptive statistics and crude Odds Ratios (95% CI) are presented.
Results: Valid cohort at study end (4/2/2010) comprised 4053 patients (mean age 53.4 yrs (SD 17.5); 57.1% (n = 2315) female. 3743 (92.4%) were vaccinated (mean time to vaccine uptake 58.4 days (SD 16.2)). Vaccinees were more likely to be: female [OR 1.6 (1.2, 2.0); health professionals [OR 2.0 (1.3, 3.2)], received another vaccine in 3 months prior [1.6 (1.2, 2.0)]; or have medical conditions other than those initially targeted [OR (1.8(1.2, 3.0)]. There were 273 self reported events of which 53 (19.4%) met the protocol SAE definition; 6 were assessed as possibly related. None of 7 deaths reported were attributed to the vaccine. Of 130 pregnancies reported during the study period, 92 (70.8%) were pregnant at vaccination. There were 4 miscarriages and six infants had potentially congenital problems.
Conclusions: This pilot study demonstrates that the application of modern technology is successful, can reduce costs and improve quality of patient-reported data. The method for near ‘real-time’ monitoring, with minimal additional workload for healthcare staff should be considered as additional pharmacovigilance tools for other safety studies.
Pharmacovigilance in Public Health Programmes
OP10. Workshops and Telephone-Based Interventions to Improve ADR Reporting: A Cluster-Randomized Trial in Portugal
T.F. Herdeiro,1 I.R. Vaz,2 M.A. Ferreira,3 J.J. Polonia 2 and A.G. Figueiras 4
1 Unidade de Farmacovigilancia Norte, Faculdade de Medicina, Universidade do Porto; Centro de Investigaçao em Tecnologias da Saude, CITS, Portugal; 2 Unidade de Farmacovigilancia Norte, Faculdade de Medicina, Universidade do Porto; 3 Centro de Biologia Celular, Universidade de Aveiro, Portugal; 4 CIBER em Epidemiologia e Saude Publica (CIBERESP), Espanha
Objectives: Adverse drug reactions (ADRs) are a significant health problem, being one of the major causes of morbidity and mortality in the developed countries. However, it is estimated that only 6% of all reactions are reported.[1] The causes associated with the under-reporting behavior among physicians have been extensively described.[2,3] Continuing medical educations have been used to improve physician’s attitudes and knowledge concerning to spontaneous reporting.[4,5] The present study aimed to evaluates the results of an intervention by workshops/telephone interview in physicians, designed to improve the effectiveness and relevance of adverse drug reactions reports.
Methods: A cluster-randomized controlled trial was conducted with 6579 physicians working in Northern Portugal. After randomization, 1472 physicians were placed into the intervention group (1034 in telephone interviews and 438 in workshops), while the control group was comprised of 5107 physicians. Statistical analysis was performed, based on the intention-to-treat, and generalized of linear mixed models were applied, using the penalized quasi-likelihood method. The physicians studied were followed during 20 month period.
Results: The participation rate was 26.9% and 7.9% for the workshops and telephone intervention, respectively. In the 20 months after the workshop intervention, an significant increase (p ≤ 0.001) in the ADRs spontaneous reporting rate, when compared to the control group, by approximately four-fold (RR = 3.97; 95% CI: 3.86, 4.08). Conversely, the intervention by telephone interviews was less efficient, since no significant difference (p = 0.052) was observed in the reporting of adverse reactions (RR = 1.02; 95% CI: 1.00, 1.04) when compared with control group.
Conclusions: The strategies implemented in our educative intervention by workshops increased significantly the quantity and relevance of ADRs spontaneous reporting by physicians, but the telephone interventions were less effective. However, the effectiveness of those interventions is significant during a limited period of time. Educational strategies based on workshops, clinical practice cases, could be a fine model to reinforce the ADRs reporting.
OP11. Patient Reporting of Adverse Drug Reactions: First Italian Experience
S. Opri,1 P. D’incau,1 L. Magro,1 L. Sottosanti,2 D. Costantini, S. Potenza,2 L. Catalano,2 F. Ferrazin 2 and R. Leone 1
1 Pharmacology Unit and Pharmacovigilance Centre of Veneto Region, University Hospital of Verona, Verona, Italy; 2 Italian Medicines Agency, Pharmacovigilance Office, Rome, Italy
Background: In recent years there has been a growing interest in the role of patient as potential reporters of adverse drug reactions (ADRs).[1,2] To date, the major nations actively involved in promoting ADRs reporting by consumers are Sweden, USA, UK, Australia, Canada, Denmark, and the Netherlands. In Italy patients’ reporting has been introduced for the first time in 1991. From 2001 to 2009 only 206 patient reports have been detected in the Italian Pharmacovigilance Database.[3]
Aim: The main objective of the present study was to promote and evaluate the quality of patient reports of ADRs. The secondary objective was to evaluate the feasibility of community pharmacies as a place to promote patients’ reporting of ADRs.
Methods: The study was conducted in the Veneto region and involved 192 pharmacists working in 118 pharmacies open to the public, evenly dispersed across the region. The pharmacists were invited to participate by their association (Federfarma).
Each pharmacist was asked to select randomly around 250 patients, older than 18 years, living in Italy and who took at least one drug in the last month before the selection day.
This research has been developed within a continuing pharmacist education activity.
Results: In the four months of the study 46794 patients (28962 women and 17832 men) were selected by pharmacists. Of these, 4459 (9.5%) referred to have had an ADR. Women were most involved in ADRs than men (10.7% vs 7.5%). The 52% (n = 2312) of patients with ADRs filled the “citizen’s reporting form”. Women showed a greater propensity to fill the card than men (52% vs 46%). Overall the reports were of good quality. The drugs most reported were NSAIDs and antibacterial agents, followed by analgesics (i.e. acetaminophen) and drugs for cholesterol or high blood pressure.
A comparison between the patient reports and physician reports, sent during the study period, was made. We found no particular differences in the involved drugs, however patients reported more frequently gastrointestinal tract reactions and less frequently skin reactions than physicians.
Conclusion: To our knowledge, this is the first Italian study which involved directly patients in the pharmacovigilance. Our results confirm the relevance of this source and that community pharmacies represented a feasible service for promoting patient ADRs reporting. The Italian Medicines Agency will promote specific programs to involve the patients in the reporting system.
Cost-Effectiveness of Pharmacovigilance Systems
OP12. Cost Approach to Iatrogenic Drug
H. Filali
Department of Pharmacology, University Hospital Ibn Rochd, Casablanca, Morocco
The consequences of iatrogenic effects in terms of public health are important given the frequency of the problem, its impact in terms of morbidity, functional decline and mortality as well as economic and social repercussions.
Our study was conducted to quantify the overhead of the management of iatrogenic drug within the CHU Bnou Rushd, identify predisposing factors and therapeutic classes implicated in order to make suggestions for prevention, warning and advice on good prescribing practices. We can thus reduce costs in terms of preventable iatrogenic drug.
The notification was requested through our collection of adverse events of various departments of the CHU Bnou Rushd, with sheets of reporting side effects, including a section for estimating the cost of treatment effect. Only the direct cost was calculated (cost of hospitalization or prolongation of hospitalization, diagnostic tests, corrective treatment…)
The overall average cost of 182 cases collected during the study period (eight months) was about 2534 Euros. This cost is largely underestimated at first by a problem of under reporting of adverse events by health professionals, and a lack of support for these side effects whatsoever in terms of diagnosis and monitoring.
The liver alone have generated an average cost for their care of about 12236 Euros, followed by skin conditions that exceed the frequency of occurrence 30% and the cost of which reached 5589 and over 3000 Euros for each EIM neurological and haematological.
The predisposing factors were the iatrogenic multiple drug prescription, the multiple illnesses (cardiovascular failures, real and/or liver) and misuse.
Therapeutic classes account for more than iatrogenic cost are: antibiotics, antineoplastics, corticosteroids, antipsychotics…
A reconciliation of the reality of the impact of the extra cost and no side effects requires an awareness of health professionals in the interest of the reporting of adverse events or misuse, and collaboration with the Pharmacovigilance Unit to prevent preventable cases and reduce unnecessary expenditures.
Communication in Drug Safety
OP13. Utilisation of Fentanyl Buccal Tablets in Primary Care in England: Focus on ‘Off Label’ Use in Support of Risk Management
V. Osborne, D. Layton, M. Al Shukri, C. Fogg and S. Shakir
Drug Safety Research Unit, Southampton, UK; School of Pharmacy and Biomedical Sciences, University of Portsmouth, Portsmouth, UK
Background: Fentanyl citrate buccal tablets (Effentora®; Cephalon) are indicated for the treatment of Breakthrough Pain (BTP) in cancer, in adults who are receiving maintenance opioid therapy for chronic cancer pain. This study was conducted as part of the risk management plan of the product.
Objectives: Objective: To describe the utilisation characteristics of patients prescribed fentanyl buccal, based on an analysis of an interim Modified Prescription-Event Monitoring (M-PEM) cohort, and to assess how the product is being used in relation to terms of license of marketing approval as defined in the Summary of Product Characteristics (SmPC) at time of study.[1]
Methods: An observational cohort post-marketing surveillance study was conducted. For the interim analysis of the ongoing M-PEM study, exposure data were collected from dispensed prescriptions issued by general practitioners (GPs) between March 2009 and October 2010 (interim data lock point). Outcome data (indication, event, patient demographic and selected clinical characteristics) were collected by sending questionnaires to GPs at least 6 months after the drug was first prescribed for an individual patient. Summary descriptive statistics were calculated.
Results: The interim cohort consisted of 236 patients, of which 51.7% (n = 122 patients) were reported to be female. Where age was specified, the median age for the cohort was 63 years (IQR: 55–73 years). There was no use reported in patients aged under 18 years. Where specified, primary indications other than BTP were reported for 29.4% (60/204) patients including ‘osteoarthritis’ (n = 2) and ‘osteoarthritis hip’ (n = 2). Regular opioid therapy was reported upon starting treatment for only 162 patients (68.6% of cohort), though fentanyl buccal is contraindicated in patients who are opioid naïve or without maintenance therapy. In total 23 patients (9.7%) had one or more contraindications for use, including 9 patients who had COPD (3.8%). Where specified (n = 178) the most frequent initial titration dose was 100 mcg (n = 108) which is in line with prescribing recommendations for treatment initiation.
Conclusions: This study has highlighted that some clinicians are prescribing this product outside the recommended terms of the licence, though the majority appear to be adhering to the prescribing recommendations. Drug utilisation studies are important in describing populations that may not have been adequately studied in terms of risk in pre-marketing development programmes and these are important in the post-marketing risk management of medicines. These interim results using raw data will be subject to modification when final analysis is completed.
OP14. Room for Improvement in Safety Learning of Same Class Drugs
G. Stefansdottir,1 M.J. Knol,1 H.G. Leufkens,2 A.H. Arnardottir,3 D.E. Grobbee 1 and M.L. De Bruin 2
1 Julius Center for Health Sciences and Primary Care, University Medical Center Utrecht, Utrecht, the Netherlands; 2 Division of Pharmacoepidemiology and Clinical Pharmacology, Utrecht Institute for Pharmaceutical Sciences, Utrecht, Netherlands; 3 Department of Clinical Pharmacology, University Medical Center Groningen, University of Groningen, The Netherlands
Background: Incomplete safety knowledge at market approval makes careful safety monitoring during the post-marketing phase necessary, to this end knowledge about a same class drug can be useful.
Objectives: The aim of this study was to see whether learning occurs between same class drugs, in the context of pro-active risk management. We expected increased learning for Type A compared to Type B adverse drug reactions (ADRs).
Methods: Study population contained all drugs classes where first and second drug were centrally registered in the European Union from 1995 to 2008. A list of all registered drugs can be found on the website of the European commission.[1] Their post marketing phase was followed from marketing until September 2010, with maximum follow-up of 10 years, to identify new ADRs in the summary of product characteristics (SPC). We studied the association between type of ADR (Type A vs Type B) and learning from the first in class drug by comparing the proportion of ADRs that appeared in first SPC of second drug in class (immediate learning). For those ADRs without immediate learning we studied the time to appearance in subsequent SPCs as a measure for post-marketing learning. Multivariate models were used to adjust for number of same rapporteurs, year of marketing, exposed patients and time between marketing of first and second in class.
Results: We identified 995 ADRs from 19 drug pairs. Immediate learning occurred for 228 ADRs, post-marketing learning for 162 ADRs and absence of learning was noted for 605 ADRs. Type A ADR, longer lag time and sharing a regulator country were associated with any type of learning compared to absence of learning. Shorter lag time and sharing a regulator country was associated with post-marketing learning compared to immediate learning. Type A ADRs (HR 1.64, p 0.01), and sharing a regulator country (1.96, p < 0.001) were associated with a shorter time to learning during the post-marketing phase. Yet, sharing both regulator countries did not show a significant association with time to learning.
Conclusions: There are opportunities for improvement in the learning process in order to increase pro-active risk management. To this end, a complete picture of expected ADRS (Type A) and increased collaboration between regulators are useful.
Medication Errors and Preventability
OP15. Preventable Hospitalisations to Departments of Internal Medicine
S. Schmiedl,1 M. Rottenkolber,2 J. Szymanski,1 B. Drewelow,3 S. Müller,3 A. Zachow,3 W. Siegmund,4 K. Saljé,4 M. Arnold,4 M. Hippius,5 A. Scheuerlein,5 K. Farker,6 J. Hasford 2 and P. Thürmann 1
1 Philipp-Klee Institute of Clinical Pharmacology, HELIOS Clinic Wuppertal, Germany; Department of Medicine, Faculty of Health, University Witten/Herdecke, Germany; 2 Institute for Medical Information Sciences, Biometry, and Epidemiology, Ludwig-Maximilians-University Muenchen, Munich, Germany; 3 Regional Pharmacovigilance Center Rostock, Institute of Clinical Pharmacology, University of Rostock, Germany; 4 Regional Pharmacovigilance Center Greifswald, Institute of Clinical Pharmacology, University of Greifswald, Germany 5 Regional Pharmacovigilance Center Jena, Institute of Pharmacology and Toxicology, Department of Clinical Pharmacology, University of Jena, Germany; 6 Regional Pharmacovigilance Center Weimar, Institute of Pharmacology and Toxicology, Department of Clinical Pharmacology, University of Jena, Germany
Objectives: Studies focusing on preventable adverse drug reactions (ADR) leading to hospitalisation differ due to e.g. departments under observation, mode of detection and the preventability algorithm applied. Within the German Net of Regional Pharmacovigilance Centers (NRPC), ADR-related hospital admissions were assessed since 1997 in 4 university or academic teaching hospitals with a catchment area of approximately 500000 inhabitants. We aimed to analyse and compare characteristics of preventable and non-preventable ADR-associated hospitalisations.
Methods: Patients admitted to departments of internal medicine of the 4 NRPC hospitals were continuously and comprehensively assessed for presence of ADR leading to hospitalisation. Data concerning patient history and comorbidity, prescription and description of the ADR were collected and standardised causality assessment according to Begaud was performed. Preventability of ADR was assessed according to a standardized algorithm comprising 12 items. All data underwent quality assurance before they were reported to the national authority (BfArM). Patients with an at least ‘possible’ ADR (I2) admitted to hospital between 01/2000 and 06/2008 were included in this analysis.
Results: Out of 6427 ADR-affected patients with a total of 6906 ADR, 1358 ADR (19.7%) in 1253 (19.5%) patients were assessed as preventable. Patients with preventable ADR were significantly older (72.6 ± 14.2 yrs. vs 69.7 ± 15.9 yrs., p < 0.0001) and more likely to be of female gender 62.7% versus 59.3% (p = 0.0317). The most frequent preventable ADR and respective causative agents were gastrointestinal disorders (31.2% of all preventable ADR, e.g. bleeding, ulcer) caused by antithrombotics and NSAID, metabolic disorders (30.0%, e.g. hypoglycaemia, electrolyte disorders caused by antidiabetics and diuretics, respectively). Out of all preventable ADR, 1163 (85.6%) recovered completely compared to a respective rate of 81.6% for non-preventable ADR (p < 0.0004). Relevant drug-drug interactions, prescription of inappropriate drugs and non-adjusted drug dosages were present in 554 (44.2%), 267 (21.3%) and 218 (17.4%) of patients with preventable ADR (multiple answers possible). Lack of ADR prevention strategies (non-drug and drug-related) were revealed in 354 (28.3%) and 212 (16.9%), respectively.
Conclusions: In a large prospective observational study, almost one fifth of all ADR leading to hospitalisation were assessed as preventable and were mainly caused by well-known dose dependent type A ADR. Strategies focusing on safer prescribing (e.g. age-related dosing, adherence to warnings and compliance to guidelines) could be efficient in preventing drug related hospital admissions and re-admissions (supported by BfArM FoNr: V-11337/68605/2011).
OP16. Evaluating Visual Strategies to Differentiate Look-Alike Medication Names During the Medication Administration Process
S. Gabriele,1 S. Hyland,2 L.L. Gosbee,3 M. Singh,4 A. Ninan,5 R. Evans,6 O. Fernandes 7 and J. Hart 7
1 Department of Design, York University, Toronto, Canada 2 Institute for Safe Medication Practices Canada, Toronto, Canada; 3 Red Forest Consulting, Ann Arbor, MI, USA; 4 School of Nursing, York University, Toronto, ON, Canada; 5 Child Parent Resource Institute; University of Western Ontario, London, ON, Canada; 6 Child Parent Resource Institute, London, ON, Canada; 7 University Health Network, Toronto, ON, Canada
Objectives: Tallman lettering is currently recommended to help mitigate errors due to the potential confusion between look-alike medication names.[1] While there is some evidence of tallman lettering effectiveness, there is little research thus far on whether this strategy is effective in the context of the medication administration process in hospitals.
This study was designed to evaluate tallman lettering and alternative typographic strategies (lowercase, bold, black rectangle with white lettering.) The inclusion of both the generic and brand names were also evaluated. Results of this research are intended to examine current recommendations and to contribute to the design of paper and electronic applications where a look-alike name is present.
Methods: A group of 128 hospital nurses and 14 hospital pharmacists participated in three experiments and completed a short questionnaire. In the experiments, researchers recorded reaction time and accuracy in the selection of medications. Two of the experiments involved participants identifying look-alike names on a laptop display, either examining side-by-side medication names, or selecting from a list of medications on the screen of an automated dispensing machine. In the third experiment, participants were asked to manually select medications from shelves.
Results: Overall, as the tasks increased in complexity/realism, error rates decreased and time to respond increased. Researchers found the use of tallman lettering was not as effective as using other typographic alternatives. Other typographic strategies were more effective, depending on the task and the medium on which the name was displayed (paper vs computer). Additionally, the incorporation of both the generic and brand names in comparison to the inclusion of the generic name only, generated longer reaction times and more errors in the combined experiments. In individual experiments, reaction times were also longer but error rates were lower in two of the three experiments.
Conclusions: Our results suggest that tallman letters may not be as effective as previously reported. Because uppercase characters are less distinct in their design than their lowercase counterparts, they may not provide sufficient cues necessary to distinguish two look-alike medication names.[2] The mixed results with the alternatives to tallman lettering suggest more investigation is required to understand how the method of differentiation, the tasks, the amount of information displayed, and the medium affect the recognition and selection of look-alike medications.
OP17. Adverse Reactions after Medication Error Occurred in Children and Reported to the National Pharmacovigilance Network
C. Santuccio, D. Morlino, L. Tartaglia, F. Trotta and F. Ferrazin
Italian Medicines Agency, Pharmacovigilance Unit, Italy
Introduction: In Italy ADR reports are collected through the National Pharmacovigilance Network (NPN). A medication error (ME) could lead to an ADR; this could be increased in pediatrics due to the limited availability of drugs with specific formulation and dosage.[1] In order to identify the reactions due to a ME a specific field was introduced in the web system in September 2009 to be selected during the data entry according to the reported information on the cases.
Objectives: To describe cases of ADRs occurred in children reported as a ME.
Methods: The paediatric (0–17 years) spontaneous reports loaded in the NPN from September 2009 and May 2011 were searched selecting the field for ME; a supplementary search using the HLGT of Med-DRA “medication error” was performed. Each case was analyzed by type of error, drug and reaction.
Results: During the period of interest, 103 ADR reports due to a ME in children were identified, corresponding to about 25% of ME cases reported in the NPN. In particular 81 out of 103 cases were retrieved through the specific field for ME, while the remaining 22 through the search of the MedDRA’s HLGT; in the last case the reports mostly concerned accidental drug exposures.
With regard to the 81 cases of ME, the majority were serious (64%); in all but four cases (for which the outcome was not available) the ADR was resolved or improved.
The highest number of ADR reported as a ME involved drugs active on nervous system (ATC N); firstly paracetamol in the youngest children, followed by risperidone in teenagers. The second drug class involved was respiratory drugs (ATC R) especially oxatomide, salbutamol (alone or in association) and finally drugs for cough. Small numbers of reports were received after the administration of other drug classes. Since the majority of MEs concerned a dosage error, the observed ADR were often (expected) reactions due to overdosage exposure. For example following a ME with oxatomide there were neurological reactions, but also QT prolongation; following salbutamol the most frequently reported reactions were agitation and tachycardia.
Conclusions: Reporting a ME in children is essential to identify drugs most frequently associated with errors for which a regulatory action could be implemented in order to prevent ME itself, thus increasing drug safety in children.
OP18. Medication Errors Prevention Strategies: Examples of Partnerships
G. Benabdallah, R. Benkirane, A. Khattabi and R. Soulaymani
Moroccan Poison Control and Pharmacovigilance Centre
Background: There is a need to define exactly a partnership, to identify parties of partnerships and main goals of partnerships leading to implement Medication Errors (MEs) prevention strategies.
Main goals of partnerships: First do no harm, decrease MEs, prevent MEs and increase patient safety.
To achieve these goals, we need the collaboration of all concerned parties and need to build efficient partnership.
There are four levels of partnerships, all committed to patient safety.
The first level is represented by Pharmacovigilance Centres (PVCs), Poison Control Centres (PCCs) and Patient Safety Organizations (PSOs). They are partnering to have an overview of all MEs, to detect earlier MEs, to generate signals earlier and to standardize practices.
The second level is represented by patients and Health Care Professionals (HCP). Partnership could not be efficient without the involvement of levels 1 and 2 together, to notify Adverse Drug Reactions (ADRs) and MEs to level 1, and to inform, train, sensitize, educate and prevent on ME to level 2.
The third level is represented by Academia, Professional Organizations, Consumer Organizations and the Media. Partnering of level 1 with level 2 could not be efficient without the collaboration of level 3, to promote, to teach and train HCP to the concept of patient safety, and to educate patients on the importance of patient engagement in preventing MEs. Partnering with Medias is essential to promote, sensitize, strengthen and foster patient safety concept.
The fourth level is represented by Drug Regulatory Authority, Marketing Authorization Holders and Hospitals. Partnering with level 4 is essential to put in place preventive actions decided by level 1, leading to prevent recurrence of ME.
Conclusion: Collaboration between these four levels of partnerships together is the key element leading to prevent MEs. To achieve these goals, there is a need to put in place partnership between PCCs and PSO with sensitization of their HCP to the importance of such collaboration. There is a need to put in place partnership between PVCs, PCCs, PSOs and Medical and Pharmacy school to focus on teaching and training in clinical pharmacology, to focus on teaching and training practical prescribing principles for undergraduate and postgraduate’s students, and there is a need to get confidence of medias.
OP19. A Multicentric Study on Adverse Drug Reactions Preventability
R. Benkirane,1 L. Alj,1 G. Benabdallah,1 H. Sefiani,1 S. Pal,2 S. Olsson 3 and R. Soulaymani 1
1 Moroccan Pharmacovigilance Centre. Rabat, Morocco 2 World Health Organization. Geneva, Switzerland; 3 Uppsala Monitoring Centre. Uppsala, Sweden
Objectives: Over the years, pharmacovigilance centres have found that many Adverse Drug Reactions (ADR) described in case safety reports may be due to medication errors. The estimated rate of preventable ADRs reported in the literature varies from 18.7 to 80%.[1] Pharmacovigilance centres are recommended by the world health organization to expand their role and scope to identify, analyze and prevent medication errors, to improve patient safety.
For that purpose, they should develop a toolkit to identify potentially preventable ADRs among the spontaneous reports of ADRs collected. More broadly, a method needs to be developed for the identification of preventable drug related problems.
The objective of this work is to validate a method developed by Moroccan Pharmacovigilance Centre to detect preventable ADR.
Methods: The method approach is based on the identification of any risk factor that increases the likelihood of ADR occurrence. These risk factors have been selected according to professional practice, ADR mechanisms, patient’s attitude and quality of drug. These risk factors constitute the preventability criteria that should be used to assess ADR preventability.
For that purpose, 242 ADR were collected from 11 national pharmacovigilance centres. The cases were sent to these national centres to assess their preventability using the developed method. Analysis of cases will be done at least with 2 persons from pharmacovigilance staff but only one answer per case will be send.
Results: Analysis of preventability of ADRs is in progress.
Conclusions: Developing a preventability method is an opportunity for pharmacovigilance centres to contribute to the detection and prevention of medication errors and thus lead pharmacovigilance to play its important role in patient safety.
OP20. Dose Omissions in Hospitalised Patients: An Analysis of the Relative Contribution of Adverse Drug Reactions
J.J. Coleman,1 S.E. McDowell,2 D. Westwood 2 and R.E. Ferner 3
1 College of Medical and Dental Sciences, University of Birmingham, Birmingham, UK; University Hospitals Birmingham NHS Foundation Trust, Edgbaston, Birmingham, UK; 2 University Hospitals Birmingham NHS Foundation Trust, Edgbaston, Birmingham, UK; 3 College of Medical and Dental Sciences, University of Birmingham, Birmingham, UK; West Midlands Centre for Adverse Drug Reactions, City Hospital, Birmingham, UK
Omission of charted (prescribed) medicines for hospitalised patients is an important problem in the United Kingdom.[1] Inappropriate dose omissions can clearly cause harm due to lack of therapeutic effect. However, healthcare professionals administering medicines may decide that non-administration of doses is appropriate in certain circumstances (e.g. when patients show symptoms or signs of possible adverse drug reactions (ADRs)).[2] We wished to study the relative contribution of ADRs to the rate of dose omissions in hospital.
Using a hospital-wide electronic prescribing system we extracted data on 6.28 million drug administrations during 2010. We randomly selected four seven-day periods, concentrating on 470000 doses, of which 19.2% were charted but not given. We analyzed both hard-coded and free text reasons — which were coded by hand — to establish the contribution of different patient, pharmacy, environmental and other factors including ADRs to the total rate of dose omission. We constructed an Ishikawa (fishbone) diagram to illustrate these factors and present the relative contributions of each factor.
While reducing drug omissions is a desirable aim, omission may in some circumstances be rational. Electronic medication administration records allowed us to analyze the reasons for dose omission in detail. Our analysis confirms that, while many dose omissions are undesirable, some are rational and contribute to patient safety.
Post -Authorisation Safety Studies (PASS)
OP21. NSAID Exposure and Risk of Acute Liver Failure Leading to Transplantation: Principal Results of the 7 -Country Case -Population Study (SALT)
E. Gulmez,1 S. Lignot,1 D. Larrey,2 C. DeVries,3 S. Perez Gutthann,4 J. Montastruc,5 M. Sturkenboom,6 J. Bénichou,7 G. Velo,8 A. Caputi,9 F. Salvo,9 F. Hamoud,1 S. Micon,1 R. Lassalle,1 J. Jové,1 G. Pageaux,2 Y. Horsmans,10 J. Bernuau,11 F. Bissoli,12 B. Stricker,6 D. Thorburn,13 A. Gatta,14 E. Monteiro,15 I. Vafiadis,16 A. McCormick,17 H. Metselaar,18 E. Sen,18 A. Nightingale,3 P. Blin 1 and N. Moore 1
1 Pharmacology, Université Bordeaux Segalen, INSERM U657, Bordeaux, France; 2 Hepatogastroenterology, CHU Hôpital Saint-Eloi, Montpellier, France; 3 Pharmacy and Pharmacology, University of Bath, Bath, UK; 4 RTI Health Solutions, Barcelona, Spain; 5 Pharmacologie Clinique, CHU de Toulouse, Toulouse, France; 6 Epidemiology, Erasmus University MC, Rotterdam, Netherlands; 7 Biostatistique, CHU de Rouen, INSERM U657, Rouen, France; 8 Policlinico Borgo Roma, University of Verona, Verona, Italy; 9 Clinical & Experimental Medicine & Pharmacology, Policlinico Universitario, Messina, Italy; 10Gastroenterology, Louvain Catholic University, Louvain, Belgium; 11Liver Unit, Beaujon Hospital, Clichy, France; 12Internal Medicine and Cardiology, Clinica San Gaudenzio, Novara, Italy; 13Liver Unit, Royal Free NHS Trust, London, UK; 14Clinical & Experimental Medicine, Padua University Hospital, Padua, Italy; 15Gastroenterology & Hepatology, Santa Maria Hospital, Lisbon, Portugal; 16Hepatogastroenterology, Athens University School of Medicine, Laiko General Hospital, Athens, Greece; 17Liver Transplant Unit, St. Vincent’s University Hospital, Dublin, Ireland; 18Gastroenterology & Hepatology, Erasmus University MC, Rotterdam, Netherlands
Background: Because of a suspected risk of hepatotoxicity with nimesulide, the Committee for Human Medicinal Products (CHMP) of the European Medicines Agency requested the marketing authorization holder to conduct a study of acute liver transplantation in patients exposed to non-steroidal anti-inflammatory drugs (NSAID), in 7 European countries. University Bordeaux Segalen was commissioned to conduct this study.
Objectives: The primary objectives of the study were to estimate the frequency of transplantation-registered NSAID-exposed ALF, and to compare the population incidence rates of liver transplantation after exposure to different NSAIDs in the participating countries.
Methods: Design and settings: Multicenter, multinational retrospective case-population study in France, Italy, Portugal, Greece, Ireland, the Netherlands, the United Kingdom, evaluating a 3-year period (01/01/2005–31/12/2007). Cases: ≥18 years of age at the time of registration on the transplant list, with ALF registered for liver transplantation with exposure to any NSAID within 30 days before initial symptoms of liver disease (index date), resident, and registered to national health care system of countries. Statistical analysis: Per country rates of NSAID-exposed transplantation registered ALF, computed as the ratio of the number of cases identified in the country to the population exposure. Population exposure is measured as defined daily dose, prescribed daily dose, and estimated annual number of patients exposed with 95% confidence intervals (CI).
Results: Fifty-four of the 57 eligible transplant centres accepted to participate, finally 50/57 eligible centres actually contributed data (87.7%). A total of 8824 cases registered for transplantation at the contributing centres, of which 500 were ALF, 241 were exposed to a drug within 30 days prior to index date. Of these, 34 were exposed to 37 NSAID, 123 to drugs other than NSAIDs, and 84 were acute drug intoxications. Event rates per million treatment-years were 4.4 (95% CI 3.0, 6.1) for all NSAIDs pooled, 5.6 (2.4–11.1) for nimesulide (8 cases), 5.8 (2.8–10.6) for ibuprofen (10 cases), 4.5 (1.5–10.4) for diclofenac (5 cases), and 4.7 (1.0–13.6) for ketoprofen (3 cases). Seventy-one of the 157 non-intoxication cases were exposed to paracetamol (9.8; 95% CI 7.7, 12.3), and 83 of the 84 acute drug intoxications.
Conclusion: Acute liver failure leading to an indication for transplantation after exposure to NSAIDs is extremely rare with no obvious differences between NSAIDs. Non-overdose paracetamol-associated liver failure was twice more common.
Perception of Risks and Communication
OP22. Indicators of Dependence and Aberrant Behaviours During Post -Marketing Use of Fentanyl Buccal Tablets: Risk Scores in Support of Risk Management
V. Osborne, D. Layton, M. AlShukri, C. Fogg and S. Shakir Drug Safety Research Unit, Southampton, UK; School of Pharmacy and Biomedical Sciences, University of Portsmouth, Portsmouth, UK
Background: Misuse (in terms of abuse and addiction) of prescription opioids is an important issue and data are needed in order to develop appropriate risk management strategies. As part of a Modified Prescription-Event Monitoring (M-PEM) study of Effentora® (fentanyl citrate buccal tablet; Cephalon), the construction of a risk score is being explored to identify patients at risk of dependence and addiction.
Objectives: To characterise the nature and types of indicators of aberrant behaviour and dependence reported during Effentora® treatment, based on an analysis of an interim M-PEM cohort.
Methods: Interim analysis of ongoing M-PEM observational cohort study. Exposure data collected from dispensed prescriptions issued by general practitioners (GPs) March 2009–October 2010 (interim data lock point). Outcome data (including events, selected clinical characteristics) collected from questionnaires sent to GPs 6+ months after first Effentora® prescription for each patient. Questionnaires requested GPs to report potential risk factors for substance misuse in patients (indicators of dependence/addiction) and aberrant behaviour during treatment (indicators of abuse). Descriptive statistics and simple (non-weighted) risk scores were constructed on aggregate counts for indicators of dependence and aberrant behaviours.
Results: The interim cohort consisted of 236 patients, 51.7% female. The frequencies of factors strongly associated with dependence are: smoking (19.9%, n = 47), alcohol misuse (4.2%, n=10), psychiatric disorders (7.2%, n = 17; eight specified depression) and previous history of substance misuse (1.3%, n = 3; two specified past misuse of heroin). The majority of patients had no past history of factors associated with dependence (n = 176, 74.6%, risk score = 0). In total, 60 (25.4%) patients had a risk score >1; one patient had risk score of 4. The frequencies of aberrant behaviours are: overwhelming focus on opioid related drug issues (0.8%, n = 2); escalating drug use (3.4%, n = 8); unclear aetiology/exaggeration of pain (4.2%, n = 10); opioid withdrawal syndrome and unsanctioned diversion to third parties/accidental exposure during treatment (n = 0). The majority of patients had no aberrant behaviours reported (n = 222, 94.1%, risk score = 0). In total, 14 (6.0%) patients had risk score >1; 4 patients reported to have risk score of 3. Conclusions: The frequency of aberrant behaviours and indicators of dependence was low in this interim cohort, though there were potential risk factors for misuse of Effentora® reported in some patients. Such risk scores could provide useful tools to inform on the post-marketing risk management of such products. However, further development work is needed. These interim results using raw data will be subject to modification when final analysis is completed.
OP23. Which Aspects of New Glucose Lowering Drugs do Different Stakeholders Value? A Qualitative Study
A. Arnardottir,1 F. Haaijer Ruskamp,1 S. Straus,3 S. Piening,1 M. Monster Simons,2 P. De Graeff 1 and P. Mol 1
1 Clinical Pharmacology, University Medical Center Groningen, Groningen, The Netherlands; 2 Dutch Medicines Evaluation Board, The Hague, The Netherlands; 3 Medical Informatics, Erasmus Medical Center, Rotterdam, The Netherlands Regulatory authorities approve a new drug based on clinical trials taking a decision on results obtained on a population level. In daily practice drugs are used by individual patients that may differ from the trial population with different expectations than regulators and health care professionals (HCPs).
Objectives: Identify key values of new drugs to treat type 2 diabetes that are considered important by regulators, HCPs and patients.
Methods: In this qualitative study open interviews are conducted with a purposeful sample of stakeholders in diabetes care; 7 patients, 3 nurse practitioners (NPs), 5 general practitioners (GP), 4 internists and 3 regulators. Interviews last 45–60 minutes, are recorded and transcribed verbatim. A content analysis based on Grounded Theory is performed by two authors. Results: Up to now 20 respondents have been interviewed. Preliminary analyses show that patients find ease of use, avoidance of hypoglycemia and inducement of weight loss important drug characteristics. The patients (n = 6) were more concerned with short-term risks (glycaemic control, adverse events) than long-term risks (cardiovascular, neuropathy. NPs (n = 2) valued ease of use, inducement of weight loss but also long-term prevention of disease-related complications. GPs (n = 5) were conservative and not willing to take risks, preferring long-term experience with a drug. They valued ease of use and weight loss, but the latter through lifestyle change and not drug-induced. Internists (n = 4) considered it important that the drug stops progression of insulin resistance and induces weight loss. Regulators (n = 3) considered hard endpoints, risk of hypoglycemia and gastrointestinal complications important but did not value ease of use much. Slowing disease progression was considered less important than demonstrated HbA1c control.
Conclusions: Different stakeholders value different aspects of drugs for type 2 diabetes treatment. They especially valued the need for demonstrated various long-term effects differently, with the GPs not willing to use drugs that lacked long-term clinical experience. Most respondents agreed drugs should be easy to use and cause few short-term inconveniences. The extent of these differences between stakeholders will be studied in a quantitative survey.
OP24. Patients, Medicines and Perceptions — “Bridging Continents” for Improving Risk Assessment and Communication
P. Bahri
European Medicines Agency, London, UK
Background: For long, pharmacovigilance specialists and patients have felt being on two “continents”, and healthcare professionals have been expected to act as the bridge between specialist knowledge and patient perceptions. The resulting traditional communication model was characterised by providing safety news to healthcare professionals through mass communication tools and educating patients mainly at individual level, aiming at adherence and safe use of medicines. In the meantime however, patients have increasingly evolved from receivers to information seekers and want physicians to listen to their experiences for shared therapeutic decision-making. This development is paralleled by direct patient reporting of adverse reactions and participation of patient organisations in regulatory procedures, where they contribute their valuable views, or perceptions, to evaluations for marketing authorisation and pharmacovigilance.
Objectives: This presentation will explore the concept of perceptions and inspire discussion what role they play in risk assessment and communication.
Methods: Relevant concepts surrounding the term perception have been extracted from the social and psychological literature. Examples of medicine-related concerns with diverging perceptions are available, and the examples of HPV and pandemic influenza vaccines will be reviewed in more depth. Experiences from involving patients in regulatory processes will be provided. In addition, learnings from anthropology and linguistics, as expected to be discussed at an upcoming Birk-beck Conference “The Language of Illness and Pain”, may further help to understand patient perspectives and their adverse reactions reports.
Conclusions and discussion: For engaging in a dialogue with others, specialists gain from understanding that perceptions are formed from beyond the emotional and also apply to themselves. Perception denotes the processing of information, and this happens within a mental model. The mental model corresponds to believes, where knowledge, uncertainties and unknowns get merged. Only when this kind of rationality is met by values — i.e. our morals and personal preferences — and by emotion-based motivation, humans are able to take decisions and actions. As pharmacovigilance specialists we have to understand our own perceptions as much as be open to learn about those of patients, healthcare professionals and the general public. Only “travelling all continents” will enable us to engage in a true dialogue and to understand concerns over the safety of medicines from various perspectives. We then can address them comprehensively in risk assessment and in communication for the safe and effective use of medicines and the well-being of patients.
Paediatric Pharmacovigilance
OP25. Antidepressant Drug Prescribing in Children and Adolescents in Germany
M. Doerks, I. Langner, U. Dittmann, A. Timmer and E. Garbe
Bremen Institute for Prevention Research and Social Medicine, University of Bremen, Bremen, Germany
Background: Intensive off-label use of antidepressant medication in pediatric patients has been reported from the US and other European countries. An increased risk of suicide has been of concern particularly for selective serotonin reuptake inhibitors (SSRI), leading to a warning of the Committee for Medicinal Products for Human Use (CHMP) of the European Medicines Agency (EMA) in April 2005.[1]
Objectives: To characterize prescribing of antidepressant drugs for children and adolescents in Germany in 2004–2006.
Methods: We obtained data from the German Pharmacoepidemiological Research Database (GePaRD) for the years 2004–2006.This database includes more than 14 million insurance members from 4 German health insurances. Prevalence of antidepressant use was assessed. Off-label use of all antidepressant prescribing was considered in relation to age and indication. Logistic regression analysis was used to identify predictors of off-label use.
Results: Of 2599685 children, we identified 9383 who received a total of 26543 antidepressant drug dispensations in the study period. Prevalence of antidepressant drug use (SSRI use) was 1.84 (0.47) per 1000 person-years in 2004, 1.57 (0.45) in 2005 and 1.66 (0.54) in 2006. Of all antidepressant dispensations, 11172 (42.09%) were tricyclic antide-pressants (TCA), 9179 (34.58%) were SSRI, 4371 (16.47%) were drugs of St John’s wort and 1821 (6.86%) were other antidepressants. Of all antidepressant dispensations, 52.2% were prescribed off-label by age and/or indication. When considered separately, 41.63% were prescribed off-label with respect to age and 18.32% with respect to indication. Specialist treatment and female sex increased the risk of getting an antidepressant prescribed off-label with odds ratios of 1.22 (95% CI 1.15 to 1.28) and 1.07 (95% CI 1.02 to 1.13), respectively.
Conclusions: Our study showed considerable off-label use of antidepressants in pediatric patients in Germany. After warning of CHMP, prevalence of SSRI use did not decrease during the study period.
In vitro Fertilisation and Pharmacovigilance
OP26. Use of Ovulation Stimulation (OS) Alone, Intrauterine Insemination (IUI) and Assisted Reproductive Techniques (ART) and the Risk of Multiplicity: The TWINPREG Study
A. Berard,1 O. Sheehy,2 W. Fraser,1 F. Bissonnette,3 S. Tan,4 J. Trasler 4 and P. Monnier 4
1 University of Montreal, Montreal, QC, Canada; 2 CHU Ste-Justine, Montreal, QC, Canada; 3 OVO Fertility Clinic, Montreal, QC, Canada; 4 McGill University, Montreal, QC, Canada
Background: Very little is known about the risk of multiplicity associated with the use of OS alone, without IUI or other ART.
Objectives: We aimed to estimate the risk of multiplicity associated with the use of: OS alone, without IUI or other ART.
Methods: Between 2006–2008, all multiple pregnancies in Quebec were identified by the Régie de l’assurance maladie du Québec (RAMQ), and defined as the study cases. Three singleton pregnancies (controls) were randomly selected among all Quebec pregnancies and matched to each case on maternal age and year of delivery. Cases and controls were contacted by mail to collect information on infertility history, use of OS, IUI, ART, and lifestyles. Data from the questionnaires were linked to their health services utilization data (RAMQ), hospitalization data (MedEcho), and Quebec’s birth data. The risk of multiplicity in all exposure groups were quantified and compared using multi-variate logistic regression models, adjusting for potential confounders.
Results: A total of 4987 women were studied. After adjustment, pregnant women who used oral OS alone and those who used injectable OS were respectively 4.5 times (95% CI 3.1, 6.3), and 11.3 times (95% CI 2.9, 44.1) more at risk of multiplicity than those who spontaneously conceived. OS with IUI and ART were also increasing the risk of multiplicity (p < 0.05).
Conclusions: Although the risk associated with ART can be decreased by implementing Single Embryo Transfer (SET), the risk associated with OS alone or with IUI is directly attributable to the medication taken and much more difficult to prevent.
New Horizons in Pharmacovigilance
OP27. Using Resources for Scientific Driven Pharmacovigilance Switching from Many Product Safety Documents to the Product Safety Master File
G. Furlan
PrimeVigilance, Milan, Italy
Background: Regulators have acknowledged the need of simplifying pharmacovigilance regulations and significant steps have been undertaken to reduce beaurocratic requirements, especially those regarding the reporting of adverse reactions.[1,2] However, the possibility of reducing the number of documents in order to focus on the actual science underpinning drug safety, rather then devolving resources to producing overlapping documents, does not seem to have attracted sufficient attention. The ICH E2C[3] business plan recognizes the overlap between the periodic safety update report (PSUR),[4] the developmental safety update report (DSUR)[5] and the risk management plan (RMP),[6] but states ‘the issue will be re-evaluated once more experience on these documents is gained’.
The subsequent risk therefore is to shift the available resources from the real scope of drug safety (the detection, characterization and minimization of drug risks) to the production of documents.
Objective and Methods: The main scientific topics required by drug safety guidelines and templates have been reviewed in order to analyse where they may differ, to identify the core drug safety activities that need to be undertaken for protecting patient safety and to reduce the number of documents describing the results of these activities to the essential output.
Results: As shown in table I, (where only DSUR, PSUR and RMP are considered) the scientific topics and sources that need to be taken into account in the main regulatory documents greatly overlap. Many of the inter-document differences are substantially formal: the DSUR, for example, requires to separately present the safety issues emerging from different sources and then to perform an overall evaluation of each safety issue. The RMP, instead, requires the production of a detailed description of the safety issues, without separately presenting the evidence deriving from each source. To some extent, however, the different documents require an in depth analysis of different components: the RMP, for example, requires a description of the epidemiology of the indication for which the drug is used and of its risks. This is not specifically required by other documents.
Conclusions: The main pharmacovigilance documents seem to be signal detection reports on the basis of which risk minimization actions are taken. It is proposed to merge all of these documents in a drug safety master file analysing drug safety issues with the evidence and importance. A summary of this document could be periodically provided to regulators, with the whole master file upon request.
OP28. Linking in Safety with Marketing SupportProgrammes
S. Tomczyk,1 D. Lewis 2 and D. Lewis 1
1 Novartis Pharma AG; 2 Faculty of Health and Human Sciences, University of Hertfordshire, UK
Pharmacovigilance within marketing and sales support programmes is a hot topic that has been raised by regulatory inspectors in Europe.
Discussions are ongoing within the European regulatory forum, and within federations representing the pharmaceutical industry. Because the primary objectives of patient support programmes (PSPs) are not primarily related to the safety of medicines it is important for Marketing Authorisation Holders (MAH) to consider their obligations.
There is a lack of harmonisation in the interpretation of the regulations and guidelines in Europe and the US, which further complicates the management of safety data collected from these programmes. A variety of proposals will be presented, including:
-
• A definition of Patient Support Programmes;
-
• Requirement that all company-sponsored PSPs must be subject to contractual agreements between the MAH and the provider of the programme (vendor);
-
• Methods for ensuring the involvement of pharmacovigilance experts in PSPs;
-
• Standardised safety data management for PSPs;
-
• Aspects of expedited and aggregate reporting required for PSPs, including a solution for ensuring compliance with regulatory requirements in the EEA & US;
-
• Options for analyses and presentation of safety data from PSPs.
OP29. Internet Accounts of Survivors of Serious Adverse Drug Reactions: A Study of Experiences of Stevens -Johnson Syndrome and Toxic Epidermal Necrolysis
T.F. Butt,1 A.R. Cox,2 J. Oyebode 3 and R.E. Ferner 4
1 Department of Clinical Pharmacology, School of Clinical and Experimental Medicine, University of Birmingham, UK; 2 Pharmacy Department, School of Clinical and Experimental Medicine, University of Birmingham, UK; 3 Department of Psychology, University of Birmingham, UK, and Birmingham and Solihull Mental Health Foundation Trust, UK; 4 West Midlands Centre for Adverse Drug Reactions, City Hospital, Birmingham, UK
Background: Life-threatening adverse drug reactions (ADRs) such as Stevens Johnson Syndrome (SJS) and Toxic Epidermal Necrolysis (TEN) continue to affect patients’ lives long after the event.[1] Survivors and their relatives can rely heavily on internet sources for support and advice, but narratives of their experiences posted on patient websites have not been previously explored.
Objectives: To analyse internet narratives drug-induced SJS and TEN and consider the reasons for individuals posting on patient websites, and the concerns they reflect.
Methods: We identified personal accounts posted by public users on the internet detailing experiences of drug-induced SJS and TEN from support group websites and blogs, and analysed them using a thematic qualitative approach.
Results: A total of 208 internet postings were analysed. Motivation for posting included a desire to share experiences and to seek advice from others. Patients and their relatives expressed concern that the ADR may be hereditary, worries about effects on fertility, and a fear of recurrence. They also indicated a desire to increase awareness of the harms associated with drugs, and to inform others of the suspected cause of the ADR.
Conclusions: Individuals experiencing SJS or TEN had many unanswered questions and concerns regarding the ADR long after the event. Our findings could guide healthcare professionals in the management of survivors of the ADR, and in communicating more effectively with patients and their relatives. Internet forum postings of patient reports of ADRs provide insight into patient concerns and supplement findings from detailed face-to-face interviews.
Other Topics
OP30. Venous Thromboembolism and Combined Hormonal Contraceptives: Where is the Signal?
P. CaduffJanosa, H.Y. Kwan, D. Pavelic Ferretti and R. Stoller
Swissmedic — Swiss Agency of Therapeutic Products, Berne, Switzerland
The causal association between combined hormonal contraceptives (CHC) and venous thromboembolism (VTE) has been established in the 1970ies particularly with high oestrogen doses.
Spontaneous reports do not allow to calculate the incidence of adverse drug reactions (ADR) nor to compare different products. They can, however, contribute significantly to identify drug utilisation problems and patient risk factors.
The Swiss National Pharmacovigilance Centre at Swissmedic has received a considerable number of reports of VTE over the years and in approximately one third of the reports listing pulmonary embolism as ADR, CHC were the suspected drug, with 10% of these reports describing a fatal outcome.[1] The time elapsed between the first symptoms and the correct diagnosis varied considerably, thus delaying adequate therapy for some of the patients. Half of the deceased women had one or more risk factors for VTE besides CHC intake.
Evidence from recent epidemiological studies[3–5] suggests that CHC containing antiandrogenics, as the 3rd generation CHC, carry an increased risk of VTE compared to CHC of the 2nd generation. Nevertheless, these products are prescribed far more widely than the apparently safer 2nd generation ones.
Recognizing VTE can be tricky and overseeing it is the most frequent diagnostic mistake according to Schiff et al.[2] in their recent analysis of medication errors. Failure to promptly diagnose VTE in young, healthy CHC users and indiscriminate intake of CHC suggests that neither health care professionals nor the public are sufficiently aware of this risk.
The actual signal is therefore this lack of awareness and not the causal relation between CHC and VTE as established over 30 years ago. Health care professionals should take the recent pharmacoepidemiological data into consideration when advising women seeking contraception and when prescribing CHC.
Consumers also should be made aware of the different potential risks of the various CHC to be able to make an informed decision between alternatives and be encouraged to seek immediate professional help if experiencing any symptoms suggesting VTE.
OP31. The Application of Pedagogy to Training in Pharmacovigilance
L. Fram and E. Brown
Elliot Brown Consulting Ltd, UK
In recent years there has been increasing emphasis on the need for effective training and communication in the context of pharmacovigilance and risk management. Training is an essential element of the Quality Management System in pharmaceutical companies[1] and training records and content are subject to regulatory inspection;[2] there have been various initiatives for improving the quality of pharmacovigilance training with development of curricula and courses. In a broader sense, training may also be a component of the education of patients and healthcare professionals in risk management programmes as well as an element of ongoing initiatives to increase reporting of adverse events and other experiences by healthcare professionals and consumers.[3]
In this paper we consider some of the principles of teaching and how these might be used to good effect in training relevant to pharmacovigilance. The training might include, for example: training the trainers; training on SOPs; training company staff at all levels from top management to reception personnel on pharmacovigilance obligations; training those working in pharmacovigilance in companies, regulatory agencies, contract organisations and academia on all aspects of pharmacovigilance — regulatory, scientific and medical; training clinical trial investigators; and training the wider public.
Some of the principles include: understanding the current knowledge of trainees, the objectives of the training and the required end-result; selection of appropriate tools for delivering training; awareness of characteristics and behaviours of the trainees (for example, age increasing the resistance of trainees towards interactive methods; continual questioning by trainees not indicating active learning; limitations of foreign language skills); the advantage of presenting in short sections, use of application by working through an example or problem-solving, consolidation by testing and questions and answers; provocation as a means of developing trainee involvement; trainer improvement by feedback.
The paper will also describe the use of multiple media for delivery of training, some of the limitations of PowerPoint presentations and how these can be overcome, how role-play can be of value in various situations and how these and other methods[4] may aid trainee involvement and imparting of information.
OP32. Study of Reliability of Medicines -Related Information in Internet -Based Health Sources
H. Lebanova, M. Bileva and I. Getov
Department of Social Pharmacy, Faculty of Pharmacy, Medical University-Sofia, Sofia, Bulgaria
Background: The theoretical definition of infovigilance is: “…activity of error or inaccuracy notification in information sources which could be responsible for medication errors”. Information disseminated by medicines information systes is not always easy to apply. Sometimes there is conflicting information in reference books, in journals, or in official sources like regulatory sites.
Nowadays internet provides access to enormous volume and range of information that was previously inaccessible or too poorly organized to be searched easily and friendly.
Objectives: The aim of the study is to assess internet as a source of medicines related information and to create test methodology to evaluate the top 10 visited health-related web-sites in Bulgaria, according to Gemius.
Methods: Using existing methodologies for evaluation of web sources, a new algorithm of three-step approach consisting of score-card validation to assess the drug-related information in the 10 most visited Bulgarian web-sites was created. Results: The preliminary results show that in many cases the medicines information in the internet sites contains errors and discrepancies.
Conclusions: There is a need of monitoring the medicines information available online in order to prevent patient misinformation and confusion that could lead to medication errors. Strict regulatory measures concerning information in global web and its reliability are indispensable.
Discussion: The web-based medicines information sources give the patients a rapid access to drug information. No one edits the vast amount of medicine information on the internet to ensure its quality and accuracy. Some web sites may be accurate while others offer information that only may be advertising, medicine e-marketing or worse harmful. There are obvious disadvantages to the plethora of unregulated web-information. There is a large volume of incorrect and out-of-date data that causes considerable information noise and it is a threat to patients’ safety and rational drug use.
OP33. Treatment of Paediatric Epilepsy in Germany: Antiepileptic Drug Utilisation in Children and Adolescents from 2004–2006
M. Doerks, I. Langner, A. Timmer and E. Garbe
Bremen Institute for Prevention Research and Social Medicine, Bremen, Germany
Objectives: Treatment of paediatric epilepsy has advanced with the development of new antiepileptic drugs (AEDs). Data are lacking for Germany to which extent new AEDs are used in the treatment of childhood epilepsy. To characterise utilisation of antiepileptics in children and adolescents with a specific emphasis on new AEDs.
Methods: Data was obtained from the German Pharmacoepidemiological Research Database for the period 2004–2006. Descriptive analyses were performed to assess prevalence and incidence of AED use stratified by age and sex. Mono- and combination therapy were considered as well as diagnoses and clinical speciality of the prescribing physician.
Results: We identified 13197 children with AED use who received a total of 226856 AED prescriptions. The majority of children treated with an AED were diagnosed with epilepsy (11872; 89.96%). Of all AEDs used, 140992 (62.15%) were conventional and 85864 (37.85%) were new AEDs. One-year prescribing prevalence ranged between 4.10 and 4.11 per 1000 children. Incidence of AED use was 0.91 (95% CI 0.87, 0.95) per 1000 person-years in 2005 and 0.84 (95% CI 0.81, 0.89) per 1000 person-years in 2006. Monotherapy (9 821; 74.42%) was found to be more prevalent than combination therapy. Most anti-epileptics were prescribed by paediatricians (147150; 64.86%).
Conclusions: Conventional AEDs were the most commonly prescribed drugs for treatment of childhood epilepsy in Germany. This is in contrast to international studies in adults where new antiepileptics are reported to have a greater impact on prescribing.[1,2]
OP34. QPPV Training — Just the QPPV?
S.G. Douglas 1,2
1 SGD Consulting Ltd, Director, Albrighton, Shropshire, UK; 2 Primevigilance Ltd, Director, Surrey Technology Centre, Guildford, Surrey, UK
Although the Pharmacovigilance regulations and guidelines refer with certainty to the requirement for a Qualified Person for Pharmacovigilance (QPPV)[1,2] there is no real clarity regarding what ‘qualified’ may mean. Unlike the position of a Good Manufacturing Practice Qualified Person (GMPQP) there are no requirements for the QPPV to follow a specific curriculum or be independently assessed with regard to knowledge or ability.
It appears that at least most QPPVs and Pharmacovigilance practitioners accept that, as detailed in Vol 9A, ‘The QPPV should be appropriately qualified, with documented experience in all aspects of Pharmacovigilance in order to fulfil the responsibilities and tasks of the post.’[1]
Due to the extensive tasks that may fall upon the QPPV plus potentially complex Pharmacovigilance systems it is noted that ‘The QPPV may therefore delegate specific tasks, under supervision, to appropriately qualified and trained individuals’[1]
Additionally, Vol 9A clearly defines the responsibility of the Market Authorisation Holder (MAH):
‘The Marketing Authorisation Holder should adequately support the QPPV and ensure that there are appropriate processes, resources, communication mechanisms and access to all sources of relevant information in place for the fulfilment of the QPPV’s responsibilities and tasks.’[1]
Defining the technical aspects of the QPPV role is probably the most straightforward aspect of the development of a QPPV training curriculum and may include topics such as General PV Awareness, Seriousness & Causality, Signal Detection, Regulatory Inspections & Audits, Quality Management Awareness. The technical roles will depend very much on the size of the company and how directly the QPPV is involved in day to day tasks.
Remembering that the QPPV retains legal responsibility from an MAH the skills required inevitably move beyond the merely technical. The QPPV should know how to effectively delegate and manage. The QPPV will inevitably come into situations where negotiation and influencing skills are required, not only within the company but also with competent authorities and ultimately, but hopefully rarely, with the remit of the law. The appointment of a QPPV may be made on the grounds of Pharmacovigilance expertise, and in some cases medical expertise. The presentation will seek to examine three aspects: 1.What are the appropriate skills required by a QPPV beyond the technical? 2. Does one size fit all? 3. Where else within the MAH should QPPV training be undertaken?
OP35. Beyond Bureaucracy: How Pharmacovigilance Might be Resuscitated
Bruce P. Hugman
Uppsala Monitoring Centre, Uppsala, Sweden
The purpose of this paper is to examine the reasons for the failure of spontaneous reporting systems to capture credible numbers of incidents of suspected patient harm and to propose ways in which much more comprehensive intelligence might be gathered.
Studies have repeatedly suggested that ADR reports received by the authorities represent a very small percentage of the total number of suspected ADRs experienced by patients.[1,2] Some of the most powerful obstacles to reporting are to be found in the methods used by authorities, and in the disposition of potential reporters.[3] Both of these areas are amenable to change, if there is insight, vision and energy to pursue it.
These problems may be analysed and remedied by the application of relatively simple principles of good management, training and communications, and by the elevation of intangibles, such as empathy, motivation, positive reinforcement, reciprocity, to much higher places in the practical planning and operation of systems.
Many of the procedures (e.g. form-filling) are burdensome; they need radical rethinking. Overall, the human relations and communications within PV systems are deficient. Both areas require new approaches, such as
-
• reform of taken-for-granted procedures, especially reporting forms
-
• active consultation with stakeholders on methods and processes
-
• persistent development and promotion of the system
-
• more dynamic training, debate, marketing and continuous engagement
-
• the provision of benefits and individual feedback for reporters
While all this requires radical rethinking and new patterns of behaviour, it does not necessarily imply major new resources, rather a more creative and purposeful use of existing resources. This paper will demonstrate just how it can be achieved.
OP37. Pharmacovigilance of Contraceptives: Why Does it Take so Long to Take Action?
K. van Grootheest,1 L. Härmark 2 and E. van Puijenbroek 2
1 Netherlands Pharmacovigilance Centre Lareb and University of Groningen, Groningen, the Netherlands; 2 Netherlands Pharmacovigilance Centre Lareb, the Netherlands
Background: A spontaneous reporting system is meant to detect signals and the general idea is that signals need to be confirmed by a formal epidemiological studies. More and more we see a renewed appreciation of observational data, such as case series.
Objective: Different aspects of the value of signals detected through spontaneous reporting in relation to formal epidemiological studies will be discussed, using two examples in the field of contraceptives.
Methods: In 2003 the Netherlands Pharmacovigilance Centre Lareb published four cases of thrombo-embolism associated with the use of to the oral contraceptive ethinylestradiol/drospirenone (Yasmin®).[1]
On July 1st, 2011 Lareb had received 49 cases of thromboembolism in Yasmin® use and a fatal outcome was reported 8 times.
The safety of drosperidone containing oral contraceptive, final results from the European Active Surveillance study on oral contraceptives based on 142475 women years of observation.[2]
In 2011, 8 years after the initial signal was given, two epidemiological studies were published confirming an increased risk of thromboembolic events.[3,4]
No regulatory action has been taken yet, however the risk of this contraceptive seems as double as high as with so called second generation pills.
In 2010 four countries published a paper about the relation between a levonorgestrel containing intrauterine device (Mirena®) and uterine perforation in which more than 500 cases received through the spontaneous reporting system were analyzed. An epidemiological study, sponsored by the manufacturer, has been published. No independent research has been published and no regulatory action has been taken up to now.
Results: These two examples show that there is a long time between the publication of a new signal and signal confirmation by a formal epidemiological study. This leads to a delay in the regulatory decision making process.
Conclusion: Women could have been exposed to a greater risk than needed when searching for reliable contraception. Case reports have to be taken more seriously by regulators and marketing authorization holders in the benefit-harm assessment of a drug.
OP38. Characterization of Reporting of Drug -Induced Hepatic Failure to the WHO -UMC Database: Influence of Gender and Age
M. Petronijevic,1 K. Ilic 2 and A. Suzuki 3
1 Medicines and Medical Devices Agency of Serbia, Belgrade, Republic of Serbia; 2 School of Pharmacy, Department of Pharmacology, Belgrade, Republic of Serbia; 3 Gastroenterology, Duke University, Durham, NC, USA
Objectives: Drug-induced liver injury (DILI) is a potential adverse drug reaction (ADR) of many medicinal products. In addition to drug specific properties, patient’s gender, age, genetic variability, nutritional factors, and underlying disease might mediate the development and progression of DILI. There were conflicting results regarding women’s greater susceptibility to DILI.[1] Some studies suggested strong relationship between DILI severity and female sex.[2,3] The aim of this study is to identify difference in reporting of drug induced hepatic failure (HF) between males and females of different age groups.
Methods: The WHO database of individual case safety reports (VigiBase™) was screened for the HF reports submitted from January 2000 to December 2009. HF as a preferred term based on the WHO-ART dictionary and specified time period were used as search criteria. The information retrieved from the VigiBase™ referred to the suspected drug, patient’s age, gender, and reporting country. Drugs were classified according to Anatomical Therapeutic Chemical (ATC) classification. Further analysis was performed for drugs reported in at least 20 HF cases in either males or females. Variables were examined using descriptive statistics. p value <0.05 was considered significant. SPPS 16 software (Chicago, Ill) was used for statistical analysis.
Results: During the period from January 2000 to December 2009 there were in total 6370 HF reports from 38 countries; 3237 (50.8%) for females and 2754 (43.2%) for males. Females were predominated in groups of age 10–49 years (p < 0.05), while males accounted for a larger portion in the 60–69-year-old group (p < 0.05). Overall, there were 742 and 664 different drugs or their combinations reported for HF in females and males, respectively (table I). 76 drugs were reported in at least 20 case reports of HF in either males or females. Of these, 20 drugs (antidepressants — 4; analgesics — 3) were significantly more frequently reported in females, whereas males were predominated in reports associated with 16 drugs (antivirals for systemic use — 9).
Conclusions: Overall, drug induced HF was more frequently reported in females. Age groups from 10 to 49 characterized female predomination, whereas males accounted for larger portion among patients aged 60–69. Gender differences in reporting of HF were specifically observed for some drugs and/or drug classes. Females were predominated in cases of HF associated with analgesics, antiepileptics, antiinflamatory and antirheumatic products, psychoanaleptics, antibacterials for systemic use, and antidiabetic drugs. Males were over-represented in cases of HF associated with antivirals for systemic use.
Countries ADR Reports
OP39. ADR Profiles and their Relation Associated with Nifurtimox -Eflornithine Combination Therapy (NECT) in the Treatment of Human African Trypanosomiasis (HAT)
P.N. Ntamabyaliro,1 B.Y. Salumu,1 D.B. Nzolo,1 Y.N. Lula,1 G.K. Mesia,1 S.M. Mampunza 2 and G.L. Tona 1
1 Unité de Pharmacologie Clinique et Pharmacovigilance, Faculté de Médecine, Université de Kinshasa, Kinshasa, DR Congo; Centre National de Pharmacovigilance, Kinshasa, DR Congo; 2 Centre Neuro-Psycho-Pathologique, Université de Kinshasa; Centre National de Pharmacovigilance, Kinshasa, DR Congo
Background: Active measures implemented to control HAT in the early 1960s have helped to reduce its prevalence to very low levels. Unfortunately, the lack of coordination and standardization of control field methods, reduced resource allocation to HAT, nonavailability of drugs have turned the disease to neglected.[1,2] The recrudescence of HAT as a public health concern has led experts and authorities to develop innovative lines of treatment among which Eflornithine and Nifurtimox, have been rapidly associated for use in the second stage of Trypanosoma brucei gambiense sleeping sickness under the denomination of NECT. The World Health Organization has recommended active Pharmacovigilance for this new combination. DRCongo with more than 70% of all cases worldwide has the responsibility to provide data on the safety of NECT.
Objectives: To identify the profile of adverse drug reactions associated with the use of NECT in DRCongo.
Methods: All Individual Case Safety Reports (ICSRs) related to NECT committed in the international data base by the DRC National PV Centre were extracted as excel files from vigiflow and reviewed. ADR were classified according to the WHO adverse Drug Reaction Terminology (WHO-ART).
Results: A total of 17 ICSRs were committed. Forty five ADRs were experienced, which means 2.7 ADR per patient. Sex ratio M/F was 10 : 7, mean age 32.5 years (Minimum 6, Maximum 60, Median 30) and NECT was the sole therapy in case. Reactions lasted about 2.7 days in mean (Median 3) and 95.6% (43/45) of them were possibly aused by Nifurtimox against 84.4% (38/45) for Eflornithine. However, 68.9% (31/45) of reactions were medically managed and only 17.8% (8/45) were not. Only 3 ADR were considered as serious, one of them being life threatening and the two other clinically significant. All of these ADR resolved without sequelae. No death was reported.
Discussions: In fact, NECT brings a wide range of ADRs. Gastrointestinal ADRs, mostly nausea and vomiting are more frequent, followed by psychiatric disorders, represented mainly by insomnia and confusion. Most of reactions are possibly raised by Nifurtimox. Those reactions could be easily managed. This is different from deaths and encephalopathy observed with melarsoprol used for the second stage of HAT before NECT.
Conclusions: NECT seems to be safe in the treatment of HAT. But we cannot confirm that using these few data. However, these results are encouraging and more Pharmacovigilance is needed, which is being done.
OP40. The Yellow Card Scheme: Patient Reporting of Adverse Drug Reactions and Signals they have Generated
M. Foy, S. Gandhi, S. Suri, S. Cumber and M.M. Jadeja
Medines and Healthcare products Regulatory Agency, London, UK
Background: Direct patient reporting of suspected ADRs to the MHRA was introduced in January 2005. Patients were encouraged to report suspected ADRs they or someone they care for experienced; a child, partner or family member. Patient reporting in the UK was formally established in February 2008. At this time the Yellow Card reporting website which had been redeveloped was re-launched. Yellow Card promotional campaigns have continued to promote the Scheme to patients.
Objective: To review patient Yellow Card data to identify trends in reporting and discuss how patient reporting plays a valuable contribution to signal detection.
Method: Patient Yellow Card data received in 2009 and 2010 was analysed, in terms of reporting method, reporter type, region and patient demographics. Details of the ADRs reported were analysed to show what signals were generated and to identify the most commonly reported drugs, vaccines and reactions.
Results: Since launch, 11924 patient Yellow Cards have been received, and have increased by 74% since 2005. In 2010 patient reports accounted for 7% of all ADRs received. Simvastatin and Human Papilloma Virus vaccine were the most commonly reported drug and vaccine respectively. In 2010, the MHRA received 1642 suspected ADR reports from patients with 70% of these reports being submitted on-line. Of the 277 signals investigated, 53 had contributing reports from patients. In 15 of these signals the index case was a patient report. These signals included food interaction (grapefruit juice) with amlodipine, cyproterone and hepatic failure and nitrofutantoin and alveolitis fibrosing, resulting in updates to the product information. Other signals are subject to ongoing investigation. The proportion of signals identified for which ADR reports from patients contributed towards increased from 15.6% in 2009 to 23.6% in 2010.
Conclusion: Patients’ commitment to contribute to the Yellow Card Scheme is clearly demonstrated by the increasing numbers of reports received. Reports are of a high quality providing a valuable contribution to the identification of new drug safety signals for which product information for prescribers and patients were updated.
PP041. Serbian National Pharmacovigilance Centre Review of AEFI During Intensive Monitoring of Focetria Vaccine Administration
J. Pilic, J. Babic and M. Eric
Medicines and Medical Devices Agency of Serbia, Belgrade, Serbia
Introduction: After declaration of epidemic infection disease pandemic flu A (H1N1) in the Republic of Serbia (RS) in November 2009, the administration of vaccine Focetria, started on December 17, 2009. The letter describing the need of intensive monitoring of vaccinated population was sent to all health care professionals involved in the process of immunization.
Aim: The aim of this paper is to evaluate safety profile of vaccine Focetria according to post-marketing experience in RS during the period from December 17, 2009 to May 31, 2010.
Methods: Adverse Events Following Immunization (AEFI) gathered in the Paniflow base were analyzed. Emphases were put on the data source; demographic characteristics of patients and clinical importance of AEFI which were classified by the system organ class (SOC) and coded according to the Medical Dictionary for Regulatory Activities (MedDRA). For the statistical processing, there have been used the Excel (Microsoft Office).
Results: During the period of intensive monitoring, 84 cases containing 314 AEFIs were reported to the National Pharmacovigilance Centre (NPC). In respect of the results presented, there can be noticed that the majority of AEFIs were reported by physicians (71; 85%), and pharmacists participated in the reporting with 13 cases (15%). There were no significant gender differences in reported cases. The most frequently reported AEFI were temperature elevation (36; 11.4%), malaise (31; 9.9%), headache (27; 8.6%), myalgia (26; 8.3%) and fatigue (22; 7.01%). In regard to the MedDRA SOC, the largest number of AEFI was related to the general disorders (112; 35.7%), nervous system disorders (55; 17.5%), and musculoskeletal system disorders (46; 14.6%).
Discussion: In view of data on Serbian population (7.3 million) and number of vaccine doses administered (149.8222), we can conclude that the immunization response was very low (2%). Reporting rate for the temperature elevation was approximately 24 per 100.000 vaccinated persons, which corresponds to the category of rare (≥1/10.000 to ≤1/1000), and malaise, headache, myalgia and fatigue were related to the same category too.
Conclusion: All cases that were collected during the period of intensive monitoring were consistent with known safety profile described in the product information of vaccine Focetria.[1] Reporting frequency was less in relation to the defined frequency of AEFI occurrence.[1] No new safety risks were identified during the vaccination on the territory of RS.
PP042. Risk of Febrile Seizures Associated with the Measles-Mumps-Rubella-Varicella Combination Vaccine (MMRV): Data from Spontaneous Reporting in Italy
U. Moretti,1 G. Zanoni ,2 A. Conforti,1 R. Lora,1 E. Arzenton,1 F. Trotta 3 and C. Santuccio 3
1 Pharmacology Unit and Pharmacovigilance Centre of Veneto Region, University Hospital, Verona, Italy; 2 Immunology Unit, University Hospital, Verona, Italy; 3 Italian Medicines Agency, Pharmacovigilance Office, Rome; Italy
Objectives: In previous studies, associations between Measles-Mumps-Rubella Combination Vaccine (MMR) and increased risk for febrile seizures 1 to 2 weeks after vaccination were observed.[1] A recent paper showed that the use of MMRV vaccine instead of separate MMR and varicella vaccines approximately doubles the risk for fever and febrile seizures, resulting in 1 additional febrile seizure for every 2300 doses of MMRV vaccine administered instead of separate MMR and varicella vaccines.[2] In Italy MMRV vaccine has been introduced in the market in 2007. Aim of this study is it analyze the data on febrile seizures by MMR, MMRV and varicella (VAR) in the Italian spontaneous reporting database.
Methods: Adverse events have been coded according to WHO-ART terminology. Cases has been defined as reports with the WHO-ART terms “Fever convulsions” or “Febrile seizures” or reports including both any term related to seizures (e.g. “Convulsions” or “convulsions neonatal”) and any term related to fever (e.g. fever neonatal or hyperpyrexia). Non cases were all the other report related to vaccines. Exposition was determined looking at both suspected and concomitant vaccines. Reporting Odds Ratios (ROR) as a measure of disproportionate reporting was calculated comparing the studied vaccines to all the other vaccine reports.
Results: Up to March 2011 the database includes 22 030 reports related to vaccines. The total number of cases related to vaccines were 339. MMRV had an higher proportion of cases (25 cases on 264 reports, 9.5%) compared to MMR alone (119 on 3350 reports, 3.6%), MMR + VAR (5 on 114 reports, 4.4%) and VAR alone (1 on 255 reports, 0.4%). ROR values suggest a significative disproportionality of febrile seizures associated to MMRV (7.26, CI 95% 4.62, 11.32), MMR (3.15, CI 95% 2.49, 3.97) and MMR +VAR (3.01, CI 95% 1.08, 7.71) but not for VAR alone (0.25, CI 95% 0.01,1.66). ROR values shows a two-fold increased risk for MMRV compared to MMR and MMR + VAR. Both incidence and ROR values for febrile seizures are similar comparing MMR alone to MMR and varicella vaccines given separately in the same day. Values associated to the combined vaccine are significantly higher.
Conclusions: Spontaneous reporting systems have the main goal to identify signals. Our results are in line with other published studies[2] suggesting an increased risk of febrile seizures for the combined MMRV compared to a separate administration of MMR and VAR. However due to the limitations of spontaneous reporting further studies are needed to confirm this signal.
PP043. Spontaneous Reporting of Adverse Reactions to Pneumococcal Vaccination in Children
C. Santuccio,1 F. Menniti Ippolito,2 L .Tartaglia,1 F. Trotta 1, D. Morlino 1 and U. Moretti 3
1 Italian Medicines Agency, Pharmacovigilance Unit, Rome, Italy; 2 National Institute of Health, National Centre of Epidemiology, Rome, Italy; 3 University of Verona, Italy
Background: In mid 2010 the pneumococcal polysaccharide conjugate vaccine (13-valent, adsorbed) was introduced in the vaccination programs in Italy replacing progressively the pneumococcal saccharide conjugated vaccine, adsorbed, against 7 serotypes.[1,2] Most doses were co-administered with exavalent vaccine.
Objective: To describe the monitoring of adverse events occurred in children who received pneumococcal vaccination after the introduction of the 13-valent vaccine.
Methods: Adverse events to both pneumococcal vaccines (7 and 13 valent) and to exavalent vaccines reported from 1 June 2010 until 15 June 2011 to the national pharmacovigilance database were analyzed as single and co-administered vaccinations.
Results: Preliminary analysis, based on reactions with onset data between 1 June 2010 to 15 June 2011, shows that 130 reports to 7-valent pneumococcal vaccine and 256 to 13-valent vaccine were received. In most reports both vaccines were co-administered with the hexavalent: in 105 cases concerning 7-valent pneumococcal vaccine and 186 the 13-valent vaccine. A slight even if not significant increase of serious reactions associated to pneumococcal 13-valent compared to 7-valent vaccine has been found and in percentage the value was about 14.5% versus 13%.This difference is still present in the association with hexavalent vaccine 16% versus 13%.
The first four SOCs involved in the reports of both vaccines were the same but with some differences in the percentage distribution of the most frequently reported adverse events: the percentage of reactions affecting the nervous system (24%) and skin (30%) were higher for 13-valent vaccine than those reported for 7-valent pneumococcal vaccine (respectively 21% and 22%). An opposite situation was observed for reactions classified as general disorders or gastrointestinal related to Prevenar (71% and 6%) with regard to those reported for 13-valent vaccine (62% and 5%).
Conclusions: Spontaneous reports are not a tool to identify differences between products, they can only generate potential signals, furthermore the criteria of data onset can led to change overtime. After a very preliminary analysis, during the first year of immunization, the number of serious reports associated with 13-valent pneumococcal vaccine was higher than the one related to the 7-valent pneumococcal vaccine.
PP044. 2009 H1N1 Influenza Vaccines in Pregnant Women: A Survey in South West France
E. Omon,1 C. Damase Michel,1 C. Hurault,1 I. Lacroix,1 J. Montastruc,1 S. Oustric 2 and B. Escourrou 2
1 Service de Pharmacologie Clinique, Centre Midi-Pyrénées de Pharmacovigilance, de Pharmaco-épidémiologie et d’Information sur le Médicament, Inserm UMR 1027, CHU de Toulouse, Faculté de Médecine, Université de Toulouse, Toulouse, France; 2 Département de Médecine Générale, Faculté de Médecine, Université de Toulouse, CHU de Toulouse, France
In 2009, during A (H1N1)v pandemia, French Health authorities recommended influenza immunisation for pregnant women because of the higher risk of serious influenza outcomes in that population.[1] Thus, the non adjuvanted inactivated influenza vaccine Panenza® was administered to French women from the second trimester of pregnancy. Several studies suggest that inactivated seasonal influenza vaccines are safe during pregnancy but there are few data about the effects of new A(H1N1) vaccines (new antigen) on pregnant women.
Objective: The aim of the present prospective study was to describe pregnancy outcomes among women vaccinated with non adjuvanted influenza vaccine in South Western France.
Methods: The study ran from November 2009 to February 2010 and included, on a voluntary basis, pregnant women who were vaccinated against A(H1N1)influenza in vaccination clinics or maternity-wards.
Results: 569 pregnant women were monitored until delivery. Compared with the general population, the risks of maternal conditions, malformations, or neonatal conditions were not statistically different.
Conclusion: This study does not reveal any sign of safety concerns regarding the effects of the vaccine on pregnancy outcomes; The present survey is included in a larger study performed by several French Pharmacovigilance centers, Pregvaxgrip, which will allow to further assess safety of the A (H1N1)v vaccine.
PP045. Monitoring Adverse Reactions of the Cantgrip® Vaccine
C. Pop,1 A.M. Farcas,1 D.C. Leucuta,2 C. Bucsa,1 D. Faraian,3 D.R. Florea,3 D. Tatulescu 4 and M.T. Bojita 1
1 Drug Information Research Center, School of Pharmacy, University of Medicine and Pharmacy “Iuliu Hatieganu” Cluj-Napoca, Romania; 2 Medical Informatics and Biostatistics Department, University of Medicine and Pharmacy “Iuliu Hatieganu” Cluj-Napoca, Romania; 3 Epidemiology Center, Territorial Emergency Hospital, Cluj-Napoca, Romania; 4 Infectious Disease Clinical Hospital, Cluj-Napoca, Romania
Objectives: Post-marketing vaccine safety monitoring is an important component of all vaccination programs. Early detection and quick response to adverse events following immunization can lessen their negative impact on health and on immunization programs themselves. For this reason, the current non-interventional, prospective study developed a method of further evaluating the safety of the Cantgrip® vaccine for influenza virus A(H1N1) manufactured and used in Romania.
Methods: A total of 371 questionnaires were distributed to the healthcare professionals at the moment of the immunization during the national immunization campaign due to the A(H1N1) epidemic of 2009. Out of those who received the questionnaires, 309 subjects returned them filled in, in two weeks’ time.
Results: The most common injection-site reaction was pain (48.5%). Other local adverse reactions were redness, irritation and induration. The most common systemic adverse reactions reported were: muscle ache (8.7%), chills (2.9%) and sweating (1.9%). Most of the reported adverse reactions following immunization were mild-to-moderate. No life-threatening or adverse events of special interest were reported.
Conclusions: The results of our study showed that, for an initial follow up of the studied group of subjects, Cantgrip® proved to be a safe vaccine.
PP046. Abscess at Injection Site with Diphtheria, Tetanus, Pertussis and Haemophilus Influenzae Type b Vaccine (Analysis of Moroccan Pharmacovigilance Database)
A. Tebaa,1 A. Zineddine 2 and R. Soulaymani Bencheikh 1
1 Morrocan Pharmacovigilance Centre, Morocco; 2 Service d’Accueil des Urgences Pédiatriques, Hôpital d’Enfants, Casablanca
Background: Vaccines are very safe, contrary to rumours circulated by the media and anti-vaccine publications. At the routine vaccination, Common reactions to the vaccine may include soreness, redness and swelling at the injection site. The abscess is an exceptional local reaction observed after vaccination except BCG vaccination with a frequency about 0.67 to 1.23/1000 doses administered.
Aim: To analyze the report with the injection site Abscess associated to Diphtheria, Tetanus, Pertussis and Haemophilus influenzae type b Vaccine in the Moroccan pharmacovigilance database.
Method: the present analysis was performed on spontaneous reports of adverse events (AEFI) received by the Moroccan pharmacovigilance centre (CMPV). The period included was from 2008 to 2010.
Results: In this period, a total of 1939 spontaneous report of AEFI were indentified.
Local reactions according to WHO-ART are represented in 30% (470 cases), of which abscesses at injection site account were for 42% (197cases).
On the vaccine issue, DTC-HIB was the mainly vaccine taken in 69% (133 cases) of children especially in the third booster (52%). In respect to the various types of abscess, 60% of abscesses were unspecified, 12% was described as sterile abscesses and 28% as infectious abscess.
These abscesses occurred in female infants in 52%, and observed in an onset delay within two weeks to two months after vaccination in 68% of cases, among the signs associated, fever was observed in 20.5% of cases and regional lymphadenopathy in 9%.
A surgical drainage was realized in 39% of cases with a bacteriological analysis in search of the causative organism revealed an absence of germs in 90% (48 cases).
Conclusion: Following this analysis, we concluded that the spontaneous reporting rate of site injection abscess is very high according to literature and the majority of cases are classified at Level 2 of certain diagnosis as defined by the Brighton Collaboration, in addition to a lack of evidence in favour of the programmatic error (missing laboratory results, lack of investigation), therefore the abscess post vaccination remains a preventable adverse event.
PP047. Impact of Non-Vaccine-Related Reports on Statistical Signal Detection for Vaccines in Spontaneous Reporting Databases
U. Moretti,1 R. Lora,1 G. Zanoni,2 L. Tartaglia,3 F. Ferrazin,3 G.P. Velo 1 and C. Santuccio 3
1 Pharmacology Unit and Pharmacovigilance Centre of Veneto Region, University Hospital, Verona, Italy; 2 Immunology Unit, University Hospital, Verona, Italy; 3 Italian Medicines Agency, Pharmacovigilance Office, Rome, Italy
Objectives: Next to the classical case by case approach, where every individual case is reviewed, statistical approaches are nowadays an important tool in the signal detection process.[1] Based on the hypothesis that all the reactions are reported in the same proportion for all drugs, the methods used in this context analyze a disproportionate reporting of a drug-event pair. The commonly used data mining methods are the proportional reporting ratio (PRR) and the reporting odds ratio (ROR). Most of the spontaneous reporting database include both vaccine and non-vaccine related reports. However the safety profile of vaccines is very different from the safety profile of the other drugs. Aim of this study is to analyze the impact of non-vaccine-related reports on PRR values for vaccines in the Italian spontaneous reporting database.
Methods: Adverse reactions are coded in the database using both WHO-ART and MedDRA terminologies. WHO-ART Preferred Terms have been used in this study to reduce the number of vaccine-event pairs. PRRs values have been calculated for all vaccine-event pairs within only the vaccine-related report (Method A) or in the whole database (Method B). A signal of disproportionate reporting (SDR) was present when the PRR value was >2 with a lower bound of the 95% confidence interval >1 and when at least two individual cases were present.
Results: Up to March 2011 the Italian database contains about 140 000 reports, 22 000 associated to vaccines. The total number of vaccine-event pairs was 4468. The SDRs identified with method A were 724 (16.2%) compared to 1033 (23.1%) with method B. Two hundred and eleven SDRs were identified only with method A, 513 were common to both methods whereas 520 SDRs were identified only with method B. Considering the 513 SDRs identified with both procedures we found lower PRR values using method A in 380 pairs, with a median difference in the PRR value of 5.85.
SDRs identified only with method A include reactions rarely associated to vaccine but frequently reported with the other drugs. Example are cardiovascular and psychiatric reactions.
SDRs identified only with method B include reactions frequently associated to vaccines and rarely reported with the other drugs. Examples are febrile seizures, fever or reactions in the injection site
Conclusions: Quantitative analysis using the PRR gives different results when applied to the whole database or only to the vaccine-related reports. This should be considered since often case-by-case evaluation is done only to SDRs.
PP048. Review of Adverse Events Following Immunization Submitted to WHO-UMC by the Turkish Pharmacovigilance Center (TUFAM) between 2005 and May 2011
D. Aydinkarahaliloglu,1 Y. Kasap,1 E. Aykaç,1 G.Sağiş 1 C.Babacanoğlu,1 H. İlbars,1 A. Kara,2 H. Özbek 1 and S. Kerman 1
1 General Directorate of Pharmaceuticals and Pharmacy, Ministry of Health, Ankara, Turkey; 2 Hacettepe University, Faculty of Medicine, Department of Pediatrics, Ankara, Turkey
Background: The Ministry of Health, General Directorate of Primary Health Care conducts an immunization program via vaccination against 11 preventable diseases and actively monitors the adverse events that occur following immunization. On the other hand, TUFAM monitors the adverse event reports associated with the vaccines which are available apart from this immunization program in a passive manner.
Objective/aim: The vaccine related adverse reactions submitted to WHO-UMC database by TUFAM within the passive monitoring system were investigated.
Methods: A search on adverse reactions associated with approved/licensed vaccines present in Vigiflow database between 2005 and May 2011 was conducted and the data obtained in excel format through the system were investigated. The adverse reactions that occurred during influenza vaccination and considered to be related to the vaccine are presented in tabulated form.
Results: A total of 42 reports have been submitted in a period of 6 years within the passive vaccination monitoring system. The reports related to H1N1 vaccines are not included in this value. 35 of these reports (83.3%) were defined as serious by the reporter. 5 of these were life threatening and 25 of these required hospitalization. 47.6% of the subjects were females. 76.2% of the reports were submitted by the physicians, 14.3% by pharmacists, 7.1% by other healthcare professionals and 2.4% were submitted by the consumers.
Conclusion: Majority of the vaccination related adverse reactions submitted to TUFAM appear to be serious. It is of note that there are three Guillain-Barré Syndrome cases among the serious adverse reactions following influenza vaccination, particularly within 2010.
Discussion: Since immunization is carried out on healthy subjects with protection purposes, the adverse reactions need to be monitored more closely. Hence there is a small number of reportings regarding the adverse events following immunization with vaccines apart from the General Directorate of Primary Health Care immunization programme; it is required to raise awareness on this subject among healthcare professionals.
PP049. Adverse Events Following Immunization with OPV in Adults in Kinshasa: Preliminary Results
D.B. Nzolo,1 D.B. Pandi,1 T.N. Mpiempie,1 S.B. Banzundama,1 B.L. Mvete,1 O. Mboma,1 M.M. Lusakibanza,1 Y.N. Lula,1 F.B. Makila,1 G.K. Mesia,1 C.N. Nsibu2 and G.L. Tona 1
1 Unité de Pharmacologie Clinique et Pharmacovigilance, Faculté de Médecine, Université de Kinshasa, Kinshasa, DR Congo; Centre National de Pharmacovigilance, Kinshasa, DR Congo; 2 Département de Pédiatrie, Cliniques Universitaires de Kinshasa, Faculté de Médecine, Kinshasa, DR Congo; Centre National de Pharmacovigilance, Kinshasa, DR Congo
Background: Using oral vaccine, the global campaign to eradicate polio achieved a more than 90% reduction in the number of polio cases worldwide in the 11 years since it was launched.[1] Because of risk of vaccine-associated paralytic poliomyelitis, oral poliomyelitis vaccine (OPV) has been replaced by the inactived poliomyelitis vaccine (IPV) in some countries. Therefore, others adverse effect following immunization (AEFI) related OPV are less documented. This year, after outbreak of poliomyelitis mutant virus in Central Africa Region reputed to abound others viruses (ebola, monkey pox), some cases were reported even among adults. A ministry of health of DR Congo launched immunization mass campaign mainly for adults. National Pharmacovigilance Centre (CNPV) has taken this opportunity to monitor possible AEFI related to this vaccine during the second campaign.
Objectives: To determine the nature of AEFI related to OPV.
Methods: High schools and universities were chosen as sites to collect information related to AEFI. Questionnaire elaborated by CNPV was addressed mainly to those who probably experienced any AEFI after receiving OPV. Before fulfilling questionnaire, vaccination benefit was explained as well as the possibility of occurring of adverse events. All questionnaires were gathered and processed by CNPV.
Results: AEFI questionnaire from 767 persons were analyzed. There were 255 men and 512 women with a sex ratio M/F of 1:2. The average age was 16.8±5.19 years (ranged from 6 to 35.5). Each person reported a mean of 1.33±0.6 AEFI. 1020 AEFI were reported in total. The most frequent AEFI reported were headache (22.4%), abdominal pain (17.2%), fever (11.7%), diarrhea (9.9%) and asthenia (7.5%). There were 5 cases of muscle weakness and 2 suspected vaccine-associated poliomyelitis. One case of asthma-like reaction with a positive rechallenge was reported. The average AEFI onset date was 1.74±1.16 days, ranged from 1 to 9 days. Rechallenge was positive for 173 persons (22.6%). Concerning the system organ class, the most affected were gastrointestinal system (33.5%), central and peripheral nervous system (29.3%) and body as a whole (21.8%). 4.2% of persons reported musculoskeletal disorder and 3.2% skin and appendages disorders, including urticaria, rash and pruritus.
Conclusions: Fever, diarrhea, headache and other body as a whole and musculoskeletal disorder are described with OPV. Active surveillance after a immunization mass campaign has allowed to register some rare OPV related AEFI, such as a possible vaccine associated poliomyelitis.
PP050. Surveillance of Adverse Events Following Immunization (AEFI) with Trivalent Inactivated Influenza Vaccine in Canada: Was an Increase in the Number of Febrile Seizures Observed for the 2010–2011 Vaccination Campaign?
J. Lafleche, R. Pless and B. Law
Public Health Agency of Canada, Canada
Background: Mechanisms put in place for heightened vigilance during the pandemic H1N1 vaccination campaign improved adverse event following immunization(AEFI) surveillance in Canada as a whole. When Australia extended their suspension[x] of the 2010 seasonal flu vaccination program in children 5 years and younger after seeing an increase number of febrile seizures, public concern was also felt in Canada. Improvements to the Canadian system would be important to monitor vaccine safety during the 2010/2011 seasonal influenza campaign including any potential signal with febrile seizure.
Objective: To assess if an increased number of febrile seizures was reported to the Canadian Adverse Event Following Immunization Surveillance System(CAEFISS) for the 2010/2011 seasonal influenza vaccination campaign.
Methods: AEFI data going back to the 1998/1999 influenza were extracted from CAEFISS. As with other passive surveillance systems, CAEFISS is sensitive to reporting changes, which in Canada have been seen after changes in immunization programs and heightened vigilance. After a thorough review of available data, only those for children 5 and under and where influenza vaccine was administered alone were included. Cases were analysed by demographic characteristic, time to onset, and adverse events coded in MedDRA (medical dictionary for regulatory activities).
Results: There were 181 reports to CAEFISS received by June 15th, 2011 for children 5 years and younger and who had received a 2010/2011 influenza vaccine alone. Six reports of febrile seizures were received. This represented 3.3% of the 181 AEFI reports. Past flu seasons have seen a range of 0–5 febrile seizures in children receiving influenza vaccine alone (about 0 to 4%). None of the febrile seizures in the children who received the 2010/2011 influenza vaccine alone required hospitalization and there were no trends in relation to a particular vaccine lot.
Conclusion: After Australia’s suspension of their influenza vaccine program in children, the Public Health Agency of Canada in collaboration with their Provincial/Territorial (P/T) partners and other stakeholders planned to closely monitor any reports of febrile seizure as the seasonal influenza vaccination campaign unfolded. AEFI surveillance in Canada and regular communication with the vaccine vigilance working group (composed of representatives from PHAC, P/T partners and other stakeholders), did not find a signal in relation to febrile seizures during the 2010/2011 vaccination campaign in children 5 years and younger receiving influenza vaccine alone.
Pharmacovigilance Systems for HIV/Malaria/Tuberculosis
PP051. Antimalarial Drugs Pharmacovigilance in National Malaria Control Programme of DR Congo
Y.N. Lula,1 J.Y. Liwono,1 P.N. Ntamabyaliro,1 D.B. Nzolo,1 B.Y. Salumu,1 B.L. Mvete,1 G.K. Mesia,1 S.M. Mampunza2 and G.L .Tona 1
1 Unité de Pharmacologie Clinique et Pharmacovigilance, Faculté de Médecine, Université de Kinshasa, Kinshasa, DR Congo; Centre National de Pharmacovigilance, Kinshasa, DR Congo; 2 Centre Neuro-Psycho-Pathologique, Université de Kinshasa; Centre National de Pharmacovigilance, Kinshasa, DR Congo
Background: Artemisinin-based Combination Therapies (ACTs) are currently regarded as the best available treatments for uncomplicated malaria and artesunate-amodiaquine (ART-AQ) has been adopted as first-line therapy in DR Congo since 2005. Since most of the safety data on these combinations are derived from relatively small and time-limited studies, there is a need for ongoing pharmacovigilance (PV).[1] Furthermore, the deployment of new antimalarials in Africa must lead health programs to develop PV systems. Through Global Fund (GF) Round 8 Malaria project, an opportunity was given to National Centre of Pharmacovigilance (CNPV) for antimalarial drugs monitoring.
Objectives: To determine antimalarials adverse drug reactions (ADRs) patterns and to detect serious, severe or unexpected ADRs.
Methods: Stimulated spontaneous reporting approach was adopted to help health professionals for detecting especially serious and unexpected ADRs and signals related to antimalarials. All ADR reporting forms for the period October 2010–April 2011 from ten sentinel sites of National Malaria Control Programme (NMCP) at Kinshasa were gathered during supervision by CNPV staff. The detected ADRs were assessed for causality (WHO causality categories and French algorithm) and seriousness (International Conference on Harmonization E2A criteria).[2] ADRs were code using World Health Organization Adverse Reaction Terminologies (WHO-ART).
Results: A total of 122 reports (42 to antimalarials) were collected and 165 ADRs (95 to antimalarials) were experienced during this period. The ADR reporting rates to antimalarial drugs for the period was 34.4%. ACT accounted for about 78.5% with 25 cases (59.5%) related to ART-AQ (provided by GF), quinine was involved in 14.3% of cases and Sulfadoxine or Sulfalene-Pyrimethamine (SP) 7.1%. Higher incidence rate of ADRs was observed with body as whole-general disorders (24.2%, asthenia or fatigue particularly and associated to ART-AQ use, 4 cases of therapeutic response decrease), gastrointestinal disorders (18.9%, nausea and vomiting mainly), central and peripheral nervous disorders (16.8%, dizziness or vertigo mainly and associated to ART-AQ use) and skin disorders (11.6%, especially urticaria, 1 case of serious skin reaction with artesunate-SP). 13.7% of ADRs were serious (mainly with ACTs use, 1 case of deafness with quinine) and has required hospitalization.
Conclusions: This study suggests a relative high rate of ADRs with antimalarial drugs use. Even if ACTs are currently the most active antimalarials with short-course treatment, ART-AQ seems to be associated with higher of ADRs than other antimalarials.[3]
PP052. Adverse Drug Reactions to Antiretroviral Drugs at Lagos University Teaching Hospital HIV Clinic, Lagos, South West Nigeria
I.A. Oreagba,1,4 O. Agede,1 T. Adeyemo,2 C.S. Ejekam,3 O. Opanuga,3 S. Akanmu,2 O. Awodele,1 T. Adeyemo 3 and S. Akanmu 3
1 Department of Pharmacology, University of Lagos, Lagos, Nigeria; 2 Department of Haematology and Blood Transfusion, University of Lagos, Lagos, Nigeria; 3 PEPFAR (HIV) Clinic, Lagos University Teaching Hospital Lagos, Lagos, Nigeria; 4 National Pharmacovigilance Centre, National Agency for Food and Drug Administration and Control, Lagos, Nigeria
Objectives: Antiretroviral therapy (ART) in patients with HIV infection is being threatened by the adverse drug reactions (ADRs) associated with their use. ADRs can impact negatively on any national ART programme with the occurrence of therapeutic failure and resistance.[1,2]
This study aimed at determining the nature, severity, causality and risk factors for ADRs in patients on ART at LUTH HIV Clinic Nigeria.
Methods: From a population of about 8000 registered HIV infected patients, 273 ambulatory patients on antiretroviral drugs and presenting with ADRs were monitored. Intensive monitoring group (IM, n= 136) were studied prospectively over a period of 6 months using a structured data capture form. The spontaneous reporting group (SR, n = 137) were studied retrospectively within the last one year. Naranjo’s scale[3] was used to assess causality of the adverse drug reactions, WHO Severity scale was used to assess severity and multiple logistic regression used to assess the risk factors for the development of ADRs. All statistical calculations were performed using SPSS V 17.0. A p-value of <0.05 was considered as statistically significant.
Results: The most commonly prescribed ART combination was zidovudine, lamivudine and nevirapine (52.9% in IM and 53.5% in SR), The most prevalent ADRs were dizziness (39%) pruritus (39%), skin rash (37%), nausea and vomiting (27%) and weakness (24%) in IM group, and dizziness (12.4%) lipodystrophy (11.7%) pruritus (10.2%), anaemia (10.2%) and diarrheoa (8.8%) in the SR group.
Age, 21–30 yrs (OD=1.1, p = 0.03) and CD4 count 200 cells/mL (OD= 1.1, p = 0.027) were important risk factors for ADRs in the IM group, while Zidovudine/Lamivudine/Abacavir (OD= 10.9, p = 0.017) was the only significant risk factor for the development of ADRs in the SR group. ADRs observed in the IM group were mild (76.5%), moderate (19.6%) and severe (3.9%) while 42.9% of ADRs were classified as ‘probable’, 38.1%, ‘possible’ and 19% ‘doubtful’ using the Naranjo algorithm.
Conclusions: Young HIV/AIDS patients and those with CD4 count of 200 cells/mL are predictors of ADRs. This study highlights the importance of monitoring ADRs to antiretroviral drugs.
PP053. Spontaneous Adverse Event Reporting of First-Line Anti-Tuberculosis Drugs in One Regional Pharmacovigilance Center
H. Park,1 G. Jung,2 H. Hwang,2 K .Shin,1 M. Kim,1 G. Lee,1 K .Kim,1 M. Lee 1 and S. Park 1
1 Department of Internal Medicine, Pusan National University Hospital, Busan, Korea; 2 Regional Pharmacovigilance Center, Pusan National University Hospital, Busan, Korea
Objectives: Public-Private Mix (PPM) for tuberculosis (TB) care have been provided in Korea. Nurses have an important role in improving drug compliance and detecting drug adverse events (AEs) in PPM for better TB care. To evaluate the incidence, clinical manifestation and causative drugs of AEs by first-line anti-TB drugs and investigate the role of PPM nurse in detection of AEs using spontaneous AEs reporting to one regional pharmacovigilance center.
Methods: We reviewed the data based on spontaneously reported AEs of first-line anti-TB drugs between January 2009 and February 2011 to Pusan National University Hospital regional pharmacovigilance center. Serious AE was defined as any adverse drug reaction that resulted in discontinuation of one or more drugs, and/or directly resulted in hospitalization. The clinical features and causative drugs and the serious AE-related factors were evaluated.
Results: Among 1842 patients registered as active TB between Jan 2009 and Feb 2011, 121 (6.6%) patients with AEs by anti-TB drugs were spontaneously reported to our regional pharmacovigilance center. The AEs were reported by doctors (23.6%) and PPM nurses (76.4%). Among them, thirty-nine patients (32%) had serious AEs for a total 110 events. The most common serious AE was skin rash and/or itching sensation (46%). The overall incidence of serious AE was higher with rifampin (n = 34, 31%) than with isoniazide (n = 30, 27%), ethambutol (n = 24, 22%) or pyrazinamide (n = 22, 20%). Significant associated factors for serious AE of the first-line anti-TB drugs were older age (p = 0.037), concomitant respiratory disease (p = 0.038) and extrapulmonary TB (p = 0.028).
Conclusions: Based on spontaneous adverse event reporting, the most common serious AE related to first-line anti-TB drugs was skin rash and 76.4% of AEs were reported by PPM nurses. The PPM system for TB care is running a role for improving the spontaneous reporting and early detection of ADE by anti-TB drugs.
PP054. Safety of Artesunate Amodiaquine (AS/AQ) and Artemether-Lumefantrine (AL) in Accra, Ghana: A Cohort Study
A.N. Dodoo, A. Adomako Bonsu, M. Abdul Sulley and C. Otieku Boadu
Centre for Tropical Clinical Pharmacology and Therapeutics, University of Ghana Medical School, University of Ghana, Accra, Ghana
Background: Malaria, commonly caused by Plasmodium falciparum remains a major health challenge for sub-Saharan Africa. In Ghana, malaria accounts for over 40% of all outpatient attendance, with an estimated 38 000 deaths per annum.[1] Studies in sentinel sites within the country have indicated that the Plasmodium parasite has developed resistance to chloroquine (between 20–25%) in all parts of the country and increasing but variable rates of resistance to Sulphadoxine/Pyremethamine (SP). In light of these findings, Ghana has since 2005 adopted the use of Artesunate Amodiaquine and Artemether-Lumefantrine as first line treatment for uncomplicated malaria. With curative rates higher than 95% in most studies, Artemisinin-based combination therapies (ACTs) have been recommended by the WHO as the gold standard for treatment of uncomplicated malaria worldwide.[2] Attempts to enhance the availability and accessibility of these medicines by the Global Fund Against AIDS, Tuberculosis and Malaria (Global Fund), the United States President’s Malaria Initiative (PMI) and the Affordable Medicines Facility for Malaria (AMFm) have till date been successful, ensuring widespread deployment of ACT’s worldwide. Despite the relatively safe profile of ACTs, there are lingering concerns about their potential real life toxicities; noting the increased accessibility.
Objectives: This study will provide effective clues and solutions to the effects of age and gender on the real-life safety of AS + AQ and AL in Accra, Ghana.
Methods: A non-interventional cohort event monitoring program was carried out. 309 malaria patients who had received either Artesunate Amodiaquine or Artemether-Lumefantrine from pharmacies at five health facilities in Accra were randomly recruited. After five days of hospital visit, patients were actively followed up via the telephone to record adverse events if any.
Results: Out of the 309 patients, 110 (35.6%) were male, of which 75 (36.1%) and 35 (34.7%) took AS/AQ and AL respectively. 199 (64.4%) females were recruited, with 133 (63.9%) and 66 (65.7%) receiving AS/AQ and AL respectively. The age of participants was distributed as follows: <5 yrs@ 81 (26.2%) [AS/AQ 68 (32.7%), AL 13 (12.9%)]; 5–15 yrs: 56 (18.1%) [AS/AQ40 (19.2%), AL 16 (15.8%)]; 16–59 150 (48.5%) [AS/AQ 93 (44.7%), AL 57 (56.4%)] and >60 22 (7.1%) [AS/AQ 7 (3.4), AL 15 (114.6%)].
Conclusions: The incidence of adverse events was higher in participants taking AS/AQ than AL 2.61 (95% CI: 1.54–4.47). This indicates that the safety profile of artesunate amodiaquine may be relatively lower than that of lumefanterine and hence artemether lumefanterine could be a better tolerated antimalarial.
PP055. Antiretrovirals and Pregnancy: A Case Series
E. Solé, G. Maura, E. Herlem, M. Germain and T. Trenque
Pharmacovigilance and Pharmacoepidemiology Regional Centre, CHU Reims, France
Background: Treatment of HIV disease during pregnancy has progressed. Women received combination of antiretroviral therapy or triple antiretroviral drug prophylaxis throughout pregnancy.
Objective: The aim of this study was to evaluate exposure to antiretroviral therapy in a case series of pregnant women.
Methods: During three years, in a medical unit, we collected HIV infected pregnant women treated by antiretroviral therapy. For all cases, the women characteristics (treatment received during pregnancy, adverse drug reactions, hospitalisations, delivery and drugs administered during labour) and the newborn characteristics (weight, clinical features, malformations, received treatment and type of feeding) were studied.
Results: Thirteen prospective reports of antiretroviral exposure were registered. The median age was 31 years. They all have received combination therapy during their pregnancy: eight received 2 nucleoside reverse transcriptase inhibitor (NRTI) and 1 protease inhibitor (PI) ± ritonavir, two received 2 NRTI and 1 non nucleoside reverse transcriptase inhibitor (NNRTI). Three patients received 1 IP, 1 INTI and ritonavir or 2 INTI and integrase inhibitor or fusion inhibitor, IP, INTI and ritonavir. Nausea and vomiting were reported in four patients. Seven patients have been hospitalized during pregnancy for threat of premature labor. Two patients were lost to follow up. Mean gestational age at birth was 39 weeks of amenorrhea. There were nine caesarean deliveries and two natural childbirth. At birth, one neonate was premature and two showed fetal distress. The middleweight of newborn was of 2858 g. No fetal defects, no stillbirth neither birth with congenital malformation was collected. After birth, post exposure prophylaxis was provided through administration of zidovudine to all infants. In one case, triple antiretroviral therapy (zidovudine, lamivudine and lopinavir/ritonavir) was necessary. All the neonates received an artificial breastfeeding.
Discussion: Antiretroviral are widely prescribed in pregnancy as the risk of mother-to-child transmission can be reduced from 15 to 25% to less than 1%. Pregnant women with advanced HIV infection require therapy and the benefit of therapy for both mother and infant outweigh the risk. The choice of antiretroviral therapy in pregnancy may be influenced by indication, past antiretroviral therapy exposure, drug resistance, effects of pregnancy on the pharmacokinetic of the drugs and factors influencing safety and adherence treatment. In our study, treatments were well tolerated by both mother and infant.
Conclusion: Though treatments seem well tolerated physicians should carefully prescribe antiretroviral therapy during pregnancy because of the potential risk of preterm birth.
Pharmacovigilance in Low-Resource Settings
PP056. Strengthening Pharmacovigilance System Through Leveraging Resources from Public Health Programmes in Nigeria
A.I. Osakwe, U.G. Elemuwa, B.O. Akinola and C.K. Suku
National Pharmacovigilance Centre, NAFDAC, Abuja, FCT, Nigeria
Every medicinal product no matter how good its quality, poses a safety challenge. Safety monitoring of medicines becomes essential for effective use of medicines and provision of high quality healthcare in any country. However, Pharmacovigilance, an integral part of healthcare delivery, is often underfunded in many countries. The National Pharmacovigilance Programme in Nigeria was established in September 2004 with no statutory means of funding. To improve healthcare delivery through safety monitoring of medicines, it is pertinent that resources be made available to conduct Pharmacovigilance activities. It is in realization of this need that the 2009 WHO meeting of centres participating in international drug monitoring held in Morocco, called for concerted effort by all stakeholders in sourcing funds for pharmacovigilance.[1] The National Pharmacovigilance Centre in response to this call and in its effort to mobilize resources to strengthen the fledgling pharmacovigilance system in Nigeria, has established collaborative relationships with relevant stakeholders such as public health programmes. These programmes are usually adequately funded and focus on mass distribution of medicines with inadequate systems in place to monitor the safety of the medicines they distribute. Through these collaborations, we have been able to develop a National Pharmacovigilance Curriculum for in-service training of healthcare providers. Furthermore, we have trained over 2700 senior cadre health care providers (HCPs) comprising of doctors, pharmacists and nurses, over 2300 community health extension workers and community health officers, and over 3700 Patent and Proprietary Medicine Vendors in the public and private sectors of the country. These trainings are aimed at improving awareness on patient safety issues, enhancing ownership of the programme by HCPs and institutionalization of pharmacovigilance into the different levels of healthcare delivery. This improved safety awareness will benefit the healthcare system by generating evidence based safety data from pharmacovigilance activities that will consequently minimize risks associated with the use of medicines and ultimately improve acceptance for the public health programmes. This presentation therefore discusses how the National Pharmacovigilance Centre was able to make Pharmacovigilance activities more robust in Nigeria by leveraging public health programme resources.
PP057. Establishing a Pharmacovigilance Database in Romania: Practical Value
A.M. Farcas,1 T. Chiorean,2 D. Leucuta,1 R. Chereches 2 and M. Bojita 1
1 University of Medicine and Pharmacy ‘Iuliu Hatieganu’, Drug Information Research Center, Cluj-Napoca, Romania; 2 Babes-Bolyai University, Center for Health Policy and Public Health, Cluj-Napoca, Romania
Background: In Romania there is currently no pharmacovigilance database that can be used for in-depth analysis of adverse events and timely communication of safety issues except the one maintained by the National Medicines Agency.[1]
Objectives: We aimed at developing a database to record the adverse drug reactions (ADRs) collected at a university based Drug Information Research Center (DIRC) that coordinates a local pharmacovigilance program. This adverse drug reaction data storing and management system is meant to allow for the retrieval of data for regular evaluation of patterns of ADRs and further dissemination with the final goal of achieving, on the one hand, better individual care in the hospital setting and, on the other hand, for conducting advanced research.
Methods: Stimulated spontaneous reporting is the method used for the detection of ADRs in two internal medicine departments from two secondary care academic teaching hospitals. The ADRs collection is paper based, a structured ADR form being filled out by the treating physicians when an adverse event is identified. All the ADRs collected are impartially evaluated by an independent group of trained pharmacists and pharmacologists.
Results: The database includes all the aspects that characterize an ADR in a certain patient. (e.g. causality, preventability, severity, outcome, type of ADR, risk factors, drug interactions). Auxiliary databases such as ICD-10, ATC codes and the MedDRA terminology are being used. The database has been in operation for a year, during which approximately 250 ADR case reports have been evaluated and entered. All available adverse drug reaction related medical data are recorded in order to provide secure, real-time, patient-centric information needed to clinical decision-making and ADRs avoiding by providing the easy access to a patient’s medical record and to information on previous adverse events reports. Once the data have been entered different queries can be performed, accordingly to our developed routines for ADRs analysis. The database offers descriptive statistics on several key parameters. The causes for ADRs can also be quantified.
Conclusions: The database created provides a comprehensive and detailed documentation of serious, but also minor ADRs. Using a prospective method for the collection of ADRs, the data collected reflects daily practice, including off-label use of drugs, self-medication but also management of ADRs. By proper and impartial evaluation of ADR case reports, the database can be used for drug utilization and drug safety research.
PP058. Knowledge of Healthcare Professionals to Report Adverse Drug Reaction in Nepal: A Preliminary Study
S. Kc,1 P. Tragulpiankit,1 S. Gorsanan 2 and I.R.Edwards 3
1 Faculty of Pharmacy, Mahidol University, Bangkok, Thailand; Bir Hospital, Kathmandu, Nepal; 2 Faculty of Pharmacy, Siam University, Bangkok, Thailand; 3 Uppsala Monitoring Centre, Uppsala, Sweden
Background: In spite of under-reporting as a major limitation globally, spontaneous reporting system (SRS) remains the most widely used method to report adverse experiences about drugs.[1,2] Knowledge and attitude of healthcare professionals plays vital role in terms of adverse drug reaction (ADR) reporting, whereas personnel and professional characteristics of healthcare professionals have weak influence.[3] Knowledge of healthcare professionals about the ADR and ADR reporting encourages them to report ADR.
Objective: To investigate the knowledge of healthcare professionals towards ADR reporting in Nepal.
Methods: We conducted a cross-sectional study among the healthcare professionals; doctors, nurses and pharmacists; working at two hospitals located at Kathmandu, Nepal. Self administered structured questionnaire were distributed randomly to the healthcare professionals. Content and face validity of the questionnaire was done by expert panel review. Construct validity of the questionnaire was also carried out. The questionnaire was designed as multiple choices (5 options). It had total of 23 questions. Each correct answer was given a score of ‘1’ whereas each wrong answer was given a score of ‘0’. Descriptive statistics were used to analyze the data.
Results: Of the 50 questionnaires distributed, 37 responded with an overall response rate of 74%. Among the respondents, 15 (40%) were doctors, 17 (46%) were nurses and 5 (14%) were pharmacists. 30% of the respondents were not aware of the National Pharmacovigilance Center. 24% of the respondents did not know what an ADR is, and 46% of the respondents were not aware of most common type of ADR. 57% of the respondents understood the term ‘serious adverse event’ and 49% of the respondents knew about the thalidomide tragedy. Only 14% of the respondents answered correctly about the Naranjo algorithm as an important tool to establish causality of an ADR and only 8% answered correctly about the types of ADR most important to report. Only 24% of the respondents answered correctly about spontaneous reporting as the most commonly used method for reporting ADR. The total mean score±SD was 12.5±4.1 for doctors, 9.2±3.9 for nurses and 13.4±1.5 for pharmacists out of maximum possible score of 23.
Conclusions: This study showed that healthcare professionals have limited knowledge about the ADR and ADR reporting. Educational and managerial intervention will be important in understanding pharmacovigilance and improving ADR reporting by healthcare professionals.
PP059. Provision and Accuracy of Safety Information on Package Inserts of Selected Registered Medicines in Sudan
S. Osman, Z. Mutasim, A. Suliman and Y. Hamid
National Medicines and Poisons Board, MOH, Sudan
Introduction: A post marketing surveillance program was established in Sudan in 2004 aiming at checking the quality of registered medicines. In 2010 a new round of the program has started. In this round, registered medicines have been divided into 15 pharmacological groups and every two months the program targets a group, and forty percent (40%) of the registered medicines belonging to that group is randomly selected, purchased, checked and analyzed. For the purpose of checking, a check list developed by the committee of human medicines is used which have a separate section dealing with the package inserts. This check list based on the Drug Information Sheets[1] and the General Requirements for the Registration of Pharmaceutical Products in Sudan.[2]
Between October and December 2010, 168 package inserts were revised to assess both the provision and accuracy of certain safety information includes precautions and warnings, side/adverse effects, interactions, contraindications and overdose. References used to assess accuracy of information were BNF, BNFC, FDA Approved Prescription Drugs, WHO Model Formulary, Martindale and Stockley’s Drug Interactions.
Results: Seventy four (44%) of the 168 package inserts checked gave no interactions. Overdose and precautions and warnings were not provided in 38% and 19% inserts respectively. Side/Adverse effects represented the most fully accurate (85%) amongst ingredients checked. Table I shows the provision and accuracy of safety information on the 168 package inserts checked.
Regulatory actions taken: Based on the results shown above, the following actions were taken by the National Medicines and Poisons Board:
-
1.
A special unit was established at the Registration Department aiming at comprehensively review of the package inserts both premarketing authorization and at renewal of registration.
-
2.
The General Requirements for the Registration of Pharmaceutical Products have been revised and updated with more emphasis on safety information on package inserts.
-
3.
158 products have been suspended and official letters were sent to their local agents urging them to complete and/or correct the information on their package inserts.
-
4.
Since there, a debate is still ongoing on whether to ask all the manufacturers and local agents of medicines to have their package inserts written in Arabic so as to make it more readable and understandable to patients.
Pharmacovigilance in Public Health Programmes
PP060. A Difference in ADR (Adverse Drug Reaction) Mortality Rate in Thai Tuberculosis Patients between Year 2008–2009
S. Wechwithan and P. Sriphiromya
Health Product Vigilance Center, Thailand
Background: Pharmacovigilance or surveillance of adverse drug reactions (ADRs) associated with medicines in Thailand is conducted through the passive surveillance: spontaneous voluntary reporting system by hospital pharmacists and healthcare professionals all country. Adverse drug reactions reports have been collected in national spontaneous reporting database called Thaivigibase since year 1985. In Thailand, we have public health program using medicine in AIDS, Tuberculosis (TB) control program which have collected the patients’ record routinely. Integrating public health program in AIDS or TB patients and spontaneous reporting system can receive ADRs mortality rate to those drugs and compare difference and characterization in each anti-tuberculosis drug group. This ADR mortality rate may reflect TB drug group safety surveillance system.
Objective
General objective
This study is aimed to compare difference in ADRs mortality rate in Thai tuberculosis patients, between year 2008–2009.
Specific objectives
Study Design: Descriptive observational study design is used for this study since the study has to retrieve national spontaneous reporting system and TB patient disease surveillance database from Bureau of Epidemiology at the specific time.
Materials and Methods: Adverse reaction reports of patients to antituberculosis drugs from Thaivigibase (national spontaneous adverse drug reactions database) and TB patient disease surveillance database from Bureau of Epidemiology during year 2008–2009 were retrieved and calculated. The pattern of spontaneous fatal adverse reactions to anti-tuberculosis drugs are described by analyzing the data from national spontaneous reporting system in Thailand between year 2008–2009.
Results: ADRs mortality rates to anti-tuberculosis drugs were 1.97 per 1000 patients in year 2009 compared with 4.35 per 1000 patients in year 2008. Stevens -Johnson syndrome and hepatitis resulting in fatal outcome were detected in patients taking rifampicin, ethambutol, isoniazid and pyrazinamide. Anaphylactic shock was observed in patients with injected streptomycin. Skin and appendages disorders was the most common adverse health effects reported.
PP061. Analysis of Characteristics about Drug Adverse Events Reports Received in KFDA during 2008–2010
J. Ha, Y. Kim and M. Chung
Clinical Research Division, National Institute of Food and Drug Evaluation, Korea Food and Drug Administration, Chungcheonbuk-do, South Korea
Objectives: This study aims to draw consideration factors to KFDA’s perspectives for post-marketing safety measures from the current situation on domestic AE reporting.
Methods: Design: safety monitoring, descriptive statistics, Setting: drug adverse events monitoring, Exposures or Interventions: reporting sources, reported suspicious drugs, Main Outcome Measures: reported number of adverse event cases, reported number of adverse events, proportion (%), Statistical Analysis: chi-square test.
Results: Owing to 15 RPVCs (Regional Pharmacovigilance Centers), the number of drug adverse events reports has been increasing dramatically, 7210 in 2008, 26 827 in 2009 and 53 854 in 2010. To manage these mass data, KFDA established the web-based database of reported drug adverse events (RAE-DB), which contains 165853 dataset until January 31 in 2011. Medical institutions were major sources for spontaneous reporting from 49.8% in 2008 to 72.0% in 2010. On the contrary, direct reports from consumers decreased, from 4% to 0.1 %. In 2009, antiviral agent was the most frequently reported as a suspicious drug class, because of H1N1 pandemic and intensive safety monitoring. But reporting pattern of 2010 came back to 2008’s similarly.
Conclusions: We confirmed the effectiveness of some actions for boosting of spontaneous reporting, and settled down the system for management and analysis of domestic drug adverse events reports data. Upon these, KFDA could find out the domestic reporting pattern, ratio and characteristics.
PP062. Tamoxifen-Duloxetine: Risk of Reduced Therapeutic Response of Tamoxifen
J. Mahe,1 G. Veyrac,1 J. Mathevet 2 and P. Jolliet 1
1 Service de Pharmacologie Clinique, Centre Régional de Pharmacovigilance, Institut de Biologie, CHU Nantes, France; 2 Pharmacie Matheve, Chavagnes en Paillers, France
Introduction: Tamoxifen, a selective estrogen receptor modulator has been approved for the treatment of advanced estrogen receptor positive breast cancer and for the recurrence. Tamoxifen is a prodrug; the formation of its active metabolite, endoxifen, is predominantly mediated by the cytochrome P450 CYP2D6. Plasma endoxifen levels are influenced by CYP2D6 polymorphisms and by potent CYP2D6 inhibitors use.
Aim: To report a case of a decreased efficacy of tamoxifen associated with the use of duloxetine, a potent reuptake inhibitor of serotonin (5-HT) and norepinephrine used for the treatment of major depressive disorder.
Methods:The case report concerns a 48-year-old female patient with a medical history of breast cancer. She has been treated with tamoxifen since 01/06/2007. She has tolerated tamoxifen relatively well except for moderately hot flashes. She started duloxétine three months later and she observed a better tolerance of tamoxifen with decreased hot flashes. In October 2010, a breast cancer recurrence was detected and tamoxifen was stopped. A surgery has been planned with a radical mastectomy and an ovariectomy. Duloxetine is continued with lower doses.
Results:Concomitant use of a CYP2D6 inhibitor has been reported in up to 30% of patients with breast cancer.[1] The selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs) are treatments for concurrent hot flashes (65% among women with breast cancer treated by hormone therapy) and depression (10–25% in women with breast cancer).[2,3] Some SSRIs are effective therapeutics for hot flashes, possibly causing higher prescription rates although it is a misuse.
Some SSRIs, as paroxetine and fluoxetine, are strong inhibitors of CYP2D6 and their use is contraindicated with tamoxifen: the studies show a decreased of 50% of plasma levels endoxifen with paroxetine or fluoxetine.[4] Duloxetine is considered as a moderate CYP2D6 inhibitor. If our patient is a poor CYP2D6 metaboliser, genetic tests to predict tamoxifen efficacy can be useful.[5]
To our knowledge, this is the first case to suggest a decreased efficiency of tamoxifen with duloxetine. This interaction is not listed in the Summary of Product Characteristics (SPC) of duloxetine or tamoxifen and not found in the French National Pharmacovigilance database.
Conclusion:The conflicting results of different studies[6] do not suggest a reduction of effectiveness of tamoxifen with the co-administration of CYP2D6 inhibitors. However, as a reduced effect of tamoxifen cannot be excluded, co-administration with potent CYP2D6 inhibitors should be avoid whenever possible and caution to the misuse.
PP063. Interaction between Levothyroxine and Ritonavir-Boosted Amprenavir in Human Immunodeficiency Virus Infected Patients
A. Ruellan,1 G. Veyrac,1 M. Lefebvre,2 B. Bonnet,2 C. Brunet François 2 and P. Jolliet 1
1 Service de Pharmacologie Clinique, Centre Régional de Pharmacovigilance, Institut de Biologie, CHU Nantes, France; 2 Service de Maladies Infectieuses et Tropicales, CISIH, Hôtel Dieu, CHU Nantes, France
Introduction: Protease Inhibitors (PIs), fosamprenavir and ritonavir are metabolized by cytochrome P450 3A4, involving these products in numerous drug interactions. Ritonavir may also interact with glucuronosyl transferase activity affecting plasma concentrations of drugs metabolized through this pathway.
Aim:We report two cases of hypothyroidism associated with the co-administration of fosamprenavir/ritonavir and levothyroxine.
Results:A 50-year-old man with HIV infection since 1989 was first treated with pentamidine diisethionate, zidovudine, and zalcitabine. Some immunological failures have been diagnosed in 1996, involving alternative treatments. In March 2006, he was treated with ritonavir, fosamprenavir and nevirapine. At the same time, for Basedow disease, an increase treatment of levothyroxine (until 325 mg) was ineffective and the patient has developed a hypothyroidism.
The second case concerns a 42-year-old woman patient with HIV infection since 1995. She was treated with ritonavir, fosamprenavir, and nevirapine since March 2005. She was also treated with levothyroxine since November 2006, for thyroid cyst. This patient underwent a thyroidectomy for a multinodular goiter, on February 2008, but TSH serum level increased to 65µUI/mL, with 100µg of levothyroxine. The stop of fosamprenavir and/or ritonavir (in one case, fosamprenavir was substituted for darunavir) and an adapted dosage of levothyroxine allowed to obtain TSH serum level normalization, one month later, in the two cases.
Discussion:Ritonavir reduces concentrations of other glucuronidated agents like ethinylestradiol and zidovudine.[1] Since thyroxine undergoes conjugation with glucuronic acid, thyroxine concentrations may have been reduced secondary to induction of glucuronosyl transferases by ritonavir and this effect have been significantly increased with the addition of fosamprenavir in our cases.
Fosamprenavir can also be an inducer of glucuronyl transferase and the co-administration with ritonavir results in addition of pharmacological effects.
Ritonavir is a more potent CYP3A4 inhibitor than amprenavir. The area under concentration-time curve (AUC) of amprenavir increases but the effect of the use of amprenavir on ritonavir levels is not studied. An increased induction of glucuronyl transferase with ritonavir can not be rule out.[2] We have not found other notification of hypothyroidism in the French National Pharmacovigilance database but perturbation of hormonal tests results in HIV patients treated with ritonavir and lopinavir has already been reported in the international literature.[2,3]
Conclusion:The addition of fosamprenavir with ritonavir increased the metabolism of levothyroxine and leads to its inefficacy. The lack of data should not be interpreted as a lack of interaction.
PP064. Implementing Effective PV in National Malaria Control Programme of DR Congo
Y.N. Lula,1 P.N. Ntamabyaliro,1 J.Y. Liwono,1 T.N. Mpiempie,1 S.B. Bazundama,1 G.K. Mesia,1 C.N. Nsibu 2 and G.L. Tona 1
1 Unité de Pharmacologie Clinique et Pharmacovigilance, Faculté de Médecine, Université de Kinshasa, Kinshasa, DR Congo; Centre National de Pharmacovigilance, Kinshasa, DR Congo; 2 Département de Pédiatrie, Cliniques Universitaires de Kinshasa, Faculté de Médecine, Kinshasa, DR Congo; Centre National de Pharmacovigilance, Kinshasa, DR Congo
Background:Malaria remains a major public health problems in DR Congo (DRC) accounting for an estimated 11% of all malaria cases in the WHO African Region in 2006. Fixed-dose combination of amodiaquine-artesunate was introduced as first-line treatment in 2005 by the National Malaria Control Programme (NMCP). Nevertheless, treatment compliance failed because of the occurrence in some case of severe adverse events and the lack of national pharmacovigilance (PV) system. In 2010 with the Global Fund support (GF), a pilot PV project was launched in ten sentinel sites of NMCP at Kinshasa, capital of DRC.
Objectives:To awake health practitioners on Artemisinin-based Combination Therapy (ACT) adverse drug reactions (ADRs) monitoring.
Methods:A PV project was launched at Kinshasa from September 2010 to April 2011. Ten sentinel sites were selected mainly on the basis of ACT availability provided by GF or according to regular consumption of ACT. Secondary, focal persons (physicians and pharmacists) belonging to these sites (at least 2 per site) and chosen by their staff were trained in PV through a workshop organized by National PV Centre (CNPV). Consciousness raising campaigns addressed to each sentinel site medical staff were held by CNPV. ADR reporting forms were made available to all sentinel sites. Finally, one supervision per week was conducted in each site to foster PV locally and gather ADR reporting forms.
Results:Thirty two focal persons were trained in detection, assessment, reporting and management of ADRs. The training course consisted on theoretical part including group discussions and experiences sharing, and practical part with real life examples ADR reporting, causality assessment and Vigiflow. 250 healthcare professionals of sentinel sites were sensitized to the necessity of PV, burden of ADRs and cases reporting. 213 supervisions were performed with the aim of stimulating spontaneous ADRs reporting and 122 ADR reporting forms were collected during this period.
Conclusions:PV is a necessity especially in the programs where deployment of new drugs are made in large scale or more quickly by donors. Through this methodology, it is possible to implement PV in poor-setting countries to ensure safety of these medicines and to improve patient compliance. This experience could be extending to others health programs and performing in all NMCP sites combined with active surveillance.
PP065. A Suspected Local Eruption due to Simethicone
G. Lakhoua, S. El Aidli, R. Daghfous and M. Lakhal
Centre National de Pharmacovigilance de Tunis, Tunis, Tunisia
Introduction:Simethicone is usually used alone or in combination with other drugs to reduce bloating, discomfort and pain caused by excess gas in the stomach or intestinal tract. Side effects of simethicone are usually, intestinal ones such as bloating, constipation, diarrhea, gas and heartburn. Cutaneous side effects with this molecule haven’t been reported. We report here, a case of a suspected local face eruption due to simethicone and notified to the Centre National of Pharmacovigilance of Tunisia (CNPV).
Case: MI, is 61-year old women with a family history of atopy. Indeed, her daughter has a nickel and a penicillin allergy. This patient was treated by Levothyrox® (Levothyroxine) for an hypothyroidism since 2002. For her dyslipedaemia, she took since 2002 Zovatin® (simvastatin). In December 2010, she received Simvax® (simvastatin) instead of Zovatin®. Two days after the beginning of the Simvax®, she developed a maculo-papular eruption on the face (front, cheeks). She stopped the drug two days later. The eruption disappeared the next day. After this episode, she took again the Zovatin® without any problem. On February 2011, she didn’t find Zovatin® and took for the second time Simvax®. The next day, she developed the same eruption on the front. She stopped the drug, and the eruption disappeared into three days. On March 2011, she took one tablet of Antilip®, the next day she developed again an eruption. She stopped the Antilip®, and the eruption disappeared 24 hours later.
Discussion:This patient has presented a face eruption twice after her took of Simvax®. She didn’t present anything with Zovatin®. Those two drugs contain simvastatin as active agent, the simvastatin couldn’t be involved in the face eruption. The responsibility of the excipients was suspected.
Two differences exist between the two formulations. The Simvax® contains simethicone and red iron oxide, which is a stain. We suspected the incrimination of simethicone in the apparition of the symptomatology. Analyzing the third episode of the occurrence of the eruption, we comfort our hypothesis since the Antilip® contains also the simethicone and not the red iron oxide. We recommended the contraindication of simethicone to this patient.
In literature we haven’t found any case of skin eruption after the intake of simethicone. This molecule is known to be not absorbed to the general circulation.
PP066. Peginterferon Alpha 2a Side Effects: A Retrospective Study
G. Lakhoua, S. El Aidli, A. Zaiem, S. Kastalli, I. Aouinti, R. Daghfous and M. Lakhal
Centre National de Pharmacovigilance de Tunis, Tunis, Tunisia
Objectives:Peginterferon alpha 2a is now recommended as a first-line treatment associated with ribaverin for chronic Hepatitis C virus infection and in monotherapy for Hepatitis B infection.
The aim of our study is to precise the type of peginterferon side-effects’ notified to the Centre National of Pharmacovigilance of Tunisia (CNPV).
Methods:Our retrospective study has concerned all the notifications of side effects associated with the administration of peginterferon alpha 2a, notified to the CNPV between December 2009 and December 2010. We found out 28 observations. We excluded three of them: one for lack of information and two were removed because another etiology was retained.
Twenty five cases were included in this study.
Results:Twenty five patients were included among them were 18 women and 7 men. Their age varied between 42 and 72 years. Association with ribaverin was found in 22 cases. The peginterferon was associated with another drug in ten cases. The score of imputability of peginterferon was I1 (doubtful) in 12 cases and I2 or probable in 13 cases. This score was superior to the drug associated in five cases and the same score in the other five cases.
We found cutaneous adverse effects in 13 patients, hematologic disorders in 5 patients, pulmonary and hepatic disorders in two cases each. We also found one case of vomiting. Association of several disorders such as cutaneous, neurologic and hematologic was found in 2 patients.
Conclusions:The Association peginterferon/ribaverin was prescribed in 17 cases of hepatitis C infection, and in one case of co-infection HIV/HVC. In 5 cases the indication couldn’t be précised. In literature, this association is recommended as the first-line treatment for HVC infections and co-infection HIV/HVC. The monotherapy with peginterferon alone is advisable in hepatitis B infection.
In our study the most frequent side effects noted were cutaneous ones. In those cutaneous lesions we haven’t found any case of reaction at the site of injection. Although, in literature, reactions at the site of injection, are the most frequent cutaneous side effects, associated with peginterferon.
The frequency of vomiting or flue syndrome is also high in literature, whereas in our study we didn’t found any except one case of vomiting. This under notification can be explained by the benignity of both the reactions at the site of injection and the flue syndrome. We have also noted that some patients received treatment to prevent the flue syndrome.
PP067. Use of Intensive Pharmacovigilance by Specialist Physicians: Prescription of Thalidomide in Venezuela 2009–2010
L.H. Valdivieso 1 and B.C. Ruiz 2
1 CEFARVI (Pharmacovigilance Center Faculty of Pharmacy, University Central of Venezuela), Venezuela; 2 Postgrade Health Surveillance of Drugs, National Institute of Hygiene Rafael Rangel, Venezuela
Introduction:In the 1950’s, thalidomide was better known for its teratogenic effect that the therapeutic effect on humans. Thalidomide causes malformations on the fetus. Now days, it has been discovered others properties of thalidomide as: angiogenesis inhibitor, immunomodulators and blocking Tumor Necrosis Factor (TNF). These properties have made out of Thalidomide a drug useful to treat other diseases as: HIV, Erythema Nodosum leprosum, autoimmune diseases, hematologic malignancies, solid tumors among others.
Objectives:Describe the therapeutic uses, prescription condition and use of intensive pharmacovigilance in Thalidomide’s prescriptions by 18 specialist physicians in the Miranda State, Capital District. Venezuela. 2009–2010.
Methods: 1. The research realized is not an experimental design. It is a qualitative researching field. The level of the study is exploratory. 2. Sample: 18 specialist physicians, whom are prescribers of thalidomide. The physicians, are registered in the ADB’s (bank of antineoplastic drugs) database. 3. Data collection: Application of a validated by experts.
Results:
-
1.
14 out of 18 specialists consulted, prescribe thalidomide for multiple myeloma treatment.
-
2.
More than the 40% of specialist physicians included used steroid drugs plus thalidomide.
-
3.
Thalidomide is used in a range doses of 100–300mg daily, well tolerated.
-
4.
Even all the physicians advises about side effects and risk exposition on pregnant women only 50% of the physicians uses the approval patient informed consent form. Additionally, 44% of the specialists used the intensive pharmacovigilance program.
Conclusions:
-
1.
Thalidomide has some properties: Antiangiogenic and immunomodulater; which is the reason of the therapeutical uses. Some fields of uses of thalidomide are: Oncology, hematology, Dermatology, and Clinic Immunology.
-
2.
Thalidomide is prescribed for the treatment of additional different diseases it had been approved by the Venezuela health authorities. In Venezuela, Thalidomide is authorized like service drug. Thalidomide is a drug of restrained access in Venezuela. Thalidomide is distributed to patients only by ADB and IVSS (Spanish Initials).
-
3.
The thalidomide prescription in Venezuela does not follow up an intensive pharmacovigilance program approved by Venezuela health authorities, where it define conditions and restrictions for a safe and efficient use of the thalidomide. Recently a new governmental resolution about the Good Practice of Pharmacovigilance will make compulsory the establishing of these programs. The results make evident the need of creating an educational campaign in order to alert the health care professionals about the importance of pharmacovigilance.
Cost-Effectiveness of Pharmacovigilance Systems
PP068. Cost-Benefit Analysis of Pharmacist Interventions Related to Determine Preventable Adverse Drug Reactions for Hospitalized Patients in Thailand
T. Uaviseswong,1 U. Chaikledkaew 1 and P. Tragulpiankit 2
1 Division of Social and Administrative Pharmacy, Department of Pharmacy, Faculty of Pharmacy, Mahidol University, Bangkok, Thailand; 2 Division of Clinical Pharmacy, Department of Pharmacy, Faculty of Pharmacy, Mahidol University, Bangkok, Thailand
Background: Drug related problems (DRPs) due to adverse drug reactions (ADRs) can lead to hospitalization, disability and death.[1] Pharmacist intervention has been one of the most common techniques to detect and help preventing ADRs. Although until now there have been many pharmacist interventions related to determine preventable ADR in Thailand, the question still remain whether these interventions are worth to be implemented in hospitals.
Objectives: This study aimed to assess the clinical and economic impact of pharmacist interventions related to determine preventable ADR prevention for hospitalized patients in Thailand using model-based approach.
Methods: Cost -benefit analysis was used to calculate costs and benefits using a decision tree model based on the perspective of healthcare providers. Three interventions (i.e., ADR monitoring program, alerting order system, and intensive monitoring program) were compared with no intervention scenario. Only direct medical costs were included. Probability and data were obtained from previous published studies. The result was presented as the benefit to cost ratio. Sensitivity analysis was applied to test parameter uncertainties.
Results: Compared with no intervention scenario, ADR monitoring program had the highest benefit to cost ratio (4.72 times) compared to alerting order system (1.82 times) and intensive monitoring (1.39 times). The one-way sensitivity analysis result showed that the benefit to cost ratio would be higher when increasing cost avoidance, rate of detected ADRs, and rate of preventable ADRs.
Conclusions: ADR monitoring program provided higher benefit than cost compared to alerting order system and intensive monitoring program. The results from this study could be used as the information to make decision which intervention should be implemented to prevent ADRs in hospitals.
Discussion: This study was the first to evaluate the cost and benefit of three pharmacist interventions related to determine preventable ADR. When compared with no intervention, the benefit to cost ratio in this study (4.72 times) was higher than that obtained from the study of Prommeenate W. in Thailand (1.12 times).[2] The limitation of this study was that all preventable ADRs were assumed to be prevented. In addition to cost-effectiveness information, strategy to provide the intervention, method to detect preventable ADRs and ADR monitoring time were needed to consider before implementing ADR monitoring program in hospitals.
Models for Predicting Drug Safety
PP069. From Quality to Safety by Using Quality by Design (qbd)
B. Aksu,1 A. Paradkar,2 M. De Matas,2 Ö. Özer,3 T. Güneri 3 and P. York 2
1 Santa Farma Pharmaceuticals, İstanbul, Turkey; 2 Institute of Pharmaceutical Innovation, University of Bradford, UK; 3 Department of Pharmaceutical Technology, Ege University, İzmir, Turkey
The FDA announced the amendments in the cGMP to bring the 21st century outlook on the issue. In 2003, the experts working on the Quality Topics within ICH created a vision for the future pharmaceutical quality system. Since the meeting, the key framework guidance documents ICH Q8(R1), Q9 and Q10 have been developed.[4] Within this framework, the concept of QbD was defined as an approach which covers a better scientific understanding of critical process qualities, designing controls and tests based on the scientific limits of understanding during the development phase and using the knowledge obtained during the life-cycle of the product to work on a constant improvement environment.[2]
Also the quality target product profile as defined in Q8(R1) is a summary of the quality characteristics or attributes of a product that ideally will be achieved and thereby ensure the safety and efficacy of a drug product. In this respect, achieving the quality drug product, will also mean achieving safety and efficacy product.[4]
QbD is a systemic approach to pharmaceutical development. Guidelines and mathematical models are used to ensure the establishment and use of the knowledge on the subject in an independent and integrated way. In this concept, a study was made to establish the tablet formulation containing the ramipril drug substance by the QbD approach,using different processes and formulation parameters via ANN program. For this reason, Ramipril tablets containing 5mg of drug substance were prepared by wet granulation method. Besides, using different binders, disintegrants and lubricants in distinctive ratios, 128 formulations have been prepared. Two batches were manufactured. The critical quality attributes were determined. The data evaluated by the INForm software.[1]
Optimization of data obtained by tablets prepared by different process and formulation variables, was conducted in this study with INForm V.4 ANN.[3] Once INForm ANN model was trained, the model was optimized by using optimum specifications based on pharmacopeial data. Min. and max. values to be applied for optimization in the program were determined, with consideration of values for critical quality properties obtained from the study result. Tablets prepared as optimized formulation and process analyzed and as a conclusion all the parameters defined as critical quality attributes were in the range of specification limits. In the study, as a conclusion of the evaluation of the multi-experiments performed by means of ANN programs, with regards to the impact of the formulation and process parameters, a huge amount of detailed data gained that could not obtained with the routine R&D experiments.
As a result, using QbD can be a key and systematic factor for achieving the quality, safety and efficacy of drug products.
Medication Error Reporting Schemes
PP070. Impact of Polypharmacy on Adverse Drug Reactions Among Geriatric Patients in Penang Hospital
Y.W. Kassab,1 M.F. Najjar,2 H.A. Abdulrazzaq,1 Y. Hassan,3 N. Abd Aziz 3 and R. Ghazali 4
1 Deaprtment of Clinical Pharmacy, Pharmacy School, USM, Malaysia; 2 King Abdullah International Medical Research Center, The Kingdom of Saudi Arabia; 3 Faculty of Pharmacy, UiTM, Selangor, Malaysia; 4 Department of Medicine, Pulau Pinang Hospital, Malaysia p ]Background: The global population of the aged will be one of the major challenges for both health care professionals and agencies.[1] Although a large volume of evidence confirmed the importance of taking several medications to treat multiple diseases in geriatric patients. However, many previous studies reported that polypharmacy, the concurrent use of five or more different prescription medications, was a significant cause of adverse drug reaction (ADRs), drug interactions, morbidity and mortality.[2–6]
Objectives: To assess the association of polypharmacy for ADRs and mortality rates among geriatric patients admitted to medical wards.
Method: a prospective, observational cohort design with convenient sampling was used for 400 patients in medical wards of Penang General Hospital, Pulau Pinang, Malaysia. The study was approved by the Clinical Research Committee (CRC) of the hospital. Geriatric patients were followed up from the time of their admissions until they were discharge, transferred to another ward or death. Patients admitted to one of the five medical wards of Penang hospital with any acute medical disease or conditions and aged 65 years old and above. Naranjo scale was used in current study to assess the causality of ADRs.
Results: no significant association found between socio-demographic characteristics of patients and the probability of ADRs occurrence, except for length of hospital stay and/or hospital readmission (p = 0.001). Based on Naranjo causality scale, there was a significant association between ADRs and polypharmacy therapy (p-value = 0.001, RR= 11.9, 95% CI = 5.8, 24.5) among geriatric patients. Additionally, the incidence of ADRs was increased significantly (p-value <0.001) with the number of medication used. Furthermore, significant association (11.8%, p = 0.003, OR: 3.28; 95% CI: 1.44, 7.44) between ADRs and mortality rate among geriatric patients.
Conclusion: geriatric patients are more related with polypharmacy which contributed to increase the incidence of ADRs and mortality rate. Reducing the number of medications prescribed to geriatric patients and highlight the importance of ADRs reporting.
PP071. Improving Yellow Card to Detect Medication Errors
L. Alj,1 R. Benkirane,1 S. Pal,2 S. Olsson 3 and R. Soulaymani 1
1 Moroccan Pharmacovigilance Centre, Rabat, Morocco;
2 World Health Organization. Geneva, Switzerland; 3 Uppsala Monitoring Centre. Uppsala, Sweden
Background: Pharmacovigilance centres have been recognized as a potentially rich and important source of medication error identification. Studies[1–3] have pointed out the lack of items on yellow card that would help pharmacovigilance centres to catch more information on medication errors from their reporting form.
Objective: The objective of this work is to pick up key elements to add in yellow card in order to catch medication errors information from reported adverse drug reactions to Pharmacovigilance centres.
Method: We take the opportunity of the medication error training course organized in Morocco as part of European Council funded Monitoring Medicines Project to collect suggestions from participants on items which will allow pharmacovigilance centres detecting medication errors through reported ADRs. For that purpose, we scheduled a working group during the course to handle this issue. Moroccan yellow card was used as basis for as model.
Results: Thanks to all suggestions, we pointed out key elements that could be added on the yellow card in order to detect ME from reported ADRs. These elements are related to patient, drug, adverse reaction and reporter.
Discussion: We outline the data elements that countries could consider for amending their own reporting form to detect medication errors. We also report the justification for adding each item. The yellow card developed following findings is just a model on which we implement participants recommendations.
Conclusion: The step of improving yellow card is key to assess preventability of adverse drug reactions by pharmacovigilance centres. Therefore, pharmacovigilance will take part in medication error detecting and preventing and thus play a major role in patient safety network.
PP072. The Role of Pharmacovigilance Centres in Medication Errors Management
L. Alj, R. Benkirane and R. Soulaymani
Moroccan Pharmacovigilance Centre, Morocco
Introduction: It is now admitted that pharmacovigilance centres are involved in detecting medication errors. In fact, several publications[1,2] revealed the input of pharmacovigilance centres in increasing patient safety.
Objective: The objective of this presentation is to point out the role of pharmacovigilance centres in managing medication errors through the Moroccan Pharmacovigilance Centre experience in this matter.
Method: It is a review of all actions taken by Moroccan Pharmacovigilance Centre to develop medication error activity and the results of efforts furnished to manage medication errors.
Results: Moroccan Pharmacovigilance Centre started to work on medication errors since 2006. Several actions have been implemented to foster patient safety culture and to promote medication errors reporting such as organizing awareness programs for health care professionals, conducting studies, setting up a medication error database and carrying out root cause analysis.
These actions resulted in increasing health care professionals’ interest in the issue of medication errors by initiating studies to collect medication errors and taking actions to prevent their occurrence. However, they do not all share their experience with us. In our daily work, we review all adverse drug reactions in order to assess their preventability. Even the limited number of medication errors in our database, we succeed to detect signal and make decisions in collaboration with regulatory authorities.
Conclusion: Pharmacovigilance centres are a real opportunity for developing and managing medication errors issue particularly when a dedicated organization dealing with patient safety is missing. In our country, Moroccan Pharmacovigilance Centre is considered as a reference in the field of medication errors thanks to the great efforts done to collect and prevent medication error occurrence and thus improving patient care.
PP073. Medication Errors in an Hospital Ward
C. Le Beller,1 M. Soyer,2 F. Bellenfant,2 A. Lillo Le Louët 1 and D. Journois 2
1 Centre régional de Pharmacovigilance, Hôpital Européen Georges Pompidou, Assistance Publique — Hôpitaux de Paris, France; 2 Service de Réanimation Chirurgicale, Hôpital Européen Georges Pompidou, Assistance Publique — Hôpitaux de Paris, France
In France, the medication errors were defined as “omission or unintentional action during the care process involving a drug which carries a risk or leads to an adverse effect for the patient”. The error can be “confirmed”, “potential” (error intercepted before the drug administration) or “latent” (risk of error).[1] In our university hospital there was no organisation to collect medication errors. Before extension of a medication errors management process in all clinical wards, we conducted a pilot study limited to the surgical intensive care unit (ICU). The objectives were to assess the feasibility of a process aiming to collect then analyse medication errors.
Methods: A group including one head nurse, a physician from the ICU and a pharmacist from the pharmacovigilance centre were assigned to collect and analyse every medication errors. This working group designed a specific reporting form. Before the beginning of this study, training courses on medication errors reporting were organised for nurses and physicians. The medication errors recording was organised without sanction against involved health professional.
Results: The first year of reporting (between June 7, 2010 to June 7, 2011) 55 cases of drug errors were reported, concerning 43 patients, 19 women and 24 men, with a mean age of 58 years +[19–86]. The reporters were nurses (29 cases), head nurse (7 cases), nurse and physician (3 cases) or physician (16 cases). Involved drugs were antibiotics and antifungal in 14 cases, cardiovascular drugs in 9 cases, heparins in 7 cases, insulin in 3 cases. There is a majority of established errors (47 cases), detected after or during drug administration, and 8 errors avoided before drug administration. Adverse consequences in patients were observed in 7 cases: 1 hemorrhagic shock leading to surgical revision, 2 digestive hemorrhages, 2 hypoglycemias, 1 hypovolemia and 1 thrombosis of dialysis circuit. Errors related to prescription (20 cases), administration (21 cases) or both (6 cases) were more frequent. A feedback experience was regularly performed to the nurse and medical teams in order to prevent errors and to improve the good use of drugs.
Discussion/Conclusion: The pilot study confirms the feasibility of the collection and analysis of medication errors in an hospital ward. According to the literature for the ICU,[2,3] the commonly involved drugs include antibiotics, heparins and insulin. The main steps concerned are prescription and administration. The limits were human resources.
Communication in Drug Safety
PP074. Safety of Atrovent® CFC-Free MDI (Metered Dose Inhaler): An Example of Protopathic Bias in Observational Cohort Studies
V. Osborne, D. Layton, E. Tong and S. Shakir
Drug Safety Research Unit, Southampton, UK; School of Pharmacy and Biomedical Sciences, University of Portsmouth, Portsmouth, UK
Background: A surveillance study was requested by regulators to monitor the introduction of Atrovent8 CFC-free MDI into general practice, with a focus on safety surveillance of selected adverse events in past users (switchers) and Atrovent® naïve users.
Objectives: To identify any unexpected adverse events associated with starting the CFC-free formulation of Atrovent® MDI.
Methods: An observational cohort study. Exposure data collected from dispensed prescriptions issued May 2004 – February 2005. Outcome data were requested from general practitioners by questionnaire, sent 4 months after patients’ 1st prescription dates. Incidence density rate ratios (+99%CI) for events in the 1st 3 months of exposure compared to 3 months prior to starting were calculated for subgroups defined by prior history of Atrovent® use. To minimise confounding, a matched pair analysis of a priori selected events, using within person data from individuals with the event of interest in either 3-month window, was performed to estimate risk ratios (+99% CI).
Results: The cohort consisted of 13 211 patients (median age 70 years, 50.1% female; 63.5% prior users (‘switchers’), 88.0% starting treatment in Autumn and Winter season 2004). Common respiratory clinical events tended to occur at higher rates after starting treatment than prior for switchers e.g ‘Lower respiratory tract infection’ (LRTI) [ID1/IDB= 1.45 (99% CI: 1.17, 1.81)], Asthma worse [ID1/IDB= 1.58 (99% CI: 1.00, 2.51)], dyspnoea [ID1/IDB= 1.37 (99% CI: 0.81, 2.30)]. Of these events only LRTI was significant for Atrovent® naïve patients [ID1/IDB= 1.42 (99% CI: 1.04, 1.95)]. In the matched analysis, risks of asthma worse and dypsnoea in switchers were non-significantly higher after starting, but conversely non-significantly lower for Atrovent® naïve patients.
Conclusions: The results of this study suggest possible effect modification of risk as a result of prior Atrovent® CFC MDI use and this should be taken into consideration when evaluating the risk benefit profile of these types of products. The unusual observation that the rate of LRTI was higher after starting treatment than prior in both subsets of patients might be explained by protopathic bias[1] whereby patients sought medical advice because of worsening respiratory function (associated with LRTI), and subsequently the diagnosis of LRTI was recorded upon starting Atrovent® CFC-Free MDI and thus associated with starting treatment. The findings for dyspnoea in the matched analyses indicate that neither Atrovent® naive or non naive patients had their condition worsen after starting treatment.
PP075. Active Surveillance of the Introduction of Atrovent® CFC-free MDI (Metered Dose Inhaler) into General Practice in England: Characteristics of Users
V. Osborne, D. Layton, E. Tong and S. Shakir
Drug Safety Research Unit, Southampton, UK; School of Pharmacy and Biomedical Sciences, University of Portsmouth, Portsmouth, UK
Background: Aerosol medications with chlorofluorocarbon (CFC) propellants are being phased out due to environmental concerns over the ozone layer. Alternative propellants have been developed for use in metered dose inhalers (MDI). An active surveillance cohort study was requested by regulators of the manufacturer to monitor the introduction of the CFC-free formulation of Atrovent8 MDI into general practice, with an interest in identifying characteristics of patients exposed (Atrovent® naïve or switchers) in the immediate post-marketing period in accordance with prescribing recommendations.
Objectives: To monitor the utilization of Atrovent® CFC-free MDI in general practice in England.
Methods: An observational prospective cohort study using Modified Prescription-Event Monitoring (M-PEM) design. Exposure data were collected from dispensed prescriptions issued May 2004 – February 2005. Demographic, outcome data (events reported 3 month prior to and post treatment initiation) and selected clinical baseline characteristics were requested from general practitioners (GPs) by questionnaire, sent at least 3 months after patients’ 1st prescription dates. Summary descriptive statistics were calculated.
Results: The cohort consisted of 13 211 patients (median age 70 yrs, 50.1% female). Of these 6.4% (n = 851) were children aged <12 yrs, of which 91.2% (n = 776) were aged <5 yrs. The majority of patients (n = 8390, 63.5% cohort) were prior users of Atrovent® CFC MDI. The most frequent indications for use were Chronic Obstructive Pulmonary Disease (COPD) (n = 8408, 63.6% cohort and only in adults) and asthma (n = 3161, 23.9% cohort). Starting doses for patient subgroups defined by age followed recommendations; patients aged >13 yrs started Atrovent® CFC-free MDI on 4–8 puffs per day (n = 5345, 43.2%). High dose oral steroid use was reported for 16.5% (n = 2179) of the cohort, and concomitant regular medication for patients respiratory disease was reported for 83.6% of the cohort (n = 11050).
Conclusions: The results of this post-marketing surveillance study indicate that Atrovent® CFC-free MDI is being used according to the licensed prescribing recommendations for use in general practice in England, as based on data from clinical development programmes.[1,2] In collecting information on baseline characteristics of patients newly prescribed Atrovent® CFC-free MDI in general practice, such data can be used to identify sub-groups of patients for whom limited (or no) clinical-trial data is available to inform on potential risks, such as children aged <12 yrs. It is also useful to facilitate examination of reported risks in different populations (Atrovent® naïve vs switchers) under ‘real-life’ clinical practice conditions.
PP076. Analysis of Vildagliptin Utilisation from Interim Prescription-Event Monitoring (PEM) Results: Focus on ‘Off Label’ use in Support of Risk Management
V. Osborne, D. Layton, C. Fogg and S. Shakir
Drug Safety Research Unit, Southampton, UK; School of Pharmacy and Biomedical Sciences, University of Portsmouth, Portsmouth, UK
Background: Vildagliptin (Galvus®; Novartis Pharmaceuticals UK Ltd) is licensed in the UK for the treatment of type 2 diabetes mellitus (T2DM) as dual oral therapy in combination with metformin, a sulphonylurea or a thiazolidinedione.
Objectives: To describe the utilisation characteristics of patients prescribed vildagliptin in the UK, based on an analysis of an interim PEM cohort, and to assess how the product is being used in relation to the summary of product characteristics (SmPC) at time of study.[1]
Methods: An observational cohort PEM study was conducted. Exposure data were collected from dispensed prescriptions issued by primary care general practitioners (GPs) between April 2008 and November 2009 (interim data lock point). Outcome data (indication, event, patient demographics and selected clinical characteristics) were collected by sending questionnaires (green forms) to GPs at least 6 months after the drug was first prescribed for an individual patient. Summary descriptive statistics were calculated.
Results: The interim cohort consisted of 1494 patients, of which 43.6% (n=651 patients) were reported to be female. Where age was specified, the median age for the cohort was 61 years (interquartile range: 53–70 years). There was no use reported in patients aged under 18 years. Vildagliptin is not licensed for use during pregnancy; one pregnancy occurred during treatment for T2DM though no further details on outcome were available on follow up. Where specified, primary reasons for prescribing treatment other than ‘diabetes mellitus’ and conditions related to diabetes mellitus (such as ‘glycaemic control poor’) were reported for 34 patients (2.3% of patients) including ‘intolerance to previous drug’ (n = 16, 1.1%) and ‘hospital referrals’ (n = 7, 0.5%). These reasons refer to free text responses from the GP as to why treatment was prescribed, so are not necessarily the actual conditions for which treatment was required. Where specified, 1.1% (16/1445) patients were prescribed vildagliptin outside of the normal recommended starting dose (i.e. 50–100mg/day).
Conclusions: This study has highlighted that few clinicians are prescribing this product outside the recommended terms of the licence and off label use appears to be low-one pregnancy occurred during vildagliptin use for T2DM and in some cases (1.1%) vildagliptin was prescribed outside the recommended starting dose. Drug utilisation studies are important in describing populations that may not have been adequately studied in development programmes and may be important in the post-marketing risk management of medicines. Overall, vildagliptin appears to have been used appropriately in this interim cohort.
PP077. Drug Utilisation Data for Seroquel XL: Results of a First Interim Modified PEM Study Report
A. Gilchrist, M. Davies, D. Layton and S. Shakir
Drug Safety Research Unit, Southampton, UK; University of Portsmouth, Portsmouth, UK
Background: Quetiapine fumarate, an atypical antipsychotic in an extended release (XL) formulation (SEROQUEL XLTM; AstraZeneca), was approved in the UK in September 2008 as treatment for schizophrenia and manic episodes in bipolar disorder (BD). The license was extended to include treatment of major depressive episodes in patients with BD; to prevent recurrence of BD in patients whose manic, mixed or depressive episode responded to Seroquel; and as addon treatment of major depressive episodes in Major Depressive Disorder (MDD).[1]
Objectives: To describe the utilisation characteristics of patients prescribed Seroquel XL based on analysis of an interim M-PEM cohort and to assess how the product is used in relation to terms of licence of marketing approval.
Methods: A post-marketing surveillance study using the observational cohort technique of Modified-Prescription Event Monitoring (M-PEM) is ongoing. Patients were identified from prescriptions (Rx) issued by primary care doctors from September 2008. Questionnaires sent 12 months after patient’s first Rx capture demographic, drug utilisation and event data. Summary descriptive statistics were calculated; ‘off label’ use was defined according to the summary of product characteristics (SPC) at time of study.[1]
Results: 10 848 M-PEM forms were sent, 5986 (55.2%) were returned of which 3276 (54.7%) were reviewed at interim, giving a valid cohort of 2236. Median age was 43 yrs (IQR 33–56), 915 (40.9%) patients were male; 11 (0.5%) were aged <18 yrs and 280 (12.5%) were aged >65 yrs. Licensed primary indications of BD, schizophrenia and depression were reported for 52.1 % of the cohort ( 1165/2236). [Primary indication refers to 1st reported indication (not in order of clinical importance)]. Non-licensed primary indications included anxiety (n=166, 7.4%), personality disorder (n = 82, 3.7%), and dementia (n = 57, 2.6%). 68.8% of the cohort were prescribed a start dose of 50–300mg/day, as per the SPC. There were 835 reasons for stopping Seroquel XL reported for 683 pts; most frequently reported event/clinical events were ‘not effective’ (n= 129, 15.4%) and drowsiness/sedation (n = 57, 6.8%). 5 pregnancies were reported.
Conclusions: The interim results of this post-marketing surveillance study indicate there is some prescribing of Seroquel XL outside the terms of licence, including SPC recommendations for age and indication.
PP078. FDA Final Rule on IND Safety Reporting: Impact to Your Clinical Studies
S. Van Doren
BioSoteria, Inc., Emeryville, CA, USA
The FDA announced changes to the regulations on IND safety reporting, which went into effect on March 28, 2011, (although it may not be enforced until September 29, 2011).
This final rule which codifies the FDA’s expectations for timely review, evaluation, and submission of relevant and useful safety information of drug and biologic products subject to an investigational new drug (IND) application. The final rule amends parts 312 and 320 of FDA regulations by revising the requirements for IND safety reporting and for bioavailability and bioequivalence studies. The IND regulation changes involve: clarification of several definitions, what safety information to report and when (including additional safety information required for expedited reporting) and various other clarifications related to IND safety reporting.
The new rule requires that certain safety information now be reported within 15 days of becoming aware of an occurrence. These reports include findings from clinical or epidemiological studies that suggest a significant risk to study participants; serious suspected adverse reactions that occur at a rate higher than described in the IB; and SAEs from bioavailability and bioequivalence studies, among other changes. Along with this final rule, the FDA issued a draft guidance for industry and investigators that provides information and advice about the new requirements. Dr. Van Doren will review how these regulatory changes may impact your ongoing and future clinical trials.
PP079. Reliability of the Reported Ingested Dose of Acetaminophen for Predicting the Risk of Toxicity in Acetaminophen Overdose Patients
S.H. Zyoud,1 R. Awang,1 S. Syed Sulaiman 2 and S.W. Al Jabi 2
1 WHO Collaborating Centre for Drug Information, National Poison Centre, Universiti Sains Malaysia (USM), Penang, Malaysia; 2 Clinical Pharmacy Program, School of Pharmaceutical Sciences, Universiti Sains Malaysia (USM), Penang, Malaysia
Objectives: The present study examines the relationship between the dose of acetaminophen reported to have been ingested by patients and the occurrence of serum acetaminophen levels above the ‘possible toxicity’ line in patients presenting at the hospital after acetaminophen overdose. The prognostic value of patient-reported dosage cut-offs of 8g, 10g and 12g was determined.
Methods: This retrospective cohort study included patients admitted to the emergency department or hospital within 24 hours of acetaminophen ingestion. Serum acetaminophen concentrations were considered to be the gold standard, and specificity, sensitivity, and positive/negative predictive values were calculated from the reported ingested dose, to predict toxicity using the Rumack-Matthew nomogram (i.e. the ‘possible toxicity’ treatment line) and standard equations.[1,2]
Results: Of 305 patients identified, 291 met the study inclusion criteria, and 121 (41.6%) had serum acetaminophen concentrations above the ‘possible toxicity’ treatment line. The range of patient-reported acetaminophen ingested was 1–75g, with 185 patients (63.6%) reporting ≥8g. 118 patients (97.5%) who reported ingesting ≥8g had serum acetaminophen concentrations above the ‘150-line’, compared with only 3 patients (2.5%) who reported ingesting < 8 g (p < 0.001). The positive predictive value of a patient-reported dose ≥8 g for predicting serum acetaminophen concentrations above the ‘possible toxicity’ treatment line was 63.78%, with a negative predictive value of 97.17%. The sensitivity of patient-reported doses ≥8 g was high (97.52%), but with low specificity (60.59%). The sensitivity of patient-reported doses ≥10g was also high (89.26%) with low specificity (65.29%), while the sensitivity of ≥12g dose was low (61.16%) with high specificity (86.47%).
Conclusions: Patient-reported doses of acetaminophen are good risk indicators for acetaminophen overdose patients in Malaysia. Patient-reported ingestion of ≥8 g (as a cutoff dose) had a higher sensitivity than ≥10g or ≥12g. The results of this study have important implications for toxicity risk evaluations in areas with poor serum acetaminophen assay availability.
PP080. Adverse Drug Events in Hospitalized Patients with Acetaminophen Overdose Treated with Intravenous N-Acetylcysteine
S.H. Zyoud,1 R. Awang,1 S. Syed Sulaiman 2 and S.W. Al Jabi 2
1 WHO Collaborating Centre for Drug Information, Clinical Toxicology Program, National Poison Centre, Universiti Sains Malaysia (USM), Penang, Malaysia; 2 Clinical Pharmacy Program, School of Pharmaceutical Sciences, Universiti Sains Malaysia (USM), Penang, Malaysia
Objectives: Intravenous N-acetylcysteine (IV-NAC) is widely recognized as the antidote of choice for acetaminophen overdose.[1] However, its use is not without adverse drug reactions (ADR) which might affect therapeutic outcome or lead to treatment delay.[2,3] The aims of this study were to investigate the type and incidence of ADR induced by IV-NAC in patients treated for acetaminophen overdose and to assess the causality of individual ADR to IV-NAC using Naranjo’s algorithm.[4]
Methods: This is a retrospective study of patients admitted to the hospital for acute acetaminophen overdose over a period of 5 years (January 1, 2004 to December 31, 2008). The primary outcome of interest in this study was the occurrence of ADR during NAC administration. The probability of an ADR was assessed using the Naranjo algorithm, which consists of 10 questions), and has been used to determine the likelihood that an ADR was related to a specific medication. The Naranjo score takes into account other possible influences such as drugs or disease. The association scores were: ≥9 = “definite”, 5 to 8 = “probable”, 1 to 4 = “possible” and 0=“doubtful”.[4]
Results: During the study period, 305 patients with a diagnosis of overdose of paracetamol-containing compounds were admitted to the hospital for monitoring and treatment. Different types of ADR occurred in 137 patients (137/305; 44.9%). Of those patients who had an ADR, 98 (98/137; 71.5%) had been treated with IV-NAC and 39 (39/137; 28.5%) had not (p< 0.001). Comparison of different ADR in all patients showed that the following ADR were significantly associated with IV-NAC administration: nausea (p = 0.004), vomiting (p< 0.001), flushing (p< 0.001), rash (p< 0.001), pruritus (p <0.001), chest pain (p = 0.001), bronchospasm (p = 0.015), coughing (p = 0.017), headache (p<0.001), dizziness (p<0.001), convulsion (p = 0.035) and hypotension (p = 0.001). Based on Naranjo’s algorithm, 226 events were judged to be NAC-related — 31.1% probably and 67.9% possibly drug-related. None of the events were definitely drug-related (table I).
Conclusions: Adverse drug reactions to IV-NAC were common among patients with acetaminophen overdose but mostly minor, and that all reported adverse reactions were easily managed.
PP081. “Serious” Cutaneous Reactions with Protein Kinase Inhibitors
E. Bondon Guitton,1 E. Faye,1 P. Olivier Abbal,1 H. Bagheri,1 J. Montastruc 1 and The French Association of Regional Pharmacovigilance Centres 2
1 Laboratoire de Pharmacologie Médicale et Clinique, INSERM U1027 Equipe de PharmacoEpidémiologie, Faculté de Médecine de l’Université de Toulouse, Toulouse, France, and Service de Pharmacologie Clinique, Centre Midi-Pyrénées de PharmacoVigilance, de PharmacoEpidémiologie et d’Informations sur le Médicament, Centre Hospitalier Universitaire, Toulouse, France; 2 The French Association Of Regional Pharmacovigilance Centres, Lyon, France
Objectives: Results from EMIR study (Effets indésirables Médicamenteux Incidence et Risque), performed in 2007 in France, showed that the incidence of Adverse Drug Reactions (ADRs) who required hospital admission was the highest with vitamin K antagonists and then antineoplastic drugs.[1] Currently, several antineoplastic drugs, orally administered, could be taken at home (ambulatory care). As far as we know, no study described “serious” ADRs with these specific antineoplastic drugs. By using data of spontaneous reporting in France, we aimed to detect, quantify and analyze characteristics of “serious” ADRs related to oral antineoplastic agents use.
Methods: We used the French Pharmacovigilance Database to select “serious” ADR reported from 1st January 2008 to 31st December 2009 with all oral antineoplastic drugs. A “serious” ADR was defined as any untoward medical occurrence that at any dose results in death, requires hospital admission or prolongation of existing hospital stay, results in persistent or significant disability/incapacity or is life threatening.
Results: We found 589 cases of “serious” ADRs with antineoplastic drugs orally administered as “suspect” drugs. Protein kinase inhibitors (PKI) were most frequently involved drugs (271 cases, 46%) with 383 “serious” ADRs reported. “Serious” ADRs with PKI were various but most of them were cutaneous (19%) and particularly skin eruptions (51%, without Stevens-Johnson Syndrome) followed by hand-foot syndrome (18%). Risk to present “serious” cutaneous ADRs was highest in men (62%), in patients 61 years old or exposed to sorafenib (45%). PKI was withdrawn in almost half of patients (43%). Most of patients received a symptomatic treatment (78%). Evolution was favourable in 58% of cases.
Conclusions: Initiation of a PKI should be performed with a systematic cutaneous surveillance, particularly in men. An early diagnosis and management of the cutaneous ADRs could limit their seriousness and avoid the withdrawal of PKI.
PP082. Pharmacovigilance in Kyrgyzstan
S. Moldoisaeva and A. Zurdinov
Basic and Clinical Pharmacology Department, Kyrgyz State Medical Academy, Bishkeke city, Kyrgyzstan
Background: Kyrgyzstan has been official member of WHO Programme for International Drug Monitoring since 2003. The role of the National Pharmacovigilance Centre in our country is delegated to Information centre of the Drug Supply and Medical Equipment Department under Ministry of Health. At the beginning of pharmacovigilance implementation process in Kyrgyzstan this centre was supported by WHO Regional Office for Europe (WHO/Europe) and they achieve much success: Monthly information brochures for physicians and pharmacists were published by Centre, clinical pharmacologist’s activities were supported, seminars and trainings for medical workers conducted. Spontaneous report/Yellow Card system had been approved by Ministry of health’s order #535 from 25/12/02. After financing support finished pharmacovigilance implementation process came to naught and now we have problem in ADRs monitoring system.
Objectives: Investigating basal level of medical worker’s (physicians, pharmacists and nurses) awareness on pharmacovigilance.
Methods: Survey by special developed different questioners for every category of medical workers including questions about basal knowledge of ADRs, methods of their monitoring and medical worker’s adherence to ADRs monitoring. We collected 1195 questioners from physicians, 200 questioners from pharmacists and 1000 questioners from nurses.
Results: 66, 94% of doctors, 48,2% of nurses and 80, 1 % of pharmacists were faced with ADR’s in their practice. Only 49% of doctors, 22% of nurses and 34% of pharmacists register these events in medical documents. And only 9% of these events were fixed as “yellow cards”. 95, 9% of doctors, 74,3% of nurses do not know about Drug Supply and Medical Equipment Department under Ministry of Health as a National Pharmacovigilance Centre.
Conclusions: ADR’s are commonly encountered problem in Kyrgyz Republic. In most cases medical workers prefer do not register these ADR’s. Medical workers have lack of information about ADR’s monitoring system and in particular about “yellow card” system. Activity of National Pharmacovigilance Centre represented by Drug Supply and Medical Equipment Department under Ministry of Health is not enough.
Discussion: Pharmacovigilance system in Kyrgyz Republic needs modernization. Now in KR only medical workers involved. Marketing Authorization Holders are not involved in this process. Information deficiency is one of the big reasons of low adherence of medical workers.
PP083. Pharmacovigilance Committee Activities of the Association of Research-Based Pharmaceutical Companies after the Release of Pharmacovigilance Regulation in Turkey
A. Erkahraman,1 Z. Nefesoglu 2 and S. Epceli 3
1 AIFD; 2 AIFD Pharmacovigilance Committee Chairman on behalf of AIFD Pharmacovigilance Committee, Novartis;
3 AIFD Pharmacovigilance Committee Co-Chairman on behalf of AIFD Pharmacovigilance Committee, Johnson & Johnson
Association of Research-Based Pharmaceutical Companies (AİFD) was established in 2003, by research-based pharmaceutical companies operating in Turkey and has founded its Pharmacovigilance Committee in 2004 which includes members from each member company. The objective of the
AIFD is to enable Turkish people to access new and original drugs and provide effective solutions to the health conditions in our country. Throughout these years the AIFD Pharmacovigilance committee had many activities. One of these activities was Pharmacovigilance Brochure which was distributed to all member company staff. The aim of the brochure was to inform company personnel about adverse event reporting procedures.
Another activity was the short movie which was shot to train the member company staff about adverse event reporting. This movie enabled homogenius training of all member company personnel. Pharmacovigilance Committee has an important role in establishment of communication between Turkish Health Authority, Turkish Pharmacovigilance Society and AIFD. The committee continuously provides feed back to Turkish Health Authority regarding changing regulations in this dynamic field.
Data from 18 AIFD member companies were collected to evaluate the number of spontaneous reports after the release of the regulation regarding pharmacovigilance in 2005:
-
• Total number of spontaneous reports (SR) increased from 2005 to 2010. Number of SRs received was 251, 592, 947, 1499, 2089, 3051 respectively.
-
• Total number of pregnancy reports increased from 2005 to 2010. Number of pregnancy reports received was 10, 12, 117, 301, 461, 1076 respectively.
-
• % 416 increase was observed in number of SRs received from physicians in 2010 when compared to 2005 (181 reports in 2005 to 934 reports in 2010)
-
• % 1525 increase was observed in number of SRs received from pharmacists in 2010 when compared to 2005 (4 reports in 2005 to 65 reports in 2010)
-
• % 7037 increase was observed in number of SRs received from patients/caregivers in 2010 when compared to 2005 (29 reports in 2005 to 2070 reports in 2010)
As seen from the above figures, there was a dramatic increase in the number of SRs received by the member companies following release of regulation in 2005. Training activities of Turkish Health Authority, Turkish Pharmacovigilance Society and pharmaceutical companies might have played a role in this increase in number of reports. In conclusion, it seems that AİFD Pharmacovigilance Committee had an important contribution to the awareness of the system in Turkey and the Committee aims to continue its pharmacovigilance activities in Turkey.
PP084. Selective Serotonin Reuptake Inhibitors and Gastrointestinal Bleeding: A Meta-Analysis
A. Carvajal, C. Treceño, M. Sáinz, iI. Salado, N. Jimeno, V. Velasco and L. Martín Arias
Centro de Estudios sobre la Seguridad de los Medicamentos. Universidad de Valladolid, Spain
Background: Selective serotonin reuptake inhibitors (SSRIs) were associated with upper gastrointestinal bleeding in an epidemiological study, and since then, 15 additional studies addressing this topic have been published. Albeit four studies found a strong significant association between SSRIs and upper GI bleeding (a risk value higher than 2) others found no association at all; thereby, the association remains a matter of controversy. The widespread use of antidepressants, particularly SSRIs, makes even small risks account for a large number of cases, converting this problem into an important public health issue. This fact, along with the lack of consistency of the results so far obtained, has arisen a great interest on this subject.
Objective: To learn the risk of upper gastrointestinal bleeding associated with the use of SSRIs.
Methods: We systematically searched MEDLINE (1966–June 2011) and manually reviewed references. Observational studies, whether case-control or cohort studies assessing the risk of interest were included. Study selection, data abstraction were independently conducted in duplicate. Heterogeneity analysis was performed; overall estimates were calculated according to the Wolf method.
Results: Fifteen epidemiological studies assessing upper gastrointestinal risk in relation to SSRIs were retrieved; one presenting information non comparable to the others was not included. All in all these 15 studies comprise 853 744 patients. The overall adjusted estimate for the association of interest was 1.87 (95% CI, 1.76, 1.99). Numeric heterogeneity test was statistically non significant; however, in the Galbraith plot a few studies appeared as different. When considering the prospective or retrospective character of the study, the corresponding estimates were 1.95 (95% CI, 1.83, 2.08) and 1.31 (95% CI, 1.08, 1.58). Sensitivity analysis showed that none of the individual studies accounted for more than an 8% of the overall estimate.
Discussion: Since all studies were carried out in different periods, in different geographical areas and healthcare settings, with different designs and different ways of collecting information, the explanation of the different individual estimates may lie on this heterogeneity; nevertheless, retrospective or prospective character seems to be a remarkable factor of heterogeneity; thus, only 1 out of 4 prospective studies published so far found a significant risk while, in the retrospective studies, it was 9 in 12 which found a significant risk; moreover, analysis restricted to those prospective studies almost yielded to a mild association. In conclusion, it seems that the association found is milder than the one identified in a first step.
PP085. Therapeutic Drug Monitoring and Pharmacogenetic Tests: New Tools to Prevent Drug Side Effects
E. My Elhassan, F. Houda, E. Afaf and H. Farid
Department of Pharmacology Faculty of Medicine Casa, Morocco
Background: The interindividual variability to the standard dose of a given drug remains a major problem in clinical practice. An important part of the variability in drug response may be related to genetic factors through modulation of drug pharmacokinetics and/or pharmacodynamics.
Aims: The aim of this article is to provide a review of the literature and describe how to apply and interpret therapeutic drug monitoring (TDM) and certain pharmacogenetic tests.
Methods: Literature review, using MeSH system and Pubmed system. Selection of articles in English from 1991 January to 2011 January.
Results: TDM and pharmacogenetic tests play a major role in minimizing adverse drug reactions and enhancing optimal therapeutic response. The response to medication varies greatly between individuals, according to genetic constitution, age, sex, co-morbidities, environmental factors including diet and lifestyle, and drug-related factors such as pharmacokinetic or pharmacodynamic drug-drug interactions. Most adverse drug reactions are type A reactions, and represent one of the major causes of hospitalization, in some cases leading to death. However, they may be avoidable to some extent if pharmacokinetic and pharmacogenetic factors are taken into consideration. An algorithm on the use of TDM and pharmacogenetic tests to help characterize adverse drug is presented.
Conclusion: Most of side effects drugs can be avoided if pharmacokinetics and pharmacogenetics factors are taken in account. Although, in the scientific community, differences in drug response are increasingly recognized, there is an urgent need to translate this knowledge into clinical recommendations.
PP086. Benign Intracranial Hypertension Associated to Progesterone Utrogestan: About One Case
A. Elrherbi, M.E. Elkarimi, H. Filali, A. Tazi and F. Hakkou
Pharmacology Departement of Chu Ibn Rochd Casablanca, Morocco
Objective: Reporting a case of benign intracranial hypertension which occur with an hormonal therapy by progesterone utrogestan®.
Patient and methods: A 27 years old woman pregnant in her 16th week of amenorrhea received for two months 200mg/day of progesterone utrogestan® indicated for first trimester bleeding presented headache, vomiting, and a bilateral papilloedema grad III at the eyeground. An exhaustive biologic and morphologic assessment allows to eliminate infectious, vascular, and tumoral causes of this ICHT and to suspect the role of progesterone therapy. After utrogetan® discontinuation the evolution was spectacularly favorable with disappearance of all neurologic symptoms without any corrector treatment. The case was reported to the pharmacovigilance unit where it was analyzed, discussed and recorded.
Results: Using the WHO’s method of drug side effects imputability to analyze this Adverse event, we found I3 score for the intrinsic imputability and B2 score for extrinsic imputability.
Conclusion: Benign Intracranial Hypertension BICH or pseudotumor cerebri is defined as an elevation of the cerebrospinal liquid pressure in the absence of an expansive intracranial processus, a cerebral venous sinus thrombosis or a hydrocephaly. It might be drug induced as in the case reported here, where the progesterone therapy was incriminated. A severe evolution is possible with vision loss by an optic atrophy. The treatment consists of drug discontinuation with an eventual excess weight reduction and high dose corticotherapy. The evolution is characterized by a rapid recovery; surgical treatment is reserved to the rare rebellious cases.
Causality Assessment in Pharmacovigilance
PP087. A Recurrent Drug Rash with Eosinophilia and Systemic Symptoms
N. Fathallah,1 C. Jeddi,2 R. Slim,1 C. Belajouza,2 R. Nouira,2 C. Ben Salem 1 and K. Bouraoui 1
1 Department of Clinical Pharmacology and Research Unit99/UR/08-64, Faculty of Medicine, Sousse, Tunisia;
2 Department of Dermatology, Farhat Hached Hospital, Sousse, Tunisia
Introduction: Drug rash with eosinophilia and systemic symptoms (DRESS) is characterized by fever, rash and internal organ involvement after exposure to certain drugs. Most of the aromatic anticonvulsants, such as phenytoin, phenobarbital, and carbamazepine can induce DRESS. Nonaromatic drugs such as lamotrigine and valproate are known to be more safe than aromatic anticonvulsants and are less responsible of DRESS.
We report here an occurrence of DRESS following exposure to valproate and recurring after phenobarbital intake.
Case report: A 54-year-old man without previous significant medical history had been diagnosed with brain tumor. He was treated by surgery and received valproate (400 mg daily). No other medications had been taken. Three weeks later, the patient was admitted to the hospital with fever and general eruption. The patient’s face was edematous and erythematous papules were scattered over his entire body. Lymph nodes were palpable. Laboratory findings showed hypereosinophilia and elevated liver enzymes. Viral serology was negative for hepatitis A, B, and C, cytomegalovirus and Epstein-Barr virus. On suspicion of DRESS, valproate was stopped. While clinical symptoms and laboratory findings improved progressively, phenobarbital was started. The patient developed again a generalized rash and fever few days after phenobarbital administration. The neurosurgeon decided to stop phenobarbital. Symptoms resolved few days later without complications.
Discussion: Drug rash with eosinophilia and systemic symptoms is a severe adverse reaction with high mortality rates. The aromatic anticonvulsants are the most frequently incriminated drugs.[1] In DRESS, discontinuation of the offending anticonvulsant is essential for improving the prognosis. Sodium valproate is rarely responsible for DRESS and it is generally a safe alternative for aromatic anticonvulsants.[2] As far as we know, DRESS syndrome cases related solely to the use of valproate have not been previously reported. Herein, we report the first case of DRESS primarily induced by sodium valproate and secondarily to phenobarbital. This case illustrates a possible cross-reactivity between valproate and phenobarbital, which are non aromatic and aromatic anticonvulsants, respectively.
Conclusion: Clinicians should be vigilant with the risk of recurrence of DRESS with anticonvulsant agents.
PP088. Codeine-Induced Generalized Dermatitis
N. Fathallah,1 B. Trimech,2 L. Boussofara,3 I. Ghali,3 R. Slim,1 C. Ben Salem 1 and K. Bouraoui 1
1 Department of Clinical Pharmacology and Research Unit 99/UR/08-64, Faculty of Medicine Sousse, Tunisia; 2 Department of Cardiology, Farhat Hached Hospital, Sousse, Tunisia;
3 Department of Dermatology, Farhat Hached Hospital, Sousse, Tunisia
Introduction: Codeine, a methyl morphine derivative, is a widely used opioid agonist. It is generally well tolerated as analgesic and antitussive. Cutaneous side effects to oral codeine are rare and few reports of generalized dermatitis induced by oral codeine are available. Herein, we report a case of codeine-induced generalized dermatitis.
Case report: A 71-year-old woman presented with a 3-day history of generalized pruriginous rash after antitussive preparation containing codeine.
The patient’s medical history was significant for hypertension treated with irbesartan (75 mg daily), chronic atrial fibrillation treated with digoxin (125 µg daily), diabetes treated with insulin and chronic renal insufficiency. All these medications were started more than seven years ago.
The rash developed one day after taking oral codeine (120 mg daily). On physical examination, the patient was apyrexial. Vital signs were within normal range. A generalized erythematous rash was noted. There was no lymph nodes or mucosal involvement. Laboratory investigations showed hypereosinophilia. Skin biopsy showed features suggestive of drug reaction. Codeine-induced generalized dermatitis was suspected and the drug was withdrawn. The rash improved rapidly.
Discussion: Side effects to codeine are rare. Nausea, vomiting, ataxia, swelling, and drowsiness are the most frequent reported adverse effects. Codeine has been also related to much more severe adverse events such as maculopapular eruptions, angioneurotic oedema, fixed drug eruption, bullous eruption, multiform erythema or toxic epidermal necrolysis.
Opium alkaloids adverse effects are frequently due to a non-specifically histamine release leading mainly to pruritis. However, immunological reactions are not rare. A delayed type IV allergic mechanism may be responsible of these adverse events.[1] According to the Naranjo probability scale, codeine-induced generalized dermatitis was possible.
The main problem for these patients is related to which opioid could be safely used in the future. Patients sensitised to codeine must avoid using morphine and other opioids with analogous chemical structure to them. Nevertheless they could employ other opium alkaloids structurally different such as pentazocine or tramadol.[2]
Conclusion: Clinicians should be vigilant to the possibility of dermatitis-induced by codeine.
PP089. Paradoxical Exacerbation of Rash Under Budesonide Therapy
N. Fathallah,1 S. Chatti,2 R. Slim,1 C. Belajouza,3 C. Ben Salem 1 and K. Bouraoui 1
1 Department of Clinical Pharmacology and Research Unit 99/UR/08-64, Faculty of Medicine Sousse, Tunisia; 2 Department of Occupational Medicine, Farhat Hached Hospital, Sousse, Tunisia; 3 Department of Dermatology, Farhat Hached Hospital, Sousse, Tunisia
Introduction: Topical corticosteroids are a significant milestone in dermatologic therapy. The most frequent adverse effects reported with this therapy are atrophy, striae, rosacea, perioral dermatitis, acne and purpura. Contact sensitization against corticosteroids is rare.[1] This adverse event is clinically underestimated and represents a particular problem of management.
Herein, we report a case of paradoxical exacerbation of skin eruption after budesonide therapy related to contact allergy to the drug.
Case report: A 48-year-old female was suffering from an erythemato-squamous eruption affecting her both hands. She was treated by topical corticosteroid (budesonide). One month after starting the treatment, she experienced a worsening of the rash and an extension of lesions. On physical examination, generalized erythemato-squamous plaques were affecting her face and her both arms. No mucosal involvement was present. There was no notion of any medication prior to the rash exacerbation. The patient was afebrile. All blood biochemistry results were within normal ranges. The patient was patch tested with standard panel and steroids. She had a (+) reaction to budesonide. A skin biopsy including the area with rash showed hyperkeratosis and superficial perivascular mixed dermatitis with lymphocytes and eosinophil infiltration suggestive of drug reaction. The patient was instructed to avoid budesonide therapy. The lesions improved progressively within three weeks later.
Discussion: Because of the chronology of events and worsening of the eruption despite continued use of topical steroids, an allergic contact dermatitis to steroids was strongly suggested. Contact hypersensitivity to topical corticosteroids may be a cause of persistence or worsening of skin diseases. While contact sensitisation to topical corticosteroids is generally rare, its risk increases with prolonged exposure and the selection of certain drugs. Non fluorinated corticosteroids such as hydrocortisone, hydrocortisone-17-butyrate, and budesonide result in a higher prevalence of corticosteroid contact allergy in comparison with fluorinated compounds. The intermittent use of topical corticosteroids is highly effective and bears little risks for the patients. Contact sensitization to topical corticosteroids has to be distinguished from hypersensitivity to other constituents. The suggested mechanism of contact hypersensitivity to topical corticosteroids is generally a type IV delayed hypersensitivity reaction. Results of patch testing is an effective screening agent for sensitivity to hydrocortisone and its derivatives.[2]
Conclusion: Adverse effects and safety of topical corticosteroids are often neglected. Physician should be vigilant of this adverse event.
PP090. Rituximab-Induced Leucocytoclastic Vasculitis: A Case Report with Brief Review of Literature
N. Fathallah,1 A. Alaoua,2 R. Slim,1 F. Bahri,2 C. Ben Salem 1 and K. Bouraoui 1
1 Department of Clinical Pharmacology and Research Unit 99/UR/08-64, Faculty of Medicine Sousse, Tunisia; 2 Department of Internal Medicine, Farhat Hached Hospital, Sousse, Tunisia
Introduction: Rituximab is an anti-CD20 chimeric monoclonal antibody. It is being increasingly used in the treatment of several autoimmune diseases.[1] Rituximab-induced vasculitis has been rarely reported. Herein, we report the first case of rituximab-induced leucocytoclastic vasculitis occurring in a patient with systemic lupus erythematosus.
Case report: A 16-year-old girl with initial diagnosis of systemic lupus erythematosus treated by prednisolone (20 mg daily). Routine laboratory investigations revealed thrombopenia (platelet serum levels at 21000/mm3) with positive anti-platelet antibodies. The patient was asymptomatic, she was hospitalised and treated by systemic corticosteroids (1mg per kg daily) and intravenous infusion of rituximab (1000 mg per week). Two days after the second infusion of rituximab, the patient presented with generalised rash. On physical examination, erythematous patches that rapidly changed to purpuric lesions were widespread to the entire body. Skin biopsy revealed typical features of leucocytoclastic vasculitis. Laboratory investigations showed platelet serum level at 70000/mm3, C3 and C4 were at normal ranges, viral causes of leucocytoclastic vasculitis were ruled out and were negative. Rituximab-induced vasculitis was suspected and rituximab therapy was suspended. Lesions totally resolved few days later.
Discussion: Although an increasing number of patients with various disease entities are being treated with rituximab, rituximab-induced vasculitis is rare. On our review of medical literature, there are only three reported cases of rituximab-induced vasculitis.[2] According to the Naranjo probability scale, rituximab-induced vasculitis is possible. The exact pathophysiology of this adverse event is still controversial. Antibody complex deposits into vessels and there is a cytokine release of tumor necrosis factor and interleukin 6.[2] The diagnosis is often challenging and it is important to rule out other possible etiologies such as other drugs, infectious diseases and autoimmune disorders. In patients suffering from autoimmune diseases, the diagnosis of rituximab-induced vasculitis is much more difficult to establish. This cutaneous side-effect mimic vasculitis frequently encountered in these diseases.
Conclusion: Among the side-effects associated with rituximab administration, rituximab-induced vasculitis should be recognized. Rapid withdrawal of the drug is the gold stone of the prompt management of the disease.
PP091. Reactivation of Pulmonary and Cutaneous Sarcoidosis after Treatment for Chronic Hepatitis C with Pegylated Interferon Alpha and Ribavirin
N. Fathallah,1 M. Zamy,2 R. Slim,1 K. Bouraoui,1 C. Ben Salem 1 and M. Biour 2
1 Department of Clinical Pharmacology and Research Unit 99/UR/08-64, Faculty of Medicine Sousse, Tunisia;
2 Pharmacovigilance Regional Center, Saint Antoine Hospital, Paris, France
Introduction: Pegylated Interferon alpha and ribavirin are widely used in the treatment of chronic hepatitis C virus. Several reports have suggested an association between combination therapy of pegylated Interferon alpha with ribavirin and sarcoidosis.[1] Herein, we report a case of reactivation of pulmonary and cutaneous sarcoidosis after treatment for chronic hepatitis C with pegylated interferon and ribavirin.
Case Report: A 49-year-old male was diagnosed to be HIV infected in 1992 and he had been receiving antiretrovirals since that time. He was also diagnosed infected with hepatitis C virus in 1995. In 2001, he was treated with pegylated interferon alpha and ribavirin, he was diagnosed few days later with both cutaneous and pulmonary sarcoidosis and the treatment was withdrawn.
Recently, the combined therapy of interferon alpha and ribavirin was reintroduced. The patient presented with a 10-days history of acute dyspnea, cough, recent weight loss, and fatigue. Physical examination revealed painful multiple, firm subcutaneous nodules, dry cough, inspiratory crackles on chest auscultation. Chest radiograph revealed bilateral diffuse micronodular infiltrates associated with mediastinal and hilar lymph nodes. Laboratory tests except for white blood cell count which was decreased to 2100/mm3, blood chemistry and liver enzymes were within normal ranges. High resolution chest and abdominal computed tomography with contrast medium revealed several mediastinal and hilar lymph nodes and bilateral micronodular infiltrate. A skin biopsy revealed non-caseating granulomas in the subcutaneous adipose tissue consistent with sarcoidosis. Serological test for Chlamydia pneumoniae was negative. Mantoux test (tuberculin sensitivity test) was also negative.
The treatment was discontinued. After months of follow-up, the patient remained totally asymptomatic.
Discussion: We report a case of reactivation of pulmonary and cutaneous sarcoidosis in the course of combined interferon and ribavirin treatment for chronic hepatitis C. Although the etiology of sarcoidosis remains unknown, possible causative agents are reported. Infections such as viruses or mycobacteria (especially Mycobacterium tuberculosis) and drugs have been reported. Hepatitis C virus may be a co-factor in the pathogenesis of sarcoidosis in patients receiving interferon.[2] In our case, sarcoidosis was developed first at the introduction of the combined therapy and symptoms resolved after drug withdrawal. On drug-rechallenge, reactivation of cutaneous and pulmonary sarcoidosis is an argument of drug-induced disease.
Conclusion: This case report is an unusual presentation of interferon-induced sarcoidosis. Cutaneous and pulmonary sarcoidosis may appear during a pegylated interferon and ribavirin combination therapy.
PP092. Esomeprazole-Induced Recurrent Anaphylactic Shock with Positive Skin Prick Tests
N. Fathallah,1 A. Alaoua,2 R. Slim,1 F. Bahri,2 K. Bouraoui 1 and C. Ben Salem 1
1 Department of Clinical Pharmacology and Research Unit 99/UR/08-64, Faculty of Medicine Sousse, Tunisia; 2 Department of Internal Medicine, Farhat Hached Hospital, Sousse, Tunisia
Introduction: Esomeprazole is a proton pump inhibitor prescribed as gastric antisecretory agent. Few anaphylactic reactions induced by proton pump inhibitors have been reported. We report a case of recurrent anaphylactic shock induced by esomeprazole.
Case report: A 65-year-old woman with a 10-year history of hypertension treated by candesartan (16mg daily) was hospitalised for rhizomelic pseudopolyarthritis treated by corticosteroids. She was complaining about epigastralgia treated by intravenous injection of esomeprazole (40 mg). Within minutes after drug’s intake, the patient developed malaise, generalized pruritus and low systolic blood pressure at 80mmHg. The patient rapidly recovered after supportive care. No other drugs had been administered during the previous 24 hours. In the next day, she was rechallenged accidentally by esomeprazole. She witnessed a similar episode of hypotension, syncope and tachycardia. Laboratory tests were within normal ranges despite for hypereosinophilia. Skin prick tests were performed and were positive to esomeprazole.
Discussion: Adverse events to esomeprazole are uncommon. Immediatetype hypersensitivity reactions such as urticaria, angioedema, and hypotension induced by esomeprazole and other proton pump inhibitors are rare.[1] In our patient, because of the positive reintroduction test and positive skin tests, the reaction is classified as anaphylactic shock to esomeprazole. In the literature, there are few case reports on anaphylaxis to proton pump inhibitors. The Uppsala Monitoring center has reported 42 cases of anaphylactic reactions or anaphylactic shock in association with proton pump inhibitors.[2] Skin prick tests proved to be an effective tool for the identification of the offending agent in almost all cases of anaphylaxis induced by pump proton inhibitors and are also quite helpful with the problems of cross-reactivity among these agents.
Conclusion: Proton pump inhibitors are a rare cause of anaphylactic reactions such as shock. Clinicians need to be aware of this possibility when prescribing these agents.
PP093. A Study on Assessment, Monitoring and Reporting of Adverse Drug Reactions in an Indian Hospital
S. Palanisamy, K.S. Arul Kumaran and A. Rajasekaran
Department of Pharmacy Practice, KMCH College of Pharmacy, Tamilnadu, India
Objectives: The main aims of the study was to assess the incidence and pattern of ADRs, identifying co-morbidities, past and present illness, assess causality, and the offending drugs, monitoring and documenting suspected adverse drug reaction(s) and to estimate the cost involved.
Methods: A prospective, spontaneous, reporting study was conducted over a period of 6 months by clinical pharmacists. The WHO definition of an ADR was adopted. Each reported ADR was assessed for its causality by using various scales, namely the WHO probability scale, Naranjo’s scale. The severity of each reported ADR was assessed using the criterion developed by modified Hartwig et al., and Siegel scale. The management of reported ADRs and the outcome of the management of ADRs were determined.
Results: A total of 60 ADRs were identified out of which 34 (56.67%) were male and 26 (43.33%) were female patients. Out of 60 suspected ADRs, 58 (96.67%) ADRs were reported from in-patient departments and 2 (3.33%) ADRs were reported from out-patient departments. The assessment by Naranjo’s scale showed that out of 60 ADR’s 44 (73.33%) ADR’s were possible, 16 (26.67%) were classified as probable and 0 (0.0%) were definitely related to the drug. WHO probability assessment scale revealed that out of 60 ADR’s 43 (71.67%) ADR’s were possibly drug-related, 16 (26.67%) ADR’s were probably drug-related and 1 (1.66%) ADR were identified as certain. Preventability assessment showed that 54 (90.0%) ADR were probably preventable and 06 (10.0%) were non-preventable. Severity Assessment by Modified Hartwig and Siegel Scale showed that 35 (58.33%) ADRs were moderate, 21 (35%) ADRs were mild and 4 (6.66%) ADRs were severe. No lethal effects were observed or produced.
Conclusions: Adverse drug reactions (ADRs) related hospital admissions are a significant problem in the health care system. Since the majority of these adverse reactions are predictable and often preventable, there is a need for a greater awareness among the healthcare professionals, regarding not only the potential for adverse drug reactions resulting in hospital admissions, but also in the prevention (or) minimization of the occurrence of ADRs and the minimization of treatment costs.
PP094. Does the Logistic Method Perform Better than the Naranjo Algorithm for Causality Assessment of Adverse Drug Reactions?
H. Théophile,1 M. André,1 Y. Arimone,4 F. Haramburu,3 G. Miremont Salamé 3 and B. Bégaud 2
1 Univ. de Bordeaux, Bordeaux, France; 2 INSERM U657, Bordeaux, France; 3 CHU, Centre Régional de Pharmacovigilance, Département de Pharmacologie, Bordeaux, France; 4 Arme-P, Bordeaux, France
Objectives: An updated version of a logistic causality assessment method assigning a probability of drug causation has recently been proposed. To evaluate its performance, this updated version (LM) and the Naranjo’s algorithm (NA) were compared to a consensual experts’ judgement (CEJ), taken as a reference.
Methods: A sample of 51 drug-event pairs randomly sampled from spontaneous reports to the French pharmacovigilance system was assessed both by an experts’ judgement until reaching consensus and by a pharmacovigilance team using first the logistic method and, one month later, the Naranjo’s algorithm.
Results: The median of probability for drug causation given by the CEJ was 0.75 (inter-quartile 0.56–0.86) versus 0.75 (inter-quartile 0.54–0.94) for the LM. For the NA, possible causality score was predominant (63%), followed by probable (33%) and doubtful, almost certain scores (2% each). For the LM, sensitivity, specificity, positive and negative predictive values were respectively 0.95, 0.57, 0.93 and 0.67. For the NA, when possible score was considered in favour of drug causation sensitivity was 1, specificity 0.14, positive predictive value 0.88 and negative predictive value 1. Nevertheless, when possible score was considered in disfavour of drug causation sensitivity was 0.41, specificity 1, positive predictive value 1 and negative predictive value 0.21.
Conclusions: The LM by providing results expressed as probabilities overcomes the problem of a wide variety of cases under the same category. This method, which is straightforward to use and provides satisfactory sensitivity and specificity results, seems worthy to use for a reliable assessment of adverse drug reactions in routine practice.
PP095. Montelukast and Suicide: Causality Assessment Using Spontaneous Reports and Bradford Hill Guidelines
N. Iessa,1 K. Star,2 L .Wilton,1 S. Curran,3 I.R. Edwards,2 J.K. Aronson,4 M. Murray,1 F.M. Besag 5 and I.C. Wong 6
1 Centre for Paediatric Pharmacy Research, The School of Pharmacy, University of London, UK; 2 Uppsala Monitoring Centre; WHO Collaborating Centre for International Drug Monitoring, Uppsala, Sweden; Department of Public Health and Caring Sciences, Uppsala University, Uppsala, Sweden; 3 Institute of Child Health, University College London, London, UK; Institute of Psychiatry, London, UK; 4 Department of Primary Health Care, University of Oxford, UK; 5 Children’s Learning Disability Team, South Essex Partnership NHS Trust, Twinwoods Health Resource Centre, UK; 6 Centre for Paediatric Pharmacy Research, The School of Pharmacy, University of London, UK; Institute of Child Health, University College London, London, UK; Institute of Psychiatry, London, UK; Department of Pharmacology and Pharmacy, Li Ka Shing Faculty of Medicine, The University of Hong Kong, Hong Kong
Background: The association of suicide related adverse events (SRAEs) with medications is of major concern. In March 2008 the suicide of a 15 year old boy captured media attention. It was suggested that the suicide might be linked to exposure to montelukast, and the FDA requested further investigation of this signal.[1]
Objectives: To examine available evidence of an association between montelukast SRAEs in children aged 2–17 years, by reviewing the literature and Individual Case Safety Reports (ICSRs).
Methods: ICSRs related to montelukast and SRAEs in children aged 2–17 years (January 1986 — March 2010) were extracted from a worldwide database of spontaneous adverse drug reaction reports, VigiBase, maintained by the Uppsala Monitoring Centre. Reporting patterns of SRAEs were investigated.
ICSRS with death and hospitalisation as an outcome were selected and their original reports for were obtained from regulators. An expert panel assessed causality through a Delphi approach using WHO definitions. Begaud’s probabilistic method of causality was used to provide a quasi-quantitative measure. Evidence from published reviews of clinical trials, case studies and ICSRs were used to perform an overall causality assessment using a modified version of the Bradford Hill guidelines.[2]
Results: We identified 321 ICSRs, 96% originating from USA. The number of reported ICSRs increased (9 to 263 in mid 2008). There were disproportionately more ICSRs following the media reports and the FDA’s call for further investigations. Causality assessment of 47 original cases showed 21% possible (n = 10), 32% unlikely (n= 15). 47% of ICSRs (n = 22) were judged unassessable owing to limited detailed information on SRAEs. Probabilities of causality using Begaud’s method ranged between 3 and 90%. There are no published clinical trials designed to study SRAEs and ICSRs provide insufficient evidence to meet all seven modified Bradford Hill guidelines.
Conclusions: Both causality assessments of selected ICSRs and overall Bradford Hill guidelines could not show a conclusive causal relationship between montelukast and SRAEs. The data suggest that the FDA call and media attention created the signal after the coverage received in March 2008. We recommend that a follow up questionnaire be designed for SRAEs, to be issued by regulators to notifiers, to obtain more informative reports.
PP096. Causality Assessment of Adverse Drug Reaction: Comparison between Pharmaceutical Industry and Pharmacovigilance Centre Using the Updated French Causality Assessment Method
M.B. Valnet Rabier,1 Y .Arimone,1 I. Bidault,1 J.P. Dutertre,1 M. Gérardin,1 C. Guy,1 F .Haramburu,1 D. Hillaire Buys, C. Meglio,1 C. Penfornis 1 and H. Théophile 2
1 CRI (Cercle de Réflexion sur l’lmputabilité, Pharmacovigilance Working Group with Regional Centres, Pharmaceutical Industry and French Medicine Agency Representatives), France; 2 Arme-Pharmacovigilance, Bordeaux, France
Objectives: Recently, an updated version of the French causality assessment method has been developed aiming at improving the discrimination and the reproducibility of the current method, mandatory in France. Changes related to chronology, semiology, notoriety and intrinsic causality criteria have been tested by experts from pharmaceutical industry and pharmacovigilance centre. To compare causality assessments from pharmaceutical industry and pharmacovigilance centre assessors.
Methods: A random sample of 30 pairs of drug-adverse reaction from the French pharmacovigilance database was evaluated consensually by two pharmacovigilance teams, one from a regional pharmacovigilance centre and one from a pharmaceutical industry department. Another group constituted of two senior and two junior assessors, each of one from a pharmacovigilance centre and from industry, assessed individually the pairs by using the updated method twice with a time interval of one month. A weighted Kappa coefficient was used to measure the concordance between assessors. Kappa value is always less than or equal to 1, a Kappa of 1 indicating a perfect agreement.
Results: The agreement between consensual assessments from pharmacovigilance and industrial teams was poor (Kappa: 0.40).The detailed analysis of different criteria showed that the agreement for chronology and notoriety was moderate (Kappa: 0.52 and 0.57, respectively) while the agreement for semiology was poor (0.39). The agreement between individual assessments of seniors from pharmacovigilance centre and industrial department was poor for semiology criteria (Kappa: 0.29 for the first evaluation and 0.30 for the second evaluation) and moderate for chronology and notoriety criteria. The agreement between individual assessments of juniors from pharmacovigilance centre and industrial department was overall moderate for chronology, semiology and notoriety (Kappa: between 0.44 and 0.62). The agreement between senior and junior of the pharmacovigilance centre was overall moderate for the three causality criteria (Kappa: between 0.47 and 0.67) while the agreement between senior and junior of the industrial department was very poor for semiology (Kappa: 0.081 and 0.30 for the first and second evaluation, respectively) and high (0.89 and 0.74 for the first and second evaluation, respectively) for chronology criteria
Conclusions: There was a consensus for the assessment of chronology and bibliography, whatever the origin and the experience of the expert. On the other hand, the semiological assessment of the senior in industrial department appears to be different. This could be explained by the fact that industry department and pharmacovigilance centre did not have the same GOAL: one is trained to monitor drug safety, the other to detect signals.
PP097. Role of Drugs in Acute Liver Failure Leading to Transplantation: Results from the 7- Country Study of Acute Liver Transplant (SALT)
E. Gulmez,1 S. Lignot,1 D. Larrey,2 G. Pageaux,2 Y Horsmans,3 B. Stricker,4 J. Bernuau,5 F. Bissoli,6 D. Thorburn,7 J. Montastruc, F .Hamoud,1 S. Micon,1 P. Blin 1 and N. Moore 1
1 Pharmacology, Université Bordeaux Segalen, INSERM U657, Bordeaux, France; 2 Hepatogastroenterology, CHU Hôpital Saint-Eloi, Montpellier, France; 3 Gastroenterology, Louvain Catholic University, Louvain, Belgium; 4 Epidemiology, Erasmus University MC, Rotterdam, Netherlands; 5 Liver Unit, Beaujon Hospital, Clichy, France; 6 Internal Medicine and Cardiology, Clinica San Gaudenzio, Novara, Italy;
7 Liver Unit, Royal Free NHS Trust, London, UK;
8 Pharmacologie Clinique, CHU de Toulouse, INSERM U 1027, Toulouse, France
Objectives: Causes of acute liver failure (ALF) leading to transplantation vary according to viral epidemiology or drug use. These are poorly understood in general.
Methods: Multicentre, retrospective, case-population study in France, Greece, Ireland, Italy, the Netherlands, Portugal, and the UK over 3 years (2005–2007) in NSAID-exposed adult patients of ALF leading to registration for liver transplantation (LT). Data of ALF cases were sought through liver transplant registries and hospital records. Demographic and clinical data were collected for all ALF cases. Drug utilisation data within the 30 days prior to index date (ID, initial symptoms of liver disease) were collected for all cases of ALF. Drug-exposed cases of ALF were assessed individually for causality by four experts using WHO causality scale. In case of divergence, four additional experts evaluated individually to reach a consensus on causality of each drug.
Results: 50 LT centres contributed data in 7 participating countries. Among the 8824 patients identified from LT lists for the period 2005–2007, 500 (5.7%) were ALF. Cases of ALF were then classified “with identified clinical cause” (n = 197, 39.4%), “not drug-exposed and no identified clinical cause” (n=47,9.7%), and “drug-exposed and no identified clinical cause” (n = 241, 49.7%), There were 15 (3.0%) cases with unavailable medical files. Among the “drug-exposed without identified clinical cause”, 84 (17.3%) cases were “acute drug intoxication”, which were mainly with paracetamol (n = 83, 98.8%). There were 34 (7.0%) cases of ALF exposed to 37 different NSAIDs. 26 (70.3%) of those NSAIDs had the causality score of only possible, while none had probable or highly probable. Among the 157 non-intoxication-drug-exposed cases, 46 (29.3%) had the causality score possible, probable or highly probable concluded by the CAC. Among the 106 non-intoxication drug-related ALF cases with causality score possible, probable or highly probable, 46 (43.4%) were non-intoxication paracetamol-associated. 83 of the 84 cases of “acute drug intoxication” (98.8%) had causality score possible, probable or highly probable.
Conclusions: These results show that ALF leading to registration for liver transplantation represents 5.7% of registrations for LT in 7 participating countries. Non-intoxication paracetamol-associated ALF cases represented 43.4% of non-intoxication drug-associated cases of ALF.
PP098. Alendronate Tolerability before and after Market Introduction of Generics
J. Petersen, T. Jan, K. Donegan and S. Seabroke
Pharmacoepidemiology Unit, Vigilance & Risk Management of Medicines, MHRA, UK
Background: Generic weekly alendronate products have been suspected as not being tolerated as well as the innovator, Fosamax, due to the composition of excipients or other drug quality aspects; particularly with regards to upper gastrointestinal (GI) events.[1,2] Additionally laboratory studies have showed that generic formulations of alendronate had a poorer in vitro dissolution profile and a greater bioadhesiveness than the innovator, Fosamax potentially increasing the risk of tablet-induced oesophagitis, i.e. cases caused where patients have taken the tablet with too little liquid or have reclined shortly after taking the tablet.[3,4]
Objectives: The purpose of this study was to investigate the short-term tolerance/safety with weekly Fosamax versus weekly generic alendronate comparing the period four years before and after the introduction of generic weekly alendronate in 2005.
Methods: Data on drug exposure and upper GI outcomes were extracted from the General Practice Research Database (GPRD). A multivariate logistic regression model was used to study whether upper GI event rates in patients with weekly alendronate as first ever bisphosphonate were different before and after market introduction of generics. The odds ratios were adjusted for age, sex, smoking, alcohol intake, fracture history and potentially confounding drug use. Both first-ever and recurrent events were studied. Additionally trends in reporting of spontaneous reports of upper GI reactions over time were also analysed using the UK Yellow Card database.
Results: Data from 54 387 eligible patients were extracted from GPRD. The tolerability of weekly alendronate was not significantly different before and after the introduction of generics; neither for first events (aOR 1.00, 95% CI 0.87, 1.16) nor when including recurrent events (aOR 0.93, 95% CI 0.84, 1.04). The analysis of spontaneous reports also did not highlight any new signals with upper GI events as a result of the introduction of generics.
Conclusions: This study showed that upper GI event tolerability was similar overall in the periods four years before and after the introduction of generics in 2005. Tolerability issues may however have been masked by unmeasured factors that had changed over the same time period, e.g. if high risk patients were channelled towards upper GI-safe treatments (e.g. injectable bisphosphonates or strontium ranelate), if more patients were treated with gastric protectants or simply received better preventive advice. These alternative hypotheses will be studied further using ecological data.
ADRs in Clinical Trials
PP099. Investigation of Second Primary Malignancies (SPM) in Multiple Myeloma (MM) Patients Treated with Lenalidomide
N. Minton, C. Castaneda, L Weiss, N. Brandenburg, D. Gary, J. Freeman, R. Delap, R. Knight, A. Glasmacher, K. Rupalla, J.Zhang and Z. Yu
Celgene Corporation, Summit, NJ, USA
Background: MM is an incurable disease with high rates of relapse. Novel agents have improved survival, however, with longer survival SPM incidence may be higher due to immune deficiency and underlying genetic predisposition. Melphalan and stem cell transplant (SCT) are associated with SPM. Numerical imbalances of SPM in clinical trials of lenalidomide in newly diagnosed MM (NDMM) patients, prompted detailed analyses including SPM incidence rates (IR) and impact of SPM on event-free survival (EFS).
Methods: Potential SPMs were identified and incidence rates (IR) calculated/100 patient-years (py) for two pivotal lenalidomide (LEN) studies in relapsed/refractory MM (RRMM), and for 3 trials in NDMM. SPM rate from post-marketing data was also estimated.
Results: RRMM: IR for SPMs was higher for LEN/dexamethasone (DEX) compared with DEX control (3.98 v 1.38/100py). Most SPMs were non-melanoma skin cancers (2.40 v 0.91/100py). IRs for varied solid tumors were similar (1.28 v 0.91/100py), and for all invasive SPMs (1.71 v 0.91/100py; p = 0.46). Sensitivity analysis of time to progression (TTP) (HR 0.350, p< 0.001) counting invasive SPM as events — EFS: (HR 0.355, p< 0.001) was similar. There was a 39% reduced risk of death in favour of LEN/DEX prior to unblinding (HR 0.607, 95% CI 0.459, 0.803, p< 0.001); median overall survival (OS) advantage after extended follow-up and crossover was 38.0 v 31.6 months (HR 0.822, 95% CI 0.678, 0.996, p = 0.045).
NDMM: IR for SPM was 4.55 v 1.98/100py for LEN v control. AML (1.8%), MDS (0.8%) and solid tumours (2.8%) occurred on LEN in all 3 studies, with Hodgkin’s disease (0.6%) and B-acute lymphocytic leukaemia (B-ALL) (0.4%) in post-transplant studies only. EFS analyses had minimal impact on progression-free survival (PFS). Pooled analyses, accounting for death as a competing risk, showed increased risk (p< 0.0001) of invasive SPM, driven by hematological SPM.
Post-marketing: Reporting rate of SPM in MM was low (0.2%).
Conclusions: In RRMM studies of LEN/DEX, few SPM were observed, predominantly non-melanoma skin cancers of limited significance, in the presence of an OS benefit. In NDMM, SPM, mainly AML and MDS were observed on LEN with melphalan or following high dose melphalan and SCT. Hodgkin’s disease and B-ALL were also observed with LEN after SCT. OS data in NDMM studies is not yet mature but no adverse trends have been observed. Risk factors for SPM continue to be evaluated. Regulators should consider reinstating the inclusion of emergence of new cancers as part of a serious adverse event definition.
PP100. Completeness of Initial Serious Adverse Event Forms from Clinical Trial Safety Reporting: A Prospective Chart Survey
P. Ghadge,1 S. Valsan 1 and P. Watson 2
1 Tata Consultancy Services, Vikhroli, Mumbai, Maharashtra, India; 2 Roche Products Ltd, Falcon Way, Welwyn Garden City, UK
Objectives: The completeness of clinical information received during the reporting and review of safety information in clinical trials is of central importance in pharmacovigilance processes, including signal detection.[1] There has been limited recognition of problems relating to the degree of completeness of safety information in clinical trial serious adverse event (SAE) reporting. The objective of this study was to evaluate the degree of completeness of SAE forms from clinical trials.
Methods: Initial SAE forms reported from clinical trials sponsored by a multinational pharmaceutical company were assessed over a month. Each form was assessed in terms of the completeness of reporting of required fields and categorised as complete (no fields missing) or incomplete (at least one required fields missing). The data were analysed using descriptive methods.
Results: A total of 496 forms satisfying predefined criteria were included in this study. The results revealed that 180 (36%) were complete and 316 (64%), incomplete. Of 316 incomplete forms, there were 906 missing fields. The forms were further assessed according to importance of missing information; critical fields were considered to be those which negatively impacted the medical review or regulatory submission process (e.g. expedited reporting). Other fields on the SAE form were considered non-critical in this study. Analysis of the incomplete forms with respect to critical versus non critical fields, revealed that 86.6% of missing fields related to critical field information as compared to 13.4% for non critical fields. Further analysis of forms with missing critical fields revealed that 119 (38.8%) forms had one critical field missing, 72 (23.5%) were reported with two critical fields missing and 116 (37.39%) with 3 or more critical fields missing. The range of incomplete or missing fields include administrative data, causality assessment, medical history and concomitant medication, seriousness criteria, posology of administered medicine as well as the clinical case description.
Conclusions: This study suggests that a substantial proportion of initial SAE forms are reported from global clinical trials with incomplete with missing safety information. This problem may relate to the lack of awareness at investigational sites regarding the critical nature and importance of SAE information in clinical trials, as well as understanding of general principles of pharmacovigilance. Training and education for all study personnel with respect to safety reporting procedures needs to be sufficient to meet the safety reporting requirements in clinical studies. A collaborative approach between pharmaceutical sponsors and study investigator sites to improve the completeness of safety reporting is suggested.
PP101. Reasons for the Discontinuation of Treatment with Infliximab at Angers University Hospital: A Follow-Up of 5 Years
H. Martin Huyghe,1 D. Bourneau Martin,1 A. Marie,1 B. Bouvard,2 E. Metivier,3 F. Moal,4 Y. Le Corre,5 A. Jamet,1 L. Lagarce 1 and P. Lainé Cessac 1
1 Department of Pharmacovigilance, CHU Angers, Angers, France;
2 Department of Rheumatology, CHU Angers, Angers, France;
3 Department of Hepatology and Gastroenterology, CHU Angers, Angers, France;
4 Department of Pharmacy, CHU Angers, Angers, France;
5 Department of Dermatology, CHU Angers, Angers, France
Introduction: Infliximab (Remicade®) is a chimeric monoclonal antibody combining 75% human sequences and 25% mouse sequences which inhibits TNF-α. The aim of our retrospective study was to assess the incidence of and reasons for discontinuations of infliximab at Angers University Hospital.
Methods: Under the contract concerning correct use, infliximab is only available with a nominative prescription. Based on this, the prescriptions of patients who received at least one infusion of infliximab between January 2006 andDecember 2010 at Angers University Hospital were recorded. Each case involving a definitive or temporary discontinuation of treatment (more than 3 months) was analysed by consulting the computerised and paper records on patients.
Results: Our study concerned 185 patients (89 women and 96 men) with a mean age of 42 years (11-86 years). Most patients were being treated for either a digestive disease (82 patients with Crohn’s disease, ulcerative colitis) or a rheumatological disorder (81 patients with rheumatoid arthritis, ankylosing spondylitis, Still’s disease or psoriasic rheumatism). Among the main reasons for the 109 discontinuations (59%), 28 records mentioned therapeutic inefficacy (26%), 31 an adverse event (28%), 12 the onset of a remission (11%) and 10 a decision based on personal convenience (9%). Themost common adverse effects were systemic manifestations occurring within 2 hours of the infusion (14 cases, 45%) such as oedema, facial erythema, rash, hypertension, tachycardia, bronchoconstriction, flushing, malaise and headache. These events occurred between the 1st and 29th infusions, with a median of the 3rd infusion. Other effects, such as the appearance of a tumour, infection, hepatic cytolysis, asthma or eczema, were described in 12 cases. Relative to the 31 adverse events, our Pharmacovigilance Centre received 5 spontaneous notifications.
Conclusion: This study highlights a high rate of discontinuations of infliximab (more than half of patients), including a quarter for adverse events and particularly for infusion reactions. These could be prevented by systematic premedication with antihistamines and corticosteroids, at least from the 3rd infusion. The chimerism of infliximab can explain these reactions. In addition, our study demonstrated a significant rate of underreporting (84%). The organisation of occasional surveys thus enables the Pharmacovigilance Centre to overcome this problem to a certain extent, and to be more exhaustive in its analyses.
Medication Errors and Preventability
PP102. A Recurrent Acute Urinary Retention in a Child Following a Medication Error
D. Soussi Tanani, A. Chebat, R. Benkirane and R. Soulaymani Bencheikh
Moroccan Pharmacovigilance Center, Rabat, Morocco
Background: The problem of medication error (ME) has attracted worldwide interest in recent years since it is causing a significant morbidity and mortality, and therefore generates an additional economic cost for health care systems. In Morocco, a prospective multi-center study conducted in 2007 at Rabat University, found that the frequency of ME was 7.8% in pediatric intensive care and 7.3% in adults intensive care.[2]
Case report: It was 9 years old child with no medical history who has suffered for some years of enuresis. The child received medical treatment prescribed by an urologist based of oxybutynin chloride 5 mg at a rate of half a tablet three times daily for a month. The child has doubled the dose and took one tablet three times daily for 3 consecutive days and developed an acute urinary retention which required a urinary catheter in an emergency. The child after urinary catheter has kept dysuria and fifth days of drug discontinuation, he developed a second acute urinary retention with big urinary bladder distension. The evolution was slowly favorable with persistent episodes of dysuria.
Discussion: Oxybutynin chloride is an anticholinergic antispasmodic drug. It decreases the contractility of the detrusor and so decreases the amplitude and frequency of bladder contractions and the intravesical pressure. The causality assessment of the ADR was plausible with French method, and the side effect was evitable because the error was due to poor observance. The pharmacokinetic properties are useful to know to understand the clinical chronology of the drug. After oral administration, Oxybutynin is rapidly absorbed and has an extensive first pass hepatic metabolism. So the absolute systemic bioavailability is only 6.2%. The major metabolite is pharmacologically active (desethyloxybutynin). Oxybutynin is biexponential eliminated and less than 0.02% of the administered dose is excreted in the urine. Excretion is mainly hepatobiliary and half-life is only 2 hours. The persistence of the ADR could be due partly to the low hepatobiliary clearance although the drug has a short half-life, and secondly because the main metabolite is active with large interindividual variations.
Conclusion: The medication errors in children can be harmful and involve life-threatening. The pharmacokinetic profile of some drugs complicate sometimes the clinical situation.
PP103. Therapeutic Errors in Older Adults
H. Filali, I. Rahmoun, H. Elkaromi, D. M’zah, A. Miftah and F. Hakkou
Departement of Pharmacology, University Hospital Ibn Rochd Casablanca, Morocco
Objectives: To evaluate the reasons for unintentional therapeutic errors in older adults, the types of medications most frequently involved, and the medical outcomes related to these adverse drug events.
Design: Retrospective analysis of department of Pharmacology, university hospital Ibn Rochd of Casablanca.
Setting: Collects data from January to December 2010 were examined collected from different departments of medicine and surgery.
Participants: Cases involving adults aged 65 and older with a potentially toxic exposure due to unintentional therapeutic errors.
Measurements: Hazard factor analysis was conducted to identify medications that pose risk in this population.
Results: There were 98 for 302 older adults with reported therapeutic errors, of which 72 cases were followed to a known medical outcome. A major effect or death occurred in 46 cases. The most common reasons for therapeutic errors were inadvertently took or given medication twice, wrong medication taken or given, and other incorrect dose. The reasons associated with the highest rate of major effect or death were drug interaction, health professional or iatrogenic error, and more than one product containing same ingredient. Certain medication classes such as antipsychotics, analgesics, anticoagulants, antidiabetics and some cardiovascular agents were associated with high hazard factors.
Conclusion: Evaluate therapeutic errors in older adults was very interesting to identify reasons associated with frequently reported errors, as well as reasons and medications involved with errors that result in serious outcomes. Knowing the reasons why they occur can aid in developing strategies for decreasing unintentional errors in older adults.
PP104. A Pilot Prospective Observational Hospital Study on Adverse Drug Reactions due to Medication Errors
R. Leone,1 L .Magro,1 P. D’incau,1 P. Minuz,2 F. Paluani,2 R. Nuvolari,2 S. Bonafini 2 and G.P. Velo 1
1 Pharmacology Unit and Pharmacovigilance Centre of Veneto Region, University Hospital of Verona, Verona, Italy;
2 Department of Medicine, Division of Internal Medicine C, University Hospital of Verona, Verona, Italy
Background: A medication error is a failure in the treatment process that leads to, or has the potential to lead to, harm to the patient.[1] It has been estimated that 1–2% of patients admitted to US hospitals are harmed as a result of medication errors.[2] Prescribing faults and prescription errors are the major problem among medication errors. In fact, prescription errors account for 70% of medication errors that could result in adverse drug reactions (ADRs).[3]
Objective: We performed a pilot prospective observational study on adverse drug reactions due to medication errors occurred in patient aged >18 years hospitalized in an Internal Medicine Unit of Verona University Hospital from April 2010 to June 2010.
Methods: The project was of three phases. In the first one three physicians of involved unit reviewed all patient charts and registered all ADRs. A panel of experts evaluated if the ADRs were due to medication errors or not, and in the case of error they identified the cause. In the second phase educational audits directed to health professionals have been organized and tools (e.g. check-list) to reduce the medication errors have been proposed. The third phase, that is similar to the first one and takes account of tools, is in progress.
Results: Preliminary results showed that, from 14 April 2010 to 22 June 2010, 145 patients (median age 73.6, 51% female) have been enrolled. Twenty -six patients (18%) had at least one ADR occurred during the hospitalization. The total number of ADRs occurred during the hospitalization was 32. A panel of experts evaluated that 14 ADRs (44%) were due to medication errors, out of which 50% were serious. The most frequent ADRs caused by a medication error was hypotension and the drugs most involved were: amlodipine, heparin, furosemide, ramipril, morphine and electrolyte solution.
Conclusion: This pilot study confirms the high incidence of medication errors as cause of ADRs.
Therefore the prevention of medication errors is an important task to improve health patient and to reduce the health care costs. Strategies, such as a prescription check list, can be adopted to try to minimize risks.
PP105. Preventability Analysis of Adverse Drug Reactions Detected by Stimulated Spontaneous Reporting in Two Internal Medicine Departments in Romania
A.M. Farcas, C. Bucsa, A. Sinpetrean, C. Mogosan, D. Dumitrascu, A. Achimas and M. Bojita
University of Medicine and Pharmacy ‘Iuliu Hatieganu’, Cluj-Napoca, Romania
Objectives: Serious adverse drug reactions (ADRs) in hospitalized patients are common and often preventable.[1] In a prospective study conducted over a 12-month period in an internal medicine department in Romania, using stimulated spontaneous reporting for identifying ADRs, the overall incidence of serious ADRs in the hospitalized patients was 4.7%. Out of total ADRs 50% were considered preventable.[2] Our objective was to analyse preventability data on previous collected ADRs that are stored in our database in order to identify the most common drugs involved in ADRs and the prescription patterns with the final goal of proposing preventing strategies.
Methods: The first two hundred ADRs detected in the internal medicine departments and stored in our database were characterized by drug, drug class, severity, probability of causality, duration, outcome and preventability. Drug-drug interactions, inappropriate dose, off-label use, contraindications, according to the Summary of the Product Characteristics (SmPC) and Thomson Micromedex were the factors assessed for preventability. Patient-related factors like hepatic or renal dysfunction, allergy history, self-medication, non-adherence were also evaluated.
Results: 43% of the total ADRs were considered preventable. Anticoagulants (16%), followed by NSAIDs (15.5%), antibiotics (11.5%) and diuretics (9.5%) were the drugs most common involved in preventable ADRs. The ADRs that were considered preventable are as follows: gastrointestinal ADRs (20.93%), renal ADRs (13.95%), metabolic ADRs (12.79%), vascular (11.62%) and hepatic (8.13%) ADRs. In 58% of the cases of preventable ADR, they lead to the hospitalization of the patient. Drug-drug interactions (DDIs), inadequate dose, self medication, inadequate drug therapy monitoring and contraindications were the factors leading to preventable ADRs. In 14.5% cases of preventable ADRs there are clear warnings in the SmPC regarding the adverse effects. 87.2% of all preventable ADRs were type A adverse reactions.
Conclusions: Four groups of drugs account for more then half of the preventable ADRs. Moreover the two leading causes of preventable ADRs are DDIs and inadequate dose. Preventing strategies should target drug prescription.
PP106. Omitted Doses in a Paediatric Intensive Care Unit: A Pilot Study
A.R. Cox,1 F. Walele 2 and R. Isaac 3
1 West Midlands Centre for Adverse Drug Reactions, City Hospital, Birmingham, UK; Pharmacy Department, School of Clinical and Experimental Medicine, University of Birmingham, UK;
2 Aston School of Pharmacy, Aston University, Birmingham, UK;
3 Pharmacy Department, Birmingham Children’s Hospital, Birmingham, UK
Objectives: Medication errors are more common in paediatric intensive care units (PICU),[1] and omitted doses are a major concern within the UK.[2,3] The objective was to measure the incidence and nature of omitted doses on a PICU (paediatric intensive care unit) and assess the potential clinical significance of these omissions.
Method: A prospective collection of all drug administrations on the ward during a 14 day study period. Administered doses were compared with prescribed doses. Data was recorded on a standardised data capture form. The frequency of dose omissions was calculated as the sum of omitted doses divided by total prescribed doses. Dose omissions were classified by a panel of specialist paediatricians, using a questionnaire with a 5-point Likert scale. The classification was based on the National Reporting & Learning Services (NRLS) severity rating scale of patient safety incidents.[4] Potential clinical significance levels for each omission were then decided by consensus of the panel.
Results: 1995 doses were prescribed, of which 129 (6.5%) doses were omitted. The most common types of drugs that were omitted were: anti-infectives (20.2%), IV nutrition & IV fluids (15.5%), minerals (15.5%), diuretics (14.7%) and analgesics (9.3%). Less common drugs omitted included: antisecretory drugs (3.88%), laxatives (2.33%), bile acids (1.5%), hypnotics (3.1%), anti-epileptics (1.5%), anti-thyroid drugs (0.8%), corticosteroids (0.8%) and probiotics (1.5%). The dominant reason for dose omissions was intentional omission, with no documented reason (64%). Authorised omissions include: ‘at doctor’s request’ (12.%), intentional omission: ‘awaiting blood levels’ (1.5%), and ‘patient cannot receive’ (fasting/vomiting/no access) (12.%). Cumulatively, authorised omissions made up 26% of omissions. Unauthorised omissions included ‘drug not available’ (3%), intentional omission with no reason given, (64%), ‘patient away from ward’ (3%) and a blank space in chart — no reason given at all (3.88%). Unauthorised omissions accounted for 74% of omissions. 44% of omissions involved low potential harm to patient, potentially resulting in observation, 31 % involved moderate potential harm, which may cause a moderate increase in treatment and 20% of omissions involved severe potential harm, with potential to cause permanent patient harm.
Conclusions: A substantial level of omitted doses exists; a majority of which were not documented correctly. Significant omissions have the potential to cause serious harm. Revision of documenting omissions without reasons is needed and strategies should be put into place to avoid the high number of preventable omitted doses.
PP107. Leg Amputation Following Intramuscular Injection of Iron Dextran in a 32- Year-Old Woman: a Medication Error
G. Shalviri,1 K. Gholami 2 and N. Javidnikou 1
1 Iranian Adverse Drug Reaction Monitoring Center, Ministry of Health, Tehran, Iran;
2 Department of Clinical Pharmacy, College of Pharmacy, Tehran University of Medical Sciences, Tehran, Iran
Background: Hypersensitivity reactions following administration of iron dextran is not uncommon. However, there are limited published data about amputation due to hypersensitivity vasculitis induced by this medicine.
Purpose: To inform healthcare professionals of a rare serious reaction leading to leg amputation following intramuscular injection of iron dextran. To report comments for preventing such reactions.
Method: A case of leg amputation following intramuscular injection of iron dextran reported to Pharmacovigilance Center was reviewed. Patient and reaction data was collected by assessing the reported yellow card, patient chart review and interviewing with patient and physicians. World Health Organization definition for serious reactions was used to determine the seriousness of the reaction. Naranjo algorithm was used to determine probability scale. The preventability of the reaction was determined based on questionnaire of Schumock et al.
Result: The studied case was classified as a rare and serious but preventable reaction induced by intramuscular injection of iron dextran in a 32 years old woman. The probability of the reaction was estimated as “probable” based on Naranjo algorithm. The anemia was not approved at the time of prescription. Incorrect indication and inappropriate use of the medicine was detected, making the reaction a remarkable medication error.
Conclusion: Safety monitoring of medicines is an eternal and unavoidable need in the area of science and activities related to medicinal products. As far as a product is available on the market, its safety profile should be reviewed for newly established signals. Inappropriate use of medicines, as an important type of medication errors, can lead to occurrence of rare serious reactions.
Discussion: Iron dextran could cause serious and life threatening adverse effects. It is necessary for healthcare professionals to be informed of such reactions in order to apply preventive actions. We issued a dear doctor letter to health care professionals emphasizing that there are limited indications for administration of parenteral form of iron preparations. These limited indications include iron-deficiency in which the patient is unable to use oral forms; the oral forms are ineffective e.g. secondary to poor absorption, Gastrointestinal disease or intolerance; the rapid replenishment of iron stores is necessary as in hypochromic anemia of infancy or the last trimester of pregnancy; patients with chronic renal failure receiving epoetin alfa. Also using a test dose prior to the first therapeutic dose and observing for signs or symptoms of anaphylactic-type reactions during administration of iron dextran is recommended.
PP108. Medication Error in the Administration of Caffeine in Newborn: Case Report
R. Sahnoun, E. Gaïes, N. Jebabl S. Trabelsi, I. Salouage, R. Charfi, M. Lakhal and A. Klouz
Service de Pharmacologie Clinique, Centre National de Pharmacovigilance, Tunis, Tunisia
Introduction: Caffeine citrate is commonly used for prophylaxis and treatment of apnea in preterm babies in Tunisia, however, there is no pediatric form of this drug. For this reason, a dilution protocol to administrate caffeine in newborns was needed. Dilution protocol may increase the risk of medication errors and so the risk of toxicity side effects or therapeutic inefficiency.
We report a case of therapeutic inefficiency due to a medication error in caffeine dilution and illustrated by caffeine plasma monitoring.
Case: T. O. a premature baby was born at 25 weeks of gestation. Apgar was 7 in the first, fifth and tenth minute. For apnea and bronchopulmonary dysplasia, he was treated with a caffeine loading dose 20mg/kg/d and orally maintained dose of 10mg/kg/d.[1] He also received domperidone, omeprazole, alginates, valproic acid, vitamin E and ergocalciferol. Three months after the beginning of caffeine, the newborn did not improve and continued having apnea. Thus monitoring of caffeine was been required. Plasma levels measured by High Performance Liquid Chromatography (HPLC) showed a null concentration. After checking the team of neonatology we found an error in the caffeine dilution protocol. In fact, the 2 mL flacon is dosed at 25 mg of caffeine base corresponding to 50 mg of citrate caffeine which must be diluted in 25 mL of saline to have a caffeine base concentration of 1 mg/mL, but the nurse added 50 mL of saline instead of 25 mL. So the newborn received the half dose (2.5 mg/day instead of 5 mg/day he received) during the three months.
Five days after correction of the dilution error, another dosage of plasma caffeine level was done. The concentration increased to 3.35mg/mL.
Conclusion: Medical errors are frequent in pediatric inpatients and many reasons may explain this such as changes in pharmacokinetic parameters or lack of appropriate dosage as the case of caffeine. These errors can be prevented by dose checking software but it is a costly intervention and requires time to be implemented. For that plasma monitoring may represent in some cases a solution to reduce medication errors and to verify adherence to treatment.
PP109. Are Newly-Introduced Drugs Used Appropriately? An Audit of Rivaroxaban
C. Higham 1 and C. Anton 2
1 Sandwell and West Birmingham Hospitals NHS Trust, Birmingham, UK;
2 West Midlands Centre for Adverse Drug Reactions, Birmingham, UK
Introduction: In September 2010 rivaroxaban replaced enoxaparin as thromboprophylaxis agent of choice at our NHS hospital trust. Specific rivaroxaban prescribing requirements are for the first dose to be administered 6–10 hours after surgery and continued for 10–14 days for total knee replacement (TKR) and 30–35 days for total hip replacement (THR) patients.
Objectives: The primary objective was to find out if rivaroxaban was prescribed in accordance with the following above audit standards:
Method: Prior to the start, guidance for prescribing this drug was displayed in the orthopaedic theatres and elective surgery ward. Patients who underwent TKR, THR or were prescribed rivaroxaban for other surgery during September and October 2010 were included in this study. Data was collected as soon as possible after surgery.
Results: Data was gathered for 115 patients. 25 patients did not receive their first dose within the target 6–10 hours (range 2.5–54 hours) after surgery. Five of these were due to nurse error, two due to bleeding and 18 due to the wrong time being prescribed. The percentage of patients who received their first dose within 6–10 hours of surgery improved from 56% in the first quarter to 100% in the third quarter (two proportions comparison p< 0.001). Only 77 (68%) stat doses were prescribed on the front of the drug chart, and this improved from 33% in the first quarter to 94% in the fourth quarter (two proportions comparison p< 0.001). There was no significant difference between the fist and last quarters of patients who received rivaroxaban for an appropriate indication. The correct course length was prescribed for 16 TKR and 7 THR only. Prescribing improved during the audit following emails sent to the surgeons and anaesthetists after 2 and 4 weeks.
Five wound events resulting in withholding or discontinuation of rivaroxaban, three of which occurred in patients who received their first dose less than 6 hours after surgery. There were two major gastrointestinal bleeds; one had their first rivaroxaban dose 2.5 hours after surgery and had taken diclofenac for years. The other was taking aspirin and mirtazapine and was transferred to intensive care for 10 days. Two patients developed pulmonary emboli, one of whom was using HRT, one patient died from an acute myocardial infarct and one patient developed a tachycardia and was transferred to coronary care.
Discussion: New drugs are not always used as the manufacturers’ intended and this can lead to ADRs and patient harm.
PP110. National Observational Study on Rational Drug Prescribing and Dispensing in Pharmacies (Morocco)
A. Khattabi,1 R. Benkirane 1 and R. Soulaymani 2
1 Poison Control and Pharmacovigilance, Rabat, Morocco;
2 University Mohammed V, Faculty of Medicine and Pharmacy, Rabat, Morocco
Objectives: Concept of rational use of drug is new in developing countries like Morocco,[1] though several steps have been taken towards ensuring rational drug use. Analyse of prescriptions and self medication can be a good tool (or first step) to evaluate the rational use of drugs in terms of prescribing and dispensing in Morocco. We conducted a national study on rational drug prescribing and dispensing in Pharmacies with WHO financial support, in order to quantify and describe the demographic, socioeconomic and pharmacological characteristics of prescriptions and to estimate the use of drugs, without medical prescription, in a representative sample of the Moroccan population.
Methods: A national cross-sectional, descriptive study was conducted in pharmacies of Morocco, during the time period from October 27th to November 3rd 2008.
Results: Totally 1786 prescriptions and 3421 cases of self-medication were recorded during the study period, wherein 8758 drugs were dispensed (51.4% only were prescribed). The demographic, socioeconomic and pharmacological characteristics were different between prescriptions and self-medication. The average age of patients was 36-years±21 (vs 24-years+-19 in self medication), the sex ratio was 0.7 (vs 0.87), 27% of patients had medical coverage (vs 7.4%). Only 27.3% of drugs were dispensed by generic name (among them 58% were prescribed and 42% were dispensed by advice of the pharmacist). Non-narcotic analgesic antipyretic products (N02B) were most commonly dispensing both by prescription and self medication, followed in prescription by non-steroidal anti-rheumatic drugs (M01 A) and broad-spectrum penicillin (J01C). Among the drugs dispensed, 75.5% were oral followed by topical (21.0%) and parenteral forms (3.5%). The most majority of prescribing physicians were from private sector (79.5%), they were generalists (45.5%), specialists (49.5%) and dentists (2.5%). In 11% of prescriptions, we have raised errors (bugs and interactions). 90% of prescriptions were non-compliant in the form. Diagnosis was mentioned only in 2.4% (n = 30) of the prescriptions and the average cost per prescription was found to be 156.77 Moroccan dirham (US$ 21).
Conclusions: There is a need for educational intervention for prescribers and both managerial and educational intervention for the pharmacists to improve prescribing and dispensing in Morocco.
PP111. Actions Taken For Laroxyl (Amitriptyline) Intoxication in Children
D. Aydinkarahaliloglu, E. Aykaç, Y. Kasap, G. Sağis, C. Babacanoğlu, H. İlbars, H. Özbek and S. Kerman
General Directorate of Pharmaceuticals and Pharmacy, Ministry of Health, Ankara, Turkey
Background: Laroxyl is a tricyclic antidepressant containing amitripty-line as drug substance. Pediatricians report frequent Laroxyl intoxications in children, which leads to receiving intensive care treatment in many cases. Additionally, Psychiatric Association of Turkey defines an important risk regarding this drug due the lid of inner packaging which can easily be opened by children.
Objective/aim: The drug can be easily provided by families hence it’s cheap and has been excluded from the scope of green prescription. Because the cap of its inner packaging can easily be opened by children leading to intoxication, switching to child resistant closure is on the agenda.
Method: The correspondences and complaints regarding the issue were assessed. In the correspondence letter submitted to our Ministry by Dortcelik Children’s Hospital in the city of Bursa, it was reported that too many Laroxyl intoxication cases were observed and only during the 20 day long period between July 23rd, 2007 and August 12th, 2007 four children who were diagnosed with Laroxyl intoxication were treated in Intensive Care Unit. Furthermore, a report was submitted to TUFAM regarding a 4 year old girl with intoxication. Details of the case which resulted in death will be provided.
Results: There are two drug products in Turkey containing amitriptyline as drug substance. The commercial name of one of these is Laroxyl Sugarcoated pill and the other is Triptyline film coated tablet. Laroxyl is available in doses of 10 mg and 25 mg. Triptylin 10 mg Film coated tablet and Triptylin 25 mg Film coated tablet are no longer available starting since June 30th, 2003 and June 27th, 2006, respectively. Marketing Authorization holders were warned regarding the application according to variation guidelines for the necessary packaging change. Switch to “HDPE bottlepolypropylene cap” as primary packaging material for Laroxyl 25 mg 40 sugar-coated pills was approved on November 13th, 2009, and on February 1st, 2010 for Laroxyl 10 mg sugar-coated pills. The authorization holder of Triptylin 10 mg Film Coated Tablets and Triptylin 25 mg. Film Coated Tablets has committed to implement the requirements in case of recommencement of manufacturing.
Conclusion: Primary packaging material was changed as “HDPE bottlepolypropylene cap” Laroxyl 10 mg 30 sugar-coated pills and Laroxyl 25 mg 40 sugar-coated pills.
Discussion: The necessary actions have been taken for such an important public health issue.
PP112. Medication Error with High-Dose MTX Treatment
I. Salouage, E. Gaies, S. Trabelsi, R. Charfi, N. Jebabli, M. Lakhal and A. Klouz
Centre National de Pharmacovigilance, Tunis, Tunisia
Introduction: Methotrexate (MTX) is a folic acid antagonist used in the treatment of a variety of solid tumors and haematological malignancies. To prevent potentially toxicity, essentially renal, high-dose MTX is usually administered following preventive measures, using vigorous hydration and urine alkalinisation. We report a case of medication error with high-dose MTX treatment.
Case: We report a case of a 53-year-old woman with lymphoblastic B acute leukemia treated with 5 g of MTX that should be passed on 24 hours. but the drug was passed on less than 2 hours. Few hours after, the patient presented digestive disorders (vomits and diarrhea) without fever. At 48 hours after treatment beginning (H48), MTX plasmatic level was 99 mmol/L. this high plasmatic level of MTX was associated to an acute renal failure (398mmol/L), a hepatotoxicity (transaminase levels were 5 normal times) and a pancytopenia (thrombopenia at 42.103/mL, 7.3g/dL of hemoglobin and 800/mL of leukocyte). The management of this MTX intoxication was performed by the administration folinic acid (200mg/6 hours), hyper-hydration (2 L/day) and urine alkalinisation (200 mL/day of bicarbonate 4.2%). Thirteen days later, the MTX plasmatic level was 1 mmol/l with a favourable course of hepatic injury and the renal failure.
Discussion: A medication error concern the way of the administration of a toxic drug. This error was responsible of serious consequences and could be life threatening.
In the literature, management MTX intoxication can include the hemodialyses and the administration of the carboxypeptidase in addition to the rescue treatment. Our case was treated using simple means (hydration, folinic acid and urine alkalinisation).
PP113. Preventability of Adverse Drug Reactions (ADRs) Leading to Hospital Admissions
L .Alesso,1 R. Herrera Comoglio 1 and C. Nota 2
1 Pharmacovigilance Service, Hospital Nacional de Clínicas, Córdoba National University, Córdoba, Argentina;
2 Clinical Medicine Unit, Hospital Nacional de Clínicas, Córdoba National University, Córdoba, Argentina
Background: Adverse drug reactions defined as “noxious and unintended response to a medicinal product “1 are a significant cause of hospital admissions. Preventable ADRs, such as overdoses derived from known changes in patient’s conditions (inadequate monitoring of therapy) as well as interactions might be considered as a form of medication errors. Preventable ADRs can also lead to significant morbidity and mortality and financial costs.
Aim: To assess the potential preventability of ADRs reports related to hospital admissions received in a University Hospital Pharmacovigilance Unit.
Methods: A retrospective review of ADRs reports leading to hospital admissions was conducted for a 30-month period (January 2009 to June 2011). ADRs were classified as type A or B. Interactions were identified according summary of product characteristics and/or relevant literature. Causality was assessed according the WHO-UMC system. When possible, clinical charts were reviewed in order to assess causality. ADRs’ avoidability was assessed using Hallas2 definitions: Definitely avoidable, Possible avoidable and Unavoidable.
Results: There were 176 ADRs reports, in 81 reports, at least one ADR was considered to be directly related with hospital admissions. There were 2 prescription errors and 2 administration errors. In the 77 remaining reports, the relationship of admissions to drug exposure was determined to be probable in 60 cases (73%) and definite in 2 cases (2.6%). From this group, 52 (83.9%) of these events were considered definitely avoidable. Most of theses 52 both probable and avoidable ADRs were Type A (48) (92.3%). Out of type B ADRs, 2 cases reported previously documented allergy (3.84%).
Main drug classes related were: non-steroidal anti-inflammatory drugs (NSAIDs) (21.15%) oral hypoglycemic agents and insulin (17.3%), diuretics (15.38%), antipsychotic agents (15.38%), antidepressants (15.38%), immunosuppressant (methotrexate) (9.62%) antibiotics (7.7%) and oral anticoagulants (5.77%).
Discussion: Voluntary reporting can be biased by many factors. ADRs number and characteristics (drug, reaction) varied according to the reporter clinical activity (allergy, clinical medicine, and rheumatology) and to a reporting proactive approach since July 2010. Health system characteristics often didn’t allow finding confirmatory data, because of diagnostic tests’ availability and cost.
Conclusions: ADRs leading to hospital admissions are often preventable. In this sample, few drug groups of commonly prescribed drugs in elderly have been found to be related to more than 80% of ADRs leading to hospital admissions. An educational and proactive approach among healthcare professionals, patients and caregivers focusing on rational prescription and closer monitoring should be targeted.
Epidemiology
PP114. Effectiveness of Proactive-Approach in a Pharmacovigilance Unit: Review and Analysis of 3003 Notifications Received
G.A. Keller,1 M.L. Ponte,2 P.A. Alvarez,3 A. Campos 4 and G. Di Girolamo 4
1 Pharmacovigilance Unit, Second Chair of Pharmacovigilance, School of Medicine, Universidad de Buenos Aires, Ciudad Autónoma de Buenos Aires, República Argentina; Emergency Department, Hospital General de Agudos Donación Francisco J Santojanni, Ciudad Autónoma de Buenos Aires, República Argentina;
2 Pharmacovigilance Unit, Second Chair of Pharmacovigilance, School of Medicine, Universidad de Buenos Aires, Ciudad Autónoma de Buenos Aires, República Argentina; Internal Medicine Department, Hospital General de Agudos Dr Cosme Argerich, Ciudad Autónoma de Buenos Aires, República Argentina
3 Pharmacovigilance Unit, Second Chair of Pharmacovigilance, School of Medicine, Universidad de Buenos Aires, Ciudad Autónoma de Buenos Aires, República Argentina; Cardiology Division, Hospital de Clínicas José de San Martín, Ciudad Autónoma de Buenos Aires, República Argentina;
4 Pharmacovigilance Unit, Second Chair of Pharmacovigilance, School of Medicine, Universidad de Buenos Aires, Ciudad Autónoma de Buenos Aires, República Argentina
Objectives: In Argentina, Pharmacovigilance program was created in 1993 centered in the national regulatory agency with peripheral nodes. Our node, created in 1998, changed its structure in 2004. Proactive approach was established since 2006, in addition to the registration of spontaneous reports. Notifications are incorporated into a database, and then sent to national regulatory agency.
Methods: The notifications are incorporated into a database (SQL), in addition to being sent to ANMAT. We describe the notifications received (demographics and types of events reported; side effects, ineffectiveness or failure of quality) and the result of the intervention of analytical INAME, when it was required.
Results: From November 2004 to May 2011, 3003 notifications were received. There was no difference between sex, with a low proportion of pediatric patients (3.36%) and high proportion of elderly (>60 years) patients (1207, 39.09%). Most notifications corresponded to adverse effects (2853, 95%), followed by cases of lack of efficacy (123, 4.1%). The degree of severity was mild in the majority (2190, 76.76%), followed by severe (398, 13.95%) and moderate (265, 9.29%). The largest categories of drugs involved in adverse effects were antimicrobials (30.67%), drugs for cardiovascular disorders (23.24%), drugs for CNS disorders (15.21%), antineoplastics (7.71%), NSAIDs (5.57%) and drugs for lung diseases (3.58%). Among all (2853) adverse event notifications, 398 (13.95%) were serious adverse events, including cases of 254 (63.82%) hospital admissions, 98 (24.62%) prolonging an existing hospitalization, 41 (10.30%) life threatening diseases, 4 (1.01%) deads, and 1 (0.25%) persistent incapacity. Among cases of lack of efficacy the most frequently involved were cardiovascular drugs (20.00%), antimicrobials (20.00%) neurological drugs (19.33%), and NSAIDs (12.67%). All samples of products involved in notifications of failure of efficacy or quality were sent to the National Institute of Medicines (INAME). Strikingly all but one case (early in 2008) were subjected to quantitative analysis and reported as “meets the specifications.”
Conclusions: The presence of old people and groups involved in drug side effects is consistent with data from other pharmacovigilance studies. The unit obtained a gradual and sustained increase in the number of notifications received by adopting a proactive approach. Possible causes of lack of notification by the health professionals seem to include ignorance, fear, lack of time, lack of incorporation of the drug, and lack of necessary data, among others. The proactive approach allows the systematic inculcation of side effects and effectiveness evaluation as part of the activity.
PP115. Pharmacovigilance on Hospital Admission: Medication Lists and Beyond
P.A. Alvarez,1 V. Castro,2 F .Santini,1 C. Soler,1 R. Gutierrez,1 F .Bril,1 G.A. Keller,3 G. Di Girolamo 3 and C. Lopez Saubidet 1
1 Internal Medicine Department, Centro de Educación Médica e Investigación Clínica Dr. Norberto Quirno (CEMIC), Ciudad Autónoma de Buenos Aires, República Argentina;
2 Pharmacy Department, Centro de Educación Médica e Investigación Clínica Dr. Norberto Quirno (CEMIC), Ciudad Autónoma de Buenos Aires, República Argentina;
3 Pharmacovigilance Unit. Second Chair of Pharmacology, School of Medicine, Universidad de Buenos Aires, Ciudad Autónoma de Buenos Aires, República Argentina
Background: Medication documentation on hospital admission is crucial for providing adequate medical care. At epidemiological level may provide insight to drug using patterns in the community and alert of inappropriate and probably dangerous use of medications or omission of potentially useful therapeutic agents.
Objective/Aim: The aim of the present study was to describe clinical characteristics and medication utilization among patients admitted to an Internal Medicine Ward in a University Teaching Hospital in Argentina.
Methods: Each of the patients admitted from August 2010 to December 2011 were evaluated by a member ofthe Pharmacovigilance team. A form was completed that included the medications and relevant medical history. Consults, transfers from other units were excluded. The information was stored in a database for analysis.
Results: There were 426 hospital admissions (236 women, 55.4%) with an average age of 68 years (range 19–101, SD 19) and history of hypertension (183, 42.96%), dyslipidemia (109, 25.59%), cancer (77, 18.08%), diabetes (59, 13.85%) dementia (58, 13.62%), coronary disease (55, 12.91%), heart failure (51, 11.97%) renal transplant (51, 11.97%), cerebrovascular disease (29, 6.81%), gastroduodenal disease (24, 5.63%), and AIDS (7, 1.64%). The mean Charlson score was 3.71 (0–13, SD 2.24) and ADL4.67 (0–6, SD 2.31). Each patient received an average of 5 (0–18, SD 3) simultaneous drug prior to admission. The most frequent drug were omeprazole (123, 28.87%), aspirin (101, 23.71%), meprednisona (82, 19.25%), and furosemide (58, 13.62%). In the case of omeprazole only 11 (8.94%) had a history of gastroduodenal pathology. Of all patients, 93 were older than 80 (21.83%) without dementia, receiving an average of 5 simultaneous drugs (0–12 SD 3), being the most frequent: omeprazole and aspirin (29, 31.18% each drug), furosemide (25, 26.88%), levothyroxine (22, 23.66%), ate-nolol (19, 20.43%), spironolactone and amiodarone (16, 17.20% for each drug). Of all patients, 33 (7.75%) have dementia and ADL score 0, receiving an average of 5 simultaneous drugs (0-12 SD 3), being the most frequent drugs: Clonazepam (10, 30.30%), aspirin (9, 27.27%), and omeprazole (6, 18.18%). Of all patients with a history of coronary disease (55, 12.91%) only 30 (54.55%) received aspirin.
Discussion: The use of large amounts of drugs in the elderly, omeprazole overuse and underuse of aspirin are examples of irrational drug use.
Conclusion: The use of databases on drug use helps the recognition of the situation, and evaluation of strategies to promote rational drug use.
PP116. Adverse Drug Events as a Reason for Admission in a University Teaching Hospital in Argentina
P.A. Alvarez,1 V. Castro,2 F .Santini,1 C. Soler,1 R. Gutierrez, F .Bril,1 G.A. Keller,3 G. Di Girolamo 3 and C. Lopez Saubidet 1
1 Internal Medicine Department, Centro de Educación Médica e Investigación Clínica Dr. Norberto Quirno (CEMIC), Ciudad Autónoma de Buenos Aires, República Argentina
2 Pharmacy Department, Centro de Educación Médica e Investigación Clínica Dr. Norberto Quirno (CEMIC), Ciudad Autónoma de Buenos Aires, República Argentina;
3 Pharmacovigilance Unit, Second Chair of Pharmacology, School of Medicine, Universidad de Buenos Aires, Ciudad Autónoma de Buenos Aires, República Argentina
Background: Adverse drug events are an importance cause of morbidity and mortality.
Objective/Aim: To study the prevalence of Adverse Drug Reactions (ADR) as a reason for admission to an Internal Medicine Ward in a University Teaching Hospital in Argentina.
Methods: A pharmacovigilance team evaluated each of the admissions to a Internal Medicine Ward from August 2010 to December 2011. The reason Causality was evaluated using OMS scoring system as defined, probable, possible, improvable or unclassified categories.
Results: There were 426 admissions. The causes of hospitalization were 40 adverse drug reaction classified as provable causality (9.39%), 62 possible causality (14.55%), 58 Improbable (13.62%), and 266 without relation to drugs (62.44%). Considering only the probable and possible adverse events compared to other categories, the relative risk to present an adverse drug reaction related to different known medical history characteristics were significantly increased only for: heart failure history (2.45, IC 1.33–4.51). Compared with patients admitted without ADE there were not differences regarding: age, gender, other comorbidities, or number of medications. adverse events causing hospital admission were 7 gastrointestinal bleeding (17.5%), 4 pneumonia (10.0%), 3 impaired consciousness (7.5%), 3 diarrhea (7.5%), 3 Febrile Neutropenia (7.5%), 2 Hyponatremia (5%), 2 IRA (5%), 2 confusional syndrome (5%), and 1 case (2.5%) of each of the following: acute abdomen, dehydration, encephalopathy, epistaxis, fever, pathological fracture, hypercalcemia, hyperkalemia, sepsis associated with catheter infection, urinary tract infection, meningitis, pancreatitis and sinusitis. The more frequent drug involved in adverse drug reaction were Meprednisone (9, 22.50%), aspirin (4, 10.00%), Capecitabine (3, 7.50%), Cytarabine (3, 7.50%), myco-phenolate (3, 7.50%) and Tacrolimus (3, 7.50%). Grouping adverse events using the MedDRA classification, the most frequent class was infections (8 admissions, 20.0%). This is consistent with the analysis of disproportionality ratios (DPR), which show a significant risk of hospitalization due to adverse events for: meprednisone, tacrolimus and mycophenolate. Other drugs with high DPR were NSAIDs and nephrotoxic antimicrobials (vancomycin, colistin, cefalotine).
Discussion: Adverse drug events continue to be a major cause of hospitalization. Their study shows the existence of clear risk factors that can be easily obtained from the patient’s history and the listing of drugs used.
PP117. Evaluation of QT-Interval Prolongation: Detection of most Frequently Associated Drugs in Clinical Oncology
C. Bagnes,1 G.A. Keller,2 P.A. Alvarez,3 M.L. Ponte,4 W. Belloso,5 A. Campos 6 and G. Di Girolamo 6
1 Oncology Unit, Hospital General de Agudos Dr Enrique Tornú, Ciudad Autónoma de Buenos Aires, República Argentina;
2 Emergency Department, Hospital General de Agudos Donación Francisco J Santojanni, Ciudad Autónoma de Buenos Aires, República Argentina; Pharmacovigilance Unit, Second Chair of Pharmacovigilance, School of Medicine, Universidad de Buenos Aires, Ciudad Autónoma de Buenos Aires, República Argentina;
3 Cardiology Division, Hospital de Clínicas José de San Martín, Ciudad Autónoma de Buenos Aires, República Argentina; Pharmacovigilance Unit, Second Chair of Pharmacovigilance, School of Medicine, Universidad de Buenos Aires, Ciudad Autónoma de Buenos Aires, República Argentina;
4 Internal Medicine Department, Hospital General de Agudos Dr Cosme Argerich, Ciudad Autónoma de Buenos Aires, República Argentina; Pharmacovigilance Unit, Second Chair of Pharmacovigilance, School of Medicine, Universidad de Buenos Aires, Ciudad Autónoma de Buenos Aires, República Argentina;
5 Clinical Pharmacology Section, Hospital Italiano, Ciudad Autónoma de Buenos Aires, República Argentina;
6 Pharmacovigilance Unit, Second Chair of Pharmacovigilance, School of Medicine, Universidad de Buenos Aires, Ciudad Autónoma de Buenos Aires, República Argentina
Introduction: QT interval prolongation induced by oncology drugs is a frequent adverse event. Its prevalence and association with morbidity remains unknown. The aim of the study is to determine its prevalence in clinical oncology practice, related drugs, and clinical characteristics.
Materials-methods: We included patients consecutively admitted to chemotherapy cycles in one oncology specialized university hospital. An electrocardiogram was performed at baseline, and after drug chemotherapy infusion. The QT interval between the Q wave onset and end of the T wave in the electrocardiogram was quantified in milliseconds and corrected (QTc) by Bazzet formula. It was felt that QTc interval prolongation showing a delta between admission and treatment more than 20 ms.
Results: Between January and Mayo 2011,44 patients (20 men, 45.4%) were included. the average age of patients was 63.4 years (SD 12.6 years), BMI 25.5 (SD 4.11) kg/m2, and received a total of 134 infusions of chemotherapy (average 3 per subject). The drug most frequently used was platinum compounds (63.6%). The mean ± SD baseline and post-treatment QTc were: 434.5±29.9 msec (median 436.0, Q25i: 416.0, Q75s: 448.0msec) and 442.8±29.2msec (median 442.0, Q25i: 429.0, Q75s: 459.0 msec) respectively. The difference between them was 8.3 msec (95% CI 0.8, 15.8 ms, p = 0.03). In the cases with normal QTc at baseline, 21.6% (95% CI: 14.3%, 28.9%) had QTc elevation above normal limits after administration of chemotherapy. Of the total number of cases, 13.6% of patients had at least two episodes of prolonged QTc during chemotherapy. Two percent of patients had five episodes of prolonged QTc. Of the 44 patients enrolled, 9 had an episode of QTc interval prolongation (20.5%), 4 had two (9.1 %), 1 had 3 episodes and 1 had five episodes.
Discussion: Drug induced QT interval prolongation is a frequent event during chemotherapy infusion. Risk factors and related drugs should be recognized by medical professionals in order to reduce their frequency by proper control of related factors. ECG and laboratory monitoring must be essential in clinical oncology in order to not add a new cause of morbidity like as QT interval prolongation.
PP118. Evaluation of QT-Interval Prolongation: A Multicenter Study to Detect Drugs more Frequently Associated in the Clinical Practice
G.A. Keller,1 P.A. Alvarez,2 M.L. Ponte,3 W. Belloso,4 C. Bagnes,5 A. Campos 6 and G. Di Girolamo 6
1 Emergency Department, Hospital General de Agudos Donación Francisco J Santojanni, Ciudad Autónoma de Buenos Aires, República Argentina; Pharmacovigilance Unit, Second Chair of Pharmacovigilance, School of Medicine, Universidad de Buenos Aires, Ciudad Autónoma de Buenos Aires, República Argentina;
2 Cardiology Division, Hospital de Clínicas José de San Martín, Ciudad Autónoma de Buenos Aires, República Argentina; Pharmacovigilance Unit, Second Chair of Pharmacovigilance, School of Medicine, Universidad de Buenos Aires, Ciudad Autónoma de Buenos Aires, República Argentina;
3 Internal Medicine Department, Hospital General de Agudos Dr Cosme Argerich, Ciudad Autónoma de Buenos Aires, República Argentina; Pharmacovigilance Unit, Second Chair of Pharmacovigilance, School of Medicine, Universidad de Buenos Aires, Ciudad Autónoma de Buenos Aires, República Argentina;
4 Clinical Pharmacology Section, Hospital Italiano, Ciudad Autónoma de Buenos Aires, República Argentina;
5 Oncology Unit, Hospital General de Agudos Dr Enrique Tornú, Ciudad Autónoma de Buenos Aires, República Argentina;
6 Pharmacovigilance Unit, Second Chair of Pharmacovigilance, School of Medicine, Universidad de Buenos Aires, Ciudad Autónoma de Buenos Aires, República Argentina
Introduction: QT interval prolongation induced by drugs is a major adverse event associated with morbidity and mortality, and is the most common cause of drug withdrawal from the market in recent years. The aim of the study is to determine its prevalence in clinical practice and related drugs.
Materials-Methods: We included patients consecutively admitted to three hospitals. An electrocardiogram was performed at baseline, during and after drug treatment indicated. The QT interval between the Q wave onset and end of the T wave in the electrocardiogram was quantified in milliseconds and corrected by Bazzet formula. It was felt that QTc interval prolongation showing a delta between admission and treatment more than 20 ms.
Results: Between January and May 2011, 368 patients (204 men, 55%) were included. We analyzed a total of 1082 ECG (3 ECG per patient) and a total of 1020 laboratories. The average age was 59 years (18–97, SD 19), weight 74 kg (44–150, SD 14), height 168 cm (150–191, SD 9). The clinical history revealed a history of ischemic cardiomyopathy (12.0%), arrhythmia (10.9%), diabetes (9.8%), heart failure (9.2%), CNS diseases (6.0%), hypertrophic cardiomyopathy (5.7%), hypothyroidism (4.9%), and renal failure (3.5%). Prior to the start of drug treatment, patients had [mean (range, SD)]: Na 138 (122-149, 5), K 4.2 (2.3–6.9, 0.8), RR ‘824 (320–2200, 240), QT 387 (200–600, 34), QTc 431 (316–600, 34). After the start of drug treatment: Na 137 (115–148, 5), K 4.2 (2.7–4.7, 0.8), RR ’804 (360–2400, 191), QT 389 (200–720, 52), QTc 437 (283–581, 34). After treatment ends: Na 138 (125–149, 5), K 4.3 (2.6–5.7, 0.8), RR s’828 (520–2080, 158), QT 392 (320–800, 50), QTc 432 (320–730, 34). There were 79 detected cases (21.47% of patients) with QT interval prolongation greater than 20 ms compared to baseline ECG, probably related to the use of drugs. The most commonly used drugs in patients with prolonged QT interval were dextropropoxyphene (24), furosemide (9), omeprazole (7), amiodarone (6), ciprofloxacin 6), fentanyl (5), and clarithromycin (3).
Discussion: Drug induced QT interval prolongation is a frequent event in clinical practice. Risk factors and related drugs should be recognized by medical professionals in order to reduce their frequency by proper control of predisposing factors and ECG and laboratory monitoring.
PP119. Suicide Attempts in Mali
H. Hami,1 T. Diallo,2 A. Maïga,3 A. Mokhtari 1 and A. Soulaymani 1
1 Laboratory of Genetic and Biometry, Faculty of Sciences, Ibn Tofail University, Kenitra, Morocco;
2 Laboratory of Genetic and Biometry, Faculty of Sciences, Ibn Tofail University, Kenitra, Morocco; Faculty of Medicine, Pharmacy and Odonto-stomatology, Bamako, Mali;
3 Faculty of Medicine, Pharmacy and Odonto-stomatology, Bamako, Mali
Objectives: The aim of this study is to determine the profile of persons who made a suicide attempt by voluntary ingestion of toxic products in order to identify individuals and groups at high risk.
Methods: A descriptive retrospective study of voluntary poisoning cases, notified between 2000 and 2010 by two University Hospitals (CHU) and six Health Reference Centers (CSREF) in Bamako, was conducted.
Results: During the period of study, 393 suicide attempts in a cohort of 641 voluntary poisoning cases, were declared, that is 61.3%. Most of suicide attempters are teenagers and young adults aged 15–24 years (63.2%). For this age bracket, the number of suicide attempts is 19 times higher than that for successful suicides. Women make 2.36 times more suicide attempts than men (though men succeed more often than women). The medication intake is the primary means employed by suicide attempters (73.5%), followed by industrial products (14.5%). The poisoning symptoms are extremely varied, depending on involved toxins, the ingested quantity and the delay before treatment.
Conclusions: During their hospitalization, suicide attempters should receive careful medical and psychiatric supervision to avoid the risk of recurrence.
PP120. High Dimensional versus Conventional Propensity Score Matching to Reduce Confounding in a Study of Coxibs versus Nonselective NSAIDS and Gastrointestinal Complications
E. Garbe,1 S. Kloss,1 W. Schill,1 M. Suling 1 and S. Schneeweiss 2
1 Bremen Institute for Prevention Research and Social Medicine, Bremen, Germany;
2 Department of Epidemiology, Harvard Medical School, Boston, MA, USA
Objectives: High dimensional propensity score (hd-PS) adjustment has been proposed to improve control for confounding in pharmacoepi-demiologic studies using longitudinal claims databases, as large numbers of empirically identified covariates may collectively serve as proxies for unobserved confounding.[1] To compare results based on hd-PS matching versus conventional PS matching in a cohort study of coxibs versus nonselective (ns)NSAIDS and their association with gastrointestinal (GI) complications.
Methods: A cohort of new users of coxibs or nsNSAIDs was identified in the German Pharmacoepidemiological Research Database (GePaRD) and followed until discontinuation or switch of the initial NSAID, disenrollment, hospitalization for GI complication, death or end of study period whichever was earliest. Conventional PS based on 79 investigator-identified covariates and hd-PS based on 200, 500, 700 or 900 empirically identified covariates were estimated by logistic regression analysis. Initiators of coxibs were 1:1 matched to initiators of nsNSAIDs using nearest neighbour matching. Rate ratios (RR) of GI complications (haemorrhage, perforation or obstruction) associated with coxibs or nsNSAIDs were calculated with Poisson regression analysis in the full cohort and in each of the resulting matched cohorts.
Results: 37281 coxib users and 2 104614 nsNSAID users were identified. The crude RR of upper GI complications for coxib users versus nsNSAID users in this cohort was 1.21 [95% CI = 0.91, 1.61]. Conventional and hd-PS matched 37 281 nsNSAID to the 37 281 coxib users. The conventional PS resulted in a RR of 0.84 [0.56-1.26]. Using the hd-PS algorithm to identify 900 empirical covariates and additionally including age, sex, calendar year and the number of distinct drugsduring 180 days befo re cohort entry as a measure of health service intensity resulted in a RR of 0.62 [0.43-0.91].
Conclusions: hd-PS matching compared to conventional PS matching resulted in improved point estimates for treatment effects of COX-2 selective versus nsNSAIDS when benchmarked against results expected from randomized clinical trials.
PP121. Risk of Subarachnoid Hemorrhage Associated with Outpatient Anticoagulant Use
S.Behr and E. Garbe
Bremen Institute for Prevention Research and Social Medicine, Bremen, Germany
Objectives: Subarachnoid hemorrhage (SAH) accounts for 5–10% of all strokes. Drugs have not been systematically studied as risk factors for SAH. To investigate the risk of SAH associated with drug treatment with special emphasis on anticoagulant drugs.
Methods: We conducted a nested case-control study in a cohort of 13.4 million insurants of 4 German statutory health insurances (SHIs) in the German Pharmacoepidemiological Research Database. Patients were required to be continuously enrolled for 6 months prior to cohort entry. Cases were patients hospitalized for SAH between July 2004 and November 2006. Ten controls were matched to each case by SHI, year of birth and sex using risk set sampling. We used conditional logistic regression analyses to estimate odds ratios (OR) of SAH for phenprocoumon and heparin considering multiple risk factors.
Results: Analysis of the full cohort revealed an increase in incidence of SAH with increasing age and a higher incidence for female sex. The nested case-control study included 2065 cases of SAH and 20649 matched controls. The multivariate analysis showed increased risks of SAH for phenprocoumon exposure (OR: 1.73, 95% CI 1.29, 2.34), clopidogrel/ticlopidine (OR: 1.63, 95% CI 1.10, 2.43), ASA(OR= 1.53, 95% CI 1.18, 1.99)and SSRI (OR: 1.67, 95% CI 1.19, 2.23), There was no increased risk observed for heparin. Our study confirmed known risk factors with highest risks observed for recent history of SAH, cerebral aneurysm and polycystic renal disease.
Conclusions: In contrast to a recent study[1] which did not find an increased risk of SAH associated with vitamin K antagonists, the vitamin K antagonist phenprocoumon and platelet inhibitors were associated with an increased risk of SAH in our study.
PP122. Persistence of Pharmacological Treatment into Adulthood for ADHD Patients who Started Treatment in Childhood or Adolescence in UK Primary Care
S. Mccarthy,1 L Wilton,2 M. Murray,2 P. Hodgkins,3 P. Asherson 4 and I.C. Wong 5
1 School of Pharmacy, University College Cork, Cork, Ireland;
2 Centre for Paediatric Pharmacy Research, School of Pharmacy, University of London, UK;
3 Shire Pharmaceuticals, Wayne, Pennsylvania, USA Wayne, PA, USA;
4 MRC Social, Genetic and Developmental Psychiatry Centre, Institute of Psychiatry, London;
5 Department of Pharmacology and Pharmacy, Li Ka Shing Faculty of Medicine, The University of Hong Kong, Hong Kong
Background: Studies conducted into persistence of ADHD from childhood into adulthood have reported rates of persistence of approximately 65%, when symptomatic definition of remission is used.[1] Recent ADHD guidelines suggest that for children and adults who respond adequately to pharmacological treatment, such treatment should continue for as long as it remains clinically effective, subject to regular review.[2] However the extent to which patients persist with pharmacological treatment during the transition from childhood/ adolescence into adulthood is not well known.
Objectives: To estimate the persistence of ADHD pharmacological treatment by patients who started pharmacological treatment aged 6–17 years. To estimate the percentage who continued such treatment into adulthood, in the UK primary care setting.
Methods: The Health Improvement Network (THIN) database was used to identify patients aged ≥6 years with a diagnosis of ADHD/HKD and a prescription for methylphenidate, dexamfetamine or atomoxetine (study drugs) coded on the database from 2003–2008. From this cohort, patients who received their first prescription on the database for a study drug aged 6–17 years were identified. Patients were monitored until their ‘censored date’ (e.g. end of study period; date transferred out of practice). To ascertain their treatment status in adulthood, only patients with data on the database at age ≥18 years were included in the study. Persistence of pharmacological treatment was estimated using Kaplan-Meier (KM) analysis and the percentage of patients who continued pharmacological treatment into adulthood was calculated.
Results: 2376 patients started pharmacological treatment aged 6–12 years; 213 of whom had data at >18 years. From KM analysis, median treatment duration was 5.9 years. 61.5% (131/213) stopped treatment before 18 years, 38.5% (82/213) remained on treatment aged ≥18 years. 898 patients started pharmacological treatment aged 13–17 years, of whom 397 had data at >18 years. From KM analysis, median treatment duration was 1.6 years. 57.2% (227/397) of patients stopped treatment before 18 years, 42.8% (170/397) remained on treatment aged ≥18 years.
Conclusions: Persistence of pharmacological treatment into adulthood for those who started treatment as children or as adolescents was lower (∼40%) than published rates of persistence of ADHD (approximately 65%). Due to the limited number of patients who had data past 18 years at the time of this study, it is important that monitoring of GP prescribing patterns into later adulthood is continued, in particular to observe the impact of recent guideline recommendations on the pharmacological treatment of this condition in this age group.
PP123. The Epidemiology of Pharmacologically-Treated Attention Deficit Hyperactivity Disorder (ADHD) in Children, Adolescents and Adults in UK Primary Care
S. McCarthy,1 L. Wilton,2 M. Murray,2 P. Hodgkins,3 P. Asherson 4 and I.C. Wong 5
1 School of Pharmacy, University College Cork, Cork, Ireland;
2 Centre for Paediatric Pharmacy Research, School of Pharmacy, University of London, UK;
3 Shire Pharmaceuticals, Wayne, PA, USA;
4 MRC Social, Genetic and Developmental Psychiatry Centre, Institute of Psychiatry, London, UK
5 Department of Pharmacology and Pharmacy, Li Ka Shing Faculty of Medicine, The University of Hong Kong, Hong Kong
Background: Attention Deficit Hyperactivity Disorder (ADHD) is a neurodevelopmental disorder characterised by symptoms of inattention, impulsivity and hyperactivity. Prevalence of ADHD in school-aged children and adolescents in the United Kingdom (UK) using DSM-IV criteria is estimated at 5%.[1] ADHD was perceived as a condition of childhood only; increasing evidence has highlighted the existence of ADHD in older adolescents and adults. Estimates for prevalence of ADHD in adults range from 2.5–4%.[2–5] Few data exist on prescribing trends of methylphenidate, dexamfetamine and atomoxetine in UK.
Objectives: To investigate prevalence and incidence of pharmacologically-treated ADHD in children, adolescents and adults in UK primary care.
Methods: The Health Improvement Network (THIN) database was used to identify all patients aged ≥6 years with a diagnosis of ADHD/HKD and prescription for methylphenidate, dexamfetamine or atomoxetine from 2003–2008. Annual prevalence and incidence of pharmacologically-treated ADHD in patients on THIN database were calculated by age category and sex.
Results: 4530 patients (3874 male, 85.5%) met the inclusion criteria and received 118 929 prescriptions for study drugs. Annual Prevalence of pharmacologically-treated ADHD (per 1000 mid-year population aged >6 years on THIN database) increased within each age category 2003 to 2008; although it decreased with increasing age, in each year. Figures for 2003 and 2008 are shown 6–12 years: 4.185 (95% CI: 3.939, 4.441) - 8.286 (95% CI: 7.929, 8.655) 13–17 years: 3.142 (95% CI: 2.886, 3.415)- 6.698 (95% CI: 6.339, 7.073) 18–24 years: 0.218 (95% CI: 0.163, 0.287)- 0.972 (95% CI: 0.858, 1.098) 25–45 years: 0.014 (95% CI: 0.008, 0.024)- 0.069 (95% CI: 0.053, 0.088) >45 years: 0.007 (95% CI: 0.003, 0.013) - 0.017 (95% CI: 0.011, 0.026) Whilst male patients aged 6–12 years had the highest prevalence; the relative increase in prescribing was higher for female patients of the same age (relative increase in prevalence 2.15 for females aged 6–12 years; 1.96 for males 6–12 years) (Table I).
The incidence of pharmacologically-treated ADHD (per 1000 midyear population aged >6 years at risk on THIN database) increased over the study period. Incidence was highest for males aged 6–12 years.
Conclusions: Prevalence of pharmacologically treated ADHD increased over the period 2003–2008, in all age categories and for both male and female patients. However the numbers of pharmacologically-treated adult ADHD patients are much lower than the published estimated prevalence of ADHD in this age group. This study has added to the limited knowledge on prescribing for ADHD in primary care, particularly surrounding drug treatment in adulthood.
PP124. Development of Search Strategies to Identify Reports of Off-Label Drug Use in EMBASE
B. Mesgarpour,1 M. Müller 1 and H. Herkner 2
1 Department of Clinical Pharmacology, Medical University of Vienna, Vienna, Austria;
2 Department of Emergency Medicine, Medical University of Vienna, Vienna, Austria
Background: Prescription for off-label purposes of approved medications has been reported commonplace despite lack of sufficient evidence. A growing body of studies on creative use of medications attempts to provide supporting data for off-label use of drugs.
Objectives: Since reports of using certified medications in uncertified indications are varying in terms of description and study type, off-label drug use studies are not easy to locate in bibliographic databases. Our objective was to develop a search strategy that facilitates detection of the off-label drug use documents in EMBASE via OvidSP.
Methods: OvidSP EMBASE was searched from 1988 to 28 February of 2011. Search queries, including search words and strings, were conceived based on definitions of off-label use of medications. The retrieval performance of the selected search terms was compared with a gold standard reference set in this study. The gold standard was compiled from reports of off-label drug use identified by a sensitive search of MEDLINE and EMBASE.
Results: From 6151 retrieved documents, 3846 (62.5%) off-label drug use studies were found, “off label*.af.” was the most sensitive single term (sensitivity 77.5%, precision 88.1%). The highest sensitive search strategy was achieved by combining 36 search queries with sensitivity of 94.0% and precision of 69.5%. An optimal sensitive and precise search strategy was yielded precision 87.4% at the expense of decreasing sensitivity to 89.4%.
Conclusions: The retrieval of off-label drug use documents in EMBASE can be enhanced by application of empirically derived search strategies.
PP125. Detecting Adverse Drug Event by Trigger Tool at a Province Hospital, Thailand
P. Tragulpiankit,1 N. Yeesoonpan,1 W. Keratitechakorn,2 T. Ninsananda,3 T. Uaviseswong,1 U. Chaikledkaew,1 B. Chindavijak,1 S. Chulavatnatol 1 and Adcopt Working Team 3
1 Faculty of Pharmacy, Mahidol University, Bangkok, Thailand;
2 Pharmacy Department, Mongkut Memorial, Phetchaburi Province, Thailand;
3 The Association of Hospital Pharmacy (Thailand), Bangkok, Thailand
Background: The first step for preventing drug-induced harm is an effective method for adverse drug event (ADE) detecting. Unfortunately, traditional ADE detection has been limited in daily practice. The trigger tool has been developed for increasing ability to ADE detection.[1]
Objectives: To determine the frequency characteristics of ADEs by the Institute of Healthcare Improvement (IHI) trigger tool for ADE detecting [1] and to evaluate the tool in hospitalized patients.
Methods: This cross-sectional study was an observational design at medical wards, one province hospital. IHI ADE trigger tool which consisted of 24 triggers were looked by retrospectively manual chart review and then suspected ADE was determined. The numbers of positive triggers were recorded. The trigger detection data and ADE detection data were analyzed using descriptive statistics.
Results: Total 300 medical records were reviewed and found total 35 ADEs suffered from 33 (11.0%) patients. ADE related to hospital admission was 25 events. Total 13 (37.1%) preventable ADEs were determined. Total 27 (77.1 %) ADEs were categorized into F severity level (an events may have contributed to or resulted in temporary harm to the patient and required initial or prolong hospitalization). Antidiabetic drugs were common drug groups caused adverse events by 9 out of 35 ADEs (25.7%). Total 13 triggers found in the present study and 11 positive triggers were found. Table I shows the number of trigger found and positive triggers with their percentage.
Conclusions: Although the trigger tool for ADE detection seemed to be not gold standard of ADE detection, this method resulted in relatively increasing the number of ADE detection.
Discussion: The results of positive triggers and ADE occurring suggest to modification of ADE triggers in Thai hospitalized patients. The combination of triggers which matched in drug utilization and clinical practice should be developed.
PP126. Is Chest Pain Related to Ischemic Heart Diseases Only in Cardiac Patients?
H.A. Abdulrazzaq,1 S. Syed Sulaiman,1 Y.W. Kassab 1 and O. Ismail 2
1 Deaprtment of Clinical Pharmacy, Pharmacy School, USM, Malaysia;
2 Department of Cardiology, Penang Hospital, Pulau Pinang, Malaysia
Background: Many studies found that chest pain is the common symptoms to ischemic heart diseases (IHD) like angina and myocardial infarction,[1,2] but few determined the contributing factors like concurrent medications and demographic data. Other studies found that several medications like statin caused muscles problems.[3–5]
Objectives: Are to determine the incidence of chest pain. Also prediction the contributing factors like demographic data, concurrent medications and diseases.
Method: Cross-sectional study conducted to 500 cardiac outpatients of Penang General Hospital, Malaysia. Validated questionnaire used to collect the patients complains on chest pain. Patients voluntarily took part in this study and approval got from the Clinical Research Committee (CRC) of hospital. Demographic data, information of concurrent diseases and medications collected from patients’ progress file. SPSS version 18 used in analysis of collected data, and statistical tests used are logistic regression and chi-square. Results with p value less than 0.05 considered significant.
Results: The incidence of chest pain in this study found 42.2%. The incidence of severity levels of chest pain was; 24.8%, 13.4% and 4% for mild, moderate and severe respectively. Significant factors increased ADRs incidences were; Indian race (48.12%, p = 0.008, OR = 2.2, CI = 1.2, 3.8), consumption of alcohol (59.6%, p = 0.002, OR = 3.9, 1.7-9.1), statin (27%, p = 0.03, OR= 1.5, CI= 1.1, 3.0), lovastatin dose 60 mg (82%, p = 0.01, OR=1.4, CI = 0.9, 2.1), and IHD (66.8%, p = 0.046, OR = 1.6, CI = 1.0, 2.6).
Conclusion: Chest pain was significantly higher associated with consuming of alcohol, followed by race, IHD, statin and lovastatin doses. It recommended stopping consuming of alcohol, changing in type of statin or dosing to reduce the adverse drug reactions induced by statin.
PP127. Skin Rash Induced by Statin in Cardiac Outpatients of Penang General Hospital, Malaysia
H.A. Abdulrazzaq,1 S. Syed Sulaiman,1 Y.W. Kassab 1 and O. Ismail 2
1 Deaprtment of Clinical Pharmacy, Pharmacy School, USM, Malaysia;
2 Department of Cardiology, Penang Hospital, Pulau Pinang, Malaysia
Background: Statin is the drug of choice to control cholesterol and prophylaxis to serious cardiovascular events.[1,2] About 90% of Malaysian cardiac patients use statin,[3] therefore, several adverse drug reactions (ADRs) induced by statin found during therapy. Many studies related to ADRs induced by statin,[4,5] but few related to minor ADRs like skin problems.
Objectives: Are to find out the incidence of skin rash in cardiac outpatients, and the contributing factors related to increase it.
Method: Cross-sectional design used to 500 cardiac outpatients. These patients participated voluntarily in reporting their ADRs. This study conducted in Cardiac Clinic of Penang General Hospital in Malaysia, and it approved from Clinical Research Committee (CRC) of hospital. Validated questionnaire used in reporting of skin rash. This reporting depended on patients beliefs about skin rash, and its severity divided into mild, moderate and severe. One point was given to mild, while two for moderate and three for severe case. The other information such as demographic data, statin information and concurrent diseases and medications collected from patients rogress file. SPSS version 18 was used to analyze the data, and statistical tests used were logistic regression and odd ratio (OR), and chi-square. All results with p value less than 0.05 considered significant.
Results: The incidence of skin rash found in cardiac outpatients was 24.2%. The incidence for mild, moderate and severe found 16.4%, 5.8% and 1.6%, respectively. After prediction the variables contributed in rising of incidence of skin rash. Chinese (27%, p = 0.01, OR = 1.97, CI = 1.17, 3.29), age more than 65 years old(31%,p = 0.019,OR = 2.02, CI = 1.13, 3.63), having ischemic heart disease (IHD) (64.7%, p = 0.042, OR=1.76, CI=1.02, 3.035), and statin (25%, p = 0.02, OR = 1.63, CI =1.1, 3.01) was very common.
Conclusion: High incidence of skin rash found in Malaysian cardiac outpatients. Race (Chinese), geriatric, IHD and statin the main contributed factors which increased the incidence of skin rash. The type of statin should be appropriately managed to avoid the incidence of skin rash.
PP128. Stevens-Johnson Syndrome and Drugs and Vaccines: A Case-Control Study in Children
F. Menniti Ippolito,1 R. Rossi,2 G. Traversa,1 R. Da Cas,1 C. Rafaniello,3 N. Mores,4 G. Bersani,4 N. Pirozzi,2 U. Raucci 2 and Italian Multicenter Study Group on Safety of Drugs and Vaccines in Children 1
1 National Centre of Epidemiology, National Institute of Health, Rome, Italy;
2 Department of Emergency, Anesthesia and Intensive Care, Children’s Hospital Bambino Gesù, Rome, Italy;
3 Department of Experimental Medicine, Section of Pharmacology “L Donatelli”, Second University of Naples, Naples, Italy;
4 Department of Pharmacology, Università Cattolica S. Cuore, Rome, Italy
Objectives: Cutaneous adverse drug reactions (CADRs) are the most common ADRs in children. Several studies have found CADRs to be the most prevalent ADRs in hospitalized children. The majority of CADRs in children are not considered serious, although they do account for a substantial proportion of clinical visits with an estimated 2% being severe and life threatening. Stevens-Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN) are severe cutaneous adverse drugs reactions, characterized by extensive detachment of epidermis and erosions of mucous membranes.[1,2] Since 1999 an active surveillance focusing on the role of drugs and vaccines in the occurrence of specific clinical conditions (among which cutaneous diseases) responsible for hospitalization in children has been conducted in Italy. The study coordinated by the Italian National Institute of Health involves nine pediatric hospitals or university wards.
The aim of this study was to estimate a possible association between drugs and vaccines and the occurrence of SJS in children.
Methods: All children hospitalized through the emergency department for a SJS, regardless of drug and vaccine use, were enrolled in the study. An analysis, performed according to a case-control design was conducted to estimate the risks of developing SJS and drug and vaccine use. Diagnosis was validated from the clinical records. Drug or vaccine exposure in children admitted with SJS (cases) was compared to similar exposures in children admitted for neurological disorders (controls). Drug and vaccine exposure was assessed interviewing parents in cases and controls during the hospitalization of children.
Results: From November 1999 to April 2011 we enrolled 36 cases with SJS and 1386 children with neurological disorders (excluding convulsions). Cases were younger than controls (median age 3 and 4 years respectively). As already reported in the literature antiepileptics presented the highest adjusted OR of developing SJS: 18.2 (95% CI 6.0, 55.1). An increased risk was observed also for antibiotics (OR = 4.9; 95% CI 2.4, 9.7), among these penicillins and cephalosporins showed risks higher than macrolides, respectively (OR=4.3; 95% CI 1.9, 9.7) and (OR=4.5; 95% CI 1.9, 10.7). The antibiotic with the highest OR was cephaclor (OR=7.0; 95% CI 1.9, 25.5). A moderate increased risk was estimated for the complex of NSAIDs (OR= 1.3; 95% CI 0.5, 3.8), among these niflumic acid presented a higher risk (OR = 3.9; 95% CI 0.9, 17.7). All ORs were adjusted for concomitant use of all other drugs.
Conclusions: This study confirms an etiologic role of specific drug categories in the occurrence of SJS also in children.
PP129. Intensive Monitoring Programme of Adverse Drug Reactions in Emergency Department (MEREAFaPS Study): The Tuscan Experience
M. Tuccori,1 A. Pergola,2 M. Rossi,3 A. Capogrosso,3 M. Moschini,4 A. Vannacci,4 F. Rimoli,5 E. Cecchi,6 E. Ruggiero,3 S. Mantarro,2 L. Picchianti,3 M.C. Leo,4 G. Giustarini,3 A. Testi,3 S. Montagnani,2 C. Scollo,2 M. Santini,7 L. Spisni,8 F. Mannelli,9 M.S. Verzuri,10 T. Corona 3 and C. Blandizzi 2
1 Unit of Pharmacology, University Hospital of Pisa, Pisa, Italy;
2 Interdepartemental Centre of Research in Clinical Pharmacology and Experimental Therapeutics, University of Pisa, Pisa, Italy;
3 Tuscan Regional Centre of Pharmacovigilance, Florence, Italy;
4 Department of Pharmacology, Centre for Molecular Medicine (CIMMBA), University of Florence, Florence, Italy;
5 Pharmaceutical Unit, Hospital of Prato, Prato, Italy;
6 Emergency Department, Hospital of Prato, Prato, Italy;
7 Emergency Department, University Hospital of Pisa, Pisa, Italy;
8 Emergency Department, Hospital of Pontedera, Pisa, Italy;
9 Emergency Department, University Hospital of Siena, Siena, Italy;
10Emergency Department, Pediatric University Hospital Meyer, Florence, Italy
Objectives: The MEREAFaPS study was aimed at investigating drug-related admission to the emergency department (ED). A preliminary analysis of data, recorded in 5 Tuscan EDs from 1st July 2010 to 31st May 2011, is presented.
Methods: The MEREAFaPS study is a three-year prospective cohort, observational, multicentre, multiregional, no profit study, coordinated by the Lombardy Pharmacovigilance Centre. Patients accessing ED for a possible adverse drug reaction(ADR) were included in the study. Clinical and demographic data were collected. Data presented in this analysis have been retrieved from three databases: MEREAFaPS for ED-ADR data, ED database for the number of ED admissions and the Italian database of spontaneous ADR reporting, held by the Italian Drug Agency (AIFA), for the overall number of ADR reports.
Results: During the study period, patients screened for possible ADR-related ED admission were 243 383. Overall, 2505 ADR reports from Tuscany were recorded in the Italian database of ADRs report, 837 (33.4%) of which were issued from the Tuscan MEREAFaPS network (frequency of ED admission due to ADR: 0.34%). Among these, 245 (28.7% of overall patients with ADR) described a serious event (227 required hospitalization). ADR involved 508 females (59.6%) and 344 males (40.4%), and the age range was 17–65 years. ADR outcomes were distributed as follows: 101 complete recovery; 3 recovery with sequelae; 498 improvements; 246 outcome not available; 1 death. The drugs most frequently involved in ADRs were: amoxicillin + clavulanic acid (94 reports), acetylsalicylic acid (39), furosemide (33), ketoprofen (32), warfarin (32), paracetamol (27), lansoprazole (25), amoxicillin (22), ibuprofen (22) and allopurinol (21). The system organ class most commonly involved in ADR was skin (n = 382), followed by gastrointestinal tract (n = 255), general disorders and administration site conditions (n= 153) and nervous system (n= 146).
Conclusions: Overall, our preliminary data indicate that ADRs are a common cause of ED admission. These events are often serious and require hospitalization. Conclusive data from this study will be helpful to achieve a better clinical definition of these adverse events, thus helping ED caregivers to better recognize and manage them.
PP130. EFEMERIS (Evaluation chez la Femme Enceinte des MEdicaments et de leurs RISques), the French Prescription Database in Pregnant Women: A 4 Year-Follow Up
I. Lacroix,1 C. Hurault Delarue,1 S. Kessler,2 C. Guitard,3 A. Berrebi,2 S. Vidal,4 C. Albouy Cossard,5 R. Bourrel,6 E. Elefant,7 J. Montastruc,1 H. Bagheri 1 and C. Damase Michel 3
1 Service de Pharmacologie Clinique, CHU de Toulouse, Inserm UMR1027, Toulouse, France;
2 Centre de Diagnostic Anténatal, CHU de Toulouse, Toulouse, France;
3 Service de Protection Maternelle et Infantile, Conseil Général de la Haute-Garonne, France;
4 Caisse Primaire d’Assurance Maladie de la Haute-Garonne, Toulouse, France;
5 Centre d’Etudes des Sécurités du Système d’Information, CNAMTS, Paris, France;
6 Caisse Régionale d’Assurance Maladie MidiPyrénées, Toulouse, France;
7 Centre de Référence sur les Agents Tératogènes, Paris, France
Due to lack of evaluation, teratogenicity of many drugs remains unknown and drug choice during pregnancy is often difficult for health professionals. In France, there is no systematic follow up of women exposed to drugs and their newborns.
Objectives: The main aim of this study is to move towards setting up the first French database of reimbursed drugs prescribed to pregnant women by associating records of the drugs prescribed and delivered during pregnancy until the outcome of these pregnancies.
Methods: EFEMERIS database was set up with the data on prescription drugs given to pregnant women recorded by the Caisse Primaire d’Assurance Maladie (CPAM) of Haute-Garonne and the outcomes of these pregnancies obtained from the Protection Maternelle et Infantile (child health certificates) and the Centre de Diagnostic Antenatal (medical pregnancy interruptions). Data collection currently concerns 4 years. Women delivered from July 1st 2004 to June 30th 2008 in Haute-Garonne and registered in the French Health Insurance Service are included into the EFEMERIS database.
Results: EFEMERIS includes 40 355 mother-outcome pairs (newborns or fetus if the pregnancy was stopped). The prevalence rate of congenital anomalies is 2.3%. Pregnant women are prescribed 10.8 ± 7.6 [0–78] different drugs. Among the twenty most frequently prescribed drugs, around half of them are not evaluated in pregnant women (phloroglucinol, dompéridone, diosminey). Among the drugs for which data is available, some with proven teratogenic or fcetotoxic effects are prescribed and delivered to pregnant patients included in the EFEMERIS database: retinoids, NSAIDs…
Conclusions: EFEMERIS is the first French database of drugs prescribed and dispensed during pregnancy including the outcome of these pregnancies (birth or medical termination of pregnancy). This database would constitute a monitoring centre for the prescription of drugs to pregnant women and would allow evaluating the potential teratogenic risk of drugs.
PP131. Poor Social Environment and Altered Nutritional Status are Associated with Adverse Drug Reactions: A Hospital-Based Case-Control Study
S. Dabadie,1 P. Noize,2 M. Vandenhende,3 G. Miremont Salamé,2 N. Moore,2 P. Morlat,3 J. Pometan 1 and F. Bonnet 3
1 Pharmacie de l’Hôpital Saint-André, Centre Hospitalier Universitaire, Bordeaux, France; 2 Centre Régional de Pharmacovigilance, Service de Pharmacologie, Centre Hospitalier Universitaire, Bordeaux, France; Inserm U657, Bordeaux, France; Université Bordeaux Segalen, Bordeaux, France; 3 Service de Médecine Interne et de Maladies Infectieuses, Hôpital Saint-André, Centre Hospitalier Universitaire, Bordeaux, France
Background: Hospitalizations related to adverse drug reactions (ADRs) represent a major public health issue. Many studies have been conducted to identify factors associated with ADRs, especially those inducing hospitalizations, but few have investigated the influence of disability and social environment.[1,2]
Objective/aim: To study the influence of social environment, disability and nutritional status on the occurrence of ADRs.
Methods: A case-control study was conducted in an internal medicine unit of a French teaching hospital. Cases were prospectively identified among patients admitted between April and October 2009 (n=501) as those presenting with ADRs at admission. Two controls per case (matched on gender and age ± 5 years) were selected among other admitted patients. Data regarding socio-demographic characteristics, social environment especially aids in daily living, medical history, drug use and biological tests at admission were collected through standardized interviews and medical files. Physical abilities and autonomy were evaluated with Karnofsky and MIF (≪ Mesure de l’Indépendance Fonctionnelle ≫) scores, cognitive performances with the Mini Mental State Examination and nutritional status with the Mini Nutritional Assessment. Cases and controls were compared using univariate then multivariate conditional logistic regression: factors associated with p < 0.25 in univariate analysis were included in the multivariate model.
Results: Thirty-six patients (7.2%) presented with at least one ADR (n = 66) at admission (mean age: 80.2 years, 72.2% of women). ADRs were predominantly coagulation/hematologic disorders due to antic-oagulant/antiplatelet drugs (37.9%), hydroelectrolytic disturbances due to antihypertensive/cardiologic drugs (24.2%) and neuropsychiatric disorders due to opioid analgesics/psychotropic drugs (12.1%). In most cases, ADRs were severe according to pharmacovigilance standards (94.4%) and caused the hospitalization (80.6%). After multivariate analysis (36 cases and 72 controls), five factors were independently associated with ADRs (odds ratio [95% confidence interval]): referral by emergency units (6.0 [1.2, 28.9]), no aids by relatives (19.4 [2.4, 156.4]), poor nutritional status (6.5 [1.8, 24.2]), low creatinine clearance (10.6 [2.3, 50.2] and five drugs or more at admission (6.9 [1.1, 42.9]). Pre-existing neuropsychiatric conditions, altered cognitive performances and a high level of disability tended to be associated with ADRs but only in the univariate analysis.
Conclusion/Discussion: Despite methodological limits due to the sample size, this study suggests that social environment, especially aids by relatives, and nutritional status influence the occurrence of ADRs in addition to well-known factors such as kidney failure or polymedication. Such aspects could be interestingly considered in prevention programmes.
PP132. Long-Term Increased Risk of Dementia in Elderly Benzodiazepine Users: Results from a Cohort Study
S. Billioti De Gage,1 B. Bégaud,1 H. Verdoux,2 J. Dartigues,3 K. Pérès,3 F. Bazin 4 and A. Pariente 1
1 INSERM, U657, Pharmacology Department, Bordeaux, France; 2 CH Charles Perrens, Psychiatry Department, Bordeaux, France; 3 INSERM U897, ISPED, Bordeaux; 4 Université Bordeaux Segalen, France
Background: Benzodiazepines (BZDs) are widely prescribed in the elderly. [1] Their use is mostly chronic in the elders, regardless of good practices guidelines.[2–4] The cognitive acute side effects of benzodiazepines are well known but their responsibility in long-term cognitive adverse effects remains controversial.[5] The validity of the existing studies showing an increased risk of dementia for BZD elderly users remains questionable mainly because of an insufficient follow-up with regard to the long prodromal phase of dementia.[6] However, as dementia incidence and BZD use are both high in the elderly, even a moderate increase in the risk of dementia related to this exposure would have a major public health impact.
Objective: To study the effect of BZD use on the risk of incident dementia over a long follow-up period to allow considering the prodromal phase of dementia.
Methods: A cohort study was conducted within the PAQUID programme that included 3777 elderly aged 65 and over in 1989 and offers up to 20 years of follow-up. Non-demented non-BZD prevalent users at follow-up year 5 of the PAQUID programme were eligible for this analysis, for which this follow-up date constituted subjects’ index. BZD incident use at index date was drawn from patient’s interview completed by drug packages inspection. The outcome of interest was the incidence of dementia after index date, as assessed at each follow-up of the PAQUID programme. Multivariate Cox proportional hazard models were conducted to evaluate the risk of dementia according to BZD incident use.
Results: Overall, 1063 subjects were included in the analysis, in whom 253 incident dementias were confirmed over a median follow-up of 6.2 years (IQR: 2.6-12.3). Controlling for traditional risk factors of dementia, BZD incident use was associated with an increased risk of dementia (Hazard Ratio, HR: 1.55; 95% CI: 1.04, 2.32). Sensitivity analyses ignoring the existence of depressive symptoms or excluding subjects with important cognitive declining trend at index date gave similar results (HR: 1.61; 95% CI: 1.09, 2.38 and HR: 1.57; 95% CI: 1.05, 2.35, respectively).
Conclusion: An increased risk of dementia was found in BZD incident users compared to non-users. The respect of the proportional hazard hypothesis over up to 15 years of follow-up without initial but temporary increase in the risk of dementia after BZD start minimizes the possibility of a protopathic bias. Considering dementia incidence and BZD use in elderly, this association could have major potential impact.
Post-Authorisation Safety Studies (PASS)
PP133. Enhancing the Presentation and Evaluation of Cumulative Post-Marketing Safety Data: A Pilot Study
A. Gilchrist, D. Layton, C. Fogg and S. Shakir
Drug Safety Research Unit, Southampton, UK; University of Portsmouth, Portsmouth, UK
Background: Utilising graphical tools for evaluating and displaying quantitative data enables a concise and rapid review of key safety aspects and facilities integration of these data within regulatory safety update reports. As part of the risk management plan, a Modified-Prescription Event Monitoring (M-PEM) study was initiated to monitor the safety and use of the chlorofluorocarbon (CFC) free formulation of Pulmicort® metered dose inhaler (MDI) in general practice.
Objectives: A pilot study to optimise the presentation and evaluation of M-PEM post-marketing interim safety data through integration of graphical display.
Methods: M-PEM exposure data for this interim report were collected from prescriptions dispensed between Dec 2008 and Nov 2010. Demographic, selected past medical history data (for the 3 months prior to prescription (Rx) start date) and outcome (event) data (for 3 months post Rx start date) were collected via questionnaires sent 3 months after first Rx date. Exposure data was stratified by patient subgroups [age; indication; dose; past use of Pulmicort8 MDI (switchers, naïve)] and summarised using patient exposure plots or box and whisker plots. ID event rates (95% CI) were also displayed graphically.
Results: The interim cohort comprised of 5519 patients, median age 33 years (IQR 8 to 61), 2666 (48.3%) male. Younger patients contributed less long term exposure data (>90 days) than older age groups [45.7% for <2 yrs (off label use), 68.4% for 2–12 yrs and 74.5% for >12 yrs]. Asthma was the most common indication (85.3%; n=4693), of which 75.1% (n = 3525) contributed long term exposure data. Long-term users tended to be those prescribed higher doses (>800 mcg/day; 78.8%, n = 1020) than lower doses (<400 mcg; 63.1 %, n = 1004), and be switchers rather than product-naive (84.9%, n=1884 and 59.3%, n=1440 respectively). The graphical display of ranked ID rates identified upper respiratory infection as the most frequent clinical event to occur in the first month of treatment [ID1-ID2-3= 12.10 (95% CI 8.64, 15.55)].
Conclusions: Plots of numbers of patients exposed by time can help describe exposure in different patient subgroups and identify sub-populations whose contribution to long-term safety data appears limited. Such graphical tools can also help identify unusual or extreme values. Effective display of key data optimises the integration of drug utilisation information within ongoing safety evaluations as part of risk management plans.
PP134. Analysis of Utilisation of Ibandronic Acid from Prescription-Event Monitoring (PEM): Focus on ‘Off Label’ Use in Support of Risk Management
A. Gilchrist, V. Osborne, D. Layton and S. Shakir
Drug Safety Research Unit, Southampton, UK; University of Portsmouth, Portsmouth, UK
Background: Ibandronic acid 150 mg/month (Bonviva©) is a bipho-sphonate that was licensed in the UK in 2005 for the treatment of post-menopausal osteoporosis in women. Prescription-Event Monitoring (PEM) is a non-interventional observational cohort technique conducted by the Drug Safety Research Unit (DSRU) to monitor the safety of newly marketed drugs prescribed in general practice in England.
Objectives: To describe the utilisation characteristics of patients prescribed ibandronic acid based on an analysis of a completed PEM cohort and to assess, where possible, if the product is being used outside terms of license of marketing approval.[1]
Methods: An observational cohort PEM study was conducted. Exposure data were collected from dispensed prescriptions issued by general practitioners (GPs) between November 2005 and November 2007. Outcome data (event, patient demographic and selected clinical characteristics) were collected by sending questionnaires (green forms) to GPs at least 6 months after the drug was first prescribed for an individual patient. Summary descriptive statistics were calculated. For this study, menopause was defined by female age at 50+ years.
Results: The cohort consisted of 11 034 patients, of which 9% (n = 991 patients) were reported to be male. Where age was specified, 4.8% (529/11017) were aged <50 years, of which 0.6% (3/529) were <20 years. 398 deaths occurred (3.6% cohort). Where specified, primary indications other than post-menopausal osteoporosis were reported for 11.7% (1218/10 446) patients including ‘prophylaxis’ (n = 715), ‘osteopenia’ (n = 231) and ‘fracture spontaneous’ (n = 41). The most frequently reported clinical reasons for stopping treatment were ‘intolerance’ (n=176) and ‘dyspepsia’ (n=158). There was 1 pregnancy, reported as the reason for stopping treatment. Where dose was specified, 99.9% of patients (8625/8637) were prescribed the approved dose of 150mg per month.
Conclusions: This study has highlighted that some clinicians are prescribing this product outside the recommended terms of the licence. Use in pre-menopausal women and men was reported. This study assumed natural menopause occurred when aged 50+ years, though this does not apply for surgically menopausal women. Prescribing for indications other than osteoporosis was common, but unusual dose regimens were uncommon. Drug utilisation studies are important in describing populations that may not have been adequately studied in terms of risk in pre-marketing development programmes and these are important in the postmarketing risk management of medicines.
PP135. Worldwide Survey on Post-Authorization Safety Studies: Review of International, Regional and National Guidelines
L Montigon, G. Ferreira, C. David and A. Khromava
Sanofi Pasteur, Global Pharmacovigilance and Pharmacoepidemiology, Lyon, France
Background: Several guidelines have been developed to support the methodology of post authorization safety studies. The understanding of the various guidelines is key in the design and implementation of safety studies by global marketing holders, according to the most appropriate guidelines that apply. A gap exists in view of the absence of a systematic review of these guidelines from a pharmacoepidemiology standpoint and focused on risk management planning of vaccines.
Objectives: The primary objective was to identify and capture guideline recommendations on the methodology of pharmacoepidemiology studies from international, regional and national guidelines. The secondary objectives were to list the discordance between guidelines, to identify the recommendations not applicable for vaccines and the areas that are not covered by the guidelines.
Methods: A systematic guideline search was performed in Pubmed, scientific publications and websites of selected health authorities and international organizations. The included guidelines focused on methodology of post authorization safety studies as the main subject. Regulatory guidelines without reference to safety studies were excluded, as well as guidelines concerning the collection and reporting of individual case safety reports. The reviewed methodology areas were adapted from the STROBE Statement[1] and organized in 155 criteria, grouped by two main dimensions. For each guideline, the recommendation referring to each criterion was captured and simplified recommendations were produced based on the recommendations from various guidelines.
Results: A total of sixteen guidelines were reviewed resulting in 1111 unique recommendations captured. The recommendations were pooled into 494 simplified recommendations.
Discussion: Some recommendations were not directly applicable to studies involving vaccines, e.g. those addressing dose dependency, duration of exposure or definition of start and end date of treatment. Some particular vaccine-specific aspects were not covered by any guidelines, e.g. the definition of exposure in immunizations series.
Conclusion: The methodology allowed reviewing consistently the selected international, regional and national guidelines and to summarize a large number of useful recommendations on several areas of pharmacoepidemiology study design and implementation. Although some of the guidelines did not focus specifically on vaccine studies, the majority of recommendations is applicable or can be adapted to vaccine studies. The sixteen guidelines were very consistent and no incoherence between them was detected.
PP136. Potential Determinants of Suicidal Ideation and Suicide Attempt in users of Duloxetine
M.Al Shukri
Drug Safety Research Unit, UK
Objectives: To explore the association between selected baseline characteristics as potential risk factors for newly reported cases of suicidal ideation and suicide attempt in users of duloxetine.
Methods: A post-marketing surveillance study was conducted using the observational cohort technique of Prescription-Event-Monitoring (PEM). Patients were identified from dispensed prescriptions issued by primary care physicians September 2004 to April 2005. Demographic, exposure, selected risk factors (history of antidepressant use, indication) and outcome data were collected from questionnaires. Logistic regression (in STATA 10) modelled the impact of important determinants on the probability of the composite outcomes of interest (suicidal ideation and/or attempt from tick box responses) and calculated adjusted ORs (+95% CI). Multiple imputation by chained equations recovered missing values.
Results: The PEM cohort comprised 19485 patients (median age 51 yrs (IQR 40, 63); 76.9% (n= 14989) female; 57.4% (n= 11 176) with psychiatric indication. Where data specified, patients with psychiatric indication had a higher incidence of suicidal ideation than those with urologic and other indications [10.0% (n = 779) vs 0.2% (n = 25) vs 2.2% (n= 10)] and suicide attempt [3.9% (n = 345) vs 0.1% (n = 6) vs 1.1% (n = 5)], respectively. Younger age was a significant determinant of risk of the composite suicidal events; the OR for 60–79 yr age group relative to those aged <20 yrs was 0.4 (0.2, 0.8). Also important was psychiatric indication; the OR for those with urologic relative to psychiatric indications was 0.2 (0.16, 0.3). There was evidence of an interaction between gender and taking past antidepressant [females: OR 3.6 (2.6, 4.9); males: OR 2.3(1.6, 3.3)].
Conclusions: This exploratory analysis nested in a cohort exposed to duloxetine has highlighted some important determinants of risk of the composite suicidal events such as psychiatric indications, prior antidepressant use and younger age that clinicians should consider when prescribing this product. Furthermore there is evidence of further differential between females and males with a history of prior antidepressant use. As for other observational studies, residual confounding is an important limitation-there was no information for the whole cohort on prior history of psychiatric illness or suicidal behaviour.
PP137. Hepatotoxicity Associated with Agomelatine: A Case/Non-Case Study
M. Sáiz,1 T. Falomir,2 C. Treceño,1 I. Salado,1 N. Jimeno, L. Martín Arias,1 V. Velasco 1 and A. Carvajal 1
1 Centro para el Estudio de la Seguridad de los Medicamentos. Universidad de Valladolid, Spain; 2 Centro de Farmacovigilancia de las Islas Baleares, Spain
Background: Agomelatine is an agonist at MT1 and MT2 melatonin receptors and an antagonist at 5HT2c receptors with antidepressant and anxiolytic effects. Several cases of hepatotoxicity associated with agomelatine have been recently reported. Although chemically unrelated, other antidepressants such as nefazodone have been observed to produce hepatic injury.
Objective: To learn the risk of hepatic damage associated with the use of agomelatine.
Method: For the purpose we used a case/noncase approach in the Spanish Pharmacovigilance System database to assess the strength of the association between agomelatine exposure and hepatotoxicity. Cases were defined as reports of any hepatic damage; noncases were defined as reports of all reactions other than hepatotoxicity. Exposure was defined as the mention of agomelatine in a report, either being or not being suspected of causing the reaction. The search extended from the date each antidepressant came onto the market until June 2011. The association between hepatotoxicity and agomelatine was estimated by calculating the reporting odds ratio with a 95% confidence interval. The same ratio was calculated for other antidepressants on the market to compare the risks of hepatotoxicity.
Results: Up to date, 52 reports, in which agomelatine was associated with different adverse reactions, were collected by the Spanish Pharmacovigilance System; seven of these reports (13.5%) related to hepatic damage. The estimated strength of association between hepatotoxicity and agomelatine was 4.42 (95% CI, 1.99, 9.84). For the other antidepressants used as comparators, the same estimates range between 0.24 (95% CI, 0.10, 0.57) for bupropion to 1.69 (95% CI, 1.19, 2.40) for sertraline.
Discussion: In premarketing studies, the potential incidence of clinical significant transaminase elevations (>3 × ULN) was higher with agomelatine than with placebo; although the difference did not reach statistical significance, there was a trend of increased incidence of transaminase elevations by increasing agomelatine dose, which supports a causal role. We have found a higher risk of hepatotoxicity for agomelatine as compared to other new antidepressants. It is theoretically possible such spontaneous reporting accounts for some differences between drugs if adverse drug reactions are reported in different ways; also the various antidepressants might be used by different types of patients or different durations. Since there has been no interaction between the pharmacovigilance centers and doctors in this regard and there is no reason to explain a preferential use of any kind of antide-pressant in patients prone to develop hepatic damage or for different durations, we think these biases do not influence in our present results.
PP138. The Safety of Amlodipine and Valsartan Single Pill Combination in Hypertensive Patients
P. Kizilirmak,1 M. Berktas 1 and B. Boyaci 2
1 Novartis Pharma, Istanbul, Turkey; 2 Department of Cardiology, Gazi University Faculty of Medicine, Ankara, Turkey
Objectives: A prospective, post-marketing, non-interventional study was conducted at 166 centres in Turkey.[1] The purpose was to evaluate the efficacy, safety and tolerability of amlodipine (aml) and valsartan (val) single pill combination (SPC) in hypertensive patients.
Methods: A total of 1184 patients (62.2% female; mean±SD age: 58–11 years and 26% of patients ≥65 years) were included. Of the patients; 1024 (87%), 862 (73%) and 659 (56%) have attended to the 1st, 2nd and 3rd follow-up visits conducted in median 30 ±5, 90± 11 and 178±17 days after baseline, respectively.
Results: Aml/val SPC reduced msSBP/DBP to 131.3±0.5/80.5±0.3 at last visit from 166.5 ± 0.6/98.1 ± 0.4 at the baseline (p < 0.0001) and the control rate (≤140/90 mmHg) was 87% in entire group. During the course of the study, 150 (13%) patients experienced 174 AEs; 113 [11%], 10 [1%] and 7 [1%] of whom experienced 1, 2 and 3 AEs, respectively. Oedema was the most frequently reported AE in the entire group (83% of AEs), which was followed by headache (3%), dizziness (2%), pain (2%), flushing (1%) and hypotension (1%). More than three fourths of AEs (85% of AEs) continued until the last visit of each patient, whereas 25 (16%) AEs resolved within a median of 9 ± 38 (1–124) days. Most of AEs (72% of AEs) were mild, however 20% and 6% of them reported to be moderate and severe, respectively. Although most of AEs were reported to be related (77%) with aml/val SPC, no precaution was taken in more than half of AEs (58%). The dosage of aml/val SPC had to be changed or it was discontinued in 26% of AEs, whereas additional therapies were needed in 13% of AEs and 1 patient was hospitalized because of AE. During the study, 3 patients have experienced serious AE which have recovered completely and 2 patients died apart from other AEs. The only serious AE which was suspected to be related to aml/val SPC was hypotension. Eighty one patients (7% of patients) had oedema at baseline; 79 (7%) have experienced new-onset oedema at the follow-up visits (4%, 2% and 1% at visit 2, 3 and 4 respectively). The severity of oedema was reported mostly as mild (74% of oedema), whereas as moderate for 23% and as severe for 3% of oedema.
Conclusions: Aml/Val SPC was an efficient, safe and well-tolerated treatment option for hypertensive patients. The most frequently reported AE was oedema which was mostly mild in severity.
PP139. Effect of Long-Term Use of Proton Pump Inhibitor on Atrophic Gastritis and Gastric Cancer: A 5-Year Longitudinal Cohort Study in South Korea
K. Hong,1 S. Kim,2 S. Kang 2 and J. Kim 2
1 Drug Safety Monitoring Center, Seoul National University Hospital, Seoul, Korea; 2 Department of Internal Medicine, Seoul National University College of Medicine, Seoul, Korea
Objectives: Proton pump inhibitors (PPIs) are broadly used in acid-related disorders and study for an association between PPIs therapy and gastric cancer (GC) are limited. We evaluated the effect of long term therapy of PPIs on atrophic gastritis (AG) and GC.
Methods: We identified all adult patients took a prescription of PPIs among those who visited the Seoul National University Hospital from January 1, 2005 to December 31, 2009. We reviewed total 23 385 patients who were exposed to PPIs and performed gastroduodenoscopy. The patients were divided into three groups according to the treatment duration (group 1: <3 months; group 2: 3–12 months; group 3: >12 months) and followed from the time to take the first prescription of PPIs until the last visit. The development of GC was defined as diagnosis after more than 1 year from the first PPIs prescription day. Relative risks (RR) were calculated using Cox proportional hazards models.
Results: Total 445 patients diagnosed as AG and 100 patients as GC during average 18 563 and 19 171 person-years of follow-up, respectively. Longer duration of PPIs therapy was associated with increased risk of AG(RR: 1.29; 95% CI: 1.04, 1.59 in group 2, RR: 1.39; 95% CI: 1.01, 1.92 in group 3, p = 0.02), after adjusted for age, gender, helico-bacter infection, and co-morbidities. GC development showed increased tendency in longer duration of PPI groups but it was not statistically significant.
Conclusions: The long term use of PPI is associated with the development of atrophic gastritis. However, it was not associated with the development of gastric cancer.
Post-Authorisation Efficacy Studies (PAES)
PP140. Efficacy and Safety of Valsartan and Amlodipine Single Pill Combination in Hypertensive Patients: The Compliance Results
P. Kizilirmak,1 M. Berktas 1 and B. Boyaci 2
1 Novartis Pharma, Istanbul, Turkey; 2 Department of Cardiology, Gazi University Faculty of Medicine, Ankara, Turkey
Objectives: The prospective, post-marketing, non-interventional study was conducted at 166 centres in Turkey.[1] The purpose was to evaluate the efficacy, safety and tolerability of amlodipine (aml) and valsartan (val) single pill combination (SPC) in hypertensive patients. This sub-analysis aimed to evaluate compliance results.
Methods: The compliance rate (CR) was calculated by taking the amount of drug ingested divided by the amount the patient should have ingested and multiply by 100. The patients were classified in CR >80% group (HCR) and CR ≤80% group (LCR).
A total of 1184 patients (62.2% female; mean age: 58±11 years and 26% of patients ≥65 years) under val-aml SPC therapy were included in study. Of the patients; 1024 (87%), 862 (73%) and 659 (56%) have attended to the 1st, 2nd and 3rd follow-up visits conducted in median 30±5, 90±11 and 178±17 days after baseline, respectively.
Results: The mean CR was 96.9 ±0.2% and 94% of patients were in HCR. At visit 2, 3 and 4; the mean CR was 97.1 ±0.2%, 97.9 ±0.3% and 97.0 ±0.2%, and 94%, 93% and 92% of patients were in HCR, respectively. The mean CR reduced slightly as the time to relevant visit rose (rho = −0.36, p<0.0001).
In LCR msSBP/DBP (mmHg) reduced to 134.9±2.5/83.4± 1.4 at last visits from 165.8±4.1/98.6±2.5 at baseline; whereas in HCR, those reduced 131.2±0.5/80.4±0.3 from 164.7±0.8/97.9±0.5 (p<0.0001 for each group). The reduction in msSBP/DBP in HCR was slightly higher than LCR (4.3 ± 2.3/3.1 ± 1.3, p = 0.064 for SBP, p = 0.018 for DBP).
BP control rate (≤140/90 mmHg) was higher in HCR (88%, 74% respectively, p = 0.034). Similarly responder rate (defined as DBP <90 mmHg or ≥10 mmHg reduction in DBP compared to baseline) was also higher in HCR (96%, 84% respectively, p = 0.031).
Adverse event incidence in LCR was more than twice as high as HCR (28%, 13% respectively, p = 0.002). This difference was basically driven by higher oedema incidence in LCR (24%, 12% respectively, p = 0.005).
Conclusions: In summary, the compliance to val/aml SPC therapy is so high and val/aml SPC reduces msSBP/DBP efficaciously in both patient with high CR and patient with relatively low one. Vast majority of patients in both CR sub-groups can achieve blood pressure targets. Adverse events, especially oedema, are more common in patients with relatively low CR, which may be the reason of low compliance.
In conclusion, val/aml SPc seems to be an efficient and safe treatment for hypertensive patients, even in those with low CR.
ADRs in ‘Off-Label Use’
PP141. Reported Case of Tissue Necrosis in a Patient Who Received Intramuscular Diclofenac Injection
M.M. Younus, J.M. Kurmanji and M.F. Abdulqader
Iraqi Pharmacovigilance Center, Iraqi Ministry of Health, Baghdad, Iraq
Intramuscular Diclofenac injection is a widely used pain killer in Iraq. Most common side effects of this medication are related to gastrointestinal disorders, cardiovascular disorders and pain at the site of injection. In this case we reported one of a very rare adverse effect of this medication that causes a permanent disability which is Nicolau Syndrome at the site of injection. 45 years male underwent hemorrhoid surgery; he received Diclofenac IM injection as a postoperative pain killer, after 10 minute of the fifth dose the patient suffered from severe pain and skin erythema, followed by tissue necrosis at area about 10 × 6cm around the site of injection. The patient undergoes debridement surgery (skin graft) to recover the necrosed area. This complication might be due to two main hypothesis; either the damage of artery ending by inappropriate needle length and/or inappropriate injection site; or the toxic effect of the drug that cause vasoconstriction as a cyclo-oxygenase inhibitor. In conclusion it is better to use Diclofenac in other dosage form like suppository which obtains the equivalent effect of injection with less adverse effect in addition to that the injection’s supplier should be a well trained person to avoid any errors might lead to complications.
PP142. Rapid Bilateral Deafness Onset Associated with Concomitant Administration of Gentamicin and Kanamycin in an Adult: Case Report
B.Y. Salumu, P.N. Ntamabyaliro, Y.N. Lula, G.K. Mesia and G.L Tona
Unité de Pharmacologie Clinique et Pharmacovigilance, Université de Kinshasa; Centre National de Pharmacovigilance
Disorders of the ear rarely shorten life but many of them impair its quality thus having devastating effects on communication. Aminoglycosides are known to be the main responsible drugs involved in irreversible ototoxicity. They all have variable cochleotoxicity and vestibulotoxicity. Gentamicin ototoxicity is primarily characterized by vestibular damage (dizziness, ataxia, disequilibrium and/or oscillopsia) appearing with an exposure of 2 weeks or longer whereas kanamycin ototoxicity is of a more serious concern as it is primarily marked by cochlear (or auditory) damage (hearing loss) occurring at a frequency higher than 40% if 1 g is used for more than 30 days.[1–3]
We report here the case of bilateral deafness associated with the coadministration of gentamicin and kanamycin.
A 39 year-old man has received 80 mg of gentamicin twice-daily and an unspecified dose of thrice-daily kanamycin as post-surgical anti-infectious prophylaxis for 8 days by intramuscular route. At day-7, the patient develops left hearing loss. Both drugs are immediately stopped the next day. Three days after the withdrawal of treatment, hearing loss came up on the other ear thus involving a bilateral deafness concern. Unfortunately we did not have much information concerning the long term course of this case deafness.
Simultaneous administration of aminoglysides in therapeutic use is contra-indicated due to cumulating toxicity and literature warns against successive utilization in this class of antimicrobial agents.[4] Notwithstanding the fact the use of kanamycin has declined markedly because of its limited spectrum activity compared with other aminoglycosides, it is also the most noxious.[5] Association of 2 aminoglycosides in therapeutic use was not found in the literature and according Vigibase this case might be the first submitted to Uppsala. The rationale behind this combination is not justified in the literature. Health care professionals should be aware against the risk that gentamicin associated with kanamycin could possibly precipitate the onset of the hearing impairment. Unfortunately, many of them prescribe these antibiotics without careful consideration to what is best for the patient. Additionally, periodic testing of serum aminoglycosides levels and basic renal function tests are most of the time, if ever, absents. In the other hand, although exposure to aminoglycosides is important, hearing loss not absolutely appear in all cases. Environmental and/or genetic risk factors could also play a great role. For the appearance of this effect, a study demonstrated that 17–33% of patients with aminoglycoside ototoxicity bear a predisposing mutation in the mitochondrial RNA.[1]
PP143. Adverse Drug Reactions in Relation with ‘Off-Label’ Use of Aloe Vera Pulp
S. Skalli, R. Benkirane and R. Soulaymani Bencheikh
Moroccan Poison Control and Pharmacovigilance Center, Pharmacovigilance Department, Morocco
An increasing number of people in the world are using herbs for health promotion and specific symptom management. Unfortunately some of these herbs are used wrongly as herbal medicines. They are often off label use and can therefore lead to dangerous side effects. Such is the case with Aloe (Aloe vera) pulp.
Aloe is a tropical cactus belonging to the Lily family. Phytomedicine describes aloe as a herb which has anti-inflammatory and anti-proliferative effects. In recent months aloe pulp which is obtained from the pulpy plant leaves, is used not properly for therapeutic purposes against the problems of the fibroid by Moroccan women. This usage seems to be reported in many other countries. Following this use and during 2011 the Moroccan Pharmacovigilance
Center has recorded 12 cases of side effects mainly type amenorrhea and early menopause that might be in relation with the taking of the pulp of Aloe vera pulp. These cases will be presented and discussed for warning with respect to this off label use.
PP144. Use of Off-Label and Unlicensed Drugs in Paediatrics: Review
J.J. Joaquim, C.I. Fonseca, C.F. Romão and T.S. Pires
Department of Pharmacy, College of Health Technology, Polytechnic Institute of Coimbra, Portugal
A great amount of medicines used in children is prescribed off-label or unlicensed.[1] Children have often been denied the access to new and/or innovative drugs, whether because the drugs have not been duly tested and/or formulated, or because they have not been given the authorization of use in suitable paediatric ages. The lack of reliable data on the paediatric population is associated with specific problems.
This work aims to be a revision therefore has used articles already published under this scope in order to get a framework of problems related with the use of drugs unlicensed and off-label.[2]
Study literature review of research in databases of reference. Were chosen, selected and included 21 scientific papers published after 2005 that were analysed by identifying the medicines and the pharma-cotherapeutic groups most commonly used as off-label/unlicensed and the adverse events verified.
The group of drugs most commonly used in Paediatrics with off-label/unlicensed prescription are Paracetamol; Morphine; Risperidone; Modafinil and Divalproate. The pharmacotherapeutic classes with more relevance have been the NSAIDs; antidepressants; antibiotics and vaccines. Only one article referenced severity of adverse reactions caused by drugs, so it is difficult to realize, through their studies if they were able to identify the gravity associated with the reactions described and reported.
We infer the existence of high level of prescriptions off-label or unlicensed in a hospital environment in relation to the ambulatory patients. It is assumed so that the risk arising from the use of drugs in off-label/unlicensed is controlled and monitored by the majority of patients being in hospital, and ambulatory patients are less exposed to these prescription systems. The drugs prescribed belong to various pharmacotherapeutic classes.[3] To sum up, has verified that the off-label/unlicensed ractice in Paediatrics is rooted in many countries and has become a very common practice in Paediatrics.[4–6]
It was difficult to identify the problems related with the use of drugs in both situations, because most of the articles does not mention the reactions caused or when it identifies do not relate to the drug. Given the methodological differences used in various studies is difficult to compare them. To get a better sense of real use in off-label/unlicensed, as of which the most prescribed drugs in children, it should would make further study with similar methodology.
It is important better research in this topic to identify the problems that could really happen in order to deal with them.
PP145. Misuse of Proparacaine Hydrochloride
D.N. Aydinkarahaliloglu,1 V. Dayan_r,2 G. Saği§,1 Y. Kasap, E. Aykaç,1 C. Babacanoğlu,1 H. İlbars,1 H. Özbek 1 and S. Kerman 1
1 General Directorate of Pharmaceuticals and Pharmacy, Ministry of Health, Ankara, Turkey; 2 Department of Ophthalmology, Adnan Menderes University, Faculty of Medicine, Department of Ophthalmology, Aydın, Turkey
Background: The reports submitted to our Ministry on misuse of eye drops containing proparacaine which is a topical anesthetic, have been reviewed and the necessary actions were taken.
Objective/aim: The aim was to assess the reports from hospitals from three different cities in Turkey regarding the uncontrolled and off-label use of eye drops containing proparacaine hydrochloride leading to the development of permanent impairment in cornea and underscore the relevant precautions taken.
Method: Ophthalmologists from Konya and Sakarya have reported misuse of proparacaine. Details of the cases were not indicated in these reports. In the third report from Aydın, the three cases were described in detail. Various actions were taken based on these reports. Results: Initially, a report from an ophthalmologist in Konya was submitted to our Ministry, stating the occurrence of permanent impairment in cornea due to uncontrolled and off-label use of the eye drops containing proparacaine. The report suggested that these pathologies may progress to further levels, impair vision and may even cause keratoplasty operations. Therefore, our Ministry decided to inform ophthalmologists and independent pharmacists regarding the subject via a “Dear Healthcare Professional Letter”. In the letter it was emphasized that proparacaine ophthalmic solution should only be used under doctor’s supervision and surveillance, should be prescribed for use of the individual patient only and should in no way be sold without prescription. However, following the distribution of this letter a report was submitted by an ophthalmologist in Sakarya, stating that misuse of proparacaine was observed very frequently, and that patients disregarded their main therapy considering they receive adequate treatment due to its temporary relief and that it leads to further progression of the pathology. Finally, another report including three cases was received from Aydın. Two of these cases belonged to welders.
Conclusion: As a result of the review on reports submitted to our Ministry, it was concluded that proparacaine ophthalmic solution should only be prescribed by ophthalmologists, the pharmacy selling the product should keep a copy of the stamped prescription for a period of one year and that maximum four products per month in the form of prescription can be sold providing that the doctor is an ophthalmologist with documented submit.
Discussion: Although the current measures are deemed adequate at this point, the subject will be closely monitored.
Perception of Risks and Communication
PP146. Knowledge and Attitude of Doctors to Adverse Drug Reactions Reporting and Need of Pharmacovigilance Training in Kolhapur, Maharashtra, India
M.A. Burande,1 A.R. Burande,2 S. Sahni 3 and S. Lohan 4
1 Department of Pharmacology, D Y Patil Medical College, D Y Patil University, Kolhapur, Maharashtra, India; 2 Department of Anatomy, D Y Patil Medical College, D Y Patil University, Kolhapur, Maharashtra, India; 3 Intern, D Y Patil Medical College, D Y Patil University, Kolhapur, Maharashtra, India; 4 MBBS student, D Y Patil Medical College, D Y Patil University, Kolhapur, Maharashtra, India
Objectives:
-
1.
Investigating the knowledge, attitude and behavior of doctors to adverse drug reactions reporting
-
2.
To find the need and willingness of Pharmacovigilance training
Methods: Questionnaire based cross sectional study including 210 randomly selected MBBS Doctors in clinical practice after getting approval from IEC and informed consent at D Y Patil Medical College and Hospital, Kolhapur, India.
Results:
Demographics: Response rate 68.09%, Mean age - 31.31 years, 118 male: 25 female, mean years of practice -10.89 years, 38.46% had additional qualification and 99.30% had their MBBS from India.
Knowledge to ADRs and reporting: 96.50% felt as Doctors are eligible to Report ADR. Only 28.67% were aware of National Pharmacovigilance Centre in INDIA, 8.39% correctly identified NEW DELHI as the office, 4.89% were aware of ADR REPORTING FORM and only 3 had ever reported ADRs. The purposes of ADR reporting scheme were correctly identified by only 39.86% respondents. ADR Reporting should be done for all reactions for OTC drugs were identified by maximum (83.91%) doctors.
Attitudes: Maximum doctors 52.44% felt one report made no difference and 49.65% doctors said that ADR reporting should be voluntary. Influencing Factors: Serious reaction (85.32%) was the most encouraging factor while Concern that the report may be wrong (46.85%) was the most discouraging factor to report ADR.
Education and Training: NONE had received training on ADRs or Pharmacovigilance and 99.30% been willing to undergo for training. The various methods were suggested by the respondents’ i.e. Active participation of pharmacology department, Easy availability of forms and training at MBBS level, Clinical meetings, Routine bulletin, Seminars and lectures on topic, short, simple and objective ADR FORM etc to improve the ADR reporting.
Conclusion and discussion: This study has shown that knowledge of doctors about ADRs and reporting is significantly inadequate (p < 0.05%) in India as compare to other countries.[1]
Ignorance, diffidence and indifference had significantly influenced while self-satisfaction, fear, financial incentives and bureaucracy had a little influence on the respondents to report ADRs.[2]
It is associated more with knowledge gaps and attitudes of the doctors rather than with personal and professional characteristics.[3,4]
These gaps need to be filled by improved training in pharmacovigilance and risk perceptions of drugs by continuous medical education, reminders and awareness on the ADR reporting scheme. Attitudinal and cultural changes including ADR reporting as an integral part of the clinical activities are must for long term improvement.[5,6]
PP147. Evaluation of General Practitioners and Community Pharmacists’ Perception Towards Consumer Reporting of Adverse Drug Reactions (ADRs) in Penang Island
M.A. Alshakka,1 M.M. Ibrahim 2 and M.A. Hassali
1 Discipline of Social and Administrative Pharmacy, USM, Malaysia; 2 Pharmacy Practice Department, QASSIM University, Saudi Arabia The study evaluates perception of general practitioners (GPs) and community pharmacies (CPs) in Penang, Malaysia towards consumer reporting of ADRs.
Methodology: A cross sectional mail survey was adopted for the conduct of the study. The survey was sent to a total of 192 CPs and 400 GPs in state of Penang, Malaysia. A follow-up reminder was sent to all non-respondents after 3 weeks of the initial mailing. Date collected from the questionnaire was analyzed using SPSS v 15. Chi-square test was used to determine association between expected and observed frequencies at alpha level of 0.05.
Results: A total of 105 respondents (47CPs and 58 GPs) were received with response rate of 18%. The results indicated that GPS and CP are aware about the importance and benefits of consumer reporting of ADRs. Majority of them (88%) think that consumer reporting will add more benefits to the existing pharmacovigilance program. It is found that 97% of the respondents agreed that ADRs reporting is necessary and 87% of respondents observed ADRs among their patients. However more than half of them were not aware of national program in Malaysia that allows consumer to report ADR. Majority of them (97%) agreed that the consumer need more education regarding reporting of ADRs. Most of them (84%) think that consumer cannot write valid reports similar to health care professionals (HCP) reports. Majority of the respondents (68% ) had not heard about consumer reporting program in Malaysia and half of them did not believed that consumer reporting can overcome under reporting, the main problem of the national pharmacovigilance program In Malaysia. The most of the respondents (64%) were pessimistic about the success of consumer reporting in Malaysia. Most GPs and CPs had the opinion that media and NGOs can play important role in the success of consumer reporting of ADR.
Conclusion: The GPs and CPs are aware about the importance and benefits of consumer reporting. Such reporting will add more benefits to the existing programmes in Malaysia, although the barrier that we are facing now is the fact that they doubt if the patients can write valid reports similar to HCP reports. Therefore, the consumers need more education about their medications. Mass media and NGOs must play their important role on determining the success of consumer reporting.
PP148. Evaluation of General Public Perception Towards Adverse Drug Reaction Reporting
M.A. Alshakka,1 M.M. Ibrahim 2 and M.A. Hassali
1 Discipline of Social and Administrative Pharmacy, USM, Malaysia; 2 Pharmacy Practice Department, QASSIM University, Saudi Arabia
Objectives: The study aims to explore the perception of Penang’s state general public towards the Adverse Drug Reactions (ADR) reporting.
Methodology: This research study was conducted using a cross-sectional study design. We used self-develop validated questionnaire as our data-gathering tool. A total of 500 questionnaires were distributed to the general public in the State of Penang, Malaysia. The questionnaire contains questions related to the awareness, understanding and perception towards ADR-reporting. The data was analyzed using the chi square test by the PSW software version 18.0.1.
Results: Out of 500 respondents, 230 (46%) respondents are male and 270 (54%) are female. A large number of our respondents are Malay (44.6%) followed by Chinese (36.8%), Indian (15.2%) and other races (3.4%). Based from the data collected, the majority of the respondents (40.6%) are university graduates. Majority of the respondents were not aware about the definition of ADRs (38.2%). Besides that, most of the respondents (52.6%) were unable to differentiate between the ADRs and side effects. Despite this, it is thought to be interesting that most of them were able to relate ADRs with the real-life situations based on their experiences (54.2%). Most of them had asked about the ADRs that they might get (61.8%) and only 48.2% claimed that physicians and pharmacists have asked them to make ADRs reports. Next, the majority of the respondents also agreed that: Everyone, irrespective of the age is susceptible to ADRs (60.8%); it is vital to collect information regarding ADRs (96.4%); the main purpose of reporting ADRs is to prevent the occurrence of the same ADRs in other individuals; the doctor who prescribed the medication needs to be informed regarding ADRs (53.8%) as they are the main source of information regarding ADR; Malaysia Adverse drug reaction advisory committee (MADRAC) is the responsible body that evaluates the ADRs reporting in Malaysia (46.8%); they have never heard of the term pharmacovigilance (94.6%); they will not make reports if the ADRs are mild (58.4%); the problem of ADRs in Malaysia is somewhat serious (46%);
Conclusion: Based on our study, we can conclude that the public in Penang is not aware about the importance of ADR-reporting and that this kind of reporting is taken lightly. However, most of the respondents agreed that the ADRs reporting gives positive impacts to the public.
PP149. Risk of Suicidality Events in Patients Taking Atomoxetine: Results of a Matched Cohort Analysis
M. Davies, D. Layton, E. Tong and S. Shakir
Drug Safety Research Unit (DSRU), Southampton, UK; University of Portsmouth, Portsmouth, UK
Objectives: Atomoxetine (Strattera™) was launched in the UK in June 04 for the treatment of Attention Deficit Hyperactivity Disorder (ADHD).[1] In Sep 05 a boxed warning was included on the US labelling[2] and additional warning statements that alerted health care providers to the increased risk of suicidal thinking in children/adolescents being treated with this drug. A meta-analysis of suicide-related behaviour events in patients treated with atomoxetine conducted by Lilly (published 2008), concluded that although uncommon, suicidal ideation was significantly more frequent in paediatric ADHD patients treated with atomoxetine compared to those treated with placebo.[3] An objective of this study was to examine the risk of suicidal events during treatment with atomoxetine compared to prior to starting treatment.
Methods: A post-marketing surveillance study conducted using the observational cohort technique of Modified-Prescription Event Monitoring (M-PEM); Patients were identified from prescriptions issued by primary care physicians between Dec 04 and Sep 09. Data-collection forms sought information on psychiatric events during and prior to starting treatment. A matched cohort analysis compared the risk of these events occurring in the during treatment period relative to the prior to starting treatment period. The matching by patient implied each patient acted as its own control. Conditional Poisson regression was used to estimate the risk ratios and 95% CIs. The events in this analysis included all reported events regardless of causality and aetiology.
Results: The cohort comprised 4711 patients; median age 12 years and 85.0% male. The four psychiatric events included in the matched analysis were suicidal ideation (SI), suicide attempt (SA), overdose (OD) and deliberate self harm (DSH). Risk ratios for these events were: [SI = 0.65, (CI: 0.45, 0.94), SA = 0.70 (CI: 0.35, 1.39), OD = 0.44 (CI: 0.23, 0.82), DSH = 0.52 (CI: 0.37, 0.73)], p-values <0.05, except for the event of SA, p-value=0.306.
Conclusions: The results suggest that the risk of developing these psychiatric events during treatment with atomoxetine is lower than prior to starting. This may reflect a successful communication of potential risk of suicidal-related events to primary care physicians; patients exhibiting worsening psychiatric symptoms may have a prompt cessation of treatment. Residual confounding is possible since the effective sample size is reduced because the analyses are based on only discordant pairs. This data should be considered with other pharmaco-epidemiological data available on this topic.
PP150. Experiences and Preferences of Healthcare Professionals with Regard to Direct Healthcare Professional Communications
S. Piening,1 F.M. Haaijer Ruskamp,1 P.A. De Graeff,2 S.M. Straus 3 and P.G. Mol 2
1 Department of Clinical Pharmacology, University Medical Center Groningen, Groningen, The Netherlands; 2 Department of Clinical Pharmacology, University Medical Center Groningen, Groningen, The Netherlands; Dutch Medicines Evaluation Board, The Hague, The Netherlands; 3 Dutch Medicines Evaluation Board, The Hague, The Netherlands; Department of Medical Informatics, Erasmus Medical Center, Rotterdam, The Netherlands
Background: Effectiveness of Direct Healthcare Professional Communications (DHPCs) or ‘Dear Doctor’ letters, to inform healthcare professionals of drug safety issues is questioned. Communication of newly identified serious drug safety issues and possible tools to prevent them from occurring in subsequent patients may be improved when more is known about healthcare professionals preferences.
Objectives: The objective of this study was to explore healthcare professionals experiences and preferences for improvement of drug risk communication, in particular the DHPC, comparing the views of general practitioners, internists, community pharmacists and hospital pharmacists.
Methods: An anonymous, pilot-tested mail questionnaire was sent to a representative sample of Dutch healthcare professionals (n = 3488) (Dec ‘09–Jan ’10). Multiple choice and open questions were posed on perception of drug safety and DHPCs, familiarity with and action taken following DHPCs, satisfaction with DHPCs and preferences for alternative communication methods. Descriptive statistics (chi-squares and ANOVA) were used to determine differences between healthcare professional groups.
Results: Thirty four percent (1164) of the healthcare professionals responded (ranging from 24% of internists to 46% of community pharmacists). Most respondents considered drug safety information to be important for their profession (mean 4.67; SD 0.56, on a scale of 1–5; p ≤ 0.001). Sixteen percent (ranging from 5% of hospital pharmacists to 28% of general practitioners) had never seen or heard of DHPCs (p≤ 0.001). Respondents indicated they undertook action following 29% of received DHPCs, ranging from 23% by internists to 37% by public pharmacists (p≤ 0.001). Overall, respondents rated their satisfaction with DHPCs on average with a 6.9 (SD 1.86, on a scale of 1 to 10; p ≤ 0.001). Respondents preferred e-mail (7.6; SD 2.3, on a scale of 1 to 10), medical journals (7.5 SD 2.0) and electronic prescribing systems (7.1; SD 2.7) as alternative information channels, preferably issued by the Dutch regulatory authority (8.1; SD 1.5), the Dutch Pharmacovigilance Center (Lareb) (8.1; SD 1,7), or own professional bodies (8.0; SD 1.7).
Conclusions: Although safety information of drugs is considered important, healthcare professionals reported to undertake action in a minority of DHPCs issued. Pharmacists seem to be more involved with and responsive to safety issues than physicians. Satisfaction was comparable. Alternatives should be developed using electronic methods and medical journals.
PP151. Implanon and Reports of Unintended Pregnancy: Media Interest in UK
D. Mahoney, J. Woolley and M. Jadeja
Vigilance and Risk Management of Medicines, Medicines and Healthcare products Regulatory Agency (MHRA), London, UK
Background: In early 2011 media interest in the UK focused on reports of unintended pregnancy with Implanon (subdermal etonogestrel implant), particularly those associated with insertion and/or removal difficulties. The UK has the highest usage of Implanon worldwide and a comprehensive training scheme is available to those who intend to insert it.
Objectives: To evaluate spontaneous reporting data for reports of unintended pregnancy with Implanon; to identify the suspected reasons for contraceptive failure; and to compare the UK reporting rate for unintended pregnancy with Implanon with that for Europe.
Methods: The MHRA Yellow Card Scheme database was interrogated for spontaneous reports of unintended pregnancy with Implanon. Reporting rates were estimated from usage data provided by the company (to 1 September 2010).
Results: Since Implanon was launched until September 2010, an estimated 1 335 584 units have been sold in the UK. During this time the MHRA received 543 reports of pregnancy, corresponding to a reporting rate of 0.040 per 100 implants sold.
The company estimates a UK reporting rate of 0.058 (per 100 implants sold), based on 792 medically confirmed reports; this compares with a rate of 0.062 per 100 implants sold for the whole of Europe. A number of possible reasons for the unintended pregnancies in the UK have been reported. In an estimated 13% of pregnancies no implant had been inserted; this compares with a Europe-wide rate of 26%.
Since this issue was publicised in the UK, the MHRA has received a further 97 reports of unintended pregnancy of which 3 (including 2 reports from patients) describe an insertion-related problem (as of 24 May 2011).
Conclusions: The reporting rate for all unintended pregnancies associated with Implanon is low. Though substantial under-reporting is likely, these data do not call into question the efficacy of Implanon when used appropriately.
In an estimated 13% of all UK reports of pregnancy no implant had been inserted, however, the proportion is lower than that for Europe as a whole. It is possible that the training programmes in place in the UK may have been effective in reducing insertion errors.
A new version of Implanon, known as Nexplanon, which is radio-opaque and has a new insertion method, was launched in the UK in late 2010 to further minimise any insertion/removal problems. Reports of unintended pregnancy will continue to be closely monitored. MHRA continues to highlight the importance of appropriate training before inserting or removing contraceptive implants.
PP152. Evaluating the Effectiveness of Health Product Risk Communications: Health Canada’s Strategic Approach
D. Jurgens, V. Hogan, G. Condran, L. Adewoye and S. Reid
Health Canada, Marketed Health Products Directorate, Ottawa, ON, Canada
Background: Most federal health product regulators struggle with defining appropriate measures of the effectiveness of health product risk communications given the complexity of confounding variables that could influence the ultimate outcome. While some work has been done by Health Canada, there has not been an overarching strategy for evaluating the effectiveness of risk communications across product lines, including pharmaceuticals, biological/biotechnology products, medical devices, and natural health products.
Objective: Health Canada is developing a strategy to outline a path forward for the systematic evaluation of the effectiveness of health product risk communications. This requires an in-depth look into issues such as:
-
• Are the risk communications reaching their intended target population?
-
• Do the risk communications bring about the action intended?
-
• Do the risk communications benefit the intended user?
Challenges:
-
1.
Many organizations and individuals play a role in communicating risks associated with health products, including manufacturers, regulators, healthcare professionals and the public;
-
2.
The relationship between awareness of risk information and actual change in behaviour is complex;
-
3.
Inadequacy/usefulness of existing sources of performance indicator data;
-
4.
The practice of medicine being a provincial/territorial responsibility in Canada, it is difficult for Health Canada to monitor whether there is a change in health professionals’ behaviour following issuance of a risk communication;
-
5.
The generation of new evidence needed to evaluate effectiveness is both time consuming and costly.
Methods: The initial focus will be on a subset of risk communications, with the intention to extend the initiative in the future. The short-term strategy includes development of a Performance Measurement and Evaluation Plan to define indicators and endpoints for measuring effectiveness and studying the effect of Dear Healthcare Professional Letters on physician prescribing practices in Canada using interrupted time series analysis. Longer-term plans include research focused on knowledge translation behavioural change, health literacy and evaluating the awareness, use and satisfaction of the public with the tools and risk information communicated.
Strategic Approach: Risk communications must be effective in order to achieve their intended outcome — to minimize risks associated with health products. The multiple factors that influence the uptake of new information make this outcome challenging to measure. Innovative methods that inform on the reach, use and benefit of health product risk communications need to be developed in order to advance the knowledge in this area. This will require a collaborative effort on the part of regulators, industry and academia.
PP153. An Investigation on the Perception of the Risk on the Use of Medicinal Plants Commonly Used and Sold by Herbalists in Tuscany
E. Gallo, E. Lucenteforte, S. Harrison, M. Di Pirro, M. Moschini, L Gori, V. Mascherini, F. Firenzuoli, A. Mugelli and A. Vannacci
University of Florence, Department of Pharmacology, CIMMBA, Centre for Integrative Medicine, Florence, Italy
Background: The herbalist represents a professional figure that is responsible for educating and making sure that the patient uses correctly medicinal plants. The objective of the present study was to evaluate the perception of the risk from the herbalists on the use of plants generally used and sold in the herbalist’s shops.
Method: The investigation was conducted “de visu” by means of a questionnaire. For each studied product/plant (Allium, Aloe gel, citrus aurantium, Cimicifuga, Escolzia., antraquinones laxatives, propolis, echinacea, Harpagophytum and Ginseng) and for some specific clinical effects. The herbalist was asked to indicate the exact proportion of risk across a simple Visual Analogic Scale. A group formed by 10 experts in this area was used as a control group.
Results: In this study 159 in 185 herbalists assisted in the inquiry. The herbalists considered plants and natural products more secure in respect to experts, in exception to plants containing antraquinones. Nevertheless, such differences were not statistically significant. With regard to Garlic, the herbalists showed a perception of the general (middle) risk but much lower in respect to the experts (Median: 2.1 and 4.6, respectively). It also emerged that graduated herbalists and herbalists with exception of 10-year-old of working experience had a perception of risk similar to that of the experts. For Citrus aurantium the herbalists were perfectly in line with the experts, considering the general risk being middle of the plants (4.0 and 5.6, respectively) and recognized that the possibility that such plants could give unfavorable cardiovascular reactions. In this case there were differences between the herbalists with more than 10 years of working experience or less. For Cimicifuga it has emerged that the herbalists, in agreement with the experts, considered this plant generally to be of middle risk (3.5 and 4.1 respectively), but did not know the possible unfavorable effects being derived from its utilization, in fact consider gastritis, allergy and liver damages as low risk.
Finally, half of the herbalists interviewed reported to having had unfavorable reports of adverse reactions from actual customers. Considering that in 8 years only about 500 reports were obtained from the National Phytovigilance System, the discrete number of adverse reactions reported by the herbalist’s in this study demonstrates that a majority of the signals were generally omitted by herbalists.
PP154. Pharmaceutical Sales Representatives and Patient Safety: A Comparative Cross-Sectional Survey of Information Quality in Canada, France and the U.S
B. Mintzes,1 M. Beaulieu,2 M. Wilkes 3 and J. Montastruc 4
1 Pharmacology & Therapeutics, University of British Columbia, Vancouver, BC, Canada; 2 Family Medicine, University of Montreal, Montreal, QC, Canada; 3 Internal Medicine, UC Davis, Sacramento, CA, US; 4 Pharmacology, University of Toulouse, Toulouse, France
Background: The information provided by sales representatives has been shown to influence physicians’ prescribing decisions, an influence that is often underestimated. For accuracy and balance, and to enable safe prescribing, all medicines information must include harm as well as benefit.
Methods: This is the first comparison of safety-related information provided by sales representatives in different regulatory environments. We carried out a comparative cross-sectional study in Vancouver, Montreal, Sacramento and Toulouse. Physicians who regularly see sales representatives were recruited to report on consecutive sales visits. These sites represent three national regulatory environments: France has the strictest standards; the French and US governments directly enforce regulations; and Canada relies primarily on industry self-regulation.
We asked how often ‘minimally adequate information for safe and appropriate use’ was provided. This was defined a priori to include: ≥1 serious adverse event, ≥1 common adverse event, ≥1 contra-indication, ≥1 indication, and no unapproved indications or unqualified safety claims.
Results: ‘Minimally adequate information’ was rarely provided in any of the sites, and no information on harmful effects was provided in two-thirds of promotions in Vancouver, Montreal, and Sacramento. Qualified and unqualified safety claims, health benefits, and insurance status were noted more frequently. In Toulouse, free samples, and ‘drug lunches’ were rarely provided, and harm was mentioned more often, mainly common adverse events.
Conclusions: Some important differences were consistent with stronger information standards in France. However, in all four sites, physicians received inadequate information on serious harmful effects of medicines, raising questions about whether information quality is compromising protection of patients’ health.
ADRs of Antidiabetic Agents
PP155. Identification of Adverse Drug Reactions Associated with Counterfeit Anti-Diabetic Herbal Products
F.A. Al Braik,1 A.S. Elgharbawy 1 and M.Y. Hasan 2
1 Drug Control & Registration Department, Ministry of Health, United Arab Emirates; 2 Faculty of Medicine, UAE University, United Arab Emirates
Background: The incidence of diabetes mellitus is increasing worldwide.[1] UAE is ranked among top countries where high percentages of population are living with disease or its complications.[2] Herbal medicines are widely used in treating diabetes and cultural practices consider herbal products safe and promote self-care without medical consultation. Herbal anti-diabetic products could be counterfeit not meeting quality standards.
Objective: This study assessed quality and safety of anti-diabetic herbal products purchased through unauthorised channels.
Methods: Samples were collected via outlets inspection or referred by patients from 2003 till 2010. Authenticity of herbal products and counterfeit with hypoglycaemic agents was performed in Drug Quality Control Laboratory, UAE. Adverse Drug Reactions (ADRs) were monitored by patients voluntary reporting.
Results: 12/15 (80%) Samples were confirmed to be counterfeit with hypoglycaemic agents. 3 products contained single anti-diabetic ingredient, 4 products contained two ingredients, 3 products were counterfeited with iron plus single ingredient and 2 products had iron along with two ingredients. Our findings showed that 9/12 samples (75%) contained metformin, 8/12 (67%) glibenclamide and 1/12 (8%) gliclazide. It is assumed that Iron was added to block detection of anti-diabetics in the analysis. ADRs were evaluated from 5 patients. 3/5 (60%) were using herbs contained single anti-diabetic (metformin or glibenclamide) and reported gastrointestinal reactions, nausea, vomiting, flatulence, diarrhoea and loss of appetite. 2/5 (40%) who suffered hypoglycaemic attacks and hospitalized were using products with multiple anti-diabetics (glibenclamide and metformin).
Discussion: Natural anti-diabetic products brought by travellers, purchased over internet or entered through illegal suppliers may contain hypoglycaemic agents. Serious events such as hypoglycaemia, therapeutic ineffectiveness could be related to adulteration of herbal products.[3] Similar studies indicated that folk anti-diabetic products could be counterfeit leading to severe hypoglycaemia.[4] Many herbal products labels do not mention standardized ingredients nor indicate information on manufacturers or country of origin.
Conclusion: Adulterations of herbs with conventional medicines is challenging and purchasing unregistered herbs from unapproved sources poses risks to patients. Pharmacovigilance and conducting educational programs would protect consumers and reduce public health risk associated with counterfeit products.
PP156. Hypoglycaemic Episodes Leading to Hospitalisation in Departments of Internal Medicine
P. Thürmann,1 S. Schmiedl,1 M. Rottenkolber,2 J. Szymanski 1 B. Drewelow,3 S . Müller,3 A. Zachow,3 W. Siegmund,4 K. Saljé,4 M. Arnold,4 M. Hippius,5 A. Scheuerlein,5 K. Farker 6 and J. Hasford 2
1 Philipp-Klee Institute of Clinical Pharmacology, HELIOS Clinic Wuppertal, Germany; Department of Medicine, Faculty of Health, University Witten/Herdecke, Germany; 2 Institute for Medical Information Sciences, Biometry, and Epidemiology, Ludwig-Maximilians-Universitaet Muenchen, Munich, Germany; 3 Regional Pharmacovigilance Center Rostock, Institute of Clinical Pharmacology, University of Rostock, Germany; 4 Regional Pharmacovigilance Center Greifswald, Institute of Clinical Pharmacology, University of Greifswald, Germany; 5 Regional Pharmacovigilance Center Jena, Institute of Pharmacology and Toxicology, Department of Clinical Pharmacology, University of Jena, Germany; 6 Regional Pharmacovigilance Center Weimar, Institute of Pharmacology and Toxicology, Department of Clinical Pharmacology, University of Jena, Germany
Objectives: In diabetic patients effective antidiabetic therapy is often associated with a certain risk of hypoglycaemia and there is some recent evidence suggesting an increased overall mortality in patients with very low HbA1c values. Within the German Net of Regional Pharmacovigilance Centers (NRPC) ADR-related hospital admissions were assessed since 1997 in 4 university or academic teaching hospitals with a catchment area of approximately 500 000 inhabitants. We aimed to analyse hypoglycaemia-associated hospitalisations focusing on causes and preventive measures.
Methods: Patients admitted to departments of internal medicine of the 4 NRPC hospitals were comprehensively assessed for presence of ADR leading to hospitalisation. Data concerning the ADR, patient and drug history were collected, standardised causality assessment according to Begaud was performed and preventability was assessed according to a standardized algorithm. Quality assurance was performed and data were reported to the national authority (BfArM). Patients with an at least ‘possible’ ADR (I2) admitted to hospital between 01/2000 and 06/2008 were included in this analysis.
Results: Out of all ADR-patients (n = 6427), 16% (n=1031) were admitted to hospital due to hypoglycaemia caused by at least one anti-diabetic drug. In comparison to the remaining ADR patients, hypoglycaemic patients (HGP) were older (73.6± 13.7 yrs. vs 69.7+ 15.9 yrs., p< 0.0001) and more frequently of female gender (63.0% vs 59.6%, p = 0.0452). Out of all HGP, 27.1% and 60.0% received exclusively oral antidiabetics or insulin, respectively, whereas both drug classes were prescribed to 12.9% of HGP. Hypoglycaemic cases were more frequently assessed as preventable compared to remaining ADRs (25.9% vs 18.3%, respectively, p > 0.0001). For the most frequent single drugs and drug-drug interactions highest preventability rates were revealed for glibenclamide (39.5%) and glibenclamide plus metformin (38.5%). Relevant drug-drug interactions, non-adjustment of anti-diabetic drug dosages and omitted laboratory investigations represented the most frequent causes in preventable hypoglycaemia. Out of all HGP with documented HbA1c (n = 612), HbA1c values <7.0% were achieved in 61% of patients and lower levels were measured in elderly HGP with 6.6±1.2% (>70 yrs.) versus 7.1 ±1.5% (≤70 yrs.; p = 0.0001).
Conclusions: In a large prospective observational study, nearly one sixth of all ADR leading to hospitalisations were caused by hypoglycaemic episodes of which one quarter was preventable. Taking into account our data and recently published results of milestone studies, dose adjustment of antidiabetic drugs according to the individual risk profile and particularly with respect to patients age seems to be the most promising strategy for preventing severe hypoglycaemia (supported by BfArM FoNr: V-1 1337/68605/2011).
PP157. The Diabetic Phytovigilance what does in Morocco?
Y Khabbal. F. Ajdi,2 Y Cherrah,3 K. Amazian 4 and N. Chami 5
1 Department of Pharmacology LABM, CHU Hassan II, Fez, Morocco; 2 Department of Endocrinology, CHU Hassan II, Fez, Morocco; 3 Laboratory of Pharmacology and Toxicology, Faculty of Medicine and Pharmacy, Rabat, Morocco; 4 CHU Hassan II, Fez; 5 Faculty of Science, Dhar el Mahrez, Fez, Morocco
Introduction: Diabetes is an epidemic disease of the millennium; it imposes a heavy economic charge especially among populations of emerging countries and poor. In Morocco or purchasing power remains low, the diabetic patients are generally forced to seek alternatives to drugs, such as herbal medicine.
This work aims to describe the profile of diabetic patients using herbal medicine and to list the adverse effects of these plants.
Materiel and Methods: This is a prospective study over three months (March–May 2011), including all patients with type 2 diabetes, men and women, adults, hospitalized or consultant to the endocrinology department. Children, type 1 diabetes and women with gestational diabetes were excluded.
The demographic, clinical, para clinical and therapeutic data were collected by the farm and then analyzed using SPSS version 17. The results are expressed as numbers, percentages or means ± standard deviation. The group of patients who use medicinal plants, and group who do not use were compared by χ (chi-square).
Result: Our study included 129 diabetic patients, hospitalized or consultant in the Department of Endocrinology of CHU-Fez, the average age of our patient was 56± 10 years, the portion most represented is that of 41±60 years. The female is dominant with 69%. For education, 51% of patients are not secularized, and 85% of them live in urban areas.
The use of herbal medicine was noted in 61% of our population. Among the 79 patients that use plants, 87% use herbal medicine because of its effectiveness, and only 4% to the cost.
Various plants are used by diabetic patients. In our study 37 plants were used (average of 2.7 ±2.15 plants for each patient). The plant is most commonly used fenugreek (Halba), followed by sage (Salmia), olive (Zaytuna), dill (chebt), oregano (zaatar) and wormwood (chiba). The use of plants has resulted in 12.7% of cases of adverse reactions recorded by the patients themselves adverse effects observed in patients using plants differ from one patient to another, but it was the gastrointestinal disorders that are most common.
Conclusion: Serious efforts should focus on awareness of the dangers of using these plants, especially those with a known potential for toxicity. The implementation of a performance system of phytovigilance is mandatory to eradicate if not reduce the danger of the plants.
Paediatric Pharmacovigilance
PP158. Gender Differences in Adverse Drug Reaction (ADR) Reporting in Children in Norway 2001–2010
J. Bergman 1 and J. Schjøtt 2
1 Regional Medicines Information and Pharmacovigilance Centre (RELIS Vest), Haukeland University Hospital, Bergen, Norway; 2 Section of Clinical Pharmacology, Laboratory of Clinical Biochemistry, Haukeland University Hospital, Bergen, Norway; Section of Pharmacology, Institute of Medicine, Faculty of Medicine and Dentistry, University of Bergen, Bergen, Norway
Background: A higher susceptibility in females for ADRs is known in the adult population[1] but less is documented in children. More ADRs have previously been reported for girls in Norway[2] with slightly higher ADR reporting for boys internationally.[3]
Objective: To describe gender differences in spontaneous reports of ADRs in Norwegian children.
Methods: Spontaneous reports from 2001–10, affecting children <18 years were collected from the Norwegian ADR database. Reports on ADRs from drug exposure in utero, through breastfeeding, due to vaccines and reports with an unlikely causality were excluded. ADRs were grouped according to the System Organ Classes (SOCs) in MedDRA 14.0, and suspected drugs according to the ATC classification system 2011.
Results: In the 10-years period there were 19 434 reports in the Norwegian ADR database and 767 (4%) reports met the inclusion criteria. 52% (n = 401) of the included reports involved girls and 47% (n = 363) boys, (n=3 with unknown gender). There were small gender differences in reports of serious or non-serious ADRs, reports from hospitals or primary care, and in reports from physicians, pharmacists or others. Average of SOCs per ADR report was >1.8 and 1.7 for girls and boys, respectively. Share of reports in girls dominated for adolescents (15–17 years), with otherwise equal reporting rates. Gender differences were noted for the decade’s top five suspected drugs, being methylpheni-date, atomoxetine, drospirenone/estrogen, infliximab and isotretinoin (Table I).
Discussion: Gender differences in ADR reporting in this study were mainly found among adolescents and for selected drugs. The reports reflects the prescription pattern in Norway with a higher general rate of drug prescriptions to girls >13 years, higher rate of use of ADHD drugs and isotretinoin in boys, and the use of oral contraceptives in girls.[4] A particular difference was the higher frequency of reported ADRs associated with infliximab in girls, but a higher rate of infusion reactions have previously been associated with females.[5] Spontaneous reports, with underreporting of ADRs, do not reflect true frequencies, but our study demonstrates a reporting pattern that seems to reflect the prescribing pattern.
Conclusion: Gender differences in reports of ADRs in children <18 years in Norway during the last decade are small, but differences can be found for specific drugs where reporting seems to reflect prescription pattern. The results can be used to test hypothesis of true gender differences with regard to ADRs and reporting behaviour, for particular drugs.
PP159. Drug Treatment of ADHD in Children and Youths in Germany
E. Garbe, R.T. Mikolajczyk, A.A. Krautand I. Langner
Bremen Institute for Prevention Research and Social Medicine, Bremen, Germany
Objectives: Total prescriptions of methylphenidate have multiplied by a factor of 184 from 1990 to 2009 in Germany,[1] but little is known about drug treatment of ADHD on individual patient level. To describe drug treatment of ADHD in children and youths in Germany.
Methods: Using data from one large German health insurance (>7.2 million insurees), a cohort of children aged 3–17 years with a first diagnosis of ADHD in 2005 was followed until discontinuation of insurance, death, or December 31st, 2008 whichever was earliest. Kaplan-Meier estimates for onset of drug treatment with methylphenidate (MPH) or atomoxetine (ATX) were calculated for different follow-up time stratified by sex. First drug treatment, galenic formulation of first MPH treatment, and switches between ATX and MPH were ascertained. Psychiatric comorbidities, age, sex and ADHD-subtype were investigated as predictors of early (<6 months after cohort entry) versus late or no drug treatment using logistic regression.
Results: 6210 newly diagnosed ADHD patients (1443 girls) with a total follow-up time of 20 817 person-years (girls: 4827 person-years) were identified. The proportion of boys (girls) with a first prescription of MPH or ATX within 90, 183, 365 days or 3 years was 29.6 (27.9), 36.6 (34.5), 43.0 (39.0) and 52.8 (46.9) percent, respectively. Among those who received treatment, 91.6% were started on MPH and 8.4% on ATX. While 17.7% of MPH treated patients were started on a retard formulation, this proportion increased to 59.6% within the first year. During the first year of follow-up after initiation of treatment, 31.9% of patients started on ATX received at least one MPH prescription, whereas in 5.8% of patients started on MPH, a switch of drug treatment to ATX was observed. Significant predictors of early drug treatment were behavioural and emotional disorders (F91-F99, OR = 1.29, 95% CI 1.11, 1.50) and a diagnosis of ADHD with conduct disorder (OR= 1.26, 95% CI 1.11, 1.44).
Conclusions: About one third of ADHD children and youths with new diagnoses of ADHD received drug treatment in the first three months and about half within three years. A considerable number of patients received MPH retard formulations already at treatment initiation.
PP160. Safe Method of Propofol Infusion in Children: Pharmacokinetics and Pharmacodynamics of Lipid Emulsion Propofol in Children
H. Byon, J. Kim, H. Kim and C. Kim
Department of Anesthesiology and Pain Medicine, Seoul National University, Seoul, Korea
Objectives: the children population demonstrated poor predictability and wide inter-individual variability of plasma concentrations of propofol in target-controlled infusion.[1] This has been attributed to unique pharmacokinetic and pharmacodynamic characteristics in children, including greater central volume of distribution and systemic clearance,[2,3] and possibly lower potency of propofol.[4,5] The aim of this study was to characterize pharmacokinetics and pharmacodynamics of lipid emulsion propofol in children.
Methods: Forty patients (ASA PS 1, 2) aged 2–12 years were given an intravenous bolus of 2% propofol (Fresofol, Fresenius Kabi Korea Ltd, Korea) 3 mg/kg, followed by continuous infusion at the rate of 0.2 mg/kg/min for variable periods. Arterial concentrations of propofol were measured at preset intervals and bispectral index (BIS) values were recorded throughout the study period. Pharmacokinetic and pharmacodynamic characteristics were evaluated using a population analysis with nonlinear mixed effects modeling.
Results: Pharmacokinetics and pharmacodynamics of propofol in children were best described by a two compartment model and inhibitory sigmoid Emax with effect-compartment model, respectively. Population parameter estimates, inter-individual variability, and median parameter values (2.5–97.5%) of the non-parametric bootstrap replicates of the final pharmacokinetic and pharmacodynamic models are shown in table 1 and 2, respectively.
Conclusions: In children, body weight was a significant covariate for V2 and Cl. The blood-brain equilibration half-time was 1.54 min for BIS.
PP161. Risk of Cardiac Events in Patients Taking Atomoxetine: Results of a Matched Cohort Analysis
M. Davies, D. Layton, E. Tong and S. Shakir
Drug Safety Research Unit (DSRU), Southampton, UK; University of Portsmouth, Portsmouth, UK
Background: Atomoxetine, [Strattera™ (Eli Lilly & Co. Ltd)] was launched in the UK in June 2004 for the treatment of Attention Deficit Hyperactivity Disorder (ADHD) in children of 6 years and older and in adolescents as part of a comprehensive treatment programme.[1] Patients taking atomoxetine may experience a modest increase in pulse (mean <10bpm) and/or increase in blood pressure (mean <5mmHg)[1] There is the potential for an increased risk of QT interval prolongation when atomoxetine is administered with other QT prolonging drugs, drugs that cause electrolyte imbalance, and drugs that inhibit CYP2D6.[2]
Objectives: To examine the risk of cardiac events during treatment with atomoxetine compared to prior to starting treatment.
Methods: A post-marketing surveillance study using the observational cohort technique of Modified-Prescription Event Monitoring (M-PEM); Patients were identified from prescriptions issued by primary care physicians between Dec 04 and Sep 09. Data-collection forms sought information on cardiac events during and prior to starting treatment. A matched cohort analysis compared the risk of these events occurring in the during treatment period relative to the prior to starting treatment period. The matching by patient implied each patient acted as its own control. Conditional Poisson regression was used to estimate the risk ratios and 95% confidence intervals (CIs). The events in this analysis included all reported events regardless of causality and aetiology.
Results: The cohort comprised 4711 patients; median age 12 yrs and 85.0% male. The five cardiac events included in the matched analysis were cardiac arrest (CA), chest pain (CP), arrhythmia (A), tachycardia (T), & prolonged QT interval (PQT). Risk ratios (RRs) for these events were: [CA=1.00(CI: 0.06, 15.99), CP = 3.29 (CI: 1.41, 7.66), A = 0.86 (CI: 0.29, 2.55), T = 2.50 (1.20, 5.21), PQT = 1.00 (CI: 0.20, 4.95)], two RRs had p-values <0.05; chest pain & tachycardia.
Conclusions: The results indicate that a patients’ risk of chest pain/tachycardia is greater during treatment with atomoxetine compared to prior to starting treatment. Prescribers should consider this association when treating patients with a history of cardiac disease; these patients may have a predisposition to the development of chest pain and thus be at higher risk of this event during treatment with atomoxetine. Residual confounding is possible since the effective sample size is reduced as the analyses are based on only discordant pairs. This data should be considered with other pharmacoepidemiological data available on this topic.
PP162. Acute Renal Failure in an Infant Following Ingestion of Peganum Harmala
D. Soussi Tanani, N. Badrane, A. Chebat, R. Benkirane and R. Soulaymani Bencheik
Moroccan Pharmacovigilance Center, Rabat, Morocco
Background: Peganum harmala is a plant of the family Zygophyllacae, cosmopolitan species very common in North Africa and particularly in Morocco.[1] This plant contains alkaloids of beta-carboline with weak inhibitory properties of monoamine oxidase-A (MAO-A).[2]
Case report: It was a female infant aged 5 months who ingested a therapeutic dose of Peganum harmala powder by a herbalist for abdominal cramps. One day after the child was hospitalized with dyspnea, a sonorous rales and functional acute renal failure (blood urea 1.9 g/L; blood creatinine 40 mg/L). The clinical and biological evolution of an infant was favorable after 4 days of hospitalization in intensive care with a purely symptomatic treatment based on rehydration and monitoring hourly urine output.
Discussion: Peganum harmala is known by its common multiorgan toxicity with serotonin syndrome. The first symptoms of toxicity MAO-A include drowsiness, dizziness, nausea, ataxia, headache, nervousness, anxiety, palpitations, nystagmus and tremor. Serious complications are hyperpyrexia, hemolysis, rhabdomyolysis, disseminated intravascular coagulation, acute renal failure, ventricular fibrillation, cardiac arrest, and pulmonary edema. When death occurs, it is usually the result of multiple organ failure or cardiac arrest.[3]
Conclusion: Peganum harmala is a toxic plant particularly severe in young children because their renal function is immature. This poisoning should be managed like antidepressants monoamine oxidase A since there is no specific antidote.
PP163. Individual Case Safety Reports and Useful Clinical Information
K. Star,1 N.B. Almandil,2 I.C. Wong 3 and I.R. Edwards 4
1 Uppsala Monitoring Centre, Uppsala, Sweden; Department of Public Health and Caring Sciences, Uppsala University, Uppsala, Sweden; 2 Centre for Paediatric Pharmacy Research, School of Pharmacy, University of London, London, UK; 3 Centre for Paediatric Pharmacy Research, School of Pharmacy, University of London, London, UK; Department of Pharmacology and Pharmacy, Li Ka Shing Faculty of Medicine, The University of Hong Kong, Hong Kong; 4 Uppsala Monitoring Centre, Uppsala, Sweden
Objectives: Individual case safety reports (ICSRs) could be an important source in giving further information to characterize the risk situation and aid in the prevention, diagnosis, management and treatment of adverse drug reactions (ADRs). The aim was to determine whether and where on the ICSRs clinically useful information was specified for rare ADRs in the paediatric population.
Methods: ICSR concerning rhabdomyolysis occurring during use of antipsychotic medicines for patients up to 17 years of age were retrieved from the WHO Global ICSR database, VigiBase. The original case reports were requested and received from the national pharmacovigilance centres. We focused on five areas of information specified in a recent guideline for publishing ADRs.[1]
Results: Eighteen original cases with an age span from 5 to 17 years were reviewed with the following outcomes.
Circumstances preceding the reaction: 9 reports included this information, consisting primarily of abdominal, muscle and back pain. In eight of these reports, the full account of the symptoms and sequence of events were only found in the narratives.
Underlying risk factors for rhabdomyolysis: Recorded for four of five patients in the narrative: seizures (n=1), strenuous physical activity (n=2), diabetic ketoacidosis (n= 1), alcohol use (n = 1). Four patients had Neuroleptic Malignant Syndrome (NMS) co-reported.
Physical examination and laboratory tests: All values for patient temperature and laboratory values were given in free text. Elevated creatine phosphokinase (CPK) or myoglobin values were recorded in 14 reports ranging from 1200 to 95 000IU/L (CPK). Patient temperature was specified for 5 patients, of whom 3 patients were also reported to experience NMS.
Drug-reaction time-to-onset: 13 reports included information on the duration from drug start to reaction onset, which ranged from 4 days to 1.5 years. 9 reports included dates in the structured data, so that time to onset could be calculated and in 4 reports the information was specified in the narratives.
Treatment of the reaction: Apart from stopping the drug (n= 18) and hospitalization (n= 16), other actions of treatment, such as forced intravenous fluids or resolving spontaneously, was given for 5 cases in the narrative.
Conclusions: This study showed that useful clinical information was available to characterize the risk situation for these patients in this subset of reports. This should be regarded in the context that ICSRs are generally considered to be of poor quality. However, access to the free text fields recorded by the reporter was crucial to capture this information.
PP164. Using PMSI Database to Identify Adverse Drug Reactions in a Pediatric University Hospital
A. Batz,1 E. Bondon Guitton,1 G. Durrieu,1 M. Lapeyre Mestre,1 D. Petiot 2 and J. Montastruc 1
1 Laboratoire de Pharmacologie Médicale et Clinique, Centre Midi-Pyrénées de PharmacoVigilance, de Pharmacoépidémiologie et d’Informations sur le Médicament, Equipe de Pharmacoépidémiologie, INSERM U1027, Université de Toulouse, Faculté de Médecine, Centre Hospitalier Universitaire, Toulouse, France; 2 Département Information Médicale, CHU de Toulouse, Université de Toulouse, Toulouse, France
Objectives: Spontaneous notifications of adverse drug reactions (ADRs) to Regional PharmacoVigilance Centers suffer from underreporting, especially in children.[1] Combination of different sources of data (spontaneous reporting+computerized medical databases) could improve ADRs notifications. We performed a previous exploratory study in order to identify ADRs using data from the Programme de Me’dicalisation des Syste’mes d’Information (PMSI). The aim of the present study was to evaluate ADRs from hospital PMSI and to compare to spontaneous notifications in the Children University Hospital of Toulouse.
Methods: The study was conducted from January 2008 to December 2009. We selected 153 ICD-10 codes (10th International Classification of Diseases) related to an ADR. From the PMSI database, we listed, during the study period, all discharge summaries including the selected ICD-10 code. Hospitalization summaries of each patient were reviewed to check out if there was any mention of ADR. From the French PharmacoVigilance (PV) database, all ADRs which occurred during the study period and were reported by physicians working in the Children University Hospital of Toulouse were collected.
Results: During the study period, we retained 35 reports from the PMSI database and 89 from the French Pharmacovigilance Database. Ten common cases were found from both databases. Mean age of children was 7.3 years for PMSI and 10.2 years for PV database. Compared to PV database, proportion of children suffering from chronic pathologies tended to be higher in PMSI database (76% vs 57%). Rate of ‘serious’ ADRs was also higher in PMSI reports (80% vs 20%). The most frequently suspected drugs were antineoplasics (n = 11), corticoids (n = 7) and immunosuppressive drugs (n = 5) for PMSI and antibiotics (n = 27), immunoglobulins (n = 22) and analgesics/NSAIDs (n= 18) in spontaneous notifications.
Conclusions: Using PMSI database can improve detection of ADRs. In our study, we obtained a 28% increase in identification of ADR. These results also show that, compared to spontaneous notifications, use of PMSI could provide additional knowledge of ADRs in children and underline the importance of this application in routine practice.
PP165. Adverse Drug Reactions to Antiretroviral Therapy: Prospective Study in Children in Sikasso (Mali)
A. Oumar,1 K. Diallo,2 L Samake,3 I. Sidibe,1 B. Togo,4 M. Sylla 4 and S. Dao 5
1 Faculty of Medicine, Pharmacy and Odontostomatology, Bamako, Mali; 2 Pediatric Hospital, Sikasso, Mali; 3 Department of Hospital Pharmacy, Sikasso, Mali; 4 Department of Pediatric Hospital Gabriel Toure, Bamako, Mali; 5 Infectious Diseases Department, CHU-point G, Bamako, Mali
Objectives:To describe the frequency, nature and preventability of community-acquired and hospital-acquired adverse drug reactions (ADRs) in Malian children.
Method: A 6 months prospective observational study of 92 children admitted to pediatric hospital in Sikasso. It was a prospective and observational study which lasted 6 months from 1 June 2009 to 30 November 2009. The patients were treated with the generic drug. Prior to treatment initiation, demographic characteristics, clinical history and biological parameters including CD4 cell counts, were collected for each patient. WHO’s sides effects classification has been used to characterize the side effects. Analysis of data has been done in the Software EPI Info version 6.04.
Results: 92 children’s HIV infected patients meet the criteria of Inclusion. After 24 weeks of treatment, we observed that 14.1% of children had at least one side effect during our study. Side effects that many were as varied and most observed were rash cutaneous, Nausea, vomiting, diarrhea, respectively 38.5%; 23.1%; 15.4% and 15.4%. The side effects dominated by digestive disorders (61.5%). Adverse effects and toxicities were grade 1, 2 and 3. Side effects were grade 1 in most cases. One case of grade 2 and one case of grade 3 were observed with rash. We observed one case of grade 3 side effects during our study. The regimen of treatment was unchanged at 84.8%. It was changed in 15.2% including one case because of side effects.
Conclusion: The primary and secondary prevention of adverse events within their routine reporting and analysis of drug accountability especially in children infected with HIV. We recommend an active pharmacovigilance system for the sustainable management of side effects of antiretroviral drugs in patients infected with HIV in Sikasso (Mali).
PP166. Drug -Related Problems in Hospitalised Children in the United Kingdom and Saudi Arabia
A.N. Rashed,1 A. Neubert,2 S. Tomlin,3 J. Jackman,3 H. Alhamdan,4 A. Shaikh,4 A. Attar,4 M. Aseeri 4 and I.C. Wong 5
1 Centre for Paediatric Pharmacy Research, The School of Pharmacy, University of London, London, UK; 2 Centre for Paediatric Pharmacy Research, The School of Pharmacy, University of London, London, UK; Department of Paediatric and Adolescent Medicine, FAU Erlangen-Nuremberg, Erlangen, Germany; 3 Evelina Children’s Hospital, Guy’s & St Thomas’ NHS Foundation Trust, London, UK; 4 Kind Abdul-Aziz Medical City-Jeddah, National Guard Health Affairs, Jeddah, Saudi Arabia; 5 Centre for Paediatric Pharmacy Research, The School of Pharmacy, University of London, London, UK; Department of Pharmacology and Pharmacy, Li Ka Shing Faculty of Medicine, The University of Hong Kong, Hong Kong
Background: Drug-related problem (DRP) is “an event or circumstance involving drug therapy that actually or potentially interferes with the desired health outcome”.[1] The extent and characteristics of DRPs in children in the UK and Saudi Arabia (KSA) is unknown.
Aim: Our aim was to identify the incidence and characteristics of DRPs in children attending A&E/admitted to a hospital in the two countries.
Methods: A prospective cohort study in children aged 0–18 years admitted to the medical ward, paediatric intensive care unit (PICU), and neonatal intensive care unit (NICU) or attending A&E during a three-month period in two hospitals were carried out. Data were collected on a form adapted from the Pharmaceutical Care Network in Europe (PCNE) DRP-Registration Form V5.01. Patients’ charts, medical records and laboratory data were reviewed daily to identify DRPs; their preventability and severity were assessed.
Results: 990 children [median 3 years, IQR; 10 months — 8 years, 58.6% male] were included. 388 patients suffered from 546 DRPs. Overall DRP incidence was 39.2% (95% CI, 36.1, 42.3) being higher in KSA than in the UK (44.8% vs 33.3%, p< 0.001). Incidence was found to be highest in PICU (59.7%; 95% CI, 47.0, 71.5). Dosing problems were the most frequently reported DRPs (n= 303, 55.5%), followed by drug choice problems (n = 91, 16.7%). 80.0% of DRP cases were preventable; 71.4% (n = 390) DRPs were assessed as minor and 27.8% (n = 152) as moderate. 295 (54.0%) were totally resolved, of which 220 (74.6%) were resolved by pharmacists.
Conclusions: DRPs are a significant problem in the paediatric population in the UK and KSA, the majority of which are preventable. Increased focus on paediatric pharmacology and pharmacotherapy within paediatric medical and nursing education is an important step in improving prescribing practices.
PP167. Drug Use and Acute Liver Injury in Children:Signal Detection Using Multiple Healthcare Databases
C. Ferrajolo,1 G. Trifirò,2 P.M. Coloma,3 M.J. Schuemie,3 R. Gini,4 R. Herings,5 J. Hippisley Cox,6 G. Mazzaglia,7 G. Picelli,8 L. Scotti,9 L .Pedersen,10 J. Van Der Lei 3 and M. Sturkenboom 11
1 Department of Medical Informatics, Erasmus Medical Center, Rotterdam, The Netherlands; Pharmacovigilance and Pharmacoepidemiology Center, Campania Region, Department of Experimental Medicine, Pharmacology Section, Second University of Napoli, Italy; 2 Department of Medical Informatics, Erasmus Medical Center, Rotterdam, The Netherlands; Department of Clinical and Experimental Medicine and Pharmacology, Section of Pharmacology, University of Messina, Messina, Italy; 3 Department of Medical Informatics, Erasmus Medical Center, Rotterdam, The Netherlands; 4 Agenzia Regionale di Sanità della Toscana, Florence, Italy; 5 PHARMO Institute, Utrecht, The Netherlands; 6 Division of Primary Care-School of Community Health Sciences, University of Nottingham, UK; 7 Società Italiana di Medicina Generale, Florence, Italy; 8 Pedianet-Società Servizi Telematici SRL, Padova, Italy; 9 Department of Statistics, Università di Milano-Bicocca, Milan, Italy; 10Department of Clinical Epidemiology, Aarhus University Hospital, Aarhus, Denmark; 11Department of Medical Informatics, Erasmus Medical Center, Rotterdam, The Netherlands; Department of Epidemiology, Erasmus Medical Center, Rotterdam, The Netherlands
Background: Drug-induced acute liver injury (ALI) is one of the leading causes of drug withdrawal from the market. There is, however, lack of data on ALI in the pediatric population. Combining multi-country electronic healthcare databases offers the opportunity to explore the risk of ALI in children and adolescents and facilitate detection of potential drug safety signals.
Objectives: To identify drugs potentially associated with ALI in the pediatric population using the EU-ADR database network and to estimate the power of such a network for signal detection concerning ALI as a function of actual drug use, minimal detectable relative risk (RR) and Background incidence rate (IR) of ALI in children and adolescents.
Methods: We extracted data on all potential cases of ALI and data concerning prescribed/dispensed drugs among individuals 0–15 years registered within eight European, population-based, electronic medical record and claims databases of the EU-ADR network during the period 1995–2010. We estimated the Background IR of ALI in the pediatric population and assessed drug use according to number of person-years (PYs) of exposure by Anatomical Therapeutic and Chemical (ATC) classification, 5th level. Based on IR of ALI derived within EU-ADR, power = 80% and alpha = 5%, we estimated how much drug exposure would be necessary to allow for detection of a signal concerning ALI. Finally, among drugs with enough exposure, all potential signals were identified by measuring age- and sex-adjusted relative risks of ALI, with all other drugs as comparator.
Results: Children 0–15 years of age contributed 20088 726 PYs of follow-up to the EU-ADR database network. The incidence rate for ALI was estimated to be 4.3 per 100000 PYs in this pediatric population. The total amount of drug exposure that would be required to detect a ‘weak’ association (RR = 2) with ALI, if present, was 186490 PYs and 28 554 PYs to detect a ‘moderate’ association (RR=4). The following drugs were identified to be potentially associated with ALI: amoxicillin (RR 4.3, 95% CI 2.6, 7.0); clarithromycin (3.7, 1.8, 7.5); cetirizine (3.1, 1.5, 6.5); flunisolide (2.5, 1.0, 6.8); budesonide (2.5, 1.1, 5.5); and amoxicillin plus clavulanic acid (2.3, 1.3, 4.1).
Conclusions: Combining multiple electronic healthcare databases may facilitate identification of potentially drug-related cases of ALI and increase the power for drug safety signal detection in the pediatric population. Except for the anti-asthmatic medications, the signals detected are already known in adults. Safety Problems of Monoclonals PP168. Meta -Analysis of Malignancy Risk in Rheumatoid Arthritis from 29 Trials: Comparison of Intention to Treat and Per Protocol Analyses
G. Moulis, A. Sommet F. Montastruc, J. Béné, L Sailler, J. Montastruc and M. Lapeyre Mestre
Department of Clinical Pharmacology, Toulouse Teaching Hospital, Toulouse, France; Pharmacoepidemiology Unit, INSERM U1027, Toulouse, France; University of Toulouse, Toulouse, France
Objectives: The risk of malignancies on anti-TNF-a therapies is controversial. [1] Sparse events are difficult to assess in meta-analyses (MA).[2] The aim of this study was to compare intention to treat (ITT) and per protocol (PP) MA assessing the initial risk of malignancies on the five marketed anti-TNF-a in adult rheumatoid patients from randomized controlled trials (RCTs).
Methods: We conducted a search strategy to identify published double-blind RCTs with an exposure to anti-TNF-α for more than 12 weeks in MEDLINE, CENTRAL and ISI Web of Science by two evaluators. Unpublished trials were assessed through the ACR and EULAR abstracts, the scientific evaluation of the drugs leading to marketing approval and clinicaltrials.gov. Quality of RCTs was assessed with Delphi list and Oxford scale. Authors and laboratories were contacted to provide missing data. Random-effect MAs were conducted on pooled data to assess the risk of cancers overall, solid tumors, hematological malignancies, skin cancers, non-melanoma skin cancers and melanomas. Null values were treated with continuity corrections (three methods tested).[2] In case of several anti-TNF-α arms in a RCT, we first considered for the analysis the arm in line with the New Drug Application (NDA), then whatever the dose, and conducted both ITT and PP analyses.
Results: Among 2037 published references and 22 unpublished trials, we selected 29 trials for MA. OR [95% CI] were: when anti-TNF-α were used in line with NDA, 0.80 [0.50–1.29] (PP) and 1.15 [0.72–1.84] (ITT); whatever the dose, 0.82 [0.54–1.24] (PP) and 1.18 [0.78–1.79] (ITT). For each type of cancer, OR (ITT) was also higher than OR (PP). For each model, there was no heterogeneity (Cochran’s Q>10%, I2 = 0%) and no publication bias (Egger’s test: p=0.55). This discrepancy can be explained by a bias of diagnosis. Indeed, loss of follow-up and other drop-out patients are more numerous in placebo arms and may be undiagnosed for a cancer; that leads to overestimate the risk on anti-TNF-α. On the contrary, PP analysis has not this bias, thus all patients included has been exposed to placebo or anti-TNF-α during all the trial, but it underestimates the risk on anti-TNF-α because it emphasizes odds in placebo group whatever the continuity correction used.
Conclusions: Avoiding a diagnosis bias, PP analysis is safer in case of important loss of follow-up, but it underestimates treatment effect in case of very sparse events (here, hematological neoplasm and melanoma).
PP169. Intensive Monitoring of Adverse Drug Reactions in Patients Receiving Pharmacological Treatments for Rheumatoid Arthritis and Other Rheumatologic Diseases, with Particular Focus on Biotechnological Drugs: The ASTRAGALUS Study
M. Tuccori,1 G. Giustarini,2 L Bazzichi,3 S. Manganelli,4 F. Peruzzi,5 O.M. Sacu,6 L. Picchianti,2 A. Capogrosso,2 M. Rossi,2 F Sernissi,3 C. Giacomelli,3 R. Neri,3 M.G. De Montis,7 F. Nacci F .Lapi,8 C. Scollo,2 S. Mantarro,2 S. Montagnani,2 L. Sabadini,6 A. Testi,2 E. Ruggiero,2 A. Vannacci,8 A. Mugelli,8 S. Bombardieri,3 M. Matucci Cerinic,5 M. Galeazzi 4 and C. Blandizzi
1 Unit of Pharmacology, University Hospital of Pisa, Pisa, Italy; 2 Tuscan Regional Centre of Pharmacovigilance, Florence, Italy; 3 Section of Rheumatology, University Hospital of Pisa, Pisa, Italy; 4 Section of Rheumatology, University Hospital of Siena, Siena, Italy; 5 Section of Rheumatology, University Hospital of Careggi, Florence, Italy; 6 Section of Rheumatology, Garbasso Hospital, Arezzo, Italy; 7 Dept. of Neurosciences, Unit of Pharmacology, University of Siena, Siena, Italy; 8 Dept. of Pharmacology, Center for Molecular Medicine (CIMMBA) — University of Florence, Florence, Italy; 9 Interdepartmental Centre of Clinical Pharmacology and Experimental Therapeutics, University of Pisa, Pisa, Italy
Objectives: ASTRAGALUS is a three-year observational study, which has been started in 2010 in Tuscany to investigate the incidence and clinical features of adverse events (AEs) in patients receiving biologic drugs for rheumatologic disorders.
Methods: Patients are being enrolled in four Rheumatology Units at the Hospitals of Pisa, Firenze, Siena and Arezzo. Medical records of eligible patients have been checked to collect retrospective information on their clinical history (adverse events, drug treatments and dose regimens, concomitant therapies, disease course, laboratory data). Patients will be then followed-up prospectively for up three years through scheduled visits. All diseases and adverse events are classified by MedDRA Term dictionary. Patients currently or formerly receiving treatments with biologic drugs (infliximab, etanercept, adalimumab, rituximab, tocilizumab, abatacept and anakinra) have been requested to read and sign informed consent to participate to the study. AEs are classified as adverse drug reactions (ADRs) when they scored at least as possible upon evaluation by Naranjo algorithm for causality assessment, [1] The present analysis reports the first 10 months of observation.
Results: Patients recorded in the study database were 396 (259 females; mean age: 54.90±13.78). 444 AEs have been recorded, 35 of which were classified as serious. Patients with at least one AE were 190, and 120 were classified as having experienced ADRs. Table I summarizes the number of patients with at least one ADR and their frequency in subgroups receiving the different biologic drugs under evaluation (Table I).
The AEs more commonly recorded in the database were: inflammatory condition (65 cases), oropharyngeal pain (52), cough (50), infectious disease (47), fever (37), transaminase increased (31), diarrhea (24), reaction related to infusion (19), dysuria (18) and leukopenia (11). Serious ADRs associated with biologic treatments were: angioedema, hemorrhagic cystitis, lung infection, Guillaine-Barre syndrome and salivary gland cancer for adalimumab; Prinzmetal angine for tocilizumab; squamous cell carcinoma, skin ulcer, myocardial infarction and pericardial effusion for etanercept; respiratory failure for rituximab; pericarditis, pleural effusion and infusion reaction for infliximab.
Conclusions: Overall, according to the present preliminary analysis, biologic medications are frequently associated with the development of adverse reactions, which are mild to moderate in severity. However, serious reactions may also occur. Our data confirmed also the development of infectious diseases and infusion reactions as prominent issues related to these therapies. Accordingly, a careful monitoring of patients receiving biologic drugs is required for an early identification and management of potentially harming adverse effects.
PP170.Tumor Necrosis Factor Inhibitors and Cancer:A 10 -Year Review of the French Pharmacovigilance Database
L .Saliba,1 N. Petitpain,2 B. Baldin,3 P. Gillet,2 J. Montastruc 1 and H. Bagheri 1
1 Centre Midi-Pyrénées de Pharmacovigilance, CHU Toulouse, Faculté de Médecine, Equipe de Recherche de Pharmacoépidémiologie INSERM U1027, France; 2 Centre de Pharmacovigilance de Nancy, France; 3 Centre de Pharmacovigilance de Nice, France
Background: TNF alpha is involved in cytotoxic T-response against lymphomatous B-cells[1] and then they could contribute to increase the risk of lymphoma.[2,3] Concerning the risk of solid cancer due to TNF inhibitors, the results of different studies remains contrasted and according to published data, the risk remains not relevant.
Objective: The aim of the present study was to describe the cases of cancer reported for adalimumab, etanercept or infliximab to the French Pharmacovigilance system.
Methods: Data of the French National Pharmacovigilance Database (FPVDB) were analyzed from January 2000 to October 2010. All Adverse Drug Reactions (ADRs) concerning cancer were classified according to the Medical Dictionary for Regulatory Activities (MedDRA) classification.
Results: A total of 356 cases of cancer classed to 2 groups were collected: “monotherapy” receiving one TNF inhibitor including 288 patients (80.9%) with a mean age of 58 years old (sex ratio=0.79) and “polytherapy” exposed to 2 or more TNF inhibitors including 68 patients (19.1%) with a mean age of 60 years old (sex ratio=0.66). No cases were reported in pediatric population. The mean delay of exposure to TNF inhibitors was 26 months for monotherapy and 32 months for polytherapy group. The majority of patients had already been treated with other immunosuppressive drugs such as methotrexate or corticosteroids (60% in the monotherapy group, 76% in the polytherapy one).
Conclusion: According to the published data, the type of cancer spontaneously reported by TNF inhibitors concerns mainly haematological tumors (lymphoma and leukemia) followed by skin, respiratory, gastrointestinal, and breast cancer. This study reported the descriptive data of anti-TNF-induced cancer in FPVDB. More studies should be necessary to confirm or infirm a potential risk.
PP171. Anaphylactic Reactions to Biological Drugs:Data from Spontaneous Reporting in Italy
U. Moretti,1 M. Donati,1 L Sottosanti,2 L Catalano,2 E. Boccola 3 and G. Zanoni 3
1 Pharmacology Unit and Pharmacovigilance Centre of Veneto Region, University Hospital, Verona, Italy; 2 Italian Medicines Agency, Pharmacovigilance Office, Rome, Italy; 3 Immunology Unit, University Hospital, Verona, Italy
Objectives: Biological drugs are large and complicated molecules with specific characteristics that can influence their safety profile. Biological drugs such as monoclonal antibodies have been associated to anaphylactic reactions. However clinical diagnosis of anaphylaxis could be a difficult, since involvement of body organ systems varies among patients. Differential diagnosis should consider common entities, such as acute generalized hives, asthma, syncope or panic attack, and cardiovascular or neurologic events. Aim of this study is to analyze reports of anaphylaxis caused by biological agents in the Italian spontaneous reporting database.
Methods: According to the European Medicines Agency definition of biological[1] and excluding vaccines and allergenic products, in the analysis we include drugs with the name ending with the string “mab” or “cept”. Cases of anaphylaxis have been defined as follows: Group A: reports associated to the WHO-Adverse Reaction Terminology Preferred Terms “Anaphylactic shock”, “Anaphylactoid reactions” and “Anaphylactic reactions” or report with the string “anaph” in the description of the adverse event; Group B: reports with adverse reactions referring to at least two of selected System Organ Classes (skin, respiratory, cardiovascular and gastrointestinal disorders) with an onset within 24 hours after administration. All selected cases were reviewed and the case definition from the “Second Symposium on the Definition and Management of Anaphylaxis” was applied to evaluate the reports.[2]
Results: The Italian database up to March 2011 contains 3820 reports related to the biological included in the study. According to selection criteria, a total of 334 reports were identified: 65 for group A and 269 for group B. By application of the anaphylaxis case definition and after the case-by-case review 2 cases in Group A and 139 in Group B were excluded. Out of 193 reports meeting the case definition, 8 (4.1%) were reported in children or adolescents up to 18 years of age. The most reported drugs were infliximab with 83 (43%) cases, followed by cetuximab (41-21%) and rituximab (28-14%); other 11 different biologicals were associated with the remaining 32 cases (22%), with up to 8 reports each.
Conclusions: Spontaneous reporting is an important source to provide further knowledge on the reactogenicity of biological agents. Three-fourths of reports were related to three chimaeric antibodies containing a murine component. A high number of cases were identified through the combination of selected reported terms, even if expert review of individual reports was needed.
PP172. Presentation of Drug Safety Surveillance Form and Tuberculosis and Malignancy Risk in Patients Using Anti -TNF Drugs
D. Aydinkarahaliloglu,1 Y. Kasap,1 E. Aykaç,1 G. Sağiş 1 C. Babacanoğlu,1 H. İlbars,1 M. Turgay,2 H. Özbek 1 and S. Kerman 1
1 General Directorate of Pharmaceuticals and Pharmacy, Ministry of Health, Ankara, Turkey; 2 Department of Rheumatology, Ankara University, Faculty of Medicine, Ankara, Turkey
Background: Anti-TNF drugs have been in use for approximately 10 years. The most important adverse reactions observed with anti-TNF drugs are infections, especially tuberculosis, and malignancies. During the prescription of these drugs, informing the patient and performing the necessary examinations on the patient with respect to the risk factors should be ensured. For that purpose the “Drug Safety Surveillance Form” and “Patient Consent Form” initially developed for infliximab, adalimumab, etanercept and subsequently introduced for abatacept and canakinumab.
Objective/Aim: The present study will focus on tuberculosis and malignancy cases resulting from anti-TNF use and will elaborately investigate three Hodgkin Lymphoma cases observed in patients with ankylosing spondylitis.
Methods: The adverse reactions resulting from anti-TNF drug use between 2005 and 2010 were investigated in Vigiflow database on excel format generated by the system.
Results: A total of 35 tuberculosis cases and 32 malignancy cases were reported to WHO database from 2005 to end of 2010. 3 of the tuberculosis cases were extrapulmonary tuberculosis cases. The most frequent malignancies were breast and lung cancers. Hodgkin Lymphoma developed in three male patients with ankylosing spondylitis at the ages of 35, 38 and 44. While two of these patients were on etanercept, one of them was on infliximab.
Conclusion: In patients receiving anti-TNF, the malignancies with an increased incidence among the corresponding gender and age group should be examined through a good anamnesis and physical examination, and the physician should be careful regarding development of extrapulmonary tuberculosis.
Discussion: The risk of latent tuberculosis reactivation and new on-set tuberculosis development shows an increase of at least two-fold during treatment with anti-TNF drugs. If the patient is also using corticosteroids, the risk increases even further.[1] The risk of lymphoma development during treatment with anti TNF drugs is considered to have increased 2.5 times compared to normal population.[2,3] Particularly the frequency of non-Hodgkin lymphoma is emphasized in adults using anti TNF drugs where Hodgkin lymphoma is rarely reported. However, anti-TNF use related Hodgkin Lymphoma was observed in three patients with ankylosing spondylitis in Turkey. It is of interest that these cases were more frequently observed in adults unlike the cases reported in Micromedex.
PP173. Risk of Activation or Reactivation of Latent Tuberculosis (TB) Associated with Monoclonal Antibody Therapy
W. Huang, S. Samalulu and D. Vu
Health Canada, Canada
Monoclonal antibody therapy is a type of immunotherapy that employs specific antibodies to bind specifically to target antigens, consequently stimulating the patient’s immune system to attack those targets. Currently, 20 monoclonal antibodies have been approved worldwide for the treatment of various serious diseases (such as rheumatoid arthritis, multiple sclerosis and different types of cancers) in humans. Monoclonal antibody therapy has obvious advantages over conventional therapy in terms of potency, specificity, and theoretically decreased side effects, as the product is engineered to bind to or interfere with a specific, distinct molecular target. These targeted immune modulators work by selectively blocking mechanisms involved in inflammatory and immune response. However, they have their own unique set of problems, principally because, they act by interfering with the body’s natural immunity, leading to concerns regarding increased rates of both common and unusual infections among treated patients. Tuberculosis (TB) has been reported in patients treated with immune suppressive monoclonal therapies, including adalimumab, infliximab, certolizumab, etanercept, abatacept, and daclizumab therapy. How a monoclonal antibody cause infection can be described by using adalimumab, as an example. Adalimumab is one of the Tumour Necrosis Inhibitor (TNF)- inhibitor, used for the treatment of rheumatoid arthritis. The TNF- is a cytokine that plays a central role in establishing and maintaining the inflammatory response against infection. TNF-blockade results in the interruption of TNF-mediated functions, which include cell activation and proliferation, cytokine and chemokine production, and the formation and maintenance of granulomas. It is therefore not surprising that TNF-inhibitors have been shown to increase the risk of granulomatous infections, most importantly tuberculosis (TB). In order to manage risk factors for TB, tuberculin skin testing, and a baseline chest X-ray, as indicated, should be performed prior to initiation of therapy, and if the patient tests positive, chemoprophylaxis for latent TB should be initiated prior to the start of treatment with monoclonal targeted immune modulators. Monitoring for active TB should also be done while patients are on immunotherapy, including those who tested negative for latent. Newer gamma interferon release assays have been advocated to enhance screening efficacy, although the effectiveness of this approach is still being evaluated.
PP174. Herceptin® (Trastuzumab) and the Incidence of Spontaneous Abortion
S. Daniels,1 M. Johnston 2 and L Hiles 2
1 Transcrip-Partners LLP, Pharmacovigilance, Reading, UK; 2 Roche Products Ltd, Safety Science, Welwyn Garden City, UK
Introduction: Trastuzumab is a recombinant humanised monoclonal antibody designed to target the human epidermal growth factor receptor 2 (HER2) and is approved for the treatment of patients with metastatic breast cancer, early breast cancer and advanced gastric cancer whose tumours overexpress HER2. Since its 1st approval in 1998, trastuzumab has been used in nearly 1 million women world-wide.[1] After the Marketing Authorisation Holder’s (MAH) internal signal detection system identified the event term ‘spontaneous abortion’ as a potential signal for further investigation within the company global safety database (based on ≥3 observed counts), an analysis was conducted to fully evaluate the signal.
Methods: The proportional reporting ratio PRRis the proportion of spontaneous reports for a given drug that are linked to a specific adverse outcome, divided by the corresponding proportion for all other drugs in the safety database. All pregnancy case reports that included event terms linked to spontaneous abortion were retrieved from the global safety database. A PRR stratified to include female patients over the age of 16 years was calculated for the retrieved reports. (see Table I).
Results: Cumulatively to March 2011, the MAH had received and processed information pertaining to 271 pregnancies in trastuzumab treated women. A total of 30 of these reportedly ended in spontaneous or missed abortion. Patients ages, provided in 23/30 case reports, ranged from 20–48 years (median 38 years).
Discussion: The overall rate of spontaneous abortion in the general population is reported as 15–20% and increases further with maternal age. The observed frequency of 30 reports of spontaneous/missed abortion represents 11 % of the total number of pregnancy reports received and is well below the expected incidence. Although the risk of foetal renal growth and/or function impairment (some of which resulted in fatal pulmonary hypoplasia of the foetus), in association with oligohydramnios is recognized,[2] this does not appear have an impact on overall spontaneous abortion rates.
Conclusion: From this data, there is no evidence to support an increased risk of spontaneous abortion in women treated with trastuzumab. It is worth noting that many of these women have multiple confounding features including their disease and/or concurrent or previous chemotherapeutic regimen and/or radiotherapy.
PP175. Impact of Adverse Drug Reactions of Drug -Substrates of the Metabolic Enzyme Cytochrome P450 2C9 and/or the Transporter Protein Pgp in a National Database
V. Macolic Sarinic,1 N. Bozina,2 N. Mirosevic Skvrce,1 D. Krnic,1 M. Banovac,1 S. Arapovic,1 A. Andric 1 and S. Tomic 1
1 Agency for Medicinal Products and Medical Devices (HALMED), Zagreb, Croatia; 2 University Hospital Centre Zagreb, Laboratory for Pharmacogenomics, Zagreb, Croatia
Objectives: Together with clinical factors and environmental factors genetic variations of metabolic enzymes and transporter proteins could be an important predisposition for the occurrence of adverse drug reactions. A retrospective observational study of adverse drug reactions (ADRs) caused by drug-substrates of the metabolic enzyme cytochrome P450 CYP2C9 and/or the transporter protein Pgp spontaneously reported to the Croatian Medicines Agency (HALMED) was performed. The aim was to identify the impact and importance of ADRs caused by drug-substrates of CYP2C9 and/or the transporter protein Pgp in comparison with all reports spontaneously reported to HALMED. The goal of the research was to estimate the role of potential genetic polymorphism in the development of adverse drug reactions.
Methods: ADRs which were caused by drug-substrates of CYP2C9 and/or the transporter protein Pgp were identified in the HALMED database for adverse drug reactions and compared with the characteristics of all national spontaneous reported ADRs in the period of 10 March 2005 till 30 June 2010. For statistical analysis SPSS 17.00 was used.
Results: 784 ADRs reports were caused by drug-substrates of CYP2C9 and/or the transporter protein Pgp in a total of 3395 spontaneous ADRs reports in the database which makes 23% of all reports. 63% of the patients who developed a ADRs caused by drug-substrates of CYP2C9 and/or the transporter protein Pgp were female, versus 56% in all reports. 63% ADRs caused by the drug-substrates are serious versus 53% ADRs in the whole database. 17% ADRs caused by the drug-substrates caused hospitalization and 7,1 % were life threatening versus 11 % and 1,2% respectively. The most ADRs caused by the drug-substrates are coded as Skin and subcutaneous tissue disorders (16,6% vs 14%) and Gastrointestinal disorders SOC ADRs (19% vs 15,6%). The ratio of ADRs reports which have 2 to 5 drugs taken by the patient is significantly higher for the drug-substrates in comparison with the reports from the whole database.
Conclusions: ADRs caused by drug-substrates of CYP2C9 and/or the transporter protein Pgp caused more hospitalization and were more life-threatening in comparison with all other reports. It seems that the role of genetic polymorphism in the development of adverse drug reactions is very important particularly in the field of interactions because the ratio of ADRs reports which have more than one drug taken by the patient is significantly higher for the drug-substrates of CYP2C9 and/or the transporter protein Pgp in comparison with the reports from the whole database.
Ecopharmacovigilance
PP176. Determination of Estrogens in Inputs and Outputs of WWTPs Using HPLC with UV Detection
A.P. Fonseca,1 S.M. Cardoso 2 and V.I. Esteves 3
1 Department of Pharmacy, College of Health Technology of Coimbra, Portugal; 2 Faculty of Medicine, University of Coimbra, Portugal; 3 CESAM — Department of Chemistry, University of Aveiro, Portugal
A precise quantification of natural and synthetic estrogens in Waste Waters Treatment Plants (WWTPs), waters for human consumption, rivers, lakes, etc., is essential for a risk assessment regarding endocrine disrupting effects in the aquatic environment. During the last years, great attention was given to the environmental diffusion of natural and synthetic estrogens, and to their harmful effects on human and wildlife health, such as increasing of the incidence of cancer and the decreasing reproductive fitness of humans. Estrone, estradiol, ethinylestradiol and estriol were identified and quantified using an HPLC procedure with UV detection, under optimized conditions, preceded by a solid phase extraction (SPE) as a pre-concentration method. The occurrence of these four compounds was studied in typical WWTPs and effluents receiving rivers. The input and outputs of estrogens in nine WWTPs located at the Portugal central region was evaluated. Our study results are in agreement with those published in similar types of water by other authors. The concentrations obtained for natural estrogens (estradiol, estrone, estriol) and for synthetic estrogen, ethinylestradiol, ranged from 80 to 120 ngL-1. These results demonstrated that a great concern should be addressed to the potential risk of the presence of estrogens in the aquatic environment.
PP177. Acute and Chronic Effects of Diclofenac in D. magna and D. longispinaJ
J.J. Joaquim,1 C. Ribeiro,2 J. Pereira 2 and F.J. Gonçalves 2
1 Department of Pharmacy, College of Health Technology, Polytechnic Institute of Coimbra, Portugal; 2 Department of Biology, University of Aveiro, Portugal
Consumption of pharmaceutical products is, in our societies, a reality in growth, originated in several factors. This continues increase in consumption induces, more and more, that the environment and in matter, the aquatic systems are the destiny of active pharmacological residues, being this contamination a concern for the incorporation of substances in the environment that can interfere in specific biological systems. In this sense the present work had as objective to identify and to evaluate the effects produced by Diclofenac Sodium, active substance present in several medicines (e.g. Voltaren® and Flameril®), in non-target aquatic organisms. For this goal we realize acute and chronic tests with cladocerans and in that we have compared the survival, reproduction and growth of Daphnia magna (a standard species) and Daphnia longispina (an autochthonous species). Diclofenac, are effective in the survivorship and reproduction of the two cladoceran species used in this study — D. magna and D. longispina. D. magna seems to be more tolerant to acute toxicity (EC50= 134.087 mg/L) and we found more sensibility to Diclofenac in D. longispina (EC50 = 35.353 mg/L). Diclofenac significantly affected the fecundity (LOEC = 38.745 mg/L) of D. magna and the somatic growth rate (LOEC = 57.713 mg/L), at the last concentration tested. For D. longispina the sublethal endpoints significantly affected by Diclofenac was fecundity (LOEC=5.0 mg/L), maturation (LOEC = 2.5mg/L). In addition, in the chronic exposure, the number and size of neonates of first brood are also impaired, in both species. Diclofenac, as an active substance with pharmacological effect for humans, generally impairs in the survivorship, reproduction and growth of the cladoceran species used in this study — D. magna and D. longispina. However, the concentration levels used to produce these effects in acute and chronic tests are much higher, if we compare with the concentration levels detected in the aquatic environment. In conclusion, Diclofenac affect more D. longispina at individuallevel endpoints (fecundity and maturation), in opposite to D. magna, where fecundity is impaired and the somatic growth rate is slightly, but significantly affected in the last concentration tested.
New Horizons in Pharmacovigilance
PP178. Approaching a New Method to Express the Incidence of Adverse Drug Reactions in Hospitalized Patients
M.L. Ponte,1 H.A. Serra 2 and A. Wachs 1
1 Hospital Argerich. Buenos Aires, Argentina; 2 First Chair of Pharmacology. Buenos Aires University, Buenos Aires, Argentina
Objectives: An increasing number of articles referring to ADRs are being published in the last fifteen years in the international bibliography. In most articles the incidence of ADRs is expressed as absolute numbers or as relative incidence of ADRs involving certain drugs or certain organ or system. Also, a lot of articles are performed in specialized hospitals or specialized rooms (nephrology, intensive care units, emergency rooms, etc). This kind of expression is useful to give a general knowledge, but it makes difficult to compare the incidence among different hospitals because it is not adjusted.
Methods: We intended to look for a general adjustment expression that can make easier to compare different works. We think the best is a form that we called ADR Rate. In the next box it can be seen the way to calculate the rate (see box): ADR rate = Number of events/number of hospital admissions in a period × 1000
Results: The possibilities of this rate are several, i.e.: • Total number of ADRs adjusted to hospital admissions (e.g. number of ADRs every 1000 admissions). • Certain kind of ADR (hepatotoxicity, nephrotoxicity, etc) adjusted to hospital admissions (number of drug induced hepatotoxicity every 1000 admissions). • Number of ADRs (total or organ specific) adjusted to admissions in a determined room (ADRs in nephrology every 1000 admissions in nephrology room). This maybe is the most important tool, because it makes possible to compare the incidence of ADRs in a monovalent hospital with a polyvalent hospital considering only ADRs and admissions in a determined room.
Conclusions: We consider that the application and standardization of this new method of expression will facilitate the comparison of different studies of pharmacovigilance performed in different hospitals. Reference
PP1 79. Nephrotoxicity Induced by Herbal Medicines Used in DR Congo
C.V.Zinga,1 N.M. Nseka,2 G.K. Mesia,3 E.K. Sumaili,2 F.B. Lepira,2 P.N. Ntamabyaliro,3 Y.N. Lula 3 and G.L. Tona 3
1 Service de Néphrologie, Cliniques Universitaires de Kinshasa, Université de Kinshasa, Kinshasa, DR Congo; Centre National de Pharmacovigilance, Kinshasa, DR Congo; 2 Service de Néphrologie, Cliniques Universitaires de Kinshasa, Université de Kinshasa, Kinshasa, DR Congo; 3 Unité de Pharmacologie Clinique et Pharmacovigilance, Facultés de Médecine et des Sciences Pharmaceutiques, Université de Kinshasa, Kinshasa, DR Congo; Centre National de Pharmacovigilance, Kinshasa, DR Congo
Background: Herbal medicines (HMs) are popular in many African countries and is now considered as an alternative medicine in low income countries.[1] Adverse drug reaction with central African herbal medicine aren’t yet well documented and patient ignore the risk of their use. During past years, serious and severe nephrotoxicities were observed in our university hospital. In the aim to establish a causality with the use of herbals, a cohort study were performed.
Objectives: To identify herbal medicines concerned and to evaluate the kidney damage induced.
Methods: A cohort study was conducted in the unit of nephrology at the University hospital between 2004 and 2009. Kidney injury was confirmed with creatinine elevated or with an acute oligo-anuria. Because of the lack of pharmacological data of most herbal, the ADR assessment was confirmed mainly by chronologic criteria after exclusion of others etiologies.
Results: 1016 patients were admitted at the nephrology unit of university hospital. During this period, 393 cases of acute kidney impairment were observed in which 201 cases of nephrotoxicity, 154 (39.2%) was attributed to herbal medicines. Herbal medicines were used for different purposes. HMs involved are: Iridacee glaliolus (25%), Tetradenia ripana (14%), Quassia africana (13%), Zingiber officinalis (8%), Pentadiplandra brazzeana Baill, Alchornea cordifolia Muell.Arg, Morinda morindoides, Ocimum americanum LINN, Hymenocardia ulmoides OLIV, Annona senegalensis PERS, Nauclea latifolia SMITH, Moringa oleifera. Some Foreign HMs as Aristolochia triangularis, Clematis chinensis, Aloe vera and Xin yi wan were also found in this cohort.
Conclusions: Nephrotoxicity is one of the serious adverse reaction and could be encountered with plant commonly used in popular medicine in DRCongo. The frequency of nephrotoxicity induced by HMs in our study is quite similar to those reported by other studies.[2] Many studies have previously reported nephrotoxicity with some foreign herbals found in this study as Aloe vera, Aristolochia Triangularis, Clematis chinensis and Xin yi wan.[3–6] The question is to determine if the effect observed is also due to aristolochic acid as reported in the literature. Therefore, it is necessary to monitor HM ADRs, to make available relevant data, to awake population consciousness and to discart from the market those with poor safety.
PP180. Online Notifications of Adverse Drug Reactions:A Study in Midi -Pyrénées Pharmacovigilance Regional Centre
D. Abadie, M. Bert, G. Durrieu and J. Montastruc Laboratory of Pharmacology Faculty of Medicine, Toulouse, France
Objectives: The Midi-Pyrénées PharmacoVigilance Regional Center (CRPV) set up in July, 2010 an innovative way to report Adverse Drug Reactions (ADRs). From this date, it is possible (for both Midi-Pyrénées practitioners and patients) to declare ADRs directly through the “Bulletin d’Information de Pharmacologie” website (http://www.bip31.fr). The main objective of the study was to evaluate the use of this new Web-based ADR reporting system. The secondary objective was to describe and to compare online notifications characteristics to those notified via conventional reporting (post, fax, telephone or visits) to Midi-Pyrénées CRPV.
Methods: We compared the characteristics of online ADR notifications reported to Midi-Pyrénées CRPV between July 7th, 2010 (first online notification) and May 1st, 2011 to those of a three times higher random sample of conventional notifications reported to the CRPV during the same period. Variables analyzed were practice location of the reporters, suspected drugs, “seriousness” and nature of the ADR. Drugs and ADRs were translated to ATC codes and MedDRA classifications, respectively. Chi-square tests were used to examine the associations between the method of reporting and variables analyzed. A p value <0.05 was considered to be significant.
Results: The total number of online reports was 146 over the 10-month period, with linearly increase over time. We sampled 438 of the 1555 notifications received at the CRPV via conventional route during the interval time. Online notifications came more often from liberal practitioners in comparison to conventional notifications (31% vs 7%, p = 2.10–14) and were less «serious‘ (58% vs 69%; p = 0.02). Whatever the declaration way, skin and gastrointestinal diseases were the most reported, “nervous system” and “anti-infectious” drugs the most frequently involved. However, besides conventional notifications, those reported online were associated with a higher proportion of eye affections (5% vs 1%, p = 0.001) and with more “nervous system” drugs (32% vs 23%, p = 0.005).
Conclusions: Online report via a website is a new method to declare ADR. We demonstrate that it is feasible to deploy a Web-based ADR reporting system that health professionals use in current practice. The increasing number of ADR reports received via http://www.bip31.fr underlines the interest of health professionals for this easy and fast ADR reporting tool.
PP181. Comparison of Signal Detection Using Healthcare Database Network versus Spontaneous Reporting System Database: the EU -ADR Experience
G. Trifirò,1 V. Patadia,2 P.M. Coloma,3 M.J. Schuemie,3 R. Gini,4 R. Herings,5 J. Hippisley Cox,6 G. Mazzaglia,7 G. Picelli,8 L. Scotti,9 L. Pedersen, 10 P. Avillach,11 J. van der Lei 3 and M. Sturkenboom 3
1 Department of Clinical and Experimental Medicine and Pharmacology, Section of Pharmacology, University of Messina, Messina, Italy; 2 Astellas Pharmaceuticals, Deerfield, IL, USA; 3 Department of Medical Informatics, Erasmus Medical Center, Rotterdam, The Netherlands; 4 Agenzia Regionale di Sanità della Toscana, Florence, Italy; 5 PHARMO Institute, Utrecht, The Netherlands; 6 Division of Primary Care-School of Community Health Sciences, University of Nottingham, UK; 7 Società Italiana di Medicina Generale, Florence, Italy; 8 Pedianet-Società Servizi Telematici SRL, Padova, Italy; 9 Department of Statistics, Università di Milano-Bicocca, Milan, Italy; 10Department of Clinical Epidemiology, Aarhus University Hospital, Aarhus, Denmark; 11LESIM, ISPED, Uni. Bordeaux 2, France
Background: The EU-ADR project aims to exploit different European electronic healthcare records (EHR) databases for drug safety signal detection. Currently, it is unknown what could be the additional value of using EHR databases for signal detection, with respect to traditional pharmacovigilance system.
Objectives: To describe the preliminary results of the comparison of signal detection, as conducted in EU-ADR database network versus US Food and Drug Administration and World Health Organization spontaneous reporting databases.
Methods: EU-ADR data sources consist of eight databases in four countries (Denmark, Italy, Netherlands, and United Kingdom) that are combined through distributed data network.[1] A custom-built software (Jerboa©) elaborates harmonized input data that are produced locally and generates aggregated data which are then stored in a central repository. These data are subsequently analyzed using a variety of signal detection methods adapted to longitudinal data (e.g., Longitudinal Gamma Poisson Shrinker). As potential signals, all drugs that are associated with ten events of interest (bullous eruptions — BE, acute renal failure — ARF, acute myocardial infarction — AMI, anaphylactic shock — AS, rhabdomyolysis — RHABD, upper gastrointestinal bleeding — UGIB, neutropenia — NEUTROP, pancytopenia — PANCYT, acute liver injury — ALI, and cardiac valve fibrosis) have been detected via different data mining techniques in the two systems. The number of drugs that could be investigated and the potential signals detected for each event of interest were then compared between spontaneous reporting systems (SRS) and EU-ADR network.
Results: SRSs could explore, as potential signals, a larger number of drugs for the ten events, in comparison to EU-ADR, particularly for rare events generally thought to be highly drug attributable (i.e. BE: 3393 vs 228). The highest proportion of signals detected in SRSs was found for BE, ARF and AS, while for AMI, ARF, and UGIB in EU-ADR. When restricted to the same set of drugs, overall EU-ADR could identify a larger number of signals than SRSs, while some signals were detected in both systems.
Conclusions: EU-ADR database network may complement traditional pharmacovigilance system, especially for the detection of signals regarding adverse events that are frequent in the general population and are not highly drug attributable.
PP182. Drug Safety Officers and Yellow Boxes: New Developments in Reporting Adverse Drug Reactions and Medication Errors in Hospitals
G. Shalviri,1 K. Gholami 2 and M. Fazlollahi 1
1 Iranian Adverse Drug Reaction Monitoring Center, Ministry of Health, Tehran, Iran; 2 Department of Clinical Pharmacy, College of Pharmacy, Tehran University of Medical Sciences, Tehran, Iran
Background: Adverse drug reactions (ADRs) and medication errors (MEs) have been recognized as important problems in hospitals. A large meta-analysis in the US introduced ADRs as reasons for 4.6% of all fatalities in hospitalized patients. Hospital admissions due to ADRs were reported around 10% in some countries.
Objective: To evaluate reasons for under-reporting in hospitals and conduct interventions to improve reporting ADRs and MEs. To evaluate frequency and nature of reported ADRs and MEs from hospitals before and after interventions.
Method: This study was conducted in three different phases. In the phase one, the reasons for under-reporting were evaluated using a questionnaire in 10 different randomly selected hospitals. In the second phase, from January through June 1998, three interventions were performed: First, submitting a guideline to 500 hospitals, in which, hospitals were asked to introduce defined Drug Safety Officer (DSO). Second, conducting 20 workshops for 500 DSOs. Third, installing designed Yellow Boxes in hospitals to facilitate access to the Yellow Cards and easier reporting. In the third phase, we evaluated frequency and nature of reports received from hospitals during two years before and after interventions.
Results: The result of phase one revealed that 24% of responders did not report because they did not know how to report, 21% did not easily access to Yellow Cards. For 13%, the reaction was expected to occur and 10% of them were unsure that the drug caused the reaction. For 8% it did not occur to them. A total of 3363 reports were received from hospitals in a two years period before interventions, which was increased to 5276 reports in a same period after interventions. Definite cases of reported fatal reactions were increased from 7 to 14 cases after interventions. The number of nurses and pharmacists as reporters increased from 2394 to 4424. Serious reports were increased from 735 to 937 cases.
Conclusion: Monitoring hospitals for occurred ADRs and MEs is a matter of importance for a national pharmacovigilance center. Hospitals need strong programs for detecting and reporting drug related problems.
Discussion: Assessing under-reporting in hospitals of our country revealed that lack of knowledge and difficulty in access to yellow cards were two factors involved in under-reporting. Informing hospital staff on safety alerts, helping them to report by employing DSOs and facilitating access to Yellow Cards and submitting forms via Yellow Boxes led to a significant increase in reporting frequency in hospitals.
PP183. Harmonization in Periodic Safety Reporting for Investigational Products: Differences between Current Annual Safety Report and New Development Safety Update Report
H. Tønsberg, S. Blomvik, L. Storm and S. Lindequist Lindeq AS, Pharmacovigilance and Risk Management, Oslo, Norway
Background: The periodic safety reporting for investigational products is harmonized by the ICH E2F Guideline recommended for adoption in the EU, USA and Japan. The Development Safety Update Report (DSUR) will replace the existing Annual Safety Report (ASR) in Europe, mandatory from September 2011. The DSUR guideline, Guidance on the collection, verification and presentation of adverse event/reaction reports arising from clinical trials on medicinal products for human use, also referred to as the CT-3 guideline, is an ICH E2F endorsed presentation of pre-marketing safety including relevant post-marketing data.[1] It deviates significantly from the content of the current guideline for ASR which is only briefly explained in the detailed guidance on the collection, verification and presentation of adverse reaction reports arising from clinical trials on medicinal products for human use.[2] We have scrutinized these guidelines and present the main differences.
Objective/Aim: The purpose of the review is to identify the implications of the change from ASR to DSUR.
Methods: The DSUR guideline was extensively reviewed and compared point to point with the guideline for the ASR. Significant differences in the requirements were identified.
Results/Discussion: The ASR guideline is rather unspecific compared to the structured and more detailed content of the DSUR. The DSUR will result in a more analytical and risk-benefit based approach of safety reporting than the ASR and also considers the efficacy of the investigational drug. The DSUR will also include relevant safety experience gained post-marketing and may overlap with the content of the Periodic Safety Update Report (PSUR). The DSUR may also provide valuable information for the Risk Management Plan (RMP). The DSUR guideline is much more structured compared to the ASR guideline and make less room for individual interpretation and variation in content.
Conclusion: The DSUR has several advantages over the ASR: Less variation in the reporting due to more descriptive and structured guideline, more focus on risk-benefit analysis, enhancing the safety aspects and includes relevant post marketing experience. The requirements to data analysis and presentation in the DSUR will require substantial more cross-functional coordination by pharmacovigilance expertise as well as implementation of new routines.
Influence of Drug/Drug, Drug/Food,Drug/Chemical Interactions in ADR Mechanisms
PP184. Drug-Drug Interactions: The Detection and Negative Clinical Consequences in Hospitalized Patients
C.D. Bucsa, A.M. Farcas, I. Cazacu and M.T. Bojita
Drug Information Research Center “Iuliu Hatieganu” University of Medicine and Pharmacy, Cluj-Napoca, Romania
Objectives: Important percentages (0.6–1%) of all hospital admissions are due to adverse drug reactions (ADRs) caused by drug-drug interactions (DDIs).[1–3] Potential drug-drug interactions (p-DDIs) may lead to drug-drug interactions (DDIs) or not. Clinically significant are the DDIs which can result in changes of therapeutic effect of one of the two drugs or in adverse drug reactions (ADRs). The aim of this study was to asses the potential DDIs as well as the DDIs with clinical negative consequences (ADRs) before and during hospitalization in patients admitted to an internal medicine ward.
Methods: The prospective observational study included 304 patients admitted during 3 months in an internal medicine ward. The patients were interviewed at least twice during the hospitalization, regarding the drugs used and present symptomatology. Other information as medical history, medication used during the hospitalization, laboratory data and the results of other clinical investigations, was collected from the patients’ charts. The potential DDIs were identified using the Thomson Micromedex program. Each patient was monitored in order to detect the clinical consequences of DDIs if present.
Results: Three hundred and four patients were enrolled in this study during 12 weeks. The mean age of the patients was 60.05 years and the median of hospitalization stay was 7 days. The median number of prescribed drugs per patient was 4 at hospital admission and 6 for drugs prescribed during hospitalization. Twelve DDIs led to 15 ADRs out of which 9 ADRs were serious, being the cause of admission or prolongation of hospitalization. Statistic correlation was found between the manifestation of DDIs and the number of medicines taken and the number of diagnostics of the patient, ATC (Anatomic Therapeutic Chemical) B and ATC-C classes of medicines and cardiovascular diseases.
A substantial number of potential drug interactions (1275) were identified in our study and this can be explained by the large number of drugs taken by patients (median number of 4 drugs/patient at hospital admission and 6 during hospitalization). Out of p-DDIs only a small number of DDIs (12) resulted in ADRs. DDIs were predictable from their mechanism of action, hence preventable.
Conclusions: Awareness of the most commonly occurring DDIs should be raised by the utilization of drug-drug interactions guides in the Romanian clinical practice which can help prescribers and pharmacists prevent their negative clinical outcomes.
PP185. Acute Hepatitis Associated with Use of Green Tea and Oral Contraceptives: A Case Report
E. Gallo,1 A. Pugi,1 V. Maggini,1 G. Pieraccini,1 R. Notaro,2 V. Annese,3 A. Mugelli,1 F. Firenzuoli 1 and A. Vannacci 1
1 University of Florence, Department of Pharmacology, CIMMBA, Centre for Integrative Medicine, Florence, Italy; 2 Istituto Toscano Tumori, ITT, Florence, Italy; 3 Gastroenterology Unit at the Careggi University Hospital of Florence, Florence, Italy
The potential health benefits associated with green tea (Camellia sinensis) consumption have been partially attributed to the anti-oxidative properties of polyphenols, particularly to catechins, among which Epigallocatechin-3-gallate(EGCG) is the most effective. Unfortunately, some reports of adverse effects, mainly hepatitis, associated to the consumption of green tea preparations (extract or infusion) have been published.
Case presentation: A 42-year-old woman with jaundice was admitted to the Gastroenterology Unit of Careggi University Hospital of Florence. Laboratory analysis revealed total bilirubin level 31 mg/dL, direct bilirubin 21 mg/dL, aspartate aminotransferase, 1447 U/L; alanine aminotransferase, 1618 U/L and a liver biopsy showed hepatocellular necrosis and mixed inflammatory infiltrate. An extensive diagnostic workup discarded any other known etiology for her liver disease. Viral serology for active hepatitis A,B,C, and extensive toxicology screening were all negative. A detailed history revealed that the patient had been drinking Japanese matcha green tea (micronized water-soluble powder of Camellia sinensis) every other day for 10 days. Green tea was withdrawn and liver functions tests normalized within some months.
Discussion: Although tea beverages have been consumed for almost 50 centuries, the co-assumption of green tea and oral contraceptive needs to be considered potentially hepatotoxic since being involved in some cases of toxic hepatitis. The mechanism of toxicity of green tea is unclear, the possibility of idiosyncratic, or immune-mediated mechanism, was suggested. Animal experiments and clinical trials have shown some evidence of a green tea interaction with CYP3A4, also mediating the oxidative metabolism of the oral contraceptive. A possible explanation may be that green tea (EGCG) inhibits the metabolic degradation via CYP3A4 of oral contraceptives with consequent increased bioavailability and relative toxicity.
This case report could confirm that green tea, even conventional infusions, may induce severe acute mixed liver injury in predisposed individuals. A possible pharmacogenetic predisposition (e.g. green tea/oral contraceptive interaction) as well as possible contaminations during the growth of the leaves or during production of the product were investigated with appropriate techniques. Results of these investigations will be reported in the present communication.
PP186. Herbal Hepatotoxicity: Data from the WHO -UMC Database
K. Ilic,1 M. Petronijevic,2 A. Suzuki 3 and M. Blagojevic 1
1 School of Pharmacy, Department of Pharmacology, Belgrade, Republic of Serbia; 2 Medicines and Medical Devices Agency of Serbia, Belgrade, Republic of Serbia; 3 Gastroenterology, Duke University, Durham, NC, USA
Objectives: Besides drugs, herbal products (HP) and dietary supplements have also been reported for hepatotoxicity.[1,2] HP are not subject to rigorous regulatory procedures and in general, patients perceive them as safe and use widely for self-medication, often in combination with drugs and/or in concomitant diseases. Spontaneous reporting of adverse drug reactions is of great importance for the identification of unexpected hepatotoxicity. The aim of this study is to identify herbal species the most frequently reported for hepatobilary disorders (HD) and determine phenotypic characteristics and risk factors of herbal hepatotoxicity (HH ).
Methods: The WHO global database (VigiBase™) of individual case safety reports (ICSRs) was screened for all the cases of HD reported in association with use of HP. Search criteria included HD as a system organ class based on the Medical Dictionary for Regulatory Activities (MedDRA), and HP according to the Herbal Anatomical Therapeutic Chemical (HATC) classification. The information retrieved from the VigiBase™ referred to the suspected herb, hepatobiliary adverse reaction (HAR), patient’s age and gender, and reporting country. Variables were examined using descriptive statistics in the SPSS 16 software package.
Results: Out of overall 6.4 million ICSRs contained in VigiBase™, 369 case reports were related to HH. This stands for 7.17% of all herbal reports in VigiBase™. HH reports were submitted from 22 countries for the past 32 years. Germany, United Kingdom and France contributed nearly 60% (33.60%, 14.09%, and 12.20%, respectively), followed by Australia (8.40%) and the USA (8.40%). Eighty three herbal species or their combinations were reported for HD. The most frequently reported were Cimicifuga racemosa (56; 15.18%), Chelidonium majus (49; 13.28%), Hypericum perforatum (29; 7.86%), Piper methysticum (29; 7.86%), and Ginkgo biloba (24; 6.50%). HARs (578) included 36 preferred terms, of which the most commonly reported were hepatitis (138; 37.40%), jaundice (112; 30.35%), and cholestatic hepatitis (45; 12.19%). Among patients reported, females were predominant (258; 69.92%; p< 0.001). The mean age of the patients was 52.8 ± 16.2 years. Females of age group 50–59 counted for the largest portion (81; 21.95%; p< 0.001). Fatal outcome was reported in 12 (3.25%) patients (3 males, 8 females, and one case with unreported gender).
Conclusions: Although reported rarely, numerous herbs were suspected for liver injury with wide range of clinical manifestations. Women were over presented and exhibited worst outcome. Age of 50–59 was over-represented among female HH cases.
PP187. Physicochemical Incompatibility of Injectable Drugs (Assessment of Knowledge Care Professionals)
Y. Khabbal,1 M. Ait El Cadi 2 and Y. Cherrah 2
1 Department of Pharmacology LABM, CHU Hassan II, Fès, Morocco; 2 Laboratory of Pharmacology and Toxicology, Faculty of Medicine and Pharmacy, Rabat, Morocco
Introduction: In the absence of precipitation or formation of a toxic compound, a mixture is called compatible when 90% of the active substance is still available in the mixture at the end of the observation period.
The AIM of this study is to evaluate the knowledge of care professional about physicochemical incompatibility of injectable drugs.
Materials and methods: This is a randomized cross-sectional study done on a homogeneous population of 100 University Hospital of Fez nurse.
A detailed anonymously and an original questionnaire was developed specifically for this study.
The data were based on personal data such as age, gender, diploma, seniority, service, training, and medical data for the assessment of knowledge was based on the compatibility of certain solutes and drugs used in daily practice. In this work, they will be exposed only 0.009 responses on NaCl.
About 20 variables were collected and analyzed and compared between services. The results were analyzed by appropriate statistical tests.
Results: The cisplatin is consistent with the NaCl9% but less than half (39.6%) of people said right on the physicochemical compatibility of this product with saline.
For the 9% NaCl and oxaliplatin, only 25.2% of the population knows the correct answer. For other drug, the results were (table I)
Conclusion: This study is part of an evaluation of the quality of the act and allows the targeting methods of prevention and intervention work to promote safe and effective and quality for patients.
PP188. Early Interaction between Tacrolimus and Rifampin
R. Charfi, I. Salouage, R. Sahnoun, S. Trabelsi, E. Gaies, N. Jebabli, M. Lakhal and A. Klouz
Service de Pharmacologie Clinique — Centre National de Pharmacovigilance de Tunis, Tunis, Tunisia
Introduction: Calcineurin-inhibitor metabolism through the hepatic cytochrome P450 system is influenced by multiple drugs.[1,2] Drug interactions are unavoidable and need to be proactively identified and appropriately managed. In particular, information about the extent, duration, and potency of the rifampin-tacrolimus interaction is limited. We present a case of an early rifampin-tacrolimus interaction in a renal transplant patient.
Case report: We report a case of a 25-year-old man with a kidney transplantation since 2.5 years. The patient was prescribed tacrolimus, cortancyl and mycophenolate mofetil. The tacrolimus blood levels (TBL) were preserved varying between 5.3 and 11.4 ng/mL and there was no need to change the dosage (4 to 6 mg/day). He presented an abdominal pain and the diagnosis of ganglionic tuberculosis was established. So, the patient started four anti-tuberculous drugs including isoniazid, 300 mg/day, rifampin 600 mg/day, ethambutol 900 mg/day and pyrazinamid 3 g/day. One day later, TBL was 2.6 ng/mL under 5 mg/day in spite of tacrolimus regular intake. Nine days later, TBL was 1.6 ng/mg under 7 mg/day. The serum creatinine was normal in each control varying between 93 and 99 micromol/L.
Discussion: In this case-report, the tacrolimus-rifampin interaction occurred just one day after rifampin introduction necessitating early TBL monitoring. This illustrates the potent and rapid effects of rifampin on tacrolimus metabolism. In fact, rifampin induces the hepatic cytochrome P4503A4 system. It may also cause induction of oxidative metabolism mediated by this system in the gut necessitating the use of large doses of tacrolimus.[3] This interaction sometimes results in allograft dysfunction leading to a tenfold increase in the daily dose requirement.[4,5] So, close monitoring of TBL and frequent dose adjustments are required to optimize allograft function. [5] Besides, the literature doesn’t provide any information about eventual tacrolimus interaction with isoniazid, pyrazinamid or ethambutol.[5,6]
PP189. Acute Renal Failure, Consequence of Perindopril and Ketoprofen Therapy: A Case Report
C.D. Bucşa,1 I. Cazacu,1 A.M. Farcaş,1 A. Achimaş 2 and M. Bojita 1
1 School of Pharmacy, “Iuliu Hatieganu” University of Medicine and Pharmacy, Cluj-Napoca, Romania; 2 School of Medicine, “Iuliu Hatieganu” University of Medicine and Pharmacy, Cluj-Napoca, Romania
A lot of medicines have the potential to induce renal toxicity and angiotensin converting enzyme (ACE) inhibitors are among them. Acute renal failure (ARF) is an adverse drug reaction to ACE inhibitors which occur mostly in the presence of some risk factors, such as associating non-steroidal anti-inflammatory drugs (NSAIDs) to ACE inhibitors therapy.
We want to present a case of a 62-year-old woman who is admitted to hospital with urinary tract infection and ARF. The patient describes nausea, loss of appetite, weakness, also presenting dysuria, pollakiuria, olyguria and dehydration at the admission. Serum creatinine is 3.0 mg/dL, serum urea 191 mg/dL and serum potassium 6.8 mEq/L. The patient is also known with arterial hypertension 1st stage, viral hepatitis, spondylarthrosis and thyroid lymph nodes and she is on therapy with perindopril 2=×4 mg/day, ketoprofen 100mg/day, silybinum 3×150 mg/day and a herbal medicine with hepatoprotective properties for 10 month.
Three days after interrupting perindopril therapy and starting iv treatment with glucose 5%, 500 mL and 6 units of insulin three times daily, the patient condition is improving, serum creatinine levels reaching 1.9 mg/dL.
The combination of ACE inhibitors and NSAIDs poses a risk of renal failure and in order to prevent this monitoring the serum creatinine and potassium levels is necessary.
PP190. Interaction between Tacrolimus and Azole Antifugal Drugs
N. Jebabli, I. Salouage, E. Gaïes, S. Trabelsi, R. Charfi, R. Sahnoun, M. Lakhal and A. Klouz
Centre National de Pharmacovigilance, Tunis, Tunisia
Introduction: Tacrolimus is an immunosuppressor indicated in solid organ transplantation. It has a large inter and intra-individual variability, a narrow therapeutic index and is subjected of numerous drug interactions. It is metabolized in enterocytes and liver by CYP3A4. Association to enzymatic inhibitors like azole antifungals increase its blood levels and may increase its toxicity.
In this study, we assessed cases of drug interaction between tacrolimus and azole antifungals.
Material and methods: It consists on a retrospective study (2009–2011), 115 residual plasma concentrations were carrying out by fluorescence polarization immunoassay (FPIA) method. A total of 14 subjects were evaluated, treated by tacrolimus and antifungal drugs.
Results: The average age was 42 years (17 to 54 years) and the sex ratio M/W was 1.8. Tacrolimus was indicated in 11 patient following kidney transplants and in 3 patients following hepatic transplant. Tacrolimus was administered orally at doses of 1–8 mg twice daily. For fungal infections, antifungals drugs were added in these cases. They were treated by fluconazole, and voriconazole.
The use of antifungals drugs in combination with tacrolimus was responsible for an average increase of 172%. Side effects observed in our patients, were liver toxicity, and increase in serum creatinine and hyperglycemia. The cessation of antifungals drugs after stabilisation of plasmatic concentration of tacrolimus was responsible for a decrease of 72%. We clinically observed that multiple adjustments were required for tacrolimus as blood tacrolimus concentrations continued to decrease for several days in the absence of dose changes for antifungal drugs.
Conclusion: The coadministration of azole antifungals and tacrolimus, it is recommended to adjust tacrolimus dosage on the basis of therapeutic tacrolimus blood monitoring in order to maintain tacrolimus concentration in therapeutic range and to avoid adverse toxic effects.
PP190. Interaction between Tacrolimus and Azole Antifugal Drugs
N. Jebabli, I. Salouage, E. Gaïes, S. Trabelsi, R. Charfi, R. Sahnoun, M. Lakhal and A. Klouz
Centre National de Pharmacovigilance, Tunis, Tunisia
Introduction: Tacrolimus is an immunosuppressor indicated in solid organ transplantation. It has a large inter and intra-individual variability, a narrow therapeutic index and is subjected of numerous drug interactions. It is metabolized in enterocytes and liver by CYP3A4. Association to enzymatic inhibitors like azole antifungals increase its blood levels and may increase its toxicity.
In this study, we assessed cases of drug interaction between tacrolimus and azole antifungals.
Material and methods: It consists on a retrospective study (2009–2011), 115 residual plasma concentrations were carrying out by fluorescence polarization immunoassay (FPIA) method. A total of 14 subjects were evaluated, treated by tacrolimus and antifungal drugs.
Results: The average age was 42 years (17 to 54 years) and the sex ratio M/W was 1.8. Tacrolimus was indicated in 11 patient following kidney transplants and in 3 patients following hepatic transplant. Tacrolimus was administered orally at doses of 1–8 mg twice daily. For fungal infections, antifungals drugs were added in these cases. They were treated by fluconazole, and voriconazole.
The use of antifungals drugs in combination with tacrolimus was responsible for an average increase of 172%. Side effects observed in our patients, were liver toxicity, and increase in serum creatinine and hyperglycemia. The cessation of antifungals drugs after stabilisation of plasmatic concentration of tacrolimus was responsible for a decrease of 72%.
We clinically observed that multiple adjustments were required for tacrolimus as blood tacrolimus concentrations continued to decrease for several days in the absence of dose changes for antifungal drugs.
Conclusion: The coadministration of azole antifungals and tacrolimus, it is recommended to adjust tacrolimus dosage on the basis of therapeutic tacrolimus blood monitoring in order to maintain tacrolimus concentration in therapeutic range and to avoid adverse toxic effects.
Other Topics
PP191. ADRs in Elderly Hospitalized Patients
M.L. Ponte,1 G. Keller,2 G. Di Girolamo 2 and W. Adolfo 1
1 Hospital Argerich, Buenos Aires, Argentina; 2 Second Chair of Pharmacology, Buenos Aires University, Argentina
Objectives: Incidence of ADRs in elderly people is really elevated because of increasing consumption of drugs, pharmacokinetics and pharmacodynamics variations. The aim of this study was to determine the incidence of ADRs in elderly hospitalized patients in a tertiary care hospital.
Methods: We performed this study during 36 months (June 2008–May 2011) in a tertiary care hospital (Hospital General de Agudos Dr Cosme Argerich ) in Buenos Aires, Argentina. All hospitalization rooms (450) except the emergency room were included. Naranjo Score was applied to determine the causality of a drug in every adverse medical event and probable and certain ones were included. We considered elderly to patients with 65 years old or more.
Results: In this period we found 782 ADRs in elderly hospitalized patients and this represented 36.95% (CI 95%: ±2.05%) of all ADRs detected (2116). 129 ADRs were serious and there were 74 ADRs — related hospitalization in elderly persons. The average of age was 78.14 years (CI 95%: ±0.80 years); 53.19% (CI 95%: ±3.49%) of ADRs appeared in men and 46.81 (CI 95%: ±3.5 years) in women. Groups of drugs most frequently involved were cardiovascular drugs 299 events (38.23%; CI 95%: ±3.4%), antibiotics 170 events (21.73%; CI 95%: ±2.89%), neuropsychiatric drugs 73 events (9.33%; 95%: ±2.03%), corticosteroids 66 events and NSAIDs 53 events. The systems/organs most frequently involved were endocrinometabolic 316 events (40.40%; CI 95%: ±3.43%), nephrotoxicity 131 (16.75%; CI 95%: ±2.61%), hepatotoxicity 92 (11.76%; CI 95%: ±2.25%). Gastrointestinal bleeding due to NSAIDs and anticoagulants and hyponatremia due to cardiovascular or neuropsychiatric drugs were the most frequent cause of hospitalization.
Conclusions: Near 20% of all ADRs in this group were serious. Unlikely other study,[1] we did not found cardiovascular drugs as drugs frequently involved in hospital admissions. The causes of ADRs — admissions were similar to the findings in other great study.[2] A lot of this ADRs are preventable strengthening clinical and laboratory controls.
PP192. Quinolone-Induced Glucose Homeostasis Impairment
M.L. Ponte,1 H.A. Serra 2 and A. Wachs 1
1 Hospital Argerich, Buenos Aires, Argentina; 2 First Chair of Pharmacology, University of Buenos Aires, Argentina
Objectives: Last years, quinolones have been associated to glucose homeostasis impairment (GHI). Gatifloxacin and moxifloxacin are the two ones most strongly related to this Adverse Drug Reaction (ADR), but there are little wrote involving other quinolones with higher consumption in our country such as ciprofloxacin, levofloxacin or norfloxacin. The aim of this study was to determine the association of this quinolones with GHI.
Methods: This study was performed in a tertiary care hospital (Hospital General de Agudo:s Dr Cosme Argerich ) at Buenos Aires, Argentina, during a period of 36 month (June 2008–May 2011). The causality of a drug in an adverse event was assessed applying the Naranjo Algorithm and we included the certain and probable ones. All hospitalization rooms were included except the emergency room.
Results: 22 events of quinolones — related Glucose Homeostasis Impairment were detected. 12 events were in male (54.54%; CI 95%: ±20.87%) and 10 in female (45.45%; IC 95%: ±20.87%). Average age of patients suffering this ADR was 63.36 years (CI 95%: 55.13, 71.59 years). Almost all ADRs (19) were caused by ciprofloxacin, two by levofloxacin and only one by norfloxacin. Hyperglycemia was the most frequent presentation: 15 events, 68.18% (CI 95%: ±19.46%); hypoglycemia (4 events) and dysglycemia (3 episodes) were less frequent.
Conclusions: We detected several GHI induced by ciprofloxacin, the quinolone most consumed in our hospital. We consider this very important because this antibiotic is frequently prescribed also in diabetic patients. We recommend to strength glucose control in patients receiving this drug in high doses, mainly in diabetic.
PP193. Utilization of Drug Information Services at Komfo Anokye Teaching Hospital, Kumasi, Ghana
K.Appiah 1,2
1 School of Medical Sciences, Kwame Nkrumah University of Science and Technology, Kumasi, Ghana; 2 Drug Information Unit, Komfo Anokye Teaching Hospital, Kumasi, Ghana
The study was carried out to determine whether the drug information unit at Komfo Anokye Teaching Hospital (KATH) in Kumasi, Ghana was utilized. It also assessed the various categories of healthcare professionals and the general public who sought information at the unit and the topics that the services provided covered.
The study was cross-sectional, descriptive and retrospective for the period 1 September to 31 December 2007. It was also nonrandomized, i.e. all query forms for the period under study were included for the data collection. Data was extracted from the query forms and filled on questionnaire forms.
During the period under study, a total number of 155 queries were received and answered of which 93.5% were from KATH Staff. 58.7% of callers were pharmacists, followed by pharmacy technician/ technologist (14.2%), doctors (12.9%), pharmacy intern (7.7%) and nurses (2.6%).
The polyclinic had the highest percentage of callers (36.1 %), followed by O & G (18.7%), medicine and child health (9.0% each), specialist pharmacy (5.8%), surgery (5.2%), oncology and administration (3.9% each).
Majority of the queries centered on therapeutics (70.3%), followed by drug availability (7.7%), pharmacokinetics and pregnancy (5.8%) each. Two modes of contact were generally used to access services at the unit, 74.2% of total number of callers used the telephone whilst the 25.8% walked in.
The KATH’s drug information unit is utilized by healthcare professionals mainly within the hospital, however only few members of the public accessed services at the unit.
The unit was mainly patronized by pharmacy staff particularly pharmacists and then followed by doctors.
Few queries were made by nurses, students, patients and other healthcare professionals.
Most of the queries to the unit fell under therapeutics. However few other queries covered drug availability, pregnancy and lactation and pharmacokinetics.
Telephone and walk in were the most commonly used modes of contact to access information at the unit.
PP194. Novel Algorithms to Identify Substandard Medicinal Products from Individual Case Safety Reports
K. Juhlin,1 G. Khodabakhshi,1 S.N. Pal,2 S. Olsson 1 and G.N. Norén 1
1 The Uppsala Monitoring Centre, Uppsala, Sweden; 2 Quality Assurance and Safety of Medicines, World Health Organization, Geneva, Switzerland
Background: Substandard and poor quality medicinal products pose significant danger to public health.[1–3] Individual case safety reports (ICSRs) are collected globally[4] and sometimes reflect cases of substandard or poor quality medicines, but there is currently no system for detecting these cases from within an ICSR database.
Objectives: To evaluate a novel algorithm for identifying substandard medicinal products in individual case safety reports.
Methods: Reports in the WHO global individual case safety report database, VigiBase, between 2001 and 2010 were studied. 24 MedDRA preferred terms indicative of quality issues were identified. Two filters for identifying medicinal products of substandard quality were developed; one filter identified medicinal products for which the proportion of reports on quality issues was substantially greater than for other medicinal products with the same substance and a second filter identified medicinal products with excess reporting[5] of quality issues during a certain year relative to the database as a whole. Both filters worked on the national level, looking at clusters of reports in a specific country.
Results: 148 726 reports on quality issues from 62 countries were found. 2946 medicinal products were highlighted with excess reporting of quality issues in comparison with other medicinal products of the same substance and 3378 were highlighted with excess reporting on quality issues in specific country-time periods. Several verified quality issues could be detected using the filters, among which a series of reports on a malfunctioning epinephrine autoinjector were identified. A risk communication regarding the autoinjector was issued by the concerned national center in 2008. The methods also highlighted a series of reports regarding a substandard Levothyroxine product, which was replaced from the national market in 2001.
Conclusions: Substandard medicinal products can be detected from reports of suspected adverse drug reactions. The proposed method demonstrates a concept for detecting such reports and manages to find several verified cases of products of insufficient quality. The WHO global database VigiBase, is an excellent resource for finding these reports with reporting rates of quality issues for each medicine over time and across regions.
PP195. Coding Clinical Safety Data into MedDRA: Impact on the Label
C.R. Knight
TranScrip Partners LLP, UK
Introduction: During the last decade there has been an increasing demand towards the outsourcing of clinical studies to Contract Research Organisations (CROs) from both pharmaceutical and biotech companies. The global spending on outsourcing services has been greater than the spending on new drug development and represents approximately one third of the total pharma and biotech R & D spending. The overall CRO revenue figures for 2010 was projected to be in the region of $20 billion.[1]
During the study conduct phase, accurate coding of safety data is essential. The coding terminology MedDRA (Medical dictionary for Regulatory Activities) was officially launched by the International Conference on Harmonisation (ICH) in 1999, to become the standard regulatory coding terminology for coding adverse events reported in clinical studies.[2] Although its use is now well established, the assessment of a CROs experience in coding with MedDRA, (especially adverse event data), should nevertheless still form an integral part of the overall CRO selection process by the study sponsor.
Methods for Assessment: The study sponsor should conduct a risk assessment of the candidate CRO to determine their MedDRA capability and experience. This is best achieved by providing the CRO with a MedDRA evaluation form. The data collected will provide the sponsor with information on key components of the CROs MedDRA capability. In addition, the CRO should be required to provide documented evidence, e.g. copies of SOPs and other relevant documentation to support their responses. The key information that the sponsor needs to consider is described below:
-
• What type of MedDRA licence
-
• Details of the CRO-SOPs/coding guidelines for MedDRA coding activities.
-
• Details of MedDRA training, and level of trainer’s experience with MedDRA
-
• Previous experience of coding in MedDRA
-
• What is the policy of the CRO regarding version changes with MedDRA — how and when are new versions updated
-
• What level of coding status reports can the CRO provide to the sponsor, and what frequency?
Of key importance in the overall evaluation is the in-house experience with MedDRA coding, and the level of training that coders have received.
Conclusion: When considering the selection of a CRO, expertise in coding clinical data into terminologies, such as MedDRA should be a key decision factor in the CRO selection process. Poorly coded clinical safety data, will inevitably impact on the product label.
PP196. Continuation Rates, Reasons for Removal and Safety of the Levonorgestrel Intrauterine Device in New Zealand Adolescents: A Nationwide Cohort Study
H. Paterson,1 M. Harrison Woolrych 2 and J. Ashton 2
1 Dunedin School of Medicine, Department of Women’s and Children’s Health, University of Otago, Dunedin, New Zealand; 2 Intensive Monitoring Programme (IMMP), Department of Preventive and Social Medicine, University of Otago, Dunedin, New Zealand
Background: There is increasing literature suggesting intrauterine devices are suitable for use in adolescents.[1] However, there remains a paucity of data on use of the levonorgestrel intrauterine device (LNG-IUD) in adolescents and such information is needed to enable adequate counselling of these young women.[2]
Aim: To establish long term continuation rates in a population of adolescent LNG-IUD users, to identify reasons for removal and other adverse events associated with its use.
Methods: A nationwide cohort of New Zealand adolescents using the LNG-IUD was established by the Intensive Medicines Monitoring Programme (IMMP) which undertakes Prescription Event Monitoring studies of selected medicines and IUDs.[3,4] Follow-up of the cohort was undertaken by questionnaires to the patient’s practitioner; record linkage to the New Zealand Health Information Service datasets and by assessment of spontaneous reports submitted to the IMMP. Returned information was used to determine the LNG-IUD ‘end-date’ (defined as the date device removed or reported to remain in-situ) where possible, reasons for IUD removal and identify other adverse events in this population.
Results: The cohort for this study included 175 adolescents under age 20 at the time of IUD insertion, between 1998 and 2007. End dates were established for 111 (63%) women in the cohort. In 86 (77.5%) of these women the device had been removed and for 25 (22.5%) the device was recorded as in-situ at the end-date. Continuation rates of the LNG-IUD in these 111 adolescents were 82% at 1 year (95% CI 0.73, 0.88), 60% at 3 years (95% CI 0.50, 0.69) and 32% at 5 years (95% CI 0.23, 0.42). There were 23 devices reported as being in-situ for greater than 5 years.
Reasons for LNG-IUD removal included: 10 of 86 devices removed for planned conception; 28 had a replacement device, 13 devices were expelled, 17 removed for adverse events and 19 recorded other or unknown reasons for removal. The 17 adverse events leading to removal were: metrorraghia (5), pelvic/lower abdominal pain (6), pain and vaginal bleeding (4), labile mood (1) and suspected PID (1) subsequently diagnosed as gastritis. There were no reported unintended pregnancies in this cohort.
Conclusion: This nationwide cohort of adolescent LNG-IUD users is the largest reported in the literature to date. Continuation, expulsion and removal rates in this cohort were similar to those reported for adult populations,[5,6] which supports use of this device in young women.
PP197. Pharmacovigilance and ADRs Reporting Knowledge among Iranian Healthcare Professionals
K. Bayati, F. Yalchi, P. Hafez Taghva and H. Faegh
Iran najo Co. No. 153, West Hoveiseh, Sabounchi St, Shahid Beheshti Ave, Tehran, Iran
Objectives: In helping to collect data, Healthcare professionals especially physicians and pharmacies have a very crucial role in Pharmacovigilance system, as in spontaneous reporting (known as yellow card). In this article, collect and gather more information about pharmacovigilance knowledge among Healthcare professionals who attended in 22ed Internal Medicine Congress in Tehran.
Methods: Distributing a questionnaire which contains 9 questions about Pharmacovigilance, among volunteer physicians and pharmacies. Questions, in this survey are designed to divided to three parts as capability to report (q: 1, 3, 6 and 7), reasons for under-reporting (q: 8) and knowledge of pharmacovigilance (q: 2, 4, 5 and 9).
Results: Unfortunately, survey response rate was below 21%. Pharmacovigilance is a new science, in 2004, WHO defined more, therefore only a few physicians know about it, in our survey, only 42 of 200 HCPs have returned questionnaire to us. The questionnaire designed in three parts:
Part one related to reporting knowledge about adverse events: in this part, just 24% of responders have yellow card in their office, 67% of them believe that in any doubts in causality assessment, it should be reported, 95% of them believe that they need more education in reporting ADRs and only 29% of them mention; for reporting ADRs, reporter identification is necessary.
Part two relate to pharmacovigilance knowledge which is in question 2, 4, 5, and 6: only 6% know that maximum population who attend in clinical phases in pre-approval trials for any drug in U.S. A or Europe is below 5000 persons, among responders, respectively 40%, 60%, 69%, 55% of them mention nursing mothers, pregnant women, elder patients and children are recognized high risk population in pharmacovigilance, respectively %45, %64, %24, %21, %40, %38, %33 of them answer death, life threatening, hospitalization, prolongation of hospitalization, incapacity, congenital anomaly and medically significant, is a serious adverse event, %43, %38, %45, %21, %21 of them answer abuse, misuse, poisoning, inefficiency, medication error and transferring an agent by drug, respectively, should be reported.
Part three related to causes of under reporting which are in question 8: the percent of ignorance, diffidence, fear, lethargy, ambition and guilty were respectively %38, %10, %12, %43, %17, %0, and %10.
Conclusions: being a new science, pharmacovigilance need more education, Obviously HCPs are in priority of learning to gather more data, as per results fundamental of education are based on recognizing ADRs, How to report ADRs and defining population at risk.
PP198. Statin Therapy and Fever in Cardiac Outpatients of Penang General Hospital of Malaysia
H.A. Abdulrazzaq,1 S. Syed Sulaiman,1 Y.W. Kassab 1 and O. Ismail 2
1 Deaprtment of Clinical Pharmacy, Pharmacy School, USM, Malaysia; 2 Department of Cardiology, Penang Hospital, Pulau Pinang, Malaysia
Background: Statin is the drug of choice for dyslipidemia and prophylaxis for other cardiovascular diseases like angina, myocardial infarction, and other mortalities.[1,2] More than half of cardiac patients in this world use statin,[3] and more than 90% of cardiac patients in Malaysia use statin.[4] Thus, high incidence of adverse drug reactions (ADRs) found during therapy. Depending on previous studies and reports fever is one of common adverse reactions found in cardiac patients.[5]
Objectives: Are to determine the incidence of fever induced by statin and predict the factors contributed to increase its incidence.
Method: Cross-sectional study conducted for 500 cardiac outpatients in Penang General Hospital of Malaysia. Validated questionnaire used to determine fever based on patients complains continuously during therapy. Approval got from Clinical Research Committee (CRC) of Hospital. The severity of fever classified to mild, moderate and severe. The other information such as demographic data, dyslipidemia type, statin information and concurrent diseases and medication collected from patients progress file. SPSS version 18 used to analyze the data, chi-square, logistic regression and odd ratio (OR) used to determine the factors contributed to increase the incidence of fever. All results with p value less than 0.05 considered significant.
Results: Majority of patients were male (70%), Chinese (37.6%), non smoker (88%), non alcohol consumer (91%). Geriatric patients were 30%, patients use statin more than 5 years were 17.6%, lovastatin (81%) and primary dyslipidemia were 51.5%. The incidence of fever found 20.8% ( 104 patients). The incidence of severity of fever was; mild 16.6% (83 patients), moderate 3.8% (19 patients), and severe 0.4% (2 patients). Consuming of alcohol is the only contributing factor which increase the incidence of fever (38.3%, p value = 0.044, OR = 1.66, CI =1.014, 2.714). However, no contribution for the other demographic data, dyslipidemia type, duration of statin use, type and dose of statin, concurrent disease and medications.
Conclusion: High incidence with severe cases found in this study depending on patients’ reporting. Stopping consumption of alcohol is required to reduce the incidence of alcohol in cardiac patients who are on chronic use of statin therapy.
PP199. Adverse Drug Reactions to Anti-Asthmatics in Patients with Bronchial Asthma
C. Kim,1 J. Cho,1 E. Jung 2 and H. Lee 3
1 Department of Internal Medicine, Inha University Hospital, Incheon, Korea; 2 Inha Regional Pharmacovigilance Center, Inha University Hospital, Incheon, Korea; 3 Department of Pharmacy, Inha University Hospital, Incheon, Korea
Objectives: The number of self-reported adverse drug reactions (ADRs) has been rapidly increased with the active pharmacovigilance activities in Korea. However, there has been few data on ADRs to anti-asthmatics in Korea. This study was conducted to investigate the clinical characteristics of ADRs to anti-asthmatics in adult patients with bronchial asthma.
Methods: ADRs to anti-asthmatics reported to Regional Pharmacovigilance Center of Inha University Hospital by two physicians were collected from Jan 2011 to April 2011. Causality assessment of adverse events was performed by using WHO-UMC criteria and Naranjo’s probability scale. Clinical information was additionally collected from electronic medical records.
Results: Twenty five ADRs to anti-asthmatics were reported in 19 (male 5, female 14) out of 228 patients with asthma. The most common offending anti-asthmatics were inhaled glucocorticoids combined with inhaled long-acting beta agonist (LABA) (12 of 19 subjects, 63.2%), theobromine (10.5%), oral LABA (10.5%), doxofylline (5.3%), acetylcysteine (5.3%), and montelukast (5.3%). Severity of ADRs was mild in most patients (13 of 19, 68.5%), and no severe ADR was detected. By frequency, oral LABA was the commonest drug associated with ADRs (2 in 17 prescription, 11.8%). ADR frequency was not different according to asthma control status. But ADRs to simultaneously prescribed drugs were more frequently detected in patients with combined upper airway diseases (ADRs to antihistamines) or patients with combined infection (ADRs to anti-infective drugs, mucolytics, oral LABA, or to SABA), or older patients with asthma.
Conclusions: Although the severity is usually mild, ADRs are relatively common in patients with bronchial asthma. Physician should monitor ADRs to anti-asthmatics or related drugs in patients with asthma, especially in older patients or in patients with multiple drug treatment for combined conditions.
PP200. Prescription Trends for Antipsychotics in Patients with Dementia in the UK
K. Donegan, C. Davies, S. Seabroke and J. Wong
VRMM, Medicines and Healthcare products Regulatory Agency, UK
Background: Antipsychotic drugs are, in general, not indicated for the treatment of dementia-related behavioural disturbances as they appear to have only a limited positive effect and have been associated with an increased risk of cerebrovascular events and mortality.[1] One exception to this is risperidone which is licensed for six weeks treatment of persistent aggression in moderate to severe Alzheimer’s dementia. In 2009, the UK Department of Health[2] concluded that the use of anti-psychotics in dementia patients in the UK was too high. Consequently, the target was set to reduce usage by two-thirds.
Objectives: To examine trends, by age, region, and drug, in anti-psychotic prescribing in dementia patients in UK general practice since the first warnings on use in 2004 and to evaluate the progress made in meeting the target. This study additionally aims to examine the use of risperidone and whether this is in-line with the licensed indication.
Methods: Antipsychotic prescriptions 2004–2011 in patients with dementia were obtained from the General Practice Research Database. Prevalent and incident usage were calculated on a quarterly basis and sensitivity analyses accounting for changes in dementia diagnosis were conducted.
Results: 57 595 dementia patients were identified. Aside from an initial decline in 2004, usage first started to decrease, in all ages and regions, in 2008. The incidence of new users of antipsychotics also decreased. However, usage has not yet decreased by the target two-thirds with prevalent use dropping from 22.1% at the end of 2008, to 19.9% at the end of 2009, and to 16.4% by March 2011. The use of the most common atypical antipsychotic, quetiapine, which increased before 2008, has decreased since 2009. Conversely, there has been an increase in risperidone use since its authorisation for dementia in 2008 although it appears that it is being used for longer than the licensed duration.
Conclusions: The apparent downward trend in the prescribing of antipsychotics for people with dementia is encouraging in light of the known risks. However, it has not yet reduced by the targeted amount. Additionally, an increasing incidence of dementia, likely to consist of more mild diagnoses, means that the actual reduction may be lower than observed. National Institute for Health and Clinical Excellence guidance states that while antipsychotics should not be first-line treatment they may be of use in a small proportion of patients in limited circumstances and so further work is needed to identify trends allowing for potentially appropriate use.
PP201. Valproic Acid-Induced Hyperammonemic Encephalopathy at Subtherapeutic Concentration
M.L. Ponte, C. Armenteros, V. Torres, N. Maddalena, S. Sosa and G. Faracce
Hospital General de Agudo:s Dr Cosme Argeric:h , Buenos Aires, Argentina
Introduction: Valproic acid can induce central nervous system toxicity, generally in a dose dependent way and infrequently can cause Hyperammonemic encephalopathy, a serious complication. Normally HAE occurs at therapeutic or supratherapeutic concentrations of valproic acid in patients with hepatopathy.[1,2] The aim of this case report is to comment a case of valproic-induced HAE at subtherapeutic concentration.
Case Report: 22-year-old female with congenital cognitive impairment and history of epilepsy treated with phenytoin and recently added valproic acid was admitted to our hospital with increased seizure activity. The patient had laboratory test showing malnutrition. At this moment urinary tract infection was detected and started antibiotics but few days after lethargy appeared and frequency of epileptic crisis increased. Plasmatic concentration of valproic acid was in infratherapeutic range and ammonia level was three times the upper normal limit. Valproic acid was withdrawn with improvement of the general and mental status. Phenobarbital and lamotrigine were added controlling epileptic crisis.
Discussion: Valproic-induced hyperammonemic encephalopathy is a rare condition that occurs most commonly in patients with liver insufficiency. [1,2] Half of the cases can be asymptomatic but in symptomatic patients plasma concentrations of valproic acid are therapeutic or supratherapeutic. There are no reports of this adverse drug reaction at subtherapeutic plasma concentration. We think this occurred because of malnutrition and infections can impair urea cycle and potentiate valproic acid toxicity blocking the urea cycle.
PP202. Healthcare Professionals’ Knowledge About Pharmaceutical Excipients: Pilot Study
H.A. Abdulrazzaq,1 S. Syed Sulaiman,1 M.F. Najjar,2 Y.W. Kassab 1 and O. Ismail 3
1 Deaprtment of Clinical Pharmacy, Pharmacy School, USM, Malaysia; 2 King Abdullah International Medical Research Center, The Kingdom of Saudi Arabia; 3 Department of Cardiology, Penang Hospital, Pulau Pinang, Malaysia
Background: There is incorrect idea by majority of people about the pharmaceutical excipients, as safe or inert materials which may cause later hazards and health problems.[1] Many of physicians, pharmacists and manufacturers believed that excipients are safe to use by patients and they are harmless. This because lack in knowledge and few conducted clinical studies about their role in increase the incidence of adverse drug reactions (ADRs) and interactions.[2,3] Most of healthcare professionals believed that ADRs induced only by active ingredients, neglecting the hidden hazards caused by excipients.[4] It is needed to develop ADR surveillance system to report and detect the ADRs of pharmaceutical excipients, to reduce incidence of ADRs and other mortalities caused by excipients.[5]
Objectives: are to evaluate the knowledge of healthcare professionals about the excipients of medications and their effects.
Method: Cross-sectional and pilot study conducted for healthcare professionals worked in University Science Malaysia. Validated and reliable (a = 0.885) questionnaire used in conducting of this study. The content of this questionnaire were reviewed by three professionals in Industrial technology and quality control. The style of questions depended on the correct, wrong, and do not know. One point was given to correct answer, while zero given to wrong or do not know answers. The information of this questionnaire based on previous reports, books and studies. Four domains included in this questionnaire are; general information of pharmaceutical excipients, toxicity and mortality, ADRs, and excipients’ interactions. Knowledge score is calculated and categorized into good and poor knowledge for all participants.
Results: There were 35 respondents voluntarily participated in this study, 54% were males, mean age 35.17±7.85 years, 63% are foreigners, 71.4% pharmacists, 60% worked as academics in USM and the mean of their experience was 8.39 ±5.28 years. The percentage of overall knowledge about the pharmaceutical excipients was 35.40%. Unfortunately healthcare professionals had also 17% wrong answers and 47.60% without knowledge. In term of knowledge’s domains about excipients, the percentages of respondents who could get the correct answers for the general Information, ADRs, contraindication and toxicity, and excipients’ interactions were 50.36%, 30.16%, 38.78% and 16%, respectively.
Conclusion: healthcare professionals had low overall knowledge of pharmaceutical excipients. Also, fair knowledge in general information of excipients, but unacceptable knowledge toward ADRs, toxicity and interactions. However, this is only pilot study to do intervention study to improve the knowledge of healthcare professionals.
PP203. Drug Use and Spontaneous Abortion: A Case-Control Study
D. Abadie,1 C. Hurault Delarue,1 C. Damase Michel,1 T. Vial,2 J. Montastruc 1 and I. Lacroix 1
1 Service de Pharmacologie Clinique, Centre Midi-Pyrénées de Pharmacovigilance, de Pharmaco-épidémiologie et d’Information sur le Médicament, Inserm UMR 1027, CHU de Toulouse, Faculté de Médecine, Université de Toulouse, Toulouse, France; 2 Centre de Pharmacovigilance et d’Information sur le Médicament de Lyon, CHU de Lyon, Lyon, France
Introduction: Few studies have been conducted to investigate drug effects on miscarriage risk. The objective of the present study was to evaluate the association between first trimester drug exposure and miscarriage occurrence.
Methods: We performed a nested case-control study using data from Terappel, a French database which records since 1984 requests from health professionals to Regional Centers of Pharmacovigilance. Terappel contains data about women exposed to drugs during pregnancy and registers corresponding pregnancy outcomes. Cases were women who had a clinically detected miscarriage (before the 22nd week of amenorrhea) and controls were women who gave birth to a child. Drug uses since the beginning of pregnancy were compared between cases and controls during the same period of pregnancy. Odds ratios were calculated by means of a multivariate logistic regression analysis adjusted for age.
Results: 838 cases and 4508 controls were identified in the database. Miscarriage was reported on average at 9.4 (±3.0) weeks of amenorrhea. Cases were older than controls [32.4 (±6.1) vs 30.6 (±5.4) years; p < 0.0001]. There was no difference in the average number of different drugs taken by women during the study period between cases [2.3 (±1.8)] and controls [2.2 (±1.9)]. Cases were more exposed than controls to “tricyclic antidepressants” (ATC code: N06AA) [2.2% vs 0.9%; OR = 2.1 (CI 95% 1.4, 3.2)], “anti-protozoals” (ATC code: P01) [2.1% vs 1.4%; OR= 1.6 (CI 95% 1.0, 2.4)] and “centrally acting anti-obesity products” [1.2% vs 0.3%; OR=3.4 (CI 95% 1.9, 6.2)]. Conversely, controls were more exposed than cases to H1 antihistamines [2.5% vs 1.6%; OR = 0.6 (CI 95% 0.4, 0.9)].
Discussion: The positive association between miscarriage risk and “tricyclic antidepressants”, “anti-protozoals” and “centrally acting anti-obesity products” exposure could be explained by the fact that the pathologies which these drugs are prescribed for (obesity, depression and infectious diseases) can increase the risk of miscarriage. About the potential protective effect of H1 antihistamines on miscarriage risk, we did not locate any pharmacoepidemiological studies reporting such a result. However, a physio-pathological mechanism could be hypothesized. Indeed, animal and clinical experimental studies have suggested links between hyper-histaminemia and gestational complications such as miscarriage, which could be explained by the contractile effect of histamine on the uterine musculature.[1]
Conclusion: This study highlights some potential associations between first trimester drug exposure and risk of miscarriage. Further studies have to be carried out to further investigate these findings.
PP204. Role of Drugs Modifying the Intra-Renal Haemodynamic in Intravenous Immunoglobulin-Induced Renal Failure: A Case-Control Study
G. Moulis, L. Sailler, A. Sommet and M. Lapeyre Mestre, J. Montastruc and Centres Régionaux De Pharmacovigilance
Department of Clinical Pharmacology, Toulouse Teaching Hospital, Toulouse, France; Pharmacoepidemiology Unit, INSERM U1027, Toulouse, France; University of Toulouse, Toulouse, France
Objectives: Risk factors for intravenous immunoglobulin-induced renal failure (IVIg-RF) were suspected from case-series studies.[1–3] This study was aimed at quantifying the risk of IVIg-RF associated with exposure to drugs that modify intra-renal hemodynamics.
Methods: We conducted a case-control study in the French Pharmacovigilance Database (FPVD). Adult IVIg-RF cases registered in the FPVD from 1996 to 2009 were reviewed. Acute IVIg-RF was defined as a calculated creatinine clearance >60 mL/min (MDRDs) and, in the event of chronic kidney disease, (i) a more than 50% increase of serum creatinine, (ii) oligo-anuria, or (iii) requirement to dialysis. Controls were patients included in the FPVD for another IVIg adverse effect. Controls were matched for sucrose content of the preparation, year of adverse event and age. Predictors of IVIg-RF assessed in conditional logistic regression were: exposure to angiotensin converting enzyme inhibitors (ACE-I), angiotensin receptor antagonists (ARA), diuretics, age, gender and weight, the IVIg delivered dose and infusion duration, a chronic kidney disease, hypertension and diabetes mellitus.
Results: Seventy-one cases were matched to 71 controls. Mean age in the IVIg-RF group was 71 ± 12 years and 73% of the patients were male. Time to onset from the first day of infusion was 3.8 ±1.2 days, peak serum creatinine was 5.6 ± 2.7 mg/dL, 66% of the patients were oligo-anuric and 49% required transient hemodialysis. IVIg were sucrose-containing in all but one case. There was no significant difference neither in weight of the patients nor in dose and duration of IVIg therapy between cases and controls. Cases had more frequently arterial hypertension (52% vs 27%, p<0.4), diabetes mellitus (33% vs 6.4%, p <0.01) and chronic renal failure (41% vs 7.0%, p < 0.01). Many patients were exposed to drugs modifying the intra-renal hemodynamic: ACE-I or ARA, 41% versus 15% (p = 0.01); diuretics, 51% versus 18% (p = 0.01), mainly loop diuretics; non-steroidal anti-inflammatory drugs, 2.8% versus 1.4% (p= 1.0). In the final multivariate model, exposure to ACE-I and/or ARA was the sole independent predictor associated with IVIg-RF (odds ratio, 7.9, 95% CI [1.3,49.2]). There was an interaction between “diabetes mellitus” and “chronic kidney disease” (p < 0.001), both being strong risk factors in univariate models (odds ratio: 7.7 [2.3–25.5] and 13.0 [3.1–54.7], respectively). Chronic hypertension was a risk factor for hemodialysis. Because of the matching, we could not investigate the effect of age and non-sucrose-containing preparations.
Conclusions: Temporary interruption of ACE-I and ARA may be considered at the time of IVIg infusion.
PP205. Sparse Batch Number Reporting for Biologicals in FDA’s Adverse Event Reporting System (AERS)
N.S. Vermeer,1 S.M. Straus,2 A.K. Mantel Teeuwisse,3 T.C. Egberts,3 H.G. Leufkens 1 and M.L. De Bruin 1
1 Utrecht Institute for Pharmaceutical Sciences (UIPS), Division of Pharmacoepidemiology and Clinical Pharmacology, Utrecht University, Utrecht, The Netherlands; Medicines Evaluation Board, The Hague, The Netherlands; 2 Medicines Evaluation Board, The Hague, The Netherlands; Department of Medical Informatics, Erasmus Medical Center, Rotterdam, The Netherlands; 3 Utrecht Institute for Pharmaceutical Sciences (UIPS), Division of Pharmacoepidemiology and Clinical Pharmacology, Utrecht University, Utrecht, The Netherlands
Background: Pharmacovigilance and risk management of biologicals is faced by several challenges, due to their specific characteristics as compared to traditional small molecule drugs.[1] Minor modifications in the formulation and production process of biologicals may have profound effects on the safety profile, which may lead to product and even batch specific adverse events. Exemplary was the sudden rise in incidence of pure red cell aplasia associated with a formulation change of a specific brand of epoetin-α.[2]
Early detection of any product and batch related problems depends on accurate recording and subsequent reporting of batch numbers for the product responsible for the adverse event. Availability of batch numbers may in addition facilitate to distinguish between different biological products, which contain the same international nonproprietary name (INN).[3]
Aim: To review the availability of batch numbers for biologicals in FDA’s Adverse Event Reporting System (AERS).
Methods: A cross-sectional study was conducted in AERS, including all suspected AEs reported in 2010. Duplicate reports were excluded. Drugs were classified into three categories: small-molecule drugs, biologicals, and unknown. Biologicals were defined as pharmaceutical products consisting of (glyco)proteins and/or nucleic acids.[4] The category unknown was assigned for verbatim data which was not reducible to a unique INN (n = 63760).
Batch number reporting rates were calculated by drug categories, and were further stratified by reporter type and drug role code category (primary suspect, secondary suspect and concomitant). Significance was tested using chi-square statistics.
Results: A total of 545436 reports, containing 1815 365 drugs were included. Overall, for 15.9% of the biologicals a batch number was reported, compared to 3.1% of the small molecule drugs (p<0.001).Differences in reporting of batch numbers were noted for different reporter types and for different drug role code categories (table I). For biologicals, 25.6% of the pharmacist reported a batch number, compared to 17.0% of the physicians (p< 0.001).
Conclusion: Despite awareness that batch number reporting is important, batch number reporting for biologicals remained sparse. Efforts should be undertaken to communicate the importance and/or to improve feasibility of batch number recording for biologicals.
PP206. Internet and Social Media Impacts on Turkish Healthcare Professionals’ Reaching Health and Drug Side Effect-Related Information
Y. Arıkan and T. Benker
Clinical Quality and Drug Safety Department, Boehringer Ingelheim, Turkey
Objectives: Health-related activities stand to benefit enormously from the Internet. The Internet is beginning to influence the health sector by improving access to health information.[1] However, the influence of internet and social media on Turkish Health Care Professionals is not documented. This study was conducted to estimate the internet and social media use of Turkish Health Care Professionals for professional purpose. This research has aimed to determine physicians internet and social media usage habits in purpose of health and drug safety related information.
Methods: This study was conducted by GfK Turkey. This study is based on a 15-minute, quantitative-administered CATI questionnaire. Data have been collected in accordance with the ESOMAR rules and regulations and GAB procedures for this study from 7th April to 10th May 2011. The physicians were selected randomly based on specialty and region. A total of 604 respondents representing 9 specialties from 6 regions of Turkey have been interviewed. T-Test is used for means, and colon test is used for statistical analysis.
Results: Approximately 95% of physicians are active internet-users. Physicians stated that they spend approximately 47% of their time on internet for scientific purposes followed by e-mail communication (24%), social networking (10%). To get info on side effects/ contraindications of drugs is the purpose of 12% of professional internet use. Websites found from Google (26%) and Pub Med (10%) are the main internet sites searched for safety information of drugs.
When there is a side effect in their patients, 27.5% of physicians notify pharmaceutical companies or/and Ministry of Health Pharmacovigilance. The internet adverse effect notification system of T.C. Ministry of Health Turkey Pharmacovigilance Center is not known by 78% of 604 physicians.
The ratio of internet users following social networking sites is 46.9%. Fifteen percent of the social network followers provide medical advice to someone through social network such as information about the disease/indication area suggestion of a medication and side effects of a drug.
Conclusions: The adverse event reporting and knowledge of reporting methods among Turkish physicians are reportedly low. Awareness programs on drug safety and notification system of T.C. Ministry of Health Turkey Pharmacovigilance Center are needed. Our study demonstrated that physicians are likely to share medical information over internet which can also be accessed by non healthcare providers. As patients frequently refer to internet for medical advice,[2] a controlled environment will provide increased patient safety and better patient — physicians’ interactions.
PP207. Turkish Patients’ Use of Internet and Social Media for Healthcare and Drug Side Effect Information
T. Benker and Y. Arıkan
Clinical Quality and Drug Safety Department, Boehringer Ingelheim, Turkey
Objectives: The internet is increasingly apartofdailylifeby facilitating networking opportunities and offering ways to associate with others who have similar interests, values, or goals.[1] The objective of this study is to show internet usage frequency and Turkish patients’ internet usage habits for obtaining health and drug safety related information.
Methods: Nielsen Monthly Consumer Omnibus was used for the study. Face to face interviewing technique was used for the survey. Target group of the study was women and men who are between the ages 16 and 64 from all SES groups. 1204 respondents attended to the survey. The fieldwork of the study was conducted in April 2011 in urban residential areas of 13 cities. T-Test is used for means. (95% confidence level).
Results: The research showed that approximately 38% of respondents are internet users.
The respondents are asked to state the major sources for health care information. Vast majority (81%) state “Physician” as the most preferred information source. It is closely followed by “Pharmacy” (11%). “Relatives and Friends” (4%), “TV” and “Internet” are other sources of information about health issues.
The ratio of respondents referring to patient information leaflets when they face a side effect with the drug is 72%. In addition, just above half of the patients ask to their physician or pharmacist (54%, 45%). Searching on Internet is not on the top of the list when side effects are faced although Internet was stated as a source for health issues (41%).
More than 1/3 of the respondents use internet everyday, while there is another 1/3 never using internet. Almost all of internet users are also social network followers (97%). Social network followers mentioned that they either had given (32%) or taken (40%) some advice about specialties to visit, treatments, drugs or side effects via social network sites.
Retrieving information on diseases (42%) and drug efficacy (40%) are major purpose of internet use for health related issues.
Conclusions: Physicians and pharmacists are still the major source of health care information among Turkish patients but the importance and the frequency of internet may increase in near future parallel to internet usage.
Lay people exchange opinion on health related issues and gives advices. These activities increase the risk of disinformation and misleading. A controlled environment which physicians also take part, can decrease the risk and improve the quality of information.[2]
PP208. Screening Local Medical Literature, not Accessible through Digital Databases, is Feasible and Highly Valuable in the Mining of Safety Information
N. Tsiakkas, K. Paschou, K. Krousti, G. Kolangi and Z. Athanassiou
Medwork Pharma Research and Consulting, Chiou 5, Argiroupoli, Athens, Greece
A significant amount of case reports and adverse events is published in journals and comes to the attention of pharmacovigilance officers through literature searches in free digital databases. Safety information drawn from literature screening has become a significant tool for MAHs and regulatory authorities. Nevertheless, there are still several medical journals in non-English speaking countries that are not included in Pubmed or other digital databases. HCPs from these countries tend to publish their work, including often case reports and adverse events, in local journals and congresses.
Since local literature is usually not accessible through digital databases, an alternative methodology needs to be established for the screening of local literature and the identification of safety information. We have established a methodology for local literature screening in Greece. Additionally, we have developed an automated system to record and handle identified adverse events.
In the absence of a generally accepted database for local medical journals, the process of selecting eligible journals and abstract books and keeping the selection up-to-date is the first step and also very essential. Upon receipt, publications are reviewed by qualified medical advisors within 5 days and identified AEs are registered in a database. Our software processes the information, identifies concerned MAHs and notifies our personnel about the reports that need to take place.
We have been using this system in Greece for over three years and currently cater 37 MAHs. Numerous reports have been received and handled timely to assure compliance with reporting requirements. Representatively, in 2010, safety information has been gathered for 501 active substances from 96 scientific journals and 55 congress abstract books. This screening yielded 1284 AE reports. Statistical analysis showed that the mean values for AE reporting were 1.93 AEs/journal issue, 6.6 AEs/journal title and 11.7 AEs/abstract book. The 10 active substances with the most AEs were found to be: Dexamethasone (26), Methotrexate (26), Cyclophosphamide (22), H1N1 Vaccine (21), Rituximab (21), Doxorubicin (20), Methylprednisolone (19), Acetylsalicylic acid (17), Ciclosporin (17) and Cisplatin (17). These numbers indicate the impact of AE reporting through publications that are not included in PubMed or Embase and the necessity to perform local literature screening, especially for those countries where spontaneous reporting from HCPs is still disappointingly limited.
From our experience so far, this is a pioneer system for a full literature screening in countries where digital medical databases do not exist.
PP209. Comparative Study of Adverse Drug Reactions Between a Public and a Private Specialist Hospital in Lagos, South West Nigeria
A. Akinyandenu,1 I. Oreagba,1,3 I. Ishola,1 S. Olayemi,1 O. Adedeji,2 M. Adekoya 2 and A. Adewunmi 4
1 Department of Pharmacology, College of Medicine, University of Lagos, Idi-araba, Lagos, Nigeria; 2 Pharmacy Department, Lagos University Teaching Hospital, Idi-araba, Lagos, Nigeria; 3 National Pharmacovigilance Centre, National Agency For Food and Drug Administration and Control, Abuja, Nigeria; 4 Department for Medicine, Lagos University Teaching Hospital, Idi-araba, Lagos, Nigeria
Objectives: To compare the profile of Adverse Drug Reactions (ADRs) between a Private Tertiary Health Institution and a Public Tertiary Health Institution and to compare the role of concomitant medicines in predisposing a patient to ADR’s in both institutions.
Methods: A retrospective study was carried out. Medical records between 2002–2009 were examined for ADRs.
Results: Of 3300 medical records examined, 7% had experienced an ADR. Female patients had an increased incidence rate of 52% compared to male patients (48%).
The profiles of ADRs were comparable between the two hospitals. Generally, the skin (36%) and the central nervous system (26%) were the most implicated systems in this study. Multiple drug therapy as a risk factor was similar in both hospitals with patients on more than three drugs having rates as high as 86% in LUTH and 91% in HSH. The effect of age on ADR occurrence was also similar in both hospitals with most patients being between ages 30–39 years of age (LUTH, 28%; HSH, 45%). The class of drugs with the highest frequency of ADRs was however different in both settings with LUTH having antiretrovirals (54%) as the most frequent cause of ADR while HSH had analgesics (30%). Moderate reactions were the most frequent in LUTH (44%) as against severe (58%) in HSH.
Conclusions: There is no significant difference in the patterns of ADRs occurrence between patients in the public and private tertiary health institutions studied. Multiple drug therapy is a significant risk factor for the occurrence of ADRs in both health institutions.
PP210. Key Elements Contributing to Adverse Drug Interaction Safety Signals
J. Strandell,1 G.N. Norén 1 and S. Hägg 2
1 Uppsala Monitoring Centre, WHO Collaborating Centre for International Drug Monitoring, Uppsala, Sweden; 2 Department of Drug Research/Clinical Pharmacology, Linköping University, Linköping, Sweden
Background: Effective surveillance of adverse drug interactions (drug combinations resulting in an adverse drug reaction (ADR)) in large collections of individual case safety reports (ICSRs) requires both clinical assessment and efficient algorithms. To date, most methods focus on disproportionality analysis, though recent results indicate that much can be gained by looking also at reported clinical and pharmacological information.
Objectives: To identify what reported information may support the identification of drug interaction safety signals, and to what extent this information is available in structured format.
Methods: Altogether, 137 case reports from three published safety signals of suspected adverse drug interaction were re-evaluated. The drug interaction probability scale (DIPS) — an operational algorithm for causality assessment of drug interactions — was used on reports in the WHO Global ICSR Database, VigiBase, and original files from the country of origin. For each DIPS element, the number of times that it was fulfilled was recorded, and the number of times that it was listed at all and in structured format was measured. Explicit notes of suspected drug interaction by the reporter/sender were also measured.
Results: The most frequently fulfilled DIPS elements were: objective evidence of a drug interaction on 79(57%) reports; plausible time to onset on 53(38%) reports; and resolution of the ADR after termination of the drug causing the changed effect on 10(7%) reports. 10 reports (7%) fulfilled both a plausible time to onset and resolution of the ADR upon termination of the drug. Most infrequently fulfilled elements were: exhaustive enough information to exclude alternative causes (0%), altered drug levels detected (1%), altered effect related to dosage change (1%), and positive rechallenge (2%). For two case series there was more information in original files and that the additional information was available in the form of free text. On 47/137(35%) the reporter had noted a suspected drug interaction, and >80% of these were rated as possible or probable according to DIPS. Among cases without notes of suspected interactions 64% were assessed as possible (56 reports) or probable (2 reports).
Conclusions: Plausible time to onset patterns and resolution of the ADR upon withdrawal of the precipitant drug each commonly strengthened the suspected causality of a drug interaction. Particularly strong cases were those containing both these key elements. The fact that some such cases were not explicitly highlighted by the reporter indicates opportunities to automatically identify additional strong cases in first-pass screening for suspected adverse drug interactions.
PP211. Short-Term Impacts of Pharmacovigilance Education on the Pharmacovigilance Knowledge Level of Fifth-Year Medical Students
A.M. Arici,1 A. Gelal,1 Y. Demiral 2 and Y. Tuncok 3
1 Dokuz Eylul University School of Medicine, Department of Medical Pharmacology, Izmir, Turkey; 2 Dokuz Eylul University School of Medicine, Department of Public Health, Izmir, Turkey; 3 Dokuz Eylul University School of Medicine, Department of Medical Pharmacology, Division of Clinical Toxicology, Izmir, Turkey
Objectives: Pharmacovigilance education has been integrated to the curriculum of Dokuz Eylul University School of Medicine for fifth year students since academic year 2008/9. The objectives of the education are to create an awareness on pharmacovigilance and to enhance their knowledge about reporting adverse drug reactions using the spontaneous adverse drug reaction (ADR) reporting form. Therefore, the aim of the present study was to evaluate the short term impacts of pharmacovigilance education on the knowledge about definitions and methods in pharmacovigilance and on awareness about the regulatory aspects of pharmacovigilance.
Methods: A structured, 46-item questionnaire was used to assess the knowledge and to obtain sociodemographic characteristics of the participants. Students completed questionnaires before and immediately after the course. The true answers were graded as one point and false answers were graded as zero point. The maximum possible point was 35. Paired sample t test was used to analyze the differences between before and after teaching assessments by the total points of the medical students. p<0.05 was considered to be statistically significant.
Results: Total number of the students was 140 in the fifth class. Out of 140, 111 students were recruited into the study and 99 completed both of the questionnaires. The mean age of the students was 23.1±0.09. Male/female ratio was 1.06. The knowledge level of the medical students were significantly increased after education (27±0.3 vs 31.4±0.3, p< 0.0001). The rate of correct answers about the definitions of the pharmacovigilance, criteria about who and how to report ADRs also increased significantly after the education (7.5±0.1 vs 8.3±0.1, p<0.0001; 4.9±0.1 vs 6.3±0.1, p<0.0001; 5.0-0.1 vs 6.2±0.1, p< 0.0001; respectively).
Conclusions: Our education increased the knowledge on pharmacovigilance among fifth year medical students. We hope the education will make them aware of their responsibility to report ADRs in their professional lives. So, further research should investigate whether our training has sustained long-term effects on the medical students’ awareness on pharmacovigilance.
PP212. Validating a Trigger Tool to Identify Adverse Drug Events Using Electronic Prescription Records: An Example Using Two Triggers in a UK Setting
U. Nwulu,1 R. Odesanya,2 S.E. McDowell 1 and J.J. Coleman 3
1 University Hospitals Birmingham NHS Foundation Trust, Edgbaston, Birmingham, UK; 2 College of Medical and Dental Sciences, University of Birmingham, Birmingham, UK; 3 University Hospitals Birmingham NHS Foundation Trust, Edgbaston, Birmingham, UK; College of Medical and Dental Sciences, University of Birmingham, Birmingham, UK
Adverse drug events (ADEs) are a frequent source of harm in hospitalized patients. Identifying and measuring the burden of harms from ADEs can be challenging due to expense and lack of sensitivity. Detecting ADEs using sentinel signals or ‘triggers’ from a patient’s medical record has been shown to be a practical and less labour-intensive approach to identify ADEs. We wished to validate the Global TriggerTool proposed by the Institute of Healthcare Improvement[1] in the USA in detecting ADEs in a UK setting and to recommend changes that can be adapted into an electronic prescribing system.
University Hospital Birmingham NHS Trust is a large teaching hospital/tertiary referral centre with approximately 1200 in-patient beds. The locally-developed Prescribing Information and Communication System (PICS) is a rules-based prescribing and drugs ordering system which is also able to collect data for audit. All prescriptions on the wards are entered and administered using this system. We investigated the use of two trigger tools to identify ADEs using a retrospective review of electronic prescribing data from a 12-month time period in 2010. Two trigger tools were used: (1) naloxone as a signal of over-sedation caused by narcotic analgesics and (2) a record of an international normalized ratio value of greater than 6 as a signal of over-anticoagulation caused by warfarin.
We validated the sensitivity of the triggers using data from a retrospective review of patients’ case notes in order to establish the positive predictive values of these trigger tools in an electronic prescribing system. The findings were also compared with data from the hospital’s voluntary medication error critical incidents reports.
PP213. Early Adopters of Accredited Course in Pharmacovigilance
D. Layton, L. Harvey and S.A. Shakir
Drug Safety Research Unit, Southampton, UK; School of Pharmacy and Biomedical Sciences, University of Portsmouth, Portsmouth, UK
Background: Currently, there are few pharmacovigilance (PV) training programmes available at Masters Level in the UK and EU to support the education of PV scientists. In response to this unmet need, the Drug Safety Research Unit, a leading provider of training in pharmacovigilance, established a higher education institute certified PV postgraduate qualification comprising of three levels (Certificate, Diploma and Masters) as a collaborative programme in conjunction with the University of Portsmouth. A market survey previously conducted by the DSRU in 2009 suggested that the expected student population would be comprised of individuals new to PV and new to the pharmaceutical industry, who would require training and education to perform their duties and to progress their career.
Objective: To characterise the first cohort of students enrolled on the accredited postgraduate course in PV.
Methods: A descriptive study of registered students examined demographic, academic and employment history at enrolment, plus learning choices in relation to module selection. Summary descriptive statistics were calculated using STATA 10.
Results: The early adoptor cohort comprised 13 students; median age at registration 31 yrs (IQR 26–40). The majority came from the UK (69.2%, n = 9); the remainder were international (3 EU and 1 outside of EU). Ten students (76.9%) already had at least one postgraduate qualification (MSc or higher), with median interval between last award and recent enrolment of 8 years (IQR 4, 10). Scientific disciplines included: medicine (n = 5), pharmacy and pharmacology (each n = 2). The majority of student stemmed from pharmaceutical industry (76.9%, n= 10), of which nine (90.0%) held senior level positions. The Diploma was most frequent level of award chosen (61.5%, n = 8) with all students opting to undertake modules covering core pharmacoepidemiological skills in their first year.
Discussion: This study of the first cohort of students enrolled in the collaborative programme supports previous findings in that the majority stemmed from the pharmaceutical industry, but unexpectedly, this cohort comprised mainly of those holding senior positions and already holding other postgraduate qualifications. One explanation could be that the change in practice and regulation of PV has generated a need to address specific learning needs of drug safety personnel at all levels. The condensed nature of course delivery (over 2–3 days) of this collaborative programme is highly desirable in minimising the impact of such necessary education and training.
PP214. Nocturnal Enuresis in a Child Associated with Valproic Acid
A. Zaiem, I. Aouinti, G. Lakhoua, R. Daghfous, M. Lakhal and S.El Aidli
Centre National de Pharmacovigilance, Tunis, Tunisia
Introduction: Valproic acid is one of the most frequently prescribed anti-epileptic drugs worldwide for the therapy of generalized and focal epilepsies. It is usually well tolerated. Its main adverse effects are gastrointestinal disturbances, weight gain, hair loss and tremor. Enuresis is a rare adverse effect. We report a case of nocturnal enuresis in a child associated with valproic acid, notified to the Tunisian pharmacovigilance Center.
Case: G.O. had been treated with valproic acid for febrile seizure at the age of one year until the age of six. According to the parents, the psychomotor development was normal. The age of sphincter control was not precised but was reached before school age.
In November 2010, at the age of 11 years, for recurrence of febrile seizure, valproic acid at the dose of 500 mg twice a day was reintroduced. At the same time, the child has presented nocturnal secondary enuresis. Early morning plasma level of valproic acid was 124mg/mL 12 hours after the night dose, above the upper therapeutic limit.
After valproic acid withdrawal, enuresis improved gradually until total cessation within ten days.
Discussion: The role of valproic acid was retained in the genesis of the nocturnal enuresis mainly because of chronological data: compatible delay (concomitant with drug onset) and suggestive evolution marked with the cessation of enuresis when valproic acid was stopped. Some studies have recorded enuresis as an adverse effect of valproate in children with a frequency between 1 and 7%.[1] Some authors recommended either reducing of redistributing the doses.[1,2]
The mechanism of nocturnal enuresis induced by valproate is still controversial.
The most likely explanations are that either it is secondary to central effect on the thirst centre resulting in polydipsia or it is a consequence of the increased depth of sleep associated with valproate.
Conclusion: This case reported a rare adverse effect of valproic acid which occurred in a child.
PP215. Adverse Reactions Associated with Quinolones
A. Zaiem, I. Aouinti, G. Lakhoua, S. Kastalli, R. Daghfous, M. Lakhal and S.El Aidli
Centre National de Pharmacovigilance, Tunis, Tunisia
Introduction: Quinolones are considered as effective and safe antibiotics used commonly in many infections. However, some adverse reactions may occur during the use of these drugs. The aim of this study is to analyze epidemiological and clinical characteristics of notifications of adverse reaction associated with quinolones reported to the Tunisian pharmacovigilance Centre.
Materials and methods: It was a retrospective study about the notification of all adverse reactions associated with quinolones reported to the Pharmacovigilance Centre between January 2009 and December 2010. The notifications were analyzed according to the French method of imputation.[1]
Results: Thirty-six cases were included in this study. The median age of patients was 44 years (20 days–76 years) and 78% were females. Among our patients 9 had a history of allergy to other drug classes including beta lactams and antibacterial sulfonamides. The Quinolones associated with the adverse reactions were fluoroquinolones in 35 cases, mainly ofloxacin and ciprofloxacin, and in one case nalidixic acid. Skin reactions (mainly maculopapular eruption) had accounted for 47% of adverse events, hypersensitivity reactions for 33% and multisystemic reaction in 20%. Twelve cases were considered as severe: two cases of anaphylactic reaction, one case of Quincke edema, two cases of DRESS syndrome, 2 cases of multiple organ damage and two cases of severe cutaneous reaction. The outcome was favorable in thirty-five cases and in one case the outcome was not specified.
Conclusion: Our study reported 36 cases of adverse reactions associated with quinolones, some of which were exceptional.
PP216. Attitudes and Knowledge of Community Pharmacy Professionals to Adverse Drug Reaction Reporting in Coimbra, Portugal
C.F. Matos, J.J. Joaquim and T.S. Pires
Department of Pharmacy, College of Health Technology, Polytechnic Institute of Coimbra, Coimbra, Portugal
Background: Spontaneous reporting of adverse drug reactions (ADRs) remains one of the most effective methods to detect new, unusual and serious drug reactions, because it covers the entire population and all medicals drugs throughout their commercial life, being also a free method.[1] It’s well known that there is a high degree of underreporting and improve it, community pharmacy professionals must play a fundamental role in spontaneous ADR reporting. They are uniquely placed to provide valuable post-marketing information on medicines and to report possible ADRs, due to the contact with the patient before and during the drug therapy. However, the country’s ADR reporting figure of 200 per million (2009) population falls far short of the WHO target of 250–300 per million.[2]
Objectives: The aim of this survey was to gain insight into the attitudes and reporting behavior of ADR in community pharmacy professionals in Coimbra, Portugal, being consequently possible to detect the factors that influence under-reporting, in order to identify a specific educational intervention strategy and potential solutions to solve this problem.
Methods: A cross-sectional descriptive-correlational study was conducted to the professional population of 49 pharmacies of Coimbra, including 156 pharmacists and 40 pharmacy technicians. They were personally interviewed with a questionnaire adapted from previous studies (based on Inman’s eight deadly sins’).[3] They were surveyed about their knowledge and attitudes to ADR reporting and the factors that encourage and discourage ADR reporting.
Results: Response rate was 82%. The seriousness of the reaction and the unusual reaction was stated to be the more important ADR’s in decision to report. Age, sex, job function and years working appear to have no influence on reporting. The results of this study show close agreement with previous studies on the attitudes of medical practitioners and pharmacists. Professionals seems to agree that they have “professional obligation to report ADRs” (96.4%) and “they don’t feel the need to report well-known ADR” (54.1%). Other attitudes and opinions associated with under-reporting were linked to: lack of time (50%), method of reporting (38.3%), and fear of legal liability (29.6%).
Conclusions: Community pharmacy professionals’ knowledge, beliefs, behavior and motivation play an important role in ADR reporting.[4] Despite of the perception of the importance assigned to pharmacovigilance by the professionals, the under-reporting remains a reality.
Discussion: That under-reporting could be minimized through educational interventions based on identified attitudes related to under-reporting.[4] Community pharmacy professionals must be a priority target for this intervention.
PP217. Comparative Assessment of Adverse Reaction Reports Submitted to WHO-UMC by the Turkish Pharmacovigilance Center (TUFAM) through 2008/2009/2010
E. Aykaç,1 D.N. Aydınkarahaliloğlu,1 Y .Kasap,1 G. Sağiş,1 C. Babacanoğlu,1 H. İlbars,1 S. Kılıç,2 H. Özbek 1 and S. Kerman 1
1 General Directorate of Pharmaceuticals and Pharmacy, Ministry of Health, Ankara, Turkey; 2 Gülhane Military Medical School, Department of Epidemiology, Etlik, Ankara, Turkey
Background: Starting from 1987, our country has been a member of World Health Organization-the Upssala Monitoring Centre (WHO-UMC) and has been reporting adverse drug reactions (ADRs) to the database of the center since then.
Objective/aim: The aim was to assess the ADRs submitted to WHO-UMC by TUFAM through 2008-2009-2010.
Methods: The ADR reports from 2008, 2009 and 2010 on Vigiflow database have been assessed in excel format provided by the system. ATC codes were used in drug classification, and system organ class (SOC) was used in ADR classification. And also, the sources (authorization holder, pharmacovigilance contact point, direct reporting) of ADR reporting healthcare professionals and reporting healthcare organizations were conveyed in excel.
Results: 389 ADR reports were submitted to WHO by TUFAM in 2008, 520 ADR reports were submitted in 2009 and finally, 1000 ADR reports were submitted in 2010. In all three years, a higher rate of ADR reports was observed in adults compared to the other age groups. Based on ATC classification, the drug class with the most frequent ADR reports was “J01 Antibacterials for Systemic Use” through all three years with proportions of 13.9%, 12.3%, and 13.6%, respectively. Based on SOC, the most commonly observed ADRs were “body as a whole general disorders” through all three years with proportions of 17.8%, 16%, 18% respectively. In 2008, 84.06% were reported by authorization holders and 2.06% were reported by contact points while 13.88% were directly reported. The proportions were 75.6%, 5.6%, 18.9% in 2009, 69.9%, 6.3%, 2.38% in 2010 respectively. When the reports were assessed based on the reporting occupational groups through all three years, it was found that physicians had submitted the most number of ADRs.
Conclusion: The suspected drugs most frequently reported to TUFAM were in “Antibacterials for Systemic Use” group. However, the assessment based on drug types showed that most frequent reports were related to TNF alpha blocker drugs (L04AB), and the most commonly observed ADRs were in “body as a whole general disorders” category based on the classification by SOC. While most of the reports were submitted by the authorization holders in all three years, a significant increase was observed in proportion of direct reportings over the years (p< 0.001).
Discussion: There was no significant difference observed in SOCs with respect to most frequent ADR reports through the years (p = 0.447).
PP218. A look at the Past: History of Rimonabant
D.N. Aydinkarahaliloglu,1 E. Aykaç,1 Y .Kasap,1 G. Sağiş,1 C. Babacanoğlu,1 H. İlbars,1 B.O. Yıldız,2 S. sSarda§,3 H. Özbek 1 and S. Kerman 1
1 General Directorate of Pharmaceuticals and Pharmacy, Ministry of Health, Ankara, Turkey; 2 Department of Endocrinology and Metabolism, Hacettepe University, Faculty of Medicine, Ankara, Turkey; 3 Department of Toxicology, Marmara University, Faculty of Pharmacy, Istanbul, Turkey
Background: Rimonabant is an anti-obesity drug and a selective cannabinoid-1 receptor (CB1) antagonist.
Objective/aim: The aim was to explain the course of rejection of authorization application for rimonabant.
Method: The decisions made during the authorization process of rimonabant, the objection of the relevant company and our references have been evaluated.
Results: Regarding rimonabant, authorization application was submitted to Turkish Ministry of Health, General Directorate of Pharmaceuticals and Pharmacy on June 14th 2006. Serious adverse events regarding the Phase III trial (CRESCENDO) were reported to the Ministry on January 26th, 2007. On January 31st, 2007, it was suggested to stop conduct of the Turkey leg of the study and provide psychiatric consultation to patients who were included and still participating in the study. On February 27th, 2007, it was requested to perform a psychiatric consultation on patients included in rimonabant studies and measurement of their depression scales (Hamilton, Beck) prior to, 1 month after, 6 months after, 1 year after and 2 years after the treatment as well as during the conduct of study with regular intervals and the results to be submitted to the Ministry. The authorization process was suspended on April 30th, 2007 until the drug safety is proven due to the finding in Phase III trials and during its use in authorized countries showing accumulation of adverse reactions such as suicidal thoughts, depression with aggression and psychosis. On May 1 1th, 2007 recommending rimonabant studies was allowed provided that a psychiatrist is added as a co-investigator in each participating center and close monitoring of adverse reactions is ensured. On October 19th, 2007 the authorization process was suspended in our country until the completion of scientific studies related to the drug and the demonstration of safety regarding development of psychiatric symptoms. The objections from the company requesting the continuation of authorization process dated January 16th, 2008 and October 10th, 2008 was rejected due to lack of sufficient safety data and authorization was not deemed as appropriate. Marketing of rimonabant was suspended in all the Member States on November 13th, 2008. The marketing authorization holder responsible for rimonabant notified the European Commission (EC) of its decision to voluntarily withdraw its marketing authorization on December 5th, 2008. On January 16th, 2009, the EC issued a decision to withdraw the marketing authorization for Acomplia.
Conclusion: The authorization application regarding rimonabant was rejected on October 10th, 2008.
PP219. Education and Training Activities of TUFAM
D. Aydinkarahaliloglu, E. Aykaç, Y. Kasap, G. Sağiş, C. Babacanoğlu, H. İlbars, H. Özbek and S. Kerman
General Directorate of Pharmaceuticals and Pharmacy, Ministry of Health, Ankara, Turkey
Background: The training activities aimed at drug safety responsible persons provide compliance to the pharmacovigilance regulations while the training activities aimed at healthcare professionals raise awareness.
Objective/AIM: It was aimed to provide insight to the training activities we have participated since June 30th, 2005.
Method: TUFAM has started its training activities after the directive has become effective.
Results: Starting from July 8th, 2005 to date, a total of 10 training programs aimed at drug safety responsible persons have been carried out. The content of the training program was prepared by TUFAM in compliance with the Directives and Guidelines. Eight of the pharmacovigilance programs were conducted in collaboration with Pharmacovigilance Association. In addition, numerous meetings were held with the pharmacovigilance contact points in various hospitals. Every year, TUFAM provides information regarding the pharmacovigilance activities for the students in master of science program and those in their final year at Hacettepe University Faculty of Pharmacy. Furthermore, recognition of TUFAM is aimed by participating in congresses cnducted by various specialty associations. Training activities are performed for pharmacovigilance contact points which are in the position of being TUFAM representatives in hospitals. In collaboration with Turkish Pharmacists Association, educational pharmacist training has been performed for community pharmacists.
The training activities and the cities where they were conducted in will be presented in tabulated form in our study.
Conclusion: The pharmacovigilance system aiming to protect individuals as well as the community against the possible drug related risks considers that the training activities are of greatly importance with regard to raising awareness among the healthcare professionals who are in charge of determining these risks.
Discussion: Our training activities have played a significant role in the increase in adverse reaction reportings submitted to TUFAM by healthcare professionals over the years ever since the establishment of TUFAM.
PP220. Turkish Pharmacovigilance Center (TUFAM) and Monitoring of Safety Warnings
Y. Kasap, D.N. Aydınkarahaliloğlu, E. Aykaç, G. Sağiş, C. Babacanoğlu, H. İlbars, H. Özbek and S. Kerman
General Directorate of Pharmaceuticals and Pharmacy, Ministry of Health, Ankara, Turkey
Background: In line with the directive, TUFAM is responsible for the follow-up of safety related matters and performing of necessary actions. During the conduct of its activities TUFAM benefits from comments of “Monitoring, Assessment and Advisory Commission for Safety of Medicinal Products for Human Use” (BTUGIDDK) when necessary.
Objective/aim: The study was designed to provide insight on actions TUFAM has taken regarding drug safety and related matters.
Methods: The warnings subjected to TUFAM agenda from April 2009 to May 2011 and the actions taken as a result of these warnings were recorded in excel format. Among these warnings were the journals published by health authorities, warnings published on official internet websites, periodical publications, company based reports (RMP, PSUR, Type II variation, final or interim reports submitted due to unexpected findings during clinical or non-clinical trials etc.), patient/physician complaints and in-house comment requesting correspondence. Calculations were made between the parameters in excel format containing information regarding the ATC codes of the drugs with safety issues, date of the issue, source of the warning, whether it was included in the commission and the resulting actions.
Results: According to the assessment based on subjects, TUFAM has included 374 safety warnings in its agenda from April 2009 to May 2011.121 of these 374 warnings (32.35%) subjected to TUFAM agenda were assessed by TUFAM and was not deemed necessary to be included in BTUGIDDK agenda. The remaining 253 warnings (67.64%) were subjected in commission agenda. The drug groups which were most commonly included in TUFAM agenda were as follows: “antineoplastics and immunomodulating agents” in group “L” (19.25%), “nervous system” in group “N” (18.18%) and “antiinfectives for systemic use” in group “J” (17.91%). As the 374 warnings subjected to TUFAM agenda were reviewed, no action was deemed necessary for 141 (37.7%) warnings and these were only recorded with the information provided. 74 (19.78%) warnings were submitted to relevant departments of General Directorate of Pharmaceuticals and Pharmacy, letters were distributed for 38 (10.16%) warnings, additions were implemented in SmPC warning section for 32 (8.56%) warnings and RMP was generated for 18 (4.81%) warnings.
Conclusion: In collaboration with international organizations, TUFAM reviews worldwide issues regarding drug safety, takes necessary actions or mediates the necessary actions to be taken.
Discussion: TUFAM plays a key role in drug safety related matters.
PP221. Drugs Recalled from the Market and Given Black-Box Warning Due to Safety Issues in Turkey
D.N. Aydinkarahaliloglu, E. Aykaç, Y. Kasap, G. Sağiş,
C. Babacanoğlu, H. İlbars, H. Özbek and S. Kerman
General Directorate of Pharmaceuticals and Pharmacy, Ministry of Health, Ankara, Turkey
Background: Hence the animal experiments are insufficient in terms of determining safety in human beings and the studies are conducted with selected patients of a limited number with their period and conditions of use differing from real life conditions, and as the frequently observed data is usually insufficient, drugs should be monitored via post-marketing surveillance.[1]
Objective/aim: In the present study, drugs that were recalled from the market between December 2002 and December 2011 were investigated. Additionally, information is provided regarding the drugs which had received a black box warning, had their authorization application suspended and the preparations that had received outer packaging warning.
Methods: The drugs with authorization suspended or cancelled due to safety reasons between November 2002–May 2011 were determined based on Directorate General records. During this assessment, the “Authorization Cancellation List’ for the period of October 8th, 2008 to April 27th, 2011 on General Directorate of Pharmaceuticals and Pharmacy website was also investigated. Additionally, each SmPC applicable for the period of May 12th, 2011 to July 25th, 2007 on General Directorate of Pharmaceuticals and Pharmacy website and in TUFAM records was investigated individually and the drugs that had received a black box warning were determined as well as the drugs that has received an outer packaging safety warning. Furthermore, drugs with suspended authorization application process will be presented in a separate table.
Results: The name of the drugs, dates of authorization, ATC codes, safety issue, date of withdrawal from the market/suspension/cancellation were tabulated for the drug substances with safety issues during the given period (i.e., nefazodone, rofecoxib, benzbromarone, tegaserod, lumira-coxib, aprotinin (systemic) clobutinol, becaplermin, efalizumab, sibutramine, bufexamac, rosiglitazone and benfluorex). Separate tables will be presented for drugs that had received an outer packaging warning due to safety reasons (i.e., rosiglitazone, pioglitazone, clozapine) as well as drugs that had their authorization application cancelled or withdrawn by the authorization holder or suspended, and drugs that had black box warning in summary of product characteristics (i.e., sibutramine, rosiglitazone, pioglitazone, eltrombopag, bosentan, isotretinoin etanercept, adalimumab, infliximab, leflunomide, antipsychotics, antidepressants, varenicline tartrate, bupropion).
Conclusion: Drug safety issues are rigorously monitored during the authorization application process of drugs as well as during the post-marketing period in our country. Consequently, the necessary actions are taken in a timely manner.
Discussion: By taking actions in a timely manner, we attempt to protect public health.
PP222. Suicidality and Selective Serotonin Reuptake Inhibitors and Serotonin and Noradrenalin Reuptake Inhibitors: Analysis of the French Pharmacovigilance Database
S. Tan,1 C. Le Beller,1 F. Coudoré,2 P. Auriche 3 and A. Lillo Le Louet 1
1 Centre régional de Pharmacovigilance, Hôpital Européen Georges Pompidou, Assistance Publique — Hôpitaux de Paris, France; 2 Pôle Biologie, Hôpital Européen Georges Pompidou, Assistance Publique — Hôpitaux de Paris, France; 3 Unité de Pharmacovigilance, AFSSAPS, Paris, France
Evidence suggests the contribution of antidepressants (AD), in particular Selective Serotonin Reuptake Inhibitors (SSRI), in worsening depression and increasing risk of suicidality in some patients. Suicidality gathers suicide ideas and plans, suicide attempts and suicides. We conducted a study from the French Pharmacovigilance database (FPD) about SSRI and suicidality, extended to Serotonin and Noradrenalin Reuptake Inhibitors (SNRI).
The suicidality was evaluated from all adverse effects (AE) reported in the FPD analysed with five SSRIs (fluoxetine, citalopram, escitalopram, paroxetine, sertraline) and three SNRIs (duloxetine, milnacipran, venlafaxine). Cases were registered from March 1986 to September 2010. The database provides AE descriptions, patient’s characteristics, details about medications (duration, indication and dosage). A manual extraction of cases using MedDRA the following preferred terms: “depression”, “suicidal ideas”, “suicide” and “suicide attempts” was performed. Ratios of suicidality-induced AE divided by the total number of AE reported were calculated for each AD studied. Cases were also extracted with the standardised MedDRA query (SMQ) “Suicide-automutilation” and results were compared with the “manual” request.
Preliminary Results: 144 cases of suicidality were extracted; after analysis, 50 were excluded. The notification rate of suicidability was 0.5% (94 cases/17520). The highest rate of suicidality-induced AE for SSRIs was observed with fluoxetine (1%, 45/4671) and the lower with paroxetine (0.1%, 7/4873). For SNRIs, duloxetine total ratio was 2% (9/415) and represented a 2-fold higher ratio compared to fluoxetine. As some publications underline that suicidality associated with use of AD is strongly age dependant (increased risk of suicidality for adults under 25 and reduced risk over 65), we analyse this rate regarding three age classes (<25 — 26–64 and >65). With SSRIs, the higher rate occurred in patients aged 25 years and less treated with fluoxetine (1.7%, 5/295) and the lowest rates in people aged over 65 treated with paroxetine (0.09%, 2/2255). With SNRIs, patients over 65 have a higher risk with duloxetine 3% (4/144). Risk of suicidality was higher in women (63%). A medical history of depression was recorded in 34% of patients. Durations of treatment varied from 2 days to 3 months and the event suicidality occurred within 1 day to 3 months after AD initiation. A transversal analysis with the SMQ “Suicide-automutilation” terms retrieved 54 cases in common with the manual request and 13 more cases. We excluded 80 cases. This comparison may provide useful information to optimize SSRIs and SNRIs treatments according to the target population.
PP223. Necessity to Implement Pharmacovigilance of Medicinal Plants in Sub-Saharan African Countries
R.K. Cimanga,1 N.K. Ngombe,2 T.M. Nanga,3 G.K. Mesia 3 and G.L. Tona 3
1 Laboratoire de Pharmacognosie et de Phytochimie, Facultés des Sciences Médicales et Pharmaceutiques; 2 Laboratoire de Chimie Médicinale, Faculté des Sciences Pharmaceutiques, Université de Kinshasa, DR Congo; 3 Unité de Pharmacologie Clinique et Pharmacovigilance, Kinshasa, DR Congo; Centre National de Pharmacovigilance, DR Congo
Few data about adverse events and toxicity of African medicinal plants are reported in traditional Pharmacopoeia or in papers and books. In developing countries especially in Africa, people are currently using medicinal plants to treat various diseases without any knowledge on their safety. For them, the natural is always safe according to their use since decade. The use of medicinal plants is considered today as an alternative medicine in our countries unfortunately, many cases of serious adverse drug reactions have been encountered after the use of some plants. This couple of years some data arise from the literature on the safety of many plants among those commonly used.[1,2]
If in the past toxicity were attributed to some chemical groups as alkaloids, cardiotonic heterosides ….It is well known today that aristolochic acid an carboxylic acid found in many plants can induce body damage leading to serious kidney impairment. In this context, pharmacovigilance of medicinal plants became a necessity and must be implemented or encouraged.
Considering the lack of these valuable data in our health system, we have initiated the elaboration of a formulary in which especially nature of compounds, pharmacological action exerted, toxicity in animal, effects in human including adverse drug reactions, interactions with other plants or synthetic compounds, contraindications and management of ADR will be included. In our knowledge, such document did not exist for plants used in our region.
Sources of information are mainly internet, traditional pharmacopoeia, books and papers. Since the writing is ongoing, more than 300 web sites have been identified, consulted allowing some information. Unfortunately some data are unavailable, and for many plants it will be necessary to perform experimental studies for the completeness of this document. At this stage we have partially collected data for more than fifty plants and it will be necessary to collect data for most plants commonly used.
Pharmacovigilance need accurate and reliable data for the assessment of adverse drug event. Experience has shown the difficulty to establish the causality relationship with medicinal plant, reducing the value and quality of Individual Case Safety Reports (ICSRs) in most of cases. This document will be also useful for practitioners, scientists and decision makers of health system.
PP224. Our 6 Years of Local Experience in Pharmacovigilance
E. Arda, F. Gezerlerand S. Altug
Medical Department, Lilly Turkey, Istanbul, Turkey
Background: An adverse drug reaction is defined as unintended harmful or unpleasant response to a medicinal product, which predicts hazard for future administration and warrants prevention or specific treatment, alteration of dosage, or discontinuation. The pharmacological management of disease should involve consideration of the balance between the beneficial effects of treatment on outcome and the probability of adverse effects. Therefore; pharmacovigilance (PhV) is very important and Lilly Turkey has been implementing PhV requirements since 2005. The aim of this study is to share the situation regarding spontaneous adverse event reporting in Lilly Turkey during a 6-year period (2005–2010).
Methods: Numbers of spontaneous adverse events received via patient support programs (PSPs), health care professionals, consumers and others like sales representatives etc. were calculated per year between 2005 to 2010. Moreover, they were classified according to therapeutic areas and types of the reports.
Results: Lilly Turkey is mainly in five therapeutic areas with 42 products. These are CNS, Diabetes, Endocrine, Men’s Health and Oncology. Based on a review of our cases yearly, the highest case numbers have been observed in 2009 and 2010, particularly in Diabetes therapeutic area, received from PSPs. It has been also determined diabetes cases include pregnancy reports as the most and the numbers of pregnancy cases are significantly high in 2009 and 2010, respectively as 39% (427/1096) and 48% (876/1828) due to insulin usage in gestational diabetes.[1] The other cases within this area include especially the events like hyperglycemia, hypoglycemia, injection site problems as common complaints related to diabetes. On the other hand, the rates of the cases received from HCPs are dramatically low in comparison with the cases received from PSPs (2% vs 93% in 2009; 4% vs 94% in 2010) and also some difficulties came up with handling of these high numbers of PSP cases as unsuccessful follow-up attempts for them due to having poor medical quality and biased information.[1]
Conclusions: Our experience suggest that education is very important for increasing adverse event reporting importance and PhV awareness of HCPs to be able to receive medically higher qualified data. Trainings always increase the awareness for HCPs. Social media (Facebook, Twitter, blogs, microblog, etc.) can be also used for increase of the awareness. In conclusion, more accurate and meaningful data in adverse event reporting are targeted in near future for Lilly Turkey.
PP225. Evaluation of Drug License Suspensions and Withdrawals between 1999 and 2010
E. Can
Hasfarma Pharmaceutical Company, Istanbul, Turkey
Background:When health authorities believe that a drug’s benefits no longer outweigh its risks, the manufacturer will be asked to withdraw the drug. A conclusion that a drug should no longer be marketed is based on the nature and frequency of the adverse events and how the drug’s benefit and risk balance compares with treatment alternatives.
Objective:In the present study, various drug active ingredients, whose licenses have been suspended or withdrawn between the years of 1999 and 2010 by EMA (European Medicines Agency)(n = 15) and FDA (Food And Drug Administration) (n = 24) have been investigated to evaluate and compare the safety reasons, therapeutic groups and development procedures.
Methods:The official data of FDA, EMA,WHO (World Health Organization) and published scientific articles between 1999 and 2010 have been searched and evaluated.[1]
Results:As evaluated by the active ingredients according to pharmacological groups, the first three in the line were analgesicantiinflammatory drugs, antipsoriasis agents, and immunomodulators (17%, 8%, and 8% respectively; n = 24) in FDA, whereas analgesicantiinflammatory drugs, antidiabetics and antiobesity drugs (27%, 20% and 7% respectively; n= 15) in EMA. It is noteworthy that molecules with effects of analgesic and antiinflammatory are the first in line among the withdrawn drugs by the both health authorities. Drugs used in cardiac diseases were in the first line with safety problems (FDA: 52%, n = 23; EMA: 56%, n= 16), and drugs for nervous system diseases were in the second line (FDA: 18%, n = 23; EMA: 13%, n= 16). Out of 39 active drug ingredients 18% were developed by biotechnological methods, whereas 82% of them were developed by conventional methods (FDA: 21%, 79% — (n:24); EMA: 13%, 87%-(n:15)).
Conclusion:Molecules that have been withdrawn from the market most frequently due to drug related adverse effects belongs to cardiac and nervous system diseases, because the clinical signs related to these systems are easy to diagnose, and causality relationships are easier to confirm. Moreover, the reason for the withdrawal and suspension of licences related to analgesic-antiinflammatory drugs might be associated with more frequent drug related adverse event reporting system since they are used by larger populations. It is early to conclude on the drugs developed by biotechnological methods since the number of withdrawals are too small to discuss.
PP226. Safety Profile of Indacaterol: Results of an Early Experience Program in México
G.A. Barrera and M.D. Fuentes
Novartis Farmacéutica, México, Distrito Federal; Drug Safety Department
Background:Indacaterol is a novel, inhaled, ultra long-acting beta 2-agonist (LABA) available in EU and other countries included Mexico, it is approved for the maintenance treatment of airflow obstruction in patients with chronic obstructive pulmonary disease (COPD) in doses of 150 and 300 mcg once daily.[1]
Objective:To describe the safety profile of indacaterol in an early experience program through spontaneous adverse events reporting by patients directly to a call center.
Methods:This program consisted of inviting patients with COPD and gave them Indacaterol through a physician prescription in a real life setting. The patients were asked to complete 3 surveys (basal, 2 and 4 weeks) about ongoing symptoms and satisfaction with Indacaterol. About 1316personswereinscribedinaperiod from 26-Sep-2010 to 04-Jan-2011. When a patient reported an adverse event spontaneously, the call center operator asked them for details about this event and additional follow-up information was then obtained (Novartis pharmacovigilance department) from relatives or prescribing physicians. The adverse events were reported according to internal procedures and local regulations.
Results:107 patients reported adverse events (AEs) in this period, 60% were female and 40% were male. The average age was 69.1 years (range 26–98). The indication of Indacaterol was COPD in 90% of these patients. The dose used was 150 mcg in 98% of these patients. The reports corresponded to 151 non serious AEs and 66 serious AEs. The most frequent non serious AEs were cough (17%), difficult for breathing (14%), reactions in throat like throat irritation and throat sore, dry throat, burning throat or burning (12%), most of them were experienced just after the administration of Indacaterol on in the next first days of the therapy. Approximately thehalf of these cases got recovered after the withdrawal of Indacaterol. Regarding the serious AEs, most of them were complications of underlying respiratory conditions included 20 fatal cases. In none of the cases was pneumonia or COPD progression related to indacaterol therapy. None of the prescribing physicians suspected that indacaterol was related to these serious AEs.
Conclusions:The early experienced programs are a useful strategy to monitor the AEs in a real life setting during the first/early postmarketing period. The profile of AE’s found for Indacaterol corresponded to described in the basic prescribing information and with the natural history of this disease.
Countries ADR Reports
PP227. The Assessment of Knowledge/Attitude of Community Pharmacists Located in Istanbul towards New Pharmacovigilance Regulations
G.C. Aşkin,1 N.P. Ay,2 G.Z. Omurtag 1 and S. Şardaş 1
1 Department of Toxicology, Pharmacogenetics and Drug Safety Unit, Marmara University Faculty of Pharmacy, Istanbul, Turkey; 2 Department of Public Health, Marmara University School of Medicine, Istanbul, Turkey
Background:In July 2005 Turkey introduced new regulations for pharmacovigilance, designed in harmony with the pharmacovigilance system that is applied within the European Union. In fact, Turkey joined the WHO International Drug Monitoring Programme in 1987 and established the Turkish National Centre for Adverse Drug Reaction Monitoring. However, the reporting rate was never very high due to lack of regulations and guidance for reporting obligation. Therefore in 2005 TÜFAM (The Turkish Pharmacovigilance Center) has been established and the new centre has been expanding its activities since then.[1]
Objectives:The university education for a pharmacy degree is for 5 years in Turkey. After 2005, topic of Pharmacovigilance has been given more focus in the teaching programme designed for the pharmacy students of 4th grade. The purpose of this study is to determine and to compare the knowledge and attitude of community pharmacists who graduated before and after 2005, in order to evaluate the effect of training and their attitudes towards the system.
Methods:Face-to-face questionnaire consisting of 39 questions was conducted with 78 community pharmacists (39 graduated before 2005 and the rest graduated after 2005). Main outcomes were analyzed by SPSS 17.0.
Results:It was determined that only 17 pharmacists have been involved in ADR reporting (8 of them graduated before 2005 and 9 were after 2005). The percentage of the pharmacists who reported ADR to TÜFAM (5.9%), and to drug companies (35.3%), are same, regardless of their graduation year. The percentage of pharmacists reporting ADR to physicians were higher in graduates after 2005. (5.9% vs 11.8%).
Reasons given for not submitting ADR reports were lack of information (48.4%), lack of time (18.8%), belief about unnecessity of reporting since most of ADRs are stated in prospectus (12.5%), not being an obligation (10.9%), belief about not being responsible in ADR reporting (3.1%), lack of clinic knowledge (3.1%), not to cause patients to lose confidence for their pharmacist (3.1%).
Conclusions:The results show that there is no difference in ADR reporting of pharmacists when compared by their graduation years. This reflects a need for further training and improved information about the spontaneous reporting system. The pharmacovigilance training should start in early grades of pharmacy and educational conferences for all health care professionals should take place to increase their involvement in the system.[2]
PP228. Metamizole (Dipyrone) and Agranulocytosis in Germany: Long-Term Consequences of a Regulatory Measure in 1986
T. Stammschulte and U. Gundert Remy
Drug Commission of the German Medical Association, Berlin, Germany
Background:In 1986 risk of agranulocytosis and shock in association with metamizole prompted regulatory measures in Germany. Over-the-counter availability was abandoned. All fixed-combinations were withdrawn from the market. Indications were restricted to acute post-traumatic and postsurgical pain, colic and cancer pain, and treatment of pain or fever if other measures are not indicated or failed. After an initial decline, prescriptions increased from < 20 million defined daily doses in 1990 to >114 million in 2009. Concurrently, spontaneous reports of agra-nulocytosis increased from about 10 per year in 1990 to >30 in 2009.
Objectives:To assess reports of agranulocytosis in association with metamizole with regard to indication, severity and outcome.
Methods:Reports of suspected metamizole-induced agranulocytosis between 1990 and 2010 were identified in the German spontaneous reporting database. Reports initially received by the DCGMA were eligible for assessment since original reporting forms and additional documents are available.
Results:A total of 335 reports were identified of which 114 were eligible for assessment. 3 cases were excluded (wrong diagnosis (2), missing exposure to metamizole (1)). 111 reports were assessed in detail. Patient characteristics are presented in table I. The most frequent indications for metamizole were post-traumatic and postsurgical pain (35 cases, 31.5%), while cancer pain (5,4.5%) and colic (none) were of minor relevance. In roughly half of the cases prescription of metamizole was not clearly in conformity with the approved indications.
Conclusions:Although agranulocytosis is a very rare adverse reaction of metamizole the number of reports in consequence of the increase of prescriptions and the severity of the cases indicate a serious health problem. The proportion of female patients, bi-or tricytopenia, fatal outcome and median time to onset in our cases are in line with findings in Sweden.[1] The prescribing pattern shows that physicians may be unaware to some extent of the restricted indications of metamizole.
PP229. Attitude and Awareness of ADR Reporting by Hospital Health Professionals in the Holy City of Makkah, Kingdom of Saudi Arabia (KSA)
N.N. Alhazmi
School of Life Sciences, Pharmacy Department, University of Bradford, Bradford, UK
Background:The necessity for all health professionals to report suspected ADRs as a professional duty relies on their attitude and awareness of the overall process.[1] This study investigated hospital ADR reporting in Makkah, the holiest city on earth to Muslims.
Objective/aim:To investigative and assess the attitude and awareness towards adverse drug reaction (ADR) reporting and factors that influences such reporting by doctors, dentists, pharmacists, nurses in Makkah hospitals.
Methods:A questionnaire was designed, circulated and to 470 health professionals in seven hospitals located in Makkah, (KSA).
Results:Of 470 circulated questionnaires, 310 were completed by: 205 doctors, 25 dentists, 49 pharmacists and 31 nurses — a response rate of 65.9%. 47.1% (n= 146) of the responders were aware of the existence of the ADR reporting and monitoring system in Makkah hospitals and 33.2% (n= 103) had actually submitted ADRs reports to the Ministry of Health (MOH) located in Makkah. In contrast, only 41% of the health professionals were aware of the existence of National Pharmacovigilance Center (NPC) in the Saudi Food and Drug Authority (SFDA). Of the respondents, 35.2% (n= 109) had been trained on how to report ADRs and 47.1% had come across patient(s) with an ADR during the last month that they actually wanted to report.
Discussion:Despite a lack of knowledge about the system of reporting, 50% of the people who had actually reported a case suggested that it had benefited their patients by identifying safe drugs. 67.1 % suggested that the mandatory program of ADR reporting was useful although the majority did not use it. Furthermore, 70% responders reported that pharmacist assistance in the detection, reporting and management of ADR had been useful, as part of their professional role a finding previously reported by van Grootheest et al. In 2004.[2] Discouragements to active ADR reporting were the apparent lack of reporting forms being available, the process was considered to be too time consuming, some did not know precisely how to make a report and finally some expressed an indifference to the system.
Conclusion:The spreading of knowledge and awareness about ADR reporting among medical professionals by relevant training and education would engender a reporting culture that may lead to the establishment of a Pharmacovigilance center in the region. Existing Pharmacists have an important role to play in developing the area of Pharmacovigilance in Makkah hospitals as first suggested by Ghosh et al in 2004.[3]
PP230. Community Pharmacists’ Attitude and Willingness Towards the Reporting of Adverse Drug Reactions in Bulgaria
V. Stoynova and I. Getov
Faculty of Pharmacy, Medical University Sofia, Bulgaria
Background:Bulgaria has a long tradition in monitoring of adverse drug reactions, but the reporting rate in the country is relatively low. Although since 2007 all health care professionals are obliged by the legislation to report serious adverse drug reactions, the pharmacists in Bulgaria are not actively reporting adverse drug reactions.
Objective:To explore community pharmacists’ attitude towards Pharmacovigilance and their willingness to participate in adverse event reporting system.
Methods:Between September 2010 and June 2011 we conducted a survey about the knowledge and attitude of 550 randomly selected community pharmacists using a face-to-face questionnaire. The questionnaire consisted of questions about the sociodemographic characteristics of the pharmacists, their knowledge of adverse events, sources of information that they are using in their daily practice and their attitudes towards ADR reporting.
Results:Respond rate was 61.27% (n = 337). Sixty four percent of the community pharmacists responded that the problem with adverse drug reactions in extremely important and 35% of them considered it important. Ninety three percent of the pharmacists stated that patients usually prefer to reported an ADR to them, but only 18% of pharmacists reported cases to the concerned organizations. The actual reporting rate of the pharmacists in Bulgaria is even lower. Only 10% stated that they are familiar with adverse event reporting system, and 53% considered that they have knowledge, but would like to receive additional information.
Conclusion:The results show that Bulgarian pharmacists have poor knowledge about adverse event reporting system, but they would like to receive additional information about pharmacovigilance. Community pharmacists have potential to play important role and can contribute substantially to ADR reporting. There is need for accredit educational programs to train them about ADR reporting both for post-graduate specialization and LLL systems.
PP231. Psychiatric and Behaviour-Related Adverse Events Occurring with Antiasthmatic Drugs Reported in the National Pharmacovigilance Network
F. Trotta, L Tartaglia, F. Ferrazin and C. Santuccio
Italian Medicines Agency, Pharmacovigilance Unit, Italy
Background:Antiasthmatic drugs (ADs) are frequently used in childhood; psychiatric and behaviour related adverse reactions have been reported especially after leukotriene inhibitors (LI).[1] An increased reporting of these reactions in children was observed in Europe.[2]
Objective:To analyze and describe psychiatric and behaviour-related adverse events occurred with ADs and reported in the National Pharmacovigilance Network.
Methods:Spontaneous reports occurring with ADs and suspected ADRs included in the SOCs Psychiatric Disorders and Nervous System Disorders were retrieved from January 2001 to June 2011.
Results:Overall, 712 reports of ADR with ADs use were identified; 170 (24%) were referred to the SOCs of interest. Considering different age groups, the 29% of cases were referred to children, while 45% and 26% were adults and elderly respectively.
With regard to the drugs, in the 32% of cases the class of LI was involved (in all but one cases the drug involved was montelukast), followed by beta-2 agonists and association between beta-2 agonists and glucocorticoids (19% and 16% respectively).
Moreover, 51 cases referred to psychiatric and behaviour-related adverse events were reported in children. A very high percentage of paediatric reports (33 out of 51, 65%) with montelukast have been observed when compared with other ADs.
The majority of the ADRs were not serious (70%), while the 19% were serious (for the remaining the seriousness was undefined). There is not a higher frequency of serious reports with LI.
A total of 241 ADRs with ADs were retrieved within the SOCs of interest. In particular, 88 out of 241 ADRs occurred with LI (57; 65% in children) while the remaining 153 ADRs with other ADs (only 25; 16% in children). The PTs more frequently reported in children following montelukast were insomnia, nightmares, headache, hyperactivity; the PTs more frequently reported in children following other ADs were agitation, insomnia, tremor, restlessness.
The AD reports were analyzed also considering specific SMQs resulting in 55 events: Depression, excluding suicide and self injury (16 events), Hostility/aggression (27 events), Psychosis and psychotic disorders (10 events), Suicide/self-injury (2 events). The 51% of these SMQ events were referred to montelukast (28 out of 55), 22 of which (78%) occurred in children.
Conclusion:A high frequency of psychiatric and behaviour-related adverse events with montelukast, particularly in children, was high-lighted. Although some psychiatric ADRs are included in the montelukast product information, it is necessary to add more evidence to improve the appropriateness of use in children.
PP232. Analysis of Spontaneous Adverse Drug Reaction (ADR) Reports from the Yellow Card Scheme (YCS) in 2010
M.M. Jadeja, S. Suri, M. Foy, S. Gandhi and S. Cumber
Vigilance Intelligence and Research Group, Vigilance and Risk Management of Medicines, Medicines and Healthcare products Regulatory Agency (MHRA), London, UK
Background:Spontaneous suspected ADRs are reported directly on a voluntary basis by Healthcare Professionals (HCPs) and since 2005 by patients through the Yellow Card Scheme (YCS). Reports are also received indirectly via the pharmaceutical industry who are legally required to report all fatal and serious ADRs. Information collected through the YCS is a vitally important pharmacovigilance tool, acting as an early warning system for the identification of signals. In 2008, MHRA launched an enhanced version of the electronic Yellow Card, to facilitate easier ADR reporting for patients and HCPs.
Aim:Through analysis of ADR data identify areas to focus the Yellow Card strategy to strengthen reporting in the UK.
Method:An analysis of UK ADR reports was performed using YCS data from the period of 2009 and 2010. All drugs were analysed by active substance using the MHRA’s drug dictionary and suspected reactions coded in MedDRA.
Results:2010, shows a 3.7% increase in the number of ADR reports received compared to 2009, including a 74% increase in patient reporting since 2005. Industry reports account for 48.3% of all reports with 13.5% of these derived from literature articles. 2010 has seen a 4% increase in electronic reporting. 70% of all patient reports were received electronically compared to 35% of HCP reports. Reporting from GPs, historically the largest group of reporters continues to decline accounting for 21.4% in 2010. Nurses are now the largest group at (23.7%) — a first since the Scheme was established (1964). Pharmacist reporting, mainly hospital based, increased by 16%. Most reported patient age group remains constant: 50–64 years. 16 Drug Safety Update articles based upon YCS data have been published, including: rivastigmine and medication errors, breast cancer with finasteride, antiepileptics and bone effects, and venous thrombotic events associated with antipsychotics. Further results of the analysis are shown in table I.
Conclusion:Analysis of ADR trends is important to inform Authorities where to target resource to raise awareness of reporting schemes and new initiatives such as electronic reporting. Sustained engagement with HCPs and patients is vital to ensure the continued success of the YCS and the effective monitoring and communication of drug safety issues.
PP233. One in Three Adverse Reactions Induced by Topical Antiglaucoma Medications is Systemic: Analysis of Adverse Drug Reactions Spontaneously Reported to Croatian Agency for Medicinal Products and Medical Devices
M. Banovac, A. Andric, V. Macolic Sarinic, N. Mirosevic Skvrce and S. Tomic
Agency for Medicinal Products and Medical Devices, Pharmacovigilance Department, Zagreb, Croatia
Objectives: The primary objective was to analyze the number and characteristics of spontaneously reported adverse drug reactions (ADRs) of antiglaucoma medications reported to the Agency for Medicinal Products and Medical Devices, with emphasis on the systemic adverse events of topical medications (primarily eye drops). The secondary objective was to relate the number of ADRs reported per class of antiglaucoma medications to the consumption of these medications.
Methods:We performed a retrospective analysis of all ADRs related to antiglaucoma medications according to the Anatomical-Therapeutic-Chemical drug classification (ATC). Analyzed ATC groups were: sympathomimetics in glaucoma therapy, carbonic anhydrase inhibitors, beta blocking agents and prostaglandin analogues. Croatian national ADR database — Vigiflow, version 4.2, was used as data source. Medical Dictionary for Drug Regulatory Affairs-MedDRA was used for coding of ADRs. We analyzed relative contribution of ADRs stratified by ATC, gender, System Organ Classes (SOCs), seriousness, type of reaction (systemic/local) and profession of the reporter. Seriousness was assessed using CIOMS V (Council for International Organizations of Medical Sciences) and European Medicines Agency’s Important Medical Events criteria. Descriptive statistical analysis was performed using SPSS 18.0.
Results:ATC groups found to cause the greatest number of ADRs were beta blocking agents (36.4%), prostaglandin analogues (29.5%), carbonic anhydrase inhibitors (20.5%) and sympathomimetics in glaucoma therapy (13.6%). Nevertheless, when we compared ADR share of ATC groups with their market share, results showed that sympathomimetics’ ADR share was over 3 times greater than their market share. There was a statistically significant difference (p < 0.0005) in reporting ratio of ADRs affecting women and men (4.2 : 1), although glaucoma prevalence is considered to be equal among genders.[1]
Mean age of patients which developed ADRs was 61,4. As expected, the great majority of ADRs were related to SOC “Eye disorders” (59%), after which “Nervous system disorders” (10%) and “Skin and subcutaneous tissue disorders” (6%) followed. In 30.7% of cases the reactions were systemic. Seven in 44 cases were assessed as serious. Opposite to standard reporting patterns in Croatia, most of the ADRs were reported by pharmacists (52.3%).
Conclusions:One in three ADRs induced by topical antiglaucoma medications have a systemic impact. Knowing that systemic absorption can be avoided by correct administration of eye drops, advice to patients during dispensing on correct administration is necessary to maximize treatment benefit and minimize ADRs. Paradoxically high percentage of sympathomimetics’ ADRs, as well as disproportionality of gender reporting ratio, need to be investigated more in depth.
PP234. Hospital Admissions Caused by Suspected Adverse Drug Reactions (ADRs) in a Hospital Clinical Medicine Unit in C′rdoba, Argentina
R. Herrera Comoglio,1 L. Alesso,1 G. Carelli,2 M. Garrido 2 and C. Nota 2
1 Pharmacovigilance Service, Hospital Nacional de Clínicas, Córdoba National University, Córdoba, Argentina; 2 Clinical Medicine Unit, Hospital Nacional de Clínicas, Córdoba National University, Córdoba, Argentina
Background:Adverse Drug Reactions (ADRs) are a substantial cause of hospital admission. Several studies have estimated the incidence of hospital admissions due to ADRs in developed countries.
Aim:to estimate the incidence of ADRs as cause admissions in a sample of clinical charts in a Hospital Clinical Medicine Unit in Argentina.
Material-Methods:Admission clinical charts’ data were collected pro-spectively from January 2011 to June 2011. Collection was not systematic, but it was aleatory. Data included: demographic data, symptoms causing hospital or emergency consultations, chronic and recent medication, medical history, laboratory, diagnostic and clinical findings; and diagnostic presumption. Data were analyzed in clinical reviews with senior and junior internists. Causality assessment was performed according WHO method. Drug-related admissions due to lack of compliance or unintentional overdose were excluded, but one suicidal attempt with deliberate neuroleptic overdose was considered as possible ADR.
Results:252 admission’s data (238 patients, 126 women and 112 men, age 55–93 yrs, mean age 77.5 yrs.) were analyzed. There were 37 admissions considered as directly related to an ADR (14.68%). Drugs classes most commonly implicated in causing these admissions included non-steroidal anti-inflammatory drugs (NSAIDs) (7) (18.2%) diuretics (7) (18.2%), oral hypoglycemic drugs and insulins (6) (16.21%), antiarrhythmics (5) (13.51%), neuroleptics (4) (10.81), antibiotics (3) (8.1%), benzodiazepines (2) (5.4%), antidepressants (2) (5.4%), tu-berculostatics (1) (2.7%), acetylcholinesterase inhibitor (1) (2.7%), immunossupressants (1) (2.7%). ADRs were assessed as probable in 23 cases, possible in 11 cases, definite in 2 cases, and conditional in one case (One suicidal attempt was considered as possible ADRs). Most frequent interactions included amiodarone and digoxin or beta-blockers (syncope); and several neuroleptics.
The most common ADRs were hyponatremia (8) (21.62%), severe anemia (7) (18.2%), hypoglycemia (5) (13.51%), syncope (5) (13.51%), severe central nervous system depression (4) ( 10.81), bradyarrhythmias (2) (5.4%). Hyponatremia was related to diuretics (4), antidepressants (venlafaxine) (2) antipsychotics (1), antibiotics (1) and diuretics and antidepressants (1). Severe anemia cases were all related with chronic NSAIDs. Severe central nervous system depression cases were related with psychiatric patients in chronic hospitalization.
Discussion:Data collection wasn’t systematic, only clinical Medicine Unit and Intensive Care Unit patients were included (no surgical, traumatology or neurology services admissions were analyzed).
Conclusion:ADRs are an important cause of directly related hospital admissions. Further systematic and larger studies will allow more accurate estimates of incidence and drug class relatedness of ADRs as cause of hospital admissions in developing countries settings.
PP235. Emergency Department Visits Caused by Adverse Drug Reactions: Results of a Turkish University Hospital
M.C. Girgin,1 S. Yanturali,1 A.M. Arici,2 N. Colak Oray,1 O. Doylan,1 Y. Demiral 3 and Y. Tuncok 4
1 Dokuz Eylul University School of Medicine, Department of Emergency Medicine, Izmir, Turkey; 2 Dokuz Eylul University School of Medicine, Department of Medical Pharmacology, Izmir, Turkey; 3 Dokuz Eylul University School of Medicine, Department of Public Health, Izmir, Turkey; 4 Dokuz Eylul University School of Medicine, Department of Medical Pharmacology, Division of Clinical Toxicology, Izmir, Turkey
Objectives:The frequency of adverse drug reactions (ADRs) lead to the emergency department (ED) visits was unknown in Turkey. Therefore, we aimed to investigate the frequency of ADRs related ED visits in Dokuz Eylul University Hospital.
Methods:In this prospective descriptive study, all patients older than 17 years old that were admitted to our ED during one-week periods of four different seasons between July 2010 and April 2011 were enrolled the study. We excluded the patients who have not taken any medication in the medical history during last 15 days. Demographics of the patients, main reason of the ED visit, medical history and last diagnosis, classification, duration and exposure route of the medication were recorded. Drug-drug and drug-food and drug-herbal product interactions were also evaluated. Data were evaluated by the project team. Causality assessment of ADRs was done according to WHO-UMC causality categories, and ADRs were categorized as certain, probable or possible.
Results:The number of all patients admitted to ED was 6928 during the study periods. Patients who have not any medication use were excluded from the study (n = 5090, 73.5%). Of the patients who are on medications, 26.5% (n= 1838) were evaluated for ADR-related ED admissions. Mean age was 51.5–20.2 (range 18–88). Male/female ratio was 0.83. Certain, probable and possible adverse drug reactions accounted for 5.8% (n= 108). The most frequently seen ADRs-related symptoms upon arrival were pruritus (19.4%, n = 21), abdominal pain (14.8%, n= 16) and diarrhea (10.2%, n=11). According to the main anatomic therapeutic classification (ATC), drugs that caused ADRs were antibacterials (30.6%, n = 33), anticoagulants (11.1%, n = 12), antiinflammatory drugs (10.2%, n = 11). We did not observe any ADR-related death in our study.
Conclusions:In our ED, nearly 6% of the admissions were medication-related ADRs. Our results showed that non-traumatic ED visits caused by ADRs are common. ADRs should always be considered ED patients who are on medication.
PP236. To Centralise or Not to Centralisey…That is the Question: A Pilot Project Analysis of Regional Pharmacovigilance Centres in the Czech Republic
V. Descikova 1 and J. Mlada 2
1 State Institute for Drug Control, Pharmacovigilance Department, Prague, Czech Republic; Charles University in Prague, Faculty of Pharmacy, Department of Social and Clinical Pharmacy, Hradec Kralove, Czech Republic; 2 State Institute for Drug Control, Pharmacovigilance Department, Prague, Czech Republic
Background:Pharmacovigilance in the Czech Republic has been centralised to one national centre located at the State Institute for Drug Control from its beginning in the 1960s. There has been a pioneer activity of two professors travelling from one healthcare centre to another in the 1980s which raised a slight interest about pharmacovigilance in our country, but this activity finished after 1989. In 2010, there was an idea of establishing Regional Pharmacovigilance Centres (RPhVC) in the area of the Czech Republic based on international experience across Europe.[1–3] The main goal of this project is to be closer to the healthcare professionals (HP) and patients and to be able to help them with recognition, prevention and reporting of adverse drug reactions (ADR).
Aim:The aim of this presentation is to describe an experience with RPhVC in the Czech Republic in the pilot phase of project. The pilot phase started in January 2011 and we would like to provide the first analysis of this impact on healthcare professionals.
Methods:In the pilot phase, Regional Pharmacovigilance Centres (RPhVC) were established in 6 of 14 regions all round the Czech Republic. They are located in the hospitals and the RPhVC staff include clinical pharmacologists or clinical pharmacists, each centre one person. Job description of RPhVC staff covers an education of healthcare professionals in the assigned region and a help with collecting and reporting of adverse drug reactions.
Results:This presentation will provide first analysis of reporting rates, quality and heterogeneity of reports and the impact of education in the period from January 2011 to October 2011. We are expecting higher reporting rate with higher heterogeneity and we are deeply interested in the opinion of healthcare professionals on RPhVC and education.
Conclusion:Based on international experience, decentralisation of pharmacovigilance should bring closer contact with HP with higher number of ADR reports in return and more educated HP with better knowledge of importance of pharmacovigilance and its tools.
PP237. Adverse Events Induced by Oral Contraceptives: A Review on Reported Cases to a National Pharmacovigilance Centre
N. Javidnikou and G. Shalviri
Iranian Adverse Drug Reaction Monitoring Center, Ministry of Health, Tehran, Iran
Background:Oral contraceptives are associated with several adverse events including thromboembolic and thrombotic disorders. Some studies suggested that the relative risk for developing fatal or nonfatal thromboembolism was 3–11 times greater in oral contraceptive users than in nonusers.
Purpose:To evaluate all registered adverse drug events induced by oral contraceptives in Iranian pharmacovigilance database. To detect preventable adverse events related to this class of medicines.
Method:All registered adverse drug events in Iranian pharmacovigilance database from 1998 through May 2011 were reviewed for adverse events induced by oral contraceptives. The extracted data were categorized based on factors related to patients, suspected medicines and adverse events. Assessment of system-organ classes, seriousness and causality of reactions was performed according to World Health Organization scale. Preventability of reported adverse events was analyzed based on Schumock questionnaire.
Results:A total of 225 cases were registered by the Center which was detected to be induced by oral contraceptives. Suspected medicines in these reports included oral contraceptive LD (128 cases), cyproterone compound (47 cases), ethinylestradiol desogestrel (18 cases), oral contraceptive HD (13 cases), cyproterone acetate (11 cases) and ethinylestradiol drospirenone (8 cases). The highest number of events has occurred in the age group of 21–30 years old (98 cases). Thromboembolic and thrombotic disorders (96 cases) were the most reported adverse event in total reported cases. A total of 90 cases (40%) were recognised to be preventable. Inappropriate use of the drug and incorrect self medication were the most reasons observed in detected preventable cases. There were 10 reports of death which was detected preventable in 8 cases. Cerebral thrombosis (5 cases), thromboembolism (2 cases), subarachnoid haemorrhage (2 cases) and convulsion (1 case) were reported adverse events in fatal reports.
Conclusion:Consumption of oral contraceptives may be associated with fatal adverse events. Contraceptive users should be well educated on contraindications and also the initial signs and symptoms of these reactions. Also these adverse drug events should be known by health care professionals and must be included in the differential diagnosis.
PP238. Reports Submitted to WHO-UMC by TUFAM through 2008/2009/2010: Elaborated Assessment of Adverse Reactions in Pediatric Population
E. Aykaç, D.N. Aydinkarahaliloğlu, Y Kasap, G. Sağiş, C. Babacanoğlu, H. Ilbars, H. Özbek and S. Kerman
General Directorate of Pharmaceuticals and Pharmacy, Ministry of Health, Ankara, Turkey
Background:Hence pediatric population is generally not included in clinical trials and drugs are often used off-label among pediatric patients, surveillance of drug safety is of particular importance in populations.[1]
Objective/aim:The aim was to specify the system organ class (SOC) of adverse drug reactions (ADRs) frequently seen in pediatric population and to specify the ATC codes of drug groups leading to these ADRs.
Method:TUFAM submits the ADRs to WHO database via Vigiflow. In this study, the SOCs related to the most commonly seen ADRs in neo-nate-infant-child-adolescent categories through 2008-2009-2010 were specified by using the excel format generated by the related WHO system.
Results:48 out of the 389 reports submitted in 2008 were observed in pediatric patients. For pediatric patients there were 73 ADRs within 48 case reports submitted to WHO in 2008. The SOC most commonly involved in reportings was “skin and appendages disorders” (21.9%). Among the drugs reported, “Antiinfectives for Systemic Use” in group “J” had the highest ranking with a proportion of 66%. 70 out of the 520 reports submitted in 2009 were observed in pediatric patients. For pediatric patients there were 122 ADRs within the 70 case reports submitted to WHO in 2009. The SOC most commonly involved in reportings was “body as a whole general disorders” with a proportion of 18.3%. “Antiinfectives for Systemic Use” in group “J” had the highest ranking among the drugs reported. 125 out of the 1000 reports submitted in 2010 were observed in pediatric patients. For pediatric patients there were 283 ADRs within the 125 case reports submitted to WHO in 2010. The SOC most commonly involved in reportings was “body as a whole general disorders” (13.8%). Based on the sorting of drug groups most commonly reported, “Antiinfectives for Systemic Use” in group “J” had the highest ranking with a proportion of 33.8%.
Conclusion:According to the assessment based on age groups, infants were the group with the highest number of ADR reports in all three years. Based on ATC classification, the drug class with the most frequent ADR reports was “J01 Antibacterials for Systemic Use” through all three years.
Discussion:It was observed that the drug class and the SOC most commonly involved in adverse reactions had remained the same through all three years.
PP239. Literature Reports Submitted to Turkish Pharmacovigilance Center (TUFAM) by Authorization Holders in 2010
G. Sağiş, C. Babacanoğlu, D.N. Aydinkarahaliloğlu, E. Aykaç, Y. Kasap, H. Ilbars, H. Özbek and S. Kerman
General Directorate of Pharmaceuticals and Pharmacy, Ministry of Health, Ankara, Turkey Background:In line with the regulation, the person responsible for drug safety is obliged to use the commonly used reference and systematic literature review databases at least once a week and review the Turkish based national information sources at least once a month, and obtain knowledge regarding the current publications.
Objective/aim:The aim of this study was to elaborately review the literature reports submitted to Turkish Pharmacovigilance Center (TUFAM) by authorization holders in 2010.
Method:The literature reports submitted to TUFAM in 2010 were recorded in excel format. The follow-up reports provided for literatures by the companies were not included in the study. When there is more than one case in one literature, the number of literatures reported by the companies equals to the number of cases. Since the cases were derived from the same literature, it was considered as a single report in our study.
Results:TUFAM received a total of 550 literature reports including 503 drug substances in 2010. According to the assessment based on drugs involved in literature reports, the most commonly reported drugs were risperidone (N05AX08), valproic acid (N03AG01), tacrolimus (L04AD02), paracetamol (N02BE01) and paroxetine (N06AB05), respectively. The national periodical publication with the highest number of TUFAM reports was “Journal of Clinical Psychopharmacology” while the international periodical publication was “Medical Oncology”. According to the assessment of drug groups based on ATC codes, the drugs most commonly involved in reports were “nervous system” in group N (33.6%), followed by “antineoplastics and immunomodulating agents” in group “L” (24.3%) and “antiinfectives for systemic use” in group “J” (15.2%).
Conclusion:Among the safety matters subjected to TUFAM agenda in 2010, the first three drug groups were as follows “antineoplastics and immunomodulating agents” in group “L”, ”nervous system” in group N and “antiinfectives for systemic use” in group “J”. This shows the correlation between the drug groups subjected to TUFAM agenda and the drug groups involved in the literature.
Discussion:We conclude that the authorization holders show more compliance to their pharmacovigilance obligations through each year and this compliance is considered to be associated in part with our educational studies.
PP240. Place of Imatinib Plasmatic Level in the Management of Cutaneous Side Effects Induced by Imatinib (Glivec®): Two Cases Studies
E. Gaies, S.Trabelsi, S.Srairi, I.Salouage, R. Charfi, N.Jebabli, R. Daghfous, M. Lakhal and A. Klouz
Service de Pharmacologie Clinique-Centre National de Pharmacovigilance, Tunis, Tunisia
Imatinib an antineoplastic drug approved for the treatment of Chronic Myelogenous Leukemia (CML) and Gastrointestinal Stromal Tumors (GISTs). This drug improved significantly the prognosis of these diseases, however it has many side effects such as hematologic, neurologic or cutaneous toxicity.[1] These toxicities seemed to be due to a high imatinib plasmatic concentration and are frequently controlled by a discontinuation or a dosage reduction of the drug.
We report herein 2 cases of cutaneous side effects induced by imatinib and illustrated by a high plasmatic concentration.
The first CASE: a T. MF 68 years old man having a GIST and treated by Glivec® (400mg/d) since October 2009. Twenty days after the beginning of the treatment, he presented a periorbital oedema followed by an eczemato-psoriasiform eruption 2 months later. This eruption was treated by administration of local steroids and Glivec® was not stopped. These side effects seemed due to Imatinib and so therapeutic monitoring of this drug was been required. Plasmatic levels measured by HPLC showed a concentration about 1792ng/mL.
The second case: a G.D 50-year-old woman, having a CML and treated by Glivec® (400 mg/d) since September 2009. Seventy five days after imatinib introduction, the patient developed a lichenoid eruption. She was treated by local steroids and lesions were resolved without discontinuation of imatinib. This lichenoid eruption seemed also due to imatinib. Plasmatic level was 1094ng/mL.
In our cases imatinib concentration is >1000ng/mL and may explain the occurrence of these side effects. We did not need to withdraw imatinib because of the regression of the eruption under symptomatic treatment. So monitoring plasma levels of imatinib allows us to control toxic side effects and to adjust dosage if necessary.
PP241. Activity of Pharmacovigilance Unit of Ibn Rochd University Hospital for 2010 (Kingdom of Morocco)
A. Elrherbi, A. Meftah, M.E. Elkarimi, I. Rahmoun, D. M’ zah, H. Fi lali, A. Tazi and F. Hakkou
Pharmacology Departement of Chu Ibn Rochd, Casablanca, Morocco
Objective: To present an overview of adverse drug reactions (ADR) reporting of Pharmacovigilance unit of Ibn Rochd university hospital for 2010.
Material-methods: our activity consists to notify, record and analyze each adverse reaction seeming to be induced by treatment medication reported by physicians from different departments of the hospital even spontaneously or after sensitization by pharmacovigilance physicians using the WHO causality ADR Assessment.
Result: Among 301 reported case of ADR, 220 ADR were characterized as Serious ADR with 4 cases of fatal issue. Classification of all reports according to System Organ Class indicated that most adverse events reported were of the ‘Skin and Appendages Disorders’ SOC (30.2%) followed by ‘liver disorders ‘ SOC (15.6%) and ‘Central and Peripheral Nervous System Disorder’ SOC (9.96%). More than half (56.9%) of reports have been associated to drugs from the following three pharmacological groups: Cardiovascular (26.1 %), Anti-infective (21.0%) and Analgesic (9.8%).
Conclusion: More efforts must to be completed to improve Moroccan pharmacovigilance system As well in the organizational terms as in the functional terms.
PP242. Cerebral Hemorrhages with Vitamin K Antagonists: A Prospective Study Over 5 Years in a French Neurosurgical Unit
Background: Bleeding is the major serious adverse drug reaction (ADR) of vitamin K antagonists (VKA), drugs widely used in France with 900000 patients treated. Pharmaco-epidemiological studies in France have demonstrated that VKA were leading drug related to hospital admissions. Cerebral hemorrhages (CH) are especially dreaded because of their fatal outcome.
Objective/aim: The present study was performed in order to describe the main characteristics of cerebral hemorrhages related to VKA reported to a French Regional Centre of Pharmacovigilance (RCPV) of patients hospitalized in a Neurosurgical unit.
Methods: We developed a specific notification form for this study. This work was conducted in the Neurosurgical unit between 1st January 2006 and 31st December 2010. Each patient hospitalized for CH was included. We registered the main characteristics of patients (age, gender), VKA (nature, indication), INR values, seriousness and medical issue. All concomitant drugs were collected.
Results: 56 patients were included. Their mean age was 79± 9 years, 73.6% were men. Recent fall was found in 56% of cases. Fluindione was the VKA most frequently implied (85%). The VKA prescription was off-label use in four cases. All ADR were serious of which 15 were lethal (26%). INR value was outside the therapeutic range in 59% of patients. The mean value of INR was higher in patients who died (maximal value >9). Patients had an average of four drugs (1–13) associated with the anticoagulant therapy. The most frequently associated pharmacological classes were antihypertensive drugs (22% of patients) and class 3 antiarrhythmics (13%). The average number of antihypertensive was higher in the group of patients who died. A drug interaction was involved in 56% of patients. An antithrombotic treatment was associated in 8 patients (mortality 50%).
Discussion/conclusion: We show that CH related to VKA is a serious adverse effect observed in polymedicated hypertensive old patients suffering from a recent fall. This study confirms the high prevalence of death in patients treated by anticoagulants with CH. Drug interaction were involved in bleedings in one case out of two. In this work, INR values strongly suggest that an important part of CH can be prevented by a better management of the treatment.
PP243. Lidocaine-Induced Neurotoxicity: A Case Report
E. Gaies, N. Jebabli, S. Trabelsi, I. Salouage, R. Charfi, M. Lakhal and A. Klouz
Service de Pharmacologie Clinique-Centre National de Pharmacovigilance, Tunis, Tunisia
Lidocaine is an amide type local anesthetic. It is the most commonly used local anesthetic in pediatric patients because of it’s rapid onset, moderate duration of action and topical activity. Unfortunately, systemic intoxication and neurologic reactions associated with its use occur frequently.[1] Neurologic toxicity occurs when lidocaine blood concentration reach 5–10mg/mL. Coma and cardiac arrest are observed when lidocaine concentration exceed 20 mg/mL.
We report here a case of neurologic intoxication induced by lidocaine during circumcision with blood concentration >20 mg/mL.
A 45 days newborn, weighing 3.56 kg, underwent circumcision under penile block with 2% lidocaine. Two hours after injection the patient developed generalized hypotonia with eyeball revulsion. Cardiotoxicty was not observed and neurologic signs were controlled by phenobarbital. Lidocaine systemic intoxication was suspected and its blood concentration was measured by HPLC method, 18 hours after the drug administration. Lidocaine concentration was 63.42 mg/mL. The newborn improved and there were no recurrence of these neurologic signs.
In our case lidocaine concentration is largely above 20 mg/mL and the newborn presents only minor neurologic toxic reactions. We confirm so the large inter and intravariability of lidocaine pharmacokinetics and that its toxicity threshold is different in patients.
References
Volume 9A of The Rules Governing Medicinal Products in the European Union — Guidelines on Pharmacovigilance for Medicinal Products for Human Use. European Commission, September 2008
ICH Harmonised Tripartite Guideline E2E: Pharmacovigilance Planning, International Conference on Harmonisation, November 2004
Guidance for Industry: Format and Content of Proposed Risk Evaluation and Mitigation Strategies (REMS), REMS Assessments, and Proposed REMS Modifications, draft guidance. Food and Drug Administration, September 2009
References
Guideline on Risk Management Systems for Medicinal Products for Human Use: Ref: EMEA/CHMP/96268/2005
Department of Health & Human Services. Food and Drug Administration (Docket No: FDA-2008-N-0174). Identification of Drug and Biological Products Deemed to Have Risk Evaluation and Mitigation Strategies for Purposes of the Food and Drug Administration Amendments Act of 2007
Banerjee S, Barr B. Risk Rationale. Pharma needs a culture of proactive pharmacovigilance and risk minimisation. Pharmaceutical Marketing 2007; July/August: 22–23
References
Am J Health-Syst Pharm, Vol 67, September 15, 2010, p 1511
Am J Health-Syst Pharm, Vol 67, September 15, 2010, p 1511
References
Hauben M, Aronson JK. Defining ‘Signal’ and its Subtypes in Pharmacovigilance Based on a Systematic Review of Previous Definitions. Drug Saf 2009; 32(2): 99–110
References
Slade BA, Leidel L, Vellozzi C, et al. Postlicensure safety surveillance for quadrivalent human papillomavirus recombinant vaccine. JAMA 2009; 302(7): 750–7
Dorleans F, Giambi C, Dematte L, et al., on behalf of the VENICE 2 project gatekeepers group. The current state of introduction of human papillomavirus vaccination into national immunisation schedules in Europe: first results of the VENICE2 2010 survey. Euro Surveill. 2010;15 (47): pii= 19730. Available online: http://www.eurosurveillance.org
References
Settimana Europea della Vaccinazione. Aprile 2011. http://www.salute.gov.it
Licensure of a 13-valent pneumococcal conjugate vaccine (PCV13) and recommendations for use among children — Advisory Committee on Immunization Practices (ACIP), 2010. Centers for Disease Control and Prevention (CDC).MMWR Morb Mortal Wkly Rep. 2010 Mar 12; 59(9): 258–61
References
Hazell L, Shakir SA. Under-reporting of adverse drug reactions: a systematic review. Drug Saf 2006; 29(5): 385–96
Herdeiro MT, Figueiras A, Polonia J, et al. Physicians’ attitudes and adverse drug reaction reporting: a case-control study in Portugal. Drug Safety: An International Journal of Medical Toxicology and Drug Experience. 2005; 28(9): 825–33
Inman W. Assessment drug safety problems. MSIG, editor. 1976
Davis D, Thomson M, Oxman A, et al. Changing physicians performance. A systematic review of the effect of continuing medical education strategies. JAMA 1995; 274(9): 700–5
Figueiras A, Herdeiro MT, Polonia J, et al. An educational intervention to improve physician reporting of adverse drug reactions: a cluster-randomized controlled trial. JAMA 2006 Sep 6; 296(9): 1086–93
References
McLernon DJ, et al. Pharmacoepidemiol Drug Saf 2011; 20: 523–31
Basch E. N Engl J Med 2010; 362: 865–9
Sottosanti L. Reazioni 2009; 3: 8
References
Muret P. Iatrogénie médicamenteuse: FMC Montbéliard; Juin 2008; Pharmacologie Clinique et Toxicologie; CHU Besançon
Detournay B, et al. Coût des hospitalisations pour effets indésirables médicamenteux. Thérapie 2000; 55: 137–9
Bates DW, Leape LL, et Petrycki S. Incidence and preventability of adverse drug events in hospitalized adults. J Gen Intern Med 1993; 8: 289–94
Bates DW, Cullen DJ, Laird N, et al. Incidence of adverse drug events and potential adverse drug events. J Am Med Assoc 1995; 274(1): 29–34
Bates DW, Boyle DL, Van der Vliet MB, et al. Relationship between medication errors and adverse drug events. J Gen Intern Med 1995; 10: 199–205
References
Cephalon. Effentora 100, 200, 400, 600 and 800 micrograms buccal tablets: Summary of Product Characteristics, January 2009
References
European Commission: Community Register [online]. Available from URL http://ec.europa.eu [Accessed September 30 2010]
References
Institute for Safe Medication Practices. 2011. FDA and ISMP Lists of Look-Alike Drug Names with Recommended Tall Man Letters. Available from URL: http://www.ismp.org/tools/tallmanletters.pdf [Accessed June 12, 2011]
Gabriele S. The Role of Typography in Differentiating Look-Alike/ Sound-Alike Drug Names. Special Issue, Patient Safety Papers 2, Healthcare Quarterly 2006; 9: 88–95
Reference
Aronson JK. Medication errors: definitions and classification. Br J Clin Pharmacol 2009 Jun; 67(6): 599–604
References
Millenson ML. Pushing the profession: how the news media turned patient safety into a priority. Qual Saf Health Care 2002; 11: 57–6
References
Expert group on Safe Medication Practices. Creation of a better medication safety culture in Europe: building up safe medication practices [online]. Available from URL: http://www.gslhealth.net/downloads/medication.safety.report.2007
References
National Patient Safety Agency. Rapid Response Report: Reducing harm from omitted and delayed medicines in hospital. NPSA/2010/ RRR 009. London: NPSA, February 2010 [online]. Available from URL: http://www.nrls.npsa.nhs.uk [Accessed 2011 Jun 30]
Barker KN, Flynn EA, Pepper GA, et al. Medication errors observed in 36 health care facilities. Arch Intern Med 2002; 162(16): 1897–903
References
Granger Morgan M, Fischhoff B, Bostrom A, et al. Risk communication: a mental models approach. Cambridge: Cambridge University Press, 2002
Slovic P. The feeling of risk: new perspectives on risk perception. London, Washington DC: Earthscan, 2010
References
European Medicines Agency finalises review of antidepressants in children and adolescents [online]. Available from URL: http://www.ema.europa.eu
References
Regulation (EU) No. 1235/2010 of the European Parliament and of the Council of 15 December 2010 amending, as regards pharmacovigilance of medicinal products for human use, Regulation (EC) No 726/2004 laying down the Community procedures for the authorization and supervision of medicinal products for human and veterinary use and establishing a European Medicines Agency, and Regulation (EC) 1394/2007 on advances therapy medicinal products
Directive 2010/84/EU of the European Parliament and of the Council of 15 December 2010 amending, as regards pharmacovigilance, Directive 2001/83/EC on the Community code relating to medicinal products for human use
International Conference of Harmonization of technical requirements for registration of pharmaceuticals for human use. Final Business Plan. Periodic Safety Update Reports for Marketed Drugs E2C (R2) and gap and potential improvement analysis of ICH E2C, E2E and E2F. 10 December 2010
International Conference of Harmonization of technical requirements for registration of pharmaceuticals for human use. Clinical Safety Data Management: Periodic Safety Update Reports for Marketed Drug E2C (R1). 6 November 2006
International Conference of Harmonization of technical requirements for registration of pharmaceuticals for human use. Developmental Safety Update Report E2F. Step 4 version 17 August 2010
European Medicines Agency Annex C: Template for EU Risk Management Plan (EU-RMP). 27 September 2009
References
Patient support programmes
Volume 9a
References
Butt TF, Cox AR, Lewis H, et al. Patient experiences of Serious Adverse Drug Reactions and their attitudes to Medicines. A qualitative study of survivors of Stevens-Johnson Syndrome and Toxic Epidermal Necrolysis in the UK. Drug Safety 2011; 34(4): 319–28
References
Knoblauch A, et al., SAeZ 2010; 91: 47
Schiff GD, et al., Arch Intern Med 2009; 169: 1881–7
Lidegaard O, et al., BMJ 2009; 339: b2890
Parkin L, et al., BMJ 2011; 340: d2139
Jick S, et al.,BMJ 2011; 340: d2151
References
1. Brown EG, Goldman SA. Preparing for regulatory inspection of company pharmacovigilance systems and practices in the EU and US. In: Carson PA, Dent NJ, editors. Good Clinical, Laboratory and Manufacturing Practices: Techniques for the QA Professional. Royal Society of Chemistry, 2007
2. Procedure for conducting pharmacovigilance inspections requested by the CHMP. GCP Inspectors Working Group. EMEA/INS/GCP/218148/ 2007, Procedure no: INS/PhV/2, November 2007
3. Optimizing drug safety monitoring to enhance patient safety and achieve better health outcomes. Monitoring Medicines [online]. Available from URL: http://www.monitoringmedicines.org. [Accessed 31 May, 2011]
4. Brown EG, Brown L, Stevens D. A customised game as an aid for medical representative training. In: Burley D, Haward C, Mullinger B, editors. The focus for pharmaceutical knowledge. Macmillan Press, 1988: 293–300
References
Ahmed OH, Sullivan SJ, Schneiders AG, et al. Concussion information online: evaluation of information quality, content and readability of concussion-related websites. British Journal of Sports Medicine. Epub 2011 Apr 18
Fusier I, Tollier C, Husson M, et al. Infovigilance: Impact on the summary product characteristics contents. [Infovigilance: Impact sur le contenu des résumés des caractéristiques du produit]. Journal De Pharmacie Clinique 2004; 23(2): 69–74
Fusier I, Tollier C, Husson M, et al. Infovigilance: Reporting errors in official drug information sources. Pharmacy World and Science 2005; 27(3): 166–9
Moreno JM, Morales del Castillo JM, Porcel C, et al. A quality evaluation methodology for health-related websites based on a 2-tuple fuzzy linguistic approach. Soft Computing 2010; 14(8): 887–97
Schmidt MM, Sharma A, Schifano F, et al. “Legal highs” on the net-evaluation of UK-based websites, products and product information. Forensic Science International 2011; 206(1–3): 92–7
References
Johannessen LC, Larsson PG, Rytter E, et al. Antiepileptic drugs in epilepsy and other disorders-a population-based study of prescriptions. Epilepsy Res 2009; 87(1): 31–9
Savica R, Beghi E, Mazzaglia G, et al. Prescribing patterns of antiepileptic drugs in Italy: a nationwide population-based study in the years 2000–2005. Eur J Neurol 2007; 14(12): 1317–21
References
Volume 9A of The Rules Governing Medicinal Products in the European Union — Guidelines on Pharmacovigilance for Medicinal Products for Human Use — 2008
Directive 2010/84/EU of the European Parliament and of the Council of 15 December 2010 — amending, as regards pharmacovigilance, Directive 2001/83/EC on the Community code relating to medicinal products for human use
References
Hazell L. Under-reporting of adverse drug reactions: a systematic review. Drug Saf 2006; 29(5): 385–96
Lopez-Gonzalez E, Herdeiro MT, Figueiras A. Determinants of underreporting of adverse drug reactions: a systematic review. Drug Saf 2009; 32(1): 19–31
Berniker Jessamyn S., Spontaneous Reporting Systems: Achieving Less Spontaneity and More Reporting [online]. Available from Leda at Harvard Law School. http://leda.law.harvard.edu [Accessed 22 June 2011]
References
van Grootheest K, Vrieling T. Thromboembolism associated with the new contraceptive Yasmin. BMJ 2003; 326: 257
Dinger JC, Heinemann LA, Kühl-Habich D. The safety of a drospirenone-containing oral contraceptive: final results from the European Active Surveillance Study on oral contraceptives based on 142475 women-years of observation. Contraception. 2007 May; 75(5): 344–54
Jick SS, Hernandez RK. Risk of non-fatal venous thromboembolism in women using oral contraceptives containing drospirenone compared with women using oral contraceptives containing levonorgestrel: case-control study using United States claims data. BMJ 2011 Apr 21; 342: d2151
Parkin L, Sharples K, Hernandez RK, et al. Risk of venous thromboembolism in users of oral contraceptives containing drospirenone or levonorgestrel: nested case-control study based on UK General Practice Research Database. BMJ. 2011 Apr 21; 342: d2139
References
Chalasani N, Björnsson E. Risk factors for idiosyncratic drug-induced liver injury. Gastroenterology 2010; 138(7): 2246–59
Andrade RJ, Lucena MI, Fernández MC, et al. Drug-induced liver injury: an analysis of 461 incidences submitted to the Spanish registry over a 10-year period. Gastroenterology 2005; 129(2): 512–521
Lucena MI, Andrade RJ, Kaplowitz N, et al. Phenotypic characterization of idiosyncratic drug-induced liver injury: the influence of age and gender. Hepatology 2009; 49: 2001–9
References
WHO, Weekly epidemiological record, N° 8, 2006
WHO, Control of the Human African Trypanosomiasis: a strategy for the African region, 2005
Reference
Report of an independent review of access to the Yellow Card scheme. The Stationary Office, 2004
Reference
SPC for Focetria. [online]. Available from URL: http://www.ema.europa.eu/ [Accessed 2010 June]
References
JAMA 2004; 292(3): 351–7
Pediatrics 2010; 126: e1–8
References
Settimana Europea della Vaccinazione. Aprile 2011 [online. Available from URL: http://www.salute.gov.it
Centers for Disease Control and Prevention (CDC). Licensure of a 13-valent pneumococcal conjugate vaccine (PCV13) and recommendations for use among children — Advisory Committee on Immunization Practices (ACIP), 2010. MMWR Morb Mortal Wkly Rep 2010 Mar 12; 59(9): 258–61
Reference
HCSP. Recommandations sur les priorités sanitaires d’utilisation des vaccins pandémiques dirigés contre le virus grippal A(H1N1)v [online]. Available from URL: http://www.hcsp.fr
References
World Health Organisation. Current World Health Organisation phase of pandemic alert. WHO website [online]. Available from URL: http://www.who.int [Accessed 2010 Apr 25]
Ferguson NM, Cummings DA, Fraser C, et al. Strategies for mitigating an influenza pandemic. Nature 2006; 442(7101): 448–52
Ministry of Health National Intersectorial Pandemic Intervention Plan [online]. Available from URL: http://www.ms.ro [Accessed 2009 22 Nov]
Summary of Product Characteristics: Cantgrip® vaccine [online]. Available from URL: http://www.anm.ro [Accessed 2009 Nov 30]
Reference
The Brighton collaboration local reactions working group for abscess at injection site “Abscess at injection site: case definition and guidelines for collection, analysis, and presentation of immunization safety data” science direct Vaccine 2007; 25: 5821–38
Reference
Montastruc JL, Sommet A, Bagheri H, et al. Benefits and Strengths of the disproportionality analysis for identification of Adverse Drug Reactions in a PharmacoVigilance database. Br J Clin Pharmacol. Epub 2011 Jun 10
Reference
TUFAM database
Reference
Meyler’s side effects of drugs, 15th edition
Reference
BMJ 2010; 340: c2419
References
Mehta U, Durrheim D, Mabuza A, et al. Malaria Pharmacovigilance in Africa. Lessons from a Pilot Project in Mpumalanga Province, South Africa. Drug safety 2007; 30(10): 899–910
Parthasarathi G, Niveditha H, Harugeri A, et al. Adverse Drug Reactions to Anti-Tuberculosis Therapy in a Public Healthcare Programme of India. Drug safety 2010; 33(10): 916
Nartey ET, Kudzi W, Obeng Adjei G, et al. Is Artesunate-Amodiaquine Associated with More Adverse Drug Events Compared with the Other Anti-Malarial Therapies? Drug safety 2010; 33(10): 958
References
Koduri PR, Parekh S. Zidovudine-related anemia with recticulocytosis. Ann Hematol 2003; 82(3): 184–5
Curkendall SM, Richardson JT, Emons MF, et al. Incidence of anaemia among HIV-infected patients treated with highly active antiretroviral therapy. HIV Med 2007; 8(8): 483–90
Naranjo CA, Busto U, Sellers EM. “A method for estimating the probability of adverse drug reactions”. Clin Pharmacol Ther 1981; 30(2): 239–45
References
Eris-Gülbay B, Ural Gürkan Ö, Akkoca Yildiz Ö, et al. Side effects due to primary antituberculosis drugs during the initial phase of therapy in 1149 hospitalized patients for tuberculosis. Respiratory Medicine 2006; 100: 1834–42
Yee D, Valiquette C, Pelletier M, et al. Incidence of Serious Side Effects from First-Line Antituberculosis Drugs among Patients Treated for Active Tuberculosis. Am J Respir Crit Care Med 2003; 167: 1472–7
Schaberg T, Rebhan K, Lode H. Risk factors for side-effects of isoniazid, rifampin and pyrazinamide in patients hospitalized for pulmonary tuberculosis. Eur Respir J 1996; 9: 2026–30
References
Ghana Health Service, 2004. WHO Anti-malarial drug combination therapy: Report of a WHO technical consultation. [Document WHO/CDS/RBM/2001.35]. Geneva
Talisuna AO, Staedke SG, D’Alessandro U. Pharmacovigilance of antimalarial treatment in Africa: is it possible? Malar J 2006; 5: 50
Update on the efficacy, effectiveness and safety of artemether-lumefantrine combination therapy for treatment of uncomplicated malaria
Reference
Mirochnick M, Best BM, Clarke DF. Antiretroviral pharmacology: special issues regarding pregnant women and neonates. Clin Perinatol 2010 Dec; 37(4): 907–27
Reference
WHO, Mobilizing resources for pharmacovigilance, Report of the Thirty-Second Annual Meeting of Representatives of National Centres Participating in the Who Programme for International Drug Monitoring; 2009 Nov 2–5; Rabat, Morocco: 41–43
Reference
1. National Medicine Agency. Informative Bulletin No.24/2007 [online]. Available from URL: http://www.anm.ro
References
Harmark L, van Grootheest AC. Pharmacovigilance: methods, recent developments and future perspectives. Eur J Clin Pharmacol 2008; 64(8): 743–52
Hazell L, Shakir SA. Under-reporting of adverse drug reactions: a systematic review. Drug Saf 2006; 29(5): 385–96
Lopez-Gonzalez E, Herdeiro MT, Figueiras A. Determinants of underreporting of adverse drug reactions: a systematic review. Drug Saf 2009; 32(1): 19–31
References
WHO, Marketing Authorization of Pharmaceutical Products with Special Reference to Multisource (Generic) Products: A Manual for Drug Regulatory Authorities — Regulatory Support Series No. 005 (1998; 213 pages)
NMPB, the General Requirements for the Registration of Pharmaceutical Products in Sudan. 2009
References
Meyboom RHB, Egberts Antonie CG, Gribnau Frank WJ. Pharmacovigilance in Perspective. Drug Saf 1999; 6: 429–47
Gholami K, Parsa S, Shalviri G, et al. Anti-infective induced adverse drug reactions in hospitalized patients. Pharmacoepidemiology and Drug Safety 2005; 14: 501–6
Brix HS, Viktil KK, Moger TA, et al. Risk of drug related problems for various antibiotics in hospital: assessment by use of a novel methods. Pharmacoepidemiology and Drug Safety 2008; 17: 834–41
Slide presentation entitled Pharmacovigilance by Selfert Harry A., presented at the 26th International conference on Pharmacoepidemiology and Therapeutic risk management, 19–22 August 2010, Brighton, UK
http://www.thompsonhc.com [Accessed 2010 Oct 3]
WHO terminology for pharmacovigilance and adverse drug reaction
Abstract of the 6th International Society of Pharmacovigilance at Reims, France, 2–6 November 2010
Thaivigibase, the adverse reaction reports database. Health product Vigilance Center, Food and Drug Administration, Thailand [Accessed 2010 oct 4]
TB patient disease surveillance database from National Disease Surveillance, Bureau of Epidemiology, Ministry of Public Health
Reference
Pharmacoepidemiol Drug Saf 2009; 18: 910–5
References
Borges S, Desta Z, Li L, et al. Quantitative effect of CYP2D6 genotype and inhibitors on TMX metabolism: Implication for optimization of breast cancer treatment. Clin Pharmacol Ther 2006; 80: 61–74
Loprinzi C, Zahasky K, Sloan G, et al. TMX induced hot flashes. Clin Breast Cancer 2000; 1: 52–6
Henry NL, Stearns V, Flockhart DA, et al. Drug interactions and pharmacogenomics in the treatment of breast cancer and depression. Am J Psychiatry. 2010; 165: 10
Jin Y, Desta Z, Stearns V, et al. CYP2D6 genotype, antidepressant use, and TMX metabolism during adjuvant breast cancer treatment. J Natl Cancer Inst 2005; 97(1): 30–9
Becquemont L, Alfirevic A, Amstutz U, et al. Practical recommendations for pharmacogenomics-based prescription: 2010 ESF-UB Conference on Pharmacogenetics and Pharmacogenomics. Pharmacogenomics 2011; 12(1): 113–24
Dezentjé VO, Van Blijderveen NJC, Gelderblom H, et al. Effect of concomitant CYP2D6 inhibitor use and tamoxifen adherence on breast cancer recurrence in early-stage breast cancer. J Clin Oncol 2010; 10; 28(14): 2423–9
References
Foisy MM, Yakiwchuk EM, Hughes CA. Induction effects of ritonavir: implications for drug interactions. Ann Pharmacother 2008; 42(7): 1048–59
Touzot M, Le Beller C, Touzot F, et al. Dramatic interaction between levothyroxine and lopinavir/ritonavir in a HIV-infected patient. AIDS 2006; 12; 20: 1210–2
Tseng A, Fletcher D. Interaction between ritonavir and levothyroxine. AIDS 1998; 12: 2235–6
References
Mehta U, Durrheim D, Mabuza A, et al. Malaria Pharmacovigilance in Africa. Lessons from a Pilot Project in Mpumalanga Province, South Africa. Drug safety 2007; 30(10): 899–910
WHO. World Malaria Report 2008. Geneva: WHO, 2008
Parthasarathi G, Niveditha H, Harugeri A, et al. Integrating Pharmacovigilance in Revised National Tuberculosis Control Programme of India: A Pilot Study. Drug safety 2010; 33(10): 915–6
Reference
Bégaud B, Evreux JC, Jouglard J, et al. Imputabilité des effets inattendus ou toxiques des médicaments. Actualisation de la méthode utilisée en France. Thérapie 1985; 40: 111–8
Reference
Bégaud B, Evreux JC, Jouglard J, et al. Imputabilité des effets inattendus ou toxiques des médicaments. Actualisation de la méthode utilisée en France. Thérapie 1985; 40: 111–8
References
Eleana González Infante, 2001, Desarrollo Químico y Galénico de la Talidomida como medicamento huérfano. Tesis doctoral: Universidad Complutense de Madrid (Facultad de Farmacia). Madrid
Mellin G, Katzenstein M. The saga of thalidomide: neuropathy to embryopathy with case reports and congenital abnormalities. N Engl J Med 1962; 267: 1184–93
Gonzalez Capdevila G, Korzewycz N, Beragua R. (farmacéuticas, área de farmacovigilancia del Hospital Italiano de Buenos Aires). ¿Qué es la farmacovigilancia y a quienes compete? Evid Actual Pract Ambul 2004; 7: 162–3
The AAPS Journal 2005; 7. Steven K.Teo. Properties of Thalidomide and its Analogues: Implications for Anticancer Therapy
Sirohi B, et al. Multiple Myeloma. The Lancet 2004; 363: 875–87
Cardona R. Salud, tiempos y personajes a manera de semblanza: Elly Silberpfening de Holz (1910–2005). Rev Inst Nac Hig 2004; 35(2): 40–2
References
Einarson TR. Drug related hospital admission. Ann Pharmacother 1993; 27: 832–40
Prommeenate W. Cost-benefit analysis of adverse drug reaction monitoring program at Lerdsin hospital in 1999 [Thesis of the degree of Master of Science in Pharmacy]. Bangkok: Faculty of Pharmacy Mahidol University; 2000
References
Aksu B. Innovative pharmaceutical manufacturing applications on the manufacturing process for the tablets containing ramipril as drug substance. Turkey: Ege University, 2010
INFORM Intelligent Formulation. UK: Intelligensys Ltd., 2009
Singh SK, Venkateshwaran TG, Simmons SP. Oral controlled drug delivery: Quality by design (QbD) approach to drug development, oral controlled release formulation design and drug delivery: Theory to practice, John Wiley & Sons, Inc, 2010
References
Rollason V, Vogt N. Reduction of polypharmacy in the elderly: A systematic review of the role of the pharmacist. Drugs and Agin 2003; 20: 817–32
Mclean AJ, Couteur DG. Aging biology and geriatric clinical pharmacology. Pharmacological Reviews 2004; 56: 163–84
Kennerfalk A, ruigo’mez A, Wallander MA, et al. Geriatric drug therapy and healthcare utilization in the United Kingdom. Annals of Pharmacotherapy 2002; 36: 797–803
Linjakumpu T, Hartikainen S, Klaukka T, et al. Use of medications and polypharmacy are increasing among the elderly. Journal of Clinical Epidemiology 2002; 55: 809–17
Blakey SA, Hixson-Wallace JA. Clinical and economic effects of pharmacy services in a geriatric ambulatory clinic. Pharmacotherapy 2002; 20: 1198–203
Hanlon JT, Weinberger M, Samsa GP, et al. A randomized, controlled trial of a clinical pharmacist intervention to improve inappropriate prescribing in elderly outpatients with polypharmacy. American Journal of Medicine 1996; 100: 428–37
References
Alj L, Touzani MDW, Benkirane R, et al. Detecting medication error in pharmacovigilance database: capacities and limits. International Jourrnal of Risk and Sadety in Medicine 2007; 19: 187–94
Caduff-Janosa P. Medication errors in Switzerland: an analysis of the spontaneous adverse reaction reports received at the Swissmedic Pharmacovigilance Centre. Drug Safety 2004; 27: 831–977
Kunac Desireé L, Tatley Michael V. Detecting Medication Errors in the New Zealand Pharmacovigilance Database: A Retrospective Analysis. Drug Safety 2011 Jan 1; 34(1): 59–71
References
Soulaymani Bencheikh R, Benabdallah G. Medication errors: pharmacovigilance centres in detection and prevention. Br J Clin Pharmacol 2009 Jun; 67(6): 687–90
Benabdallah G, Benkirane R, Khattabi A, et al. The involvement of pharmacovigilance centres in medication errors detection: a questionnaire-based analysis. International Journal of Risk and Safety in Medicine 2011; 23: 17–29
References
http://www.afssaps.fr
Kiekkas P, et al. Medication errors in critically ill adults: a review of direct observation evidence. Am J Crit Care 2011 Jan; 20(1): 36–44
Mahajan RP. Medication errors: can we prevent them? Br J Anaesth 2011 Jul; 107(1): 3–5
Reference
Tamim H, et al. Application of lag time into exposure definitions to control for protopathic bias. Pharmacoepidemiology and Drug Safety 2007; 16: 250–8
References
Taylor J, et al. Ipratropium Bromide Hydrofluroalkane inhalation aerosol is safe and effective in patients with COPD. Chest 2001; 120: 1253–61
Brazinsky S, et al. One-year evaluation of the safety and efficacy of Ipratropium Bromide HFA and CFC Inhalation aerosols in patients with chronic obstructive pulmonary disease. Clinical Drug Investigation 2003; 23(3): 181–91
Reference
Novartis Pharmaceuticals UK ltd. Summary of product characteristics: Vildagliptin (Galvus). 2008 December 5 [online]. Available from URL: http://emc.medicines.org.uk
Reference
AstraZeneca UK Limited. Summary of product characteristics: Quetiapine (Seroquel XL) 2010 August 26 [online]. Available from URL: http://www.medicines.org.uk
References
Federal Register, September 29, 2010, p59936
U.S. Code of Federal Regulations (CFR) sections 312 and 320. “Guidance to Industry and Investigators: Safety Reporting Requirements for IND and BA/BE Studies”
References
Rumack BH, Matthew H. Acetaminophen poisoning and toxicity. Pediatrics 1975; 55: 871–6
Rumack BH, Peterson RC, Koch GG, et al. Acetaminophen overdose. 662 cases with evaluation of oral acetylcysteine treatment. Arch Intern Med 1981; 141: 380–5
References
Daly FF, Fountain JS, Murray L, et al. Guidelines for the management of paracetamol poisoning in Australia and New Zealand-explanation and elaboration. A consensus statement from clinical toxicologists consulting to the Australasian poisons information centres. Med J Aust 2008; 188(5): 296–301
Sandilands EA, Bateman DN. Adverse reactions associated with acetylcysteine. Clin Toxicol (Phila) 2009; 47(2): 81–8
Zyoud SH, Awang R, Syed Sulaiman SA, et al. Incidence of adverse drug reactions induced by N-acetylcysteine in patients with acetaminophen overdose. Hum Exp Toxicol 2010; 29(3): 153–60
Naranjo CA, Busto U, Sellers EM, et al. A method for estimating the probability of adverse drug reactions. Clin Pharmacol Ther 1981; 30(2): 239–45
Reference
Hospitalisation for adverse drug reactions in France. Prescrire 2009; 29: 434–5
Reference
Zurdinov A.Z
Reference
T.C. Sağlık Bakanligi Beseri Tıbbi Ürünlerin Güvenliğinin İzlenmesi ve Değerlendirilmesi Hakkında Yönetmelik
Reference
Phillips KA, Veenstra DL, Oren E, et al. Potential role of pharmacogenomics in reducing adverse drug reactions: a systematic review. JAMA 2001; 286(18): 2270–9
Reference
Wall M. Idiopathic Intracranial Hypertension. Neurologic Clinics 2010 Aug; 28 (3)
References
Yun SJ, Lee JB, Kim EJ, et al. Drug rash with eosinophilia and systemic symptoms induced by valproate and carbamazepine: formation of circulating auto-antibody against 190-kDa antigen. Acta Derm Venereol 2006; 86: 241–4
Ben Salem C, Slim R, Denguezli M, et al. A recurrent drug rash with eosinophilia and systemic symptoms. Pediatr Dermatol. 2007 Nov–Dec; 24(6): 666–8
References
Rodriguez A, Barranco R, Latasa M, et al. Generalized dermatitis due to codeine. Cross-sensitization among opium alkaloids. Contact Dermatitis 2005 oct; 53(4): 240
Iriarte Sotés P, López Abad R, Gracia Bara MT, et al. Codeine-induced generalized dermatitis and tolerance to other opioids. J Investig Allergol Clin Immunol 2010; 20(1): 89–90
References
Chowdhury MM, Statham BN, Sansom JE, et al. Patch testing for corticosteroid allergy with low and high concentrations of tixocortol pivalate and budesonide. Contact Dermatitis 2002 May; 46(5): 311–2
Browne F, Wilkinson SM. Effective prescribing in steroid allergy: Controversies and cross-reactions. Clin Dermatol 2011 May–Jun; 29(3): 287–94
References
Lacouture ME, Baron JM, Jani AB, et al. Treatment of radiation-relapsing primary cutaneous B-cell lymphoma with an anti-CD20 monoclonal antibody. Clin Exp Dermatol 2005; 30: 46–8
Kim MJ, Kim HO, Kim HY, et al. Rituximab-induced vasculitis: A case report and review of the medical published work. J Dermatol 2009 May; 36(5): 284–7
References
López V, Molina I, Monteagudo C, et al. Cutaneous sarcoidosis developing after treatment with pegylated interferon and ribavirin: a new case and review of the literature. Int J Dermatol 2011 Mar; 50(3): 287–91
Gayet AR, Plaisance P, Bergmann JF, et al. Development of sarcoidosis following completion of treatment for hepatitis C with pegylated interferon-alpha2a and ribavirin: a case report and literature review. Clin Med Res 2010 Dec; 8(3–4): 163–7
References
Natsch S, Vinks MH, Voogt AK, et al. Anaphylactic reactions to protonpump inhibitors. Ann Pharmacother 2000 Apr; 34(4): 474–6
Fardet L, Izzedine H, Ciroldi M, et al. Pantaprazole-induced recurrent anaphylactic shock. Am J Gastroenterol 2002 Nov; 97(11): 2933
References
Nebeker Jonathan R. Clarifying Adverse Drug Events: A Clinician’s Guide to Terminology, Documentation, and Reporting. Ann Intern Med 2005; 142: 795–801
Bates DW, Leape LL, Cullen DJ, et al. Effects of computerized physician order entry and a team intervention on prevention of serious medication errors. JAMA 1998; 280(15): 1311–6
Bradbury F. How important is the role of the physician in the correct use of a drug? An observational cohort study in general practice. International Journal of Clinical Practice 2004; 58(144): 27–32
Parthasarathi G, Nyfort Hansen K, Nahata Mc. A text book of Clinical pharmacy practice. In: Adverse Drug Reactions. Hyderabad, India: Orient Longman Pvt Ltd., 2004: 90–2
Ramesh M, Pandit J, Parthasarathi G. Adverse drug reactions in a south Indian hospital-their severity and cost involved. Pharmacoepidemiol Drug Saf 2003; 12(8): 687–92
Lang DM, Alpern MB, Visintainer PF, et al. Increased risk for anaphylactoid reaction from contrast media in patients on beta-adrenergic blockers or with asthma. Ann Intern Med 1991; 115: 270–6
References
Theophile H, et al. Improvement of a causality assessment method modelizing the consensual expert judgement. Fundam Clin Pharmacol 2011; 25 Suppl. 1: 80
Naranjo CA, et al. A method for estimating the probability of adverse drug reactions. Clin Pharmacol Ther 1981; 30: 239–45
References
Early communication about an ongoing safety review of montelukast (SINGULAR). 2008
Howick J, Glasziou P, Aronson JK. The evolution of evidence hierarchies: what can Bradford Hill’s ‘guidelines for causation’ contribute? JR Soc Med 2009; 102(5): 186–94
References
Ringe JD, Möller G. Differences in persistence, safety and efficacy of generic and original branded once weekly bisphosphonates in patients with postmenopausal osteoporosis: 1-year results of a retrospective patient chart review analysis. Rheumatol Int 2009; 31: 213–21
Grima DT, et al. Adverse events, bone mineral density and discontiunation associated with generic alendronate among postmenopausal women previously tolerant of brand alendronate: a retrospective cohort study. BMC Musculoskelet Disord 2010; 11: 68
Shakweh M, et al. Comparative in vitro study of oesophageal adhesiveness of different commercial formulations containing alendronate. Eur J Pharm Sci 2007; 31: 262–70
Epstein S, et al. Disintegration and esophageal irritation profiles of alendronate formulations: implications for clinical safety and efficacy. J Appl Res 2005; 5(2): 253–65
Reference
Guidance for Industry. Good Pharmacovigilance Practices and Pharma-coepidemiologic Assessment. Center for Drug Evaluation and Research Food and Drug Administration. p5. March 2005
References
Puig Sanz L, Sáez E, Lozano MJ, et al. Reactions to infliximab infusions in dermatologic patients: consensus statement and treatment protocol. Actas Dermosifiliogr 2009 Mar; 100(2): 103–12
Askling J, Fahrbach K, Nordstrom B, et al. Cancer risk with tumor necrosis factor alpha (TNF) inhibitors: meta-analysis of randomized controlled trials of adalimumab, etanercept and infliximab using patient level data. Pharmacoepidemiology and Drug Safety 2011; 20: 119–30
References
Kaushal R, Bates DW, Landrigan C, et al. Medication Errors and Adverse Drug Events in Pediatric inpatients. JAMA 2001; 285(16): 2114–2120
Benkirane R, Abouqal R, Haimeur C, et al. Incidence of Adverse Drug Events and Medication Errors in Intensive Care Units: A Prospective Multicenter Study. Journal of Patient Safety 2009; 5(1): 16–22
References
Hajjar ER, Hanlon JT, Artz MB, et al. Adverse drug reaction risk factors in older outpatients. Am J Geriatr Pharmacother 2003; 1: 82–9
Budnitz DS, Pollock DA, Weidenbach KN, et al. National surveillance of emergency department visits for outpatient adverse drug events. JAMA 2006; 296: 1858–66
Gurwitz JH, Field TS, Harrold LR, et al. Incidence and preventability of adverse drug events among older persons in the ambulatory setting. JAMA 2003; 289: 1107–16
Cobaugh DJ, Krenzelok EP. Adverse drug reactions and therapeutic errors in older adults: A hazard factor analysis of poison center data. Am J Health Syst Pharm 2006; 63: 2228–34
References
Aronson JK. Br J Clin Pharmacol 2009; 67(6): 599–604
Barber ND, Dean BS. Clin Risk 1998; 4: 103–6
Velo GP, Minuz P. Br J Clin Pharmacol 2009; 67(6): 624–8
References
Lagnaoui R, Moore N, Fach J, et al. Adverse drug reactions in a department of systemic disease-oriented internal medicine: prevalence, incidence, direct costs and avoidability. Eur J Clin Pharmacol 2000; 55: 181–6
Farcas A, Sinpetrean A, Mogosan C, et al. Adverse drug reactions detected by stimulated spontaneous reporting in an internal medicine department in Romania. Eur J Intern Med 2010; 21(5): 453–7
References
Ross LM, Wallace J, Paton JY. Medication errors in a paediatric teaching hospital in the UK: five years operational experience. Arch Dis Child 2000; 83: 492–7
National Patient Safety Agency. Reducing harm from omitted and delayed medicines in hospital 2010 [online. Available from URL: http://www.nrls.npsa.nhs.uk [Accessed 24 Oct 2010]
National Learning and Reporting Service. Rapid Response Report NPSA/2010/RRR009: Reducing harm from omitted and delayed medicines in hospital — Supporting Information. 2010 [online]. Available from URL: http://www.nrls.npsa.nhs.uk [Accessed 17 Nov 2010]
National Learning and Reporting Service. Quarterly Data Summary: Issue 14 — England. 2009 [online]. Available from URL: http://www.nrls.npsa.nhs.uk [Accessed 27 Nov 2010]
References
American Society of Health-System Pharmacists (AHFS) Drug Information. American Society of Health-System Pharmacists. Printed in the United States of America. 2007
Koda-Kimble MA, Young LY, Kradijan WA, et al. (editors). Applied Therapeutics, The Clinical Use of Drugs. Eight Edition. Maryland, USA: Lippincott Williams and Wilkins, 2005: 71–83
Choulis NH, Dukes MNG. Metals. In: Dukes MNG, Aronson JK, editors. Meyler’s Side Effects of Drugs. 14th ed. Amsterdam, PA: Elsevier Science B.V., 2000: 700
Schumock GT, Thornton JP. Focusing on the preventability of adverse drug reactions. Hosp Pharm 1992; 27: 538
Naranjo CA, Busto U, Sellers EM. A method for estimating the probability of adverse drug reactions. Clin Pharmacother 1981; 30: 239–45
Reference
Ducrocq S, Biran-Mucignat V, Lebas F, et al. Utilisation du citrate de caféine pour le traitement des apnées idiopathiques du prématuré dans les équipes françaises de médecine néonatale. Archives de pédiatrie 2006; 13: 1305–8
Reference
National Institute for Health and Clinical Excellence. Venous throm-boembolism: reducing the risk. Clinical guideline 92. January 2010 [online]. Available from URL: http://www.nice.org.uk/guidance/CG92
Reference
1. The rational use of drugs: report of the conference f experts. Nairobi, 25–29 November 1985. Geneva, World Health Organization, 1987
Reference
TUFAM’sdata
Reference
Reutenauer S, Chauveau D, Récher C. High-dose methotrexate: toxicity, management and prevention. Reanimation 2009; 18: 654–8
References
DIRECTIVE 2010/84/EU OF THE EUROPEAN PARLIAMENT AND OF THE COUNCIL of 15 December 2010 amending, as regards pharmacovigilance, Directive 2001/83/EC on the Community code relating to medicinal products for human use EMA, Dec 3rd 2010 http://eur-lex.europa.eu
Hallas J, Harvald B, Gram LF, et al. Drug related hospital admissions: the role of definitions and intensity of data collection, and the possibility of prevention. J Intern Med 1990; 228: 83–90
References
Edwards IR, Aronson JK. Adverse drug reactions: definitions, diagnosis, and management. Lancet 2000; 356(9237): 1255–9
Evans RS, Pestotnik SL, Classen DC, et al. Preventing adverse drug events in hospitalized patients. Ann Pharmacother 1994 Apr; 28(4): 523–7
Lazarou J, Pomeranz BH, Corey PN. Incidence of Adverse Drug Reactions in Hospitalized Patients: A Meta-analysis of Prospective Studies. JAMA 1998; 279(15): 1200–15
References
Edwards IR, Aronson JK. Adverse drug reactions: definitions, diagnosis, and management. Lancet 2000; 356(9237): 1255–9
Evans RS, Pestotnik SL, Classen DC, et al. Preventing adverse drug events in hospitalized patients. Ann Pharmacother 1994 Apr; 28(4): 523–7
Lazarou J, Pomeranz BH, Corey PN. Incidence of Adverse Drug Reactions in Hospitalized Patients: A Meta-analysis of Prospective Studies. JAMA 1998; 279(15): 1200–15
Reference
Lazarou J, Pomeranz BH, Corey PN. Incidence of Adverse Drug Reactions in Hospitalized Patients: A Meta-analysis of Prospective Studies. JAMA 1998; 279(15): 1200–15
References
Ponte ML, Keller GA, Di Girolamo G. Mechanisms of Drug Induced QT Interval Prolongation. Current Drug Safety 2010; 5(1): 44–53
Bagnes C, Panchuk PN, Recondo G. Antineoplastic Chemotherapy induced QTc Prolongation. Current Drug Safety 2010; 5(1): 93–6
Reference
Ponte ML, Keller GA, Di Girolamo G. Mechanisms of Drug Induced QT Interval Prolongation. Current Drug Safety 2010; 5(1): 44–53
Reference
Faculty of Sciences, Ibn Tofail University, Kenitra, Morocco
Reference
Schneeweiss S, Rassen JA, Glynn RJ, et al. High-dimensional Propensity Score Adjustment in Studies of Treatment Effects Using Health Care Claims Data. Epidemiology 2009; 20: 512–22
Reference
Olsen M, et al. Use of vitamin K antagonists and risk of subarachnoid haemorrhage: A population-based case-control study. European Journal of Internal Medicine 2010; 21: 297–300
References
Faraone SV, Biederman J, Mick E. The age-dependent decline of attention deficit hyperactivity disorder: a meta-analysis of follow-up studies. Psychol Med 2006; 36: 159–65
National Institute for Health and Clinical Excellence. Attention deficit hyperactivity disorder: pharmacological and psychological interventions in children, young people and adults. 2008. London: The British Psychological Society and the Royal College of Psychiatrists [online]. Available from URL: http://guidance.nice.org.uk
References
National Institute for Health and Clinical Excellence. Methylphenidate, atomoxetine and dexamfetamine for the treatment of attention deficit hyperactivity disorder in children and adolescents. Technology Appraisal 98, 2006. London: NICE. Available at: http://www.nice.org.uk/TA9
Kessler RC, Adler L, Barkley R, et al. The Prevalence and Correlates of Adult ADHD in the United States: Results From the National Comorbidity Survey Replication. Am J Psychiatry 2006; 163: 716–23
Faraone SV, Biederman J. What is the prevalence of adult ADHD? Results of a population screen of 966 adults. J Atten Disord 2005; 9: 384–91
Fayyad J, De Graaf R, Kessler R, et al. Cross-national prevalence and correlates of adult attention-deficit hyperactivity disorder. Br J Psychiatry 2007; 190:402–9
Simon V, Czobor P, Bálint S, et al. Prevalence and correlates of adult attention-deficit hyperactivity disorder: meta-analysis. Br J Psychiatry 2009; 194:204–11
Reference
Rozich JD, Haraden CR, Resar RK. Adverse drug event trigger tool: a practical methodology for measuring medication related harm. Qual Saf Health Care 2003; 13: 194–200
References
Avigni N, Ippoliti M, Muccinelli M, et al. Chest pain in the emergency department: benefits of a management model modified from the ANMCO-SIMEU recommendations. G Ital Cardiol (Rome) 2011; 12(5): 365–73
Nilsson S, Scheike M, Engblom D, et al. Chest pain and ischaemic heart disease in primary care. Br J Gen Pract 2003; 53(490): 378–82
AHFS. HMG-CoA Reductase Inhibitors (Statins) — safety overview. Drug information service, University of Utah. 2007
Lazarou J, Pomeranz BH, Corey PN. Incidence of adverse drug reactions in hospitalized patients. A meta-analysis of prospective studies. JAMA 1998; 279: 1200–5
Thompson PD, Clarkson P, Karas RH. Statin associated myopathy. JAMA 2003; 289: 1681–90
References
Vaughan CJ, Gotto AM. Update on statins. Circulation 2004; 110: 886–92
AlRazzaq HAA, Abd Aziz N, Hassan Y, et al. Dyslipidemia control and contributing factors in cardiac clinic of Malaysia. HealthMED 2009; 3(4): 343–51
National cardiovascular disease database (NCVD), Malaysia, 2006
AHFS. HMG-CoA Reductase Inhibitors (Statins) — safety overview. Drug information service, University of Utah, 2007
Pfeffer MA, Keech A, Sacks FM, et al. Safety and tolerability of pravastatin in long-term clinical trials: prospective Pravastatin Pooling (PPP) Project. Circulation 2002; 105(20): 2341–6
References
Levi N, Bastuji-Garin S, Mockenhaupt M, et al. Medications as risk factors of Stevens-Johnson syndrome and toxic epidermal necrolysis in children: a pooled analysis. Pediatrics. 2009 Feb; 123(2): e297–304
Lonjou C, Borot N, Sekula P, et al., for the RegiSCAR study group. A European study of HLA-B in Stevens-Johnson syndrome and toxic epidermal necrolysis related to five high-risk drugs. Pharmacogenet Genomics 2008; 18(2): 99–107
Reference
Budnitz, et al. National Surveillance of Emergency Department Visits for Outpatient Adverse Drug Events. JAMA 2006; 296: 1858–66
References
Lacroix I, Damase-Michel C, Lapeyre-Mestre M, et al. Prescription of drugs during pregnancy in France. Lancet 2000; 356: 1735–6
Hardy JR, Leaderer BP, Holford TR, et al. Safety of medications prescribed before and during early pregnancy in a cohort of 81 975 mothers from the UK General Practice Research Database. Pharmacoepidemiol and Drug Safety 2006; 15: 555–64
Hemminki E, Gissler M. Quantity and targeting of antenatal care in Finland. Acta Obstet Gynecol Scand 1993; 72: 24–30
Hjollund NH. Information on previous spontaneous abortions in the Medical Birth Registry. Ugeskr Laeger 1996; 158: 4746–8
Gunnarskog J, Bengt Källen AJ. Drug intoxication during pregnancy: a study with central registries. Reproductive Toxicology 1993; 2: 117–21
Bakker MK, Jentink J, Vroom F, et al. Drug prescription patterns before, during and after pregnancy for chronic, occasional and pregnancy-related drugs in the Netherlands. BJOG 2006; 113: 559–68
Engeland A, Bramness JG, Daltveit AK, et al. Prescription drug use among fathers and mothers before and during pregnancy. A population-based cohort study of 106 000 pregnancies in Norway 2004–2006. Br J Clin Pharmacol 2008; 65: 653–60
References
Sanchez Munoz-Torrero JF, et al. Adverse drug reactions in internal medicine units and associated factors. Eur J Clin Pharmacol 2010; 66: 1257–64
Reis AM, et al. Adverse drug events in an intensive care unit of a university hospital. Eur J Clin Pharmacol 2011; 67: 625–32
References
Lagnaoui R, Depont F, Fourrier A, et al. Patterns and correlates of benzodiazepine use in the French general population. Eur J Clin Pharmacol 2004; 60: 523–9
Egan M, Moride Y, Wolfson C, et al. Long-term continuous use of benzodiazepines by older adults in Quebec: prevalence, incidence and risk factors. J Am Geriatr Soc 2000: 811–6
Johnell K, Fastbom J. The use of benzodiazpines and related drugs amongst older people in Sweden: associated factors and concomitant use of other psychotropics. Int J Geriatr Psychiatry 2009; 24: 731–8
Sonnenberg CM, Bierman EJ, Deeg DJ, et al. Ten-year trends in benzodiazepine use in the Dutch population. Soc Psychiatry Psychiatr Epidemiol
Verdoux H, Lagnaoui R, Begaud B. Is benzodiazepine use a risk factor for cognitive decline and dementia? A literature review of epidemiological studies. Psychol Med 2005; 35: 307–15
Amieva H, Le Goff M, Millet X, et al. Prodromal Alzheimer’s disease: successive emergence of the clinical symptoms. Ann Neurol 2008; 64: 492–8
Reference
Roche Products Limited. Summary of product characteristics: Ibandronic acid (Bonviva). 2010 February [online]. Available from: URL: http://www.medicines.org.uk
Reference
Von Elm E, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for Reporting Observational Studies. Ann Intern Med 2007; 147: 573–7
Reference
Boyaci B, Berktas M, Kizilirmak P. The efficacy and safety of angiotensin receptor blocker and calcium channel blocker combination in hypertension. Presented at American Society of Hypertension, 26th Annual Scientific Meeting and Exposition, May 21–24 2011, New York
Reference
Hagiwara T, et al. Gut 2011 May; 60(5): 624–30
Reference
Boyaci B, Berktas M, Kizilirmak P. The efficacy and safety of angiotensin receptor blocker and calcium channel blocker combination in hypertension. Presented at American Society of Hypertension,26th Annual Scientific Meeting and Exposition, May 21–24 2011, New York
References
Lie C, Leung F, Chow SP. Nicolau syndrome following intramuscular diclofenac administration: a case report. Journal of Orthopaedic Surgery 2006; 14(1): 104–7
Halit Baykan and colleagues. Tissue necrosis following intramuscular diclofenac injection. Dicle Medical Journal Cilt/Vol 37: (3): 300–1
De Sousa R, Dang A, Rataboli PV. Nicolau syndrome following intramuscular benzathine penicilin. J Postgrad Med 2008; 54: 332–4
Hamilton B, Fowler P, Galloway H, et al. Nicolau syndrome in an athlete following intra-muscular diclofenac injection. Acta Orthop Belg 2008; 74: 860–4
References
Selimoglu E. Aminoglycoside-Induced Ototoxicity. Current Pharmaceutical Design 2007; 13: 119–26
Gentamicin — Ototoxicity in children, 2nd Meeting of the Subcommittee of the Expert Committee on the Selection and Use of Essential Medicines, Geneva, 2008
3. Meyler’s Side Effects of Drugs, 15th edition
4. Thesaurus des Intéractions médicamenteuses, Afssaps, 2009
5. Goodman & Gilman’s Manual of pharmacology and therapeutics, 2008
References
Auby P. Pharmaceutical research in paediatric populations and the new EU Paediatric Legislation: an industry perspective. Child Adolesc Psychiatry Ment Health 2008; 2(1): 38
Pandolfini C, Bonati M. A literature review on off-label drug use in children. Eur J Pediatr 2005 Sep; 164(9): 552–8
Kimland E, Bergman U, Lindemalm S, et al. Drug related problems and off-label drug treatment in children as seen at a drug information centre. Eur J Pediatr 2007 Jun; 166(6): 527–32
Zito JM, Derivan AT, Kratochvil CJ, et al. Off-label psychopharmacologic prescribing for children: History supports close clinical monitoring. Child Adolesc Psychiatry Ment Health 2008; 2(1): 24
Di Paolo ER, Stoetter H, Cotting J, et al. Unlicensed and off-label drug use in a Swiss paediatric university hospital. Swiss Med Wkly 2006 Apr 1; 136(13-14): 218–22
Hsu B, Brazelton T. Off-label medication use in an academic hospital pediatric critical care unit. WMJ 2009 Oct; 108(7): 343–8
Reference
TUFAM’s Data
References
Li Q, Zhang SM, Chen HT, et al. Awareness and attitudes of healthcare professionals in Wuhan, China to the reporting of adverse drug reactions. Chin Med J 2004; 117: 856–61
Lopez-Gonzalez E, Herdeiro MT, Figueiras A. Determinants of underreporting of adverse drug reactions: a systematic review. Drug Saf 2009; 32: 19–31
Enwere OO, Fawole OI. Adverse drug reactions reporting by physicians in Ibadan, Nigeria. Pharmacoepidemiol Drug Saf 2008; 17: 517–22
Rehan HS, Vasudev K, Tripathi CD. Adverse drug reaction monitoring: knowledge, attitude and practices of medical student and prescribers. Nat Med J India 2002; 15: 24–6
Chatterjee S, Lyle N, Ghosh S. A survey of the knowledge, attitude and practice of adverse drug reaction reporting by clinicians in eastern India. Drug Saf 2006; 29: 641–2
Vallano A, Cereza G, Pedros C, et al. Obstacles and solutions for spontaneous reporting of adverse drug reactions in the hospital. Br J Clin Pharmacol 2005; 60: 653–8
References
Al-Malaq HM, Al-Aqeel SA, Al-Sultan MS. Adverse drug reaction-related hospitalization identified by discharge ICD-9 codes in a university hospital in Riyadh. Saudi Med J 2008; 8: 1145–50
Annual Report of the Malaysian Adverse Drug Reactions Advisory Committee. (2007). MADRAC Annual Reports & Statistics. Available at: http://www.cornerstone-msc.net
Arulmani R, Rajendran SD, Suresh B. Adverse drug reaction monitoring in a secondary care hospital in South India. Br J Clin Pharmacol 2008; 65: 210–6
Aziz Z, Siang TC, Badarudin NS. Reporting of adverse drug reactions: predictors of under-reporting in Malaysia. Pharmacoepidemiol Drug Saf 2007; 16: 223–8,43
Blenkinsopp A, Wilkie P, Wang M, et al. Patient reporting of suspected adverse drug reactions: a review of published literature and international experience. British Journal of Clinical Pharmacology; 2006; 63(2): 148–56
Classen DC, Pestotnik SL, Evans RS, et al. Adverse drug events in hospitalized patients. JAMA 1997; 277: 301–6
References
Medicines: Safety of Medicine -adverse drug reaction [online]. World Health Organization; [updated 2008 October; cited 2011 February 11]. Available from URL: http://www.who.int
WHO Policy Perspectives on Medicines. Pharmacovigilance: ensuring the safe use of medicine. WHO 2004 Oct; 8: 1–6
Ahmed AM, Izham IM, Subish P. How Can Malaysia Improve Its Drug Safety System? [online]. BMJ Publishing Group Ltd; [updated 2010 May 2; cited 2011 February 11]. Available from URL: http://www.bmj.comreply
Cullen G, Kelly E, Murray FE. Patients’ knowledge of adverse reactions to current medications; Blackwell publishing Ltd 2006. British Journal of Clinical Pharmacology 62: 2 232–6
Xu H, Wang Y, Liu L. A hospital-based survey of healthcare professionals in the awareness of pharmacovigilance. John Wiley & Sons, Ltd. 2009; 18: 624–30
Blenkinsopp A, Wilkie P, Wang M, et al. Patient reporting of suspected adverse drug reactions: A review of published literature and international experience. British Journal of Clinical Pharmacology 2006; 63(2): 148–56
Van Grootheest K, De Graaf L, De Jong-van den Berg LTW. Consumer Adverse Drug Reaction Reporting: A New Step in Pharmacovigilance? Drug Safety 2003; 26(4): 211–7
Herxheimer A, Crombag MR, Leonardo Alves T. Direct Patient Reporting of Adverse Drug Reactions: A Twelve-Country Survey & Literature review. HAI (Europe). 2010 Jan. 01-2010/01: 7–10
Ahmed AM, Izham IM, Subish P. Developing a Consumer Reporting Program in Malaysia: A Novel Initiative to Improve Pharmacovigilance. [online] November 2009 [cited 2011 February 3] 32 (1): 2–6. Available from URL: http://jcdr.net
Wirtz VJ, Taxis K, Dreser A. Pharmacy customers’ knowledge of side effects of purchased medicines in Mexico. Tropical Medicine and International Health 2009; 14(1): 93–100
References
1. Eli Lilly and Company Limited. Summary of Product Characteristics, 2009
2. Food and Drug Administration. Strattera (atomoxetine) Sep 2005 — labelling revision, 1-9-2005
Reference
1. Pugi A, Gallo E, Vannacci A, et al. Herbal remedies in hospital setting: an Italian explorative survey among physicians and patients on knowledge and use. Intern Emerg Med 2011 Jun 3
References
Wild S, et al. Global Prevalence of Diabetes. Diabetes Care 2004; 27(5): 1047–53
Saadi H, et al. Screening strategy for type 2 diabetes in UAE. Asia Pac J Public Health 2010; 22(3): 54S–9S
Pinn G. Adverse effects associated with herbal medicine. Australian Family Physician 2001; 30(11): 1070–5
Chaubey S, et al. Severe hypoglycaemia associated with ingesting counterfeit medication. MJA 2010; 192(12): 716–7
References
Abu-Al-Basal M. Healing potential of Rosmarinus officinalis L. Journal of Ethnopharmacology 2010; 131: 443–50
ALI OMAR mariana (2009); pharmacopée traditionnelle et valorisation d’autres ressources naturelles par la femme toubou dans le Termit-Niger
Errajraji A, Ouhdouch F, El-Anssari N. Usage des plantes médicinales dans le traitement du diabète de type 2 au Maroc. Médecine des Maladies Métaboliques 2010; 4: 301–4
Farouqi A, Harti M-A, Nejjari C. Prise en charge du diabète au Maroc: résultats de l’International Diabetes Management Practices Study (IDMPS). Médecine des Maladies Métaboliques 2010; 4(6): 704–11
References
Nicolson TJ, Mellor HR, Roberts RR. Gender differences in drug toxicity. Trends Pharmacol Sci 2010; 31(3): 108–14
Bergman J, Hauge CP, Schjøtt J. 10 years of spontaneous reporting of adverse drug reactions in children in Norway. 9th Annual Meeting of International Society of Pharmacovigilance (ISoP), Reims, France 2009. Drug Saf 2009; 32(10): 924
Star K, Norén GN, Nordin K, et al. Suspected Adverse Drug Reactions Reported For Children Worldwide: An Exploratory Study Using VigiBase. Drug Saf 2011; 34(5): 415–28
The Norwegian Prescription Database (NorPD). Norwegian Institute of Public Health [online]. Available from URL: http://www.norpd.no. (Last updated 2011 April; cited 2011 June 6)
Crandall WV, Mackner LM. Infusion reactions to infliximab in children and adolescents: frequency, outcome and a predictive model. Aliment Pharmacol Ther 2003; 17(1): 75–84
Reference
Schwabe U, Pfaffrath D. Arzneiverordnungsreport 2009. Springer Verlag
References
Rigouzzo A, Servin F, Constant I. Pharmacokinetic-pharmacodynamic modeling of propofol in children. Anesthesiology 2010; 113: 343–52
Schuttler J, Ihmsen H. Population pharmacokinetics of propofol: a multicenter study. Anesthesiology 2000; 92: 727–38
Murat I, Billard V, Vernois J, et al. Pharmacokinetics of propofol after a single dose in children aged 1–3 years with minor burns. Comparison of three data analysis approaches. Anesthesiology 1996; 84: 526–32
Hammer GB, Litalien C, Wellis V, et al. Determination of the median effective concentration (EC50) of propofol during oesophagogastro-duodenoscopy in children. Paediatr Anaesth 2001; 11: 549–53
Rigouzzo A, Girault L, Louvet N, et al. The relationship between bispectral index and propofol during target-controlled infusion anesthesia: a comparative study between children and young adults. Anesth Analg 2008; 106: 1109–16
Reference
Eli Lilly and Company Limited. Summary of Product Characteristics, 2009
References
Abbassi K, Mergaoui L, Atay Kadiri Z, et al. Effects of extracts of Peganum harmala (Zygophyllaceae) on the desert locust (Schistocerca gregaria Forskål, 1775). Zool. baetica 2002–2003; 13/14: 203–17
Kim H, Sablin SO, Ramsay RR. Inhibition of monoamine oxidase A by beta-carboline derivatives. Arch Biochem Biophys 1997; 1; 337(1): 137–42
Frison G, Favretto D, Zancanaro F, et al. A case of beta-carboline alkaloid intoxication following ingestion of Peganum harmala seed extract. Forensic Sci Int 2008; 6; 179(2-3): e37–43
Reference
Kelly WN, Arellano FM, Barnes J, et al. Guidelines for submitting adverse event reports for publication. Drug Saf 2007; 30(5): 367–73
Reference
Menniti-Ippolito F, Raschetti R, De Cas R, et al. Active monitoring of adverse drug reactions in children. Lancet 2000; 355: 1613–4
References
Anekthananon T, Ratanasuwan W, Techasathit W, et al. Safety and efficacy of a simplified fixed-dose combination of stavudine, lamivudine and nevirapine (GPO-VIR) for the treatment of advanced HIV-infected patients: a 24-week study. J Med Assoc Thai 2004; 87: 760–7
Mouhari-Touré A, Saka B, Kombat K, et al. Clinical safety of a generic fixed-dose combination of stavudine/lamivudine/nevirapine (Triomune). Study of 297 cases in Togo. Bull Soc Pathol Exot 2008; 101: 404–6
Idigbe EO, Adewole TA, Eisen G, et al. Management of HIV-1 infection with a combination of nevirapine, stavudine, and lamivudine: a preliminary report on the Nigerian antiretroviral program. J Acquir Immune Defic Syndr 2005; 40: 65–9
WHO. ARV drugs adverse events, case definition, grading, laboratory diagnosis and treatment monitoring. Geneva: WHO, 2008
Reference
1. Pharmaceutical Care Network Europe [online]. Available from URL: http://www.pcne.org/ [Accessed 2011 6 Jun
References
Onel KB, Onel K. Anti-tumor necrosis factor therapy and cancer risk in patients with autoimmune disorders. Arthritis Care Res 2010; 62(7): 1024–8
Sweeting MJ, Sutton AJ, Lambert PC. What to add to nothing? Use and avoidance of continuity corrections in meta-analysis of sparse data. Stat Med 2004; 23(9): 1351–75
Reference
Naranjo C, et al. A method for estimating the probability of adverse drug reactions. Clin Pharmacol Ther 1981; 30: 239–45
References
Clodi K, et al. Expression of tumor necrosis factor (TNF)-related apoptosis-inducing ligand (TRAIL) receptors and sensitivity to TRAIL-induced apoptosis in primary B-cell acute lymphoblastic leukaemia cells. Br J Haematol 2000; 111: 580–6
Askling J, et al. Hematopoietic malignancies in rheumatoid arthritis. Lymphoma risk and characteristics following TNF-antagosnists. Ann Rheum Dis 2005; 20: 20
Geborek P, et al. Tumor necrosis factor blockers do not increase overall tumor risk in patients with rheumatoid arthritis, but may be associated with an increased risk of lymphomas. Ann Rheum Dis 2005; 64: 699–703
References
Commission of European Communities. Commission Directive 2003/63/EC of 25 June 2003 amending Directive 2001/83/EC of the European Parliament and of the Council on the Community code relating to medicinal products for human use
JACI2005; 115(3): 584–91
References
Furst DE, Keystone EC, Fleischmann R, et al. Updated consensus statement on biological agents for the treatment of rheumatic diseases, 2009. Ann Rheum Dis 2010; 69 Suppl. 1: i2–i29
Mariette X, et al. Lymphoma in patients treated with anti-TNF. Results of the 3-year prospective French RATIO registry. Ann Rheum Dis 2010; 69(2): 400–8
Wolfe F, Michaud K. Lymphoma in rheumatoid arthritis: the effect of methotrexate and anti-tumor necrosis factor therapy in 18.572 patients. Arthritis Rheum 2004; 50(6): 1740–51
References
Margulies DH. Monoclonal antibodies: producing magic bullets by somatic cell hybridization. J Immunol 2005; 174: 2451–2
Stowell CP. Therapy with immunoglobulin: applications for monoclonal antibodies. J Infus Nurs 2006; 29: s29–44
Gea-Banacloche JC, Weinberg GA. Monoclonal antibody therapeutics and risk for infection. Pediatr Infect Dis J 2007; 26: 1049–52
Flynn JL, Goldstein MM, Chan J, et al. Tumor necrosis factor-alpha is required in the protective immune response against Mycobacterium tuberculosis in mice. Immunity 2: 561–572 ecrosis factor antagonists. Clin Infect Dis 1995; 38: 1261–5
Gardam MA, Keystone EC, Menzies R, et al. Anti-tumour necrosis factor agents and tuberculosis risk: mechanisms of action and clinical management. Lancet Infect Dis 2003; 3: 148–55
Tracey D, Klareskog L, Sasso EH, et al. Tumor necrosis factor antagonist mechanisms of action: a comprehensive review. Pharmacol Ther 2008; 117: 244–79
References
Mack R, Kerr T, Johnston M, et al. Trastuzumab Periodic Safety Update Report 1041904; 2011 (Data on file)
Puscheck EE. Early Pregnancy Loss. Medscape reference [updated 2011 Jun 9, cited 2011 June 16; online] Available from URL: http://emedicine.medscape.com
Herceptin Core Data Sheet, Version 11.0 2011 (Data on file)
References
Zhou SF, Zhou ZW, Huang M. Polymorphisms of human cytochrome P450 2C9 and the functional relevance. Toxicology. Epub 2009 Aug 26
Ingelman-Sundberg M. Pharmacogenetics: an opportunity for a safer and more efficient pharmacotherapy. J Intern Med 2001; 250: 186–200
References
Yan W, et al. Simultaneous Determination of Ten Estrogens and their Metabolites in Waters by Improved Two-Step SPE Followed by LC-MS. Chromatographia 2009; 69: 621–8
Streck G. Chemical and biological analysis of estrogenic, progestagenic and androgenic steroids in the environment. Trends in Analytical Chemistry 2009; 28(6): 635–52
References
Bendz D, Paxéus NA, Ginn TR, et al. Occurrence and fate of pharmaceutically active compounds in the environment, a case study: Höje River in Sweden. Journal of Hazardous Materials 2005; 122: 195–204
Baird DJ, Barber I, Soares AM, et al. An early life-stage test with Daphnia magna Strauss: an alternative to the 21-day chronic test? Ecotoxicol Environ Saf 1991; 22: 1–7
Fent K. Ecotoxicological problems associated with contaminated sites. Tox Let 2003; 140-141: 353–65
Flaherty CM, Dodson SI. Effects of pharmaceuticals on Daphnia survival, growth, and reproduction. Chemosphere 2005; 61: 200–7
Heberer T. Occurrence, fate, and removal of pharmaceutical residues in the aquatic environment: a review of recent research data. Tox Lett 2002; 131: 5–17
References
Ponte M, Serra A, Wachs A. Drug induced Hyponatremia in Hospitalized patients. Congreso del Hospital de Clínicas. Buenos Aires, 2010
References
Burrowes JD, Van Houten G. Use of alternativemedicine by patients with stage 5 chronic kidney disease. Adv Chronic Kidney Dis 2005; 12(3): 312–25
Luyckx VA, Ballantine R, CLaeys M, et al. Herbal Remedy — associated acute renal failure secondary to Cape aloes. Am J Kidney Dis 2002; 39: 14
Frederic D. Debell. Aristolochic acid nephropathy: A worldwide problem. Kidney Int 2008; 74: 158–69
Zhou J, Xie G, Yan X. Traditional Chinese medicines: Molecular Structures, Natural Sources and Applications, 2nd ed. Hampshire: Ashgate Publishing Ltd, 2003
Steenkamp V, Michael J. Nephrotoxicity Associated With Exposure to Plant Toxins, With Particular Reference to Africa. Ther Drug Monit 2005; 27: 270–7
Phytothérapie, la santé par les plantes, Vidal et Sélection Reader’s Digest, 2010
Reference
Coloma PM, Schuemie MJ, Trifiro G, et al., on behalf of the EU-ADR Consortium. Combining electronic healthcare databases in Europe to allow for large-scale drug safety monitoring: the EU-ADR Project. Pharmacoepidemiol Drug Saf. 2011 Jan; 20(1): 1–11
Reference
Lazarou J, Pomeranz BH, Corey PN. Incidence of adverse reactions in hospitalized patients: a meta-analysis of prospective studies. JAMA 1998; 279: 1200–5
References
Guidance on the collection, verification and presentation of adverse event/reaction reports arising from clinical trials on medicinal products for human use (CT-3) (2011/C 172/01)
Detailed guidance on the collection, verification and presentation of adverse reaction reports arising from clinical trials on medicinal products for human use, rev 2, April 2006
Urushihara H, Kawakami K. Development Safety Update Reports and Proposals for Effective and Efficient Risk Communication. Drug Safety 2010; 33(5): 341–52
References
Farcas A, Sinpetrean A, Mogosan C, et al. Adverse drug reactions detected by stimulated spontaneous reporting in an internal medicine department in Romania. Eur J Int Med 2010; (21): 453–7
Vonbach P, Dubied A, Krahenbuhl S, et al. Prevalence of drug-drug interaction at hospital entry and during hospital stay of patients in internal medicine. Eur J Intern Med 2008; (19): 413–20
Becker ML, Kallewaard M, Caspers PWJ, et al. Hospitalisations and emergency department visits due to drug-drug interactions: a literature review. Pharmacoepidemiol Drug Saf 2007; 16: 641–51
References
Boehm K, et al. Cochrane Database Syst Rev 2009 Jul 8; (3): CD005004
Colalto C. Pharmacol Res 2010 Sep; 62(3): 207–27
Mazzanti G, et al. Eur J Clin Pharmacol 2009 Apr; 65(4): 331–41
Navarro VJ, et al. N Engl J Med 2006 Feb 16; 354(7): 731–9
Zhang H, et al. Clin Pharmacokinet 2007; 46(2): 133–57
References
Stickel F, Patsenker E, Schuppan D. Herbal hepatotoxicity. J Hepatol 2005; 43(5): 901–10
Stickel F, Kessebohm K, Weimann R, et al. Review of liver injury associated with dietary supplements. Liver Int 2011; 31(5): 595–605
References
Pharmactuel Vol. 38 N∘ 3 Mai-Juin-Juillet 2005
Trissel LA. Handbook on injectable drugs. 12th ed. Bethesda, MD: American Society of Health-System Pharmacists, 2003
References
Campana C, Regazzi MB, Buggia I, et al. Clin Pharmacokinet 1996; 30: 141
Matsuda H, Iwasaki K, Shiraga T, et al. Res Commun Mol Pathol Pharmacol 1996; 91: 57
Hebert MF, Roberts JP, Prueksaritanont T, et al. Clin Pharmacol Ther 1992; 52: 453
Chenhsu RY, Loong CC, Chou MH, et al. Ann Pharmacother 2000; 34: 27
Bhaloo S, Prasad GVR. Severe reduction in tacrolimus levels with rifampin despite multiple cytochrome P450 inhibitors: a case report. Transplantation Proceedings 2003; 35: 2449–51
Modry DL, Stinson EB, Oyer PE, et al. Acute rejection and massive cyclosporine requirements in heart transplant recipients treated with rifampin. Transplantation 1985; 39: 313–4
References
Lee A, editor. Adverse Drug Reaction. 2nd ed. Padstow, Great Britain: Pharmaceutical Press, 2006
Tisdale JE, Miller DA, editors. Drug Induced Diseases. Maryland USA: American Society of Health-System Pharmacists, 2005
Baxter K, editor. Stockley’s Drug Interactions, 8th ed. London: Pharmaceutical Press, 2008
Dukes MNG, Aronson JK. Meyler’s Side Effects of Drugs. Amsterdam: Elsevier, 2000
DiPiro JT, Talbert RL, Yee GC, et al. Pharmacotherapy A Pathophysiologic Approach, 7th ed. New York: McGraw Hill; 2008
Albareda MM, Corcoy R. Reversible impairment of renal function associated with enalapril in a diabetic patient. CMAJ 1998; 159: 1279–81
References
Trifilio SM, Scheetz MH, Pi1 J, et al. Tacrolimus use in adult allogeneic stem cell transplant recipients receiving voriconazole: preemptive dose modification and therapeutic drug monitoring. Bone Marrow Transplantation 2009; 1–5
Gaïs* E, Salouage I, Sahnoun R, et al. Interaction médicamenteuse entre des antifongiques azolés et le tacrolimus chez quatre greffés rénaux. Journal de Mycologie Médicale 2010
References
Trifilio SM, Scheetz MH, Pil J, et al. Tacrolimus use in adult allogeneic stem cell transplant recipients receiving voriconazole: preemptive dose modification and therapeutic drug monitoring. Bone Marrow Transplantation 2009; 1–5
Gaïs* E, Salouage I, Sahnoun R, et al. Interaction médicamenteuse entre des antifongiques azolés et le tacrolimus chez quatre greffés rénaux. Journal de Mycologie Médicale 2010
References
Burgess C, Holman CD, Satti A. Adverse drug reactions in older Australians, 1981–2002. MJA 2005; 182: 267–70
Hartholt K, van der Velde N, Looman C, et al. Adverse Drug Reactions Related Hospital Admissions in Persons Aged 60 Years and over, The Netherlands, 1981–2007: Less Rapid Increase, Different Drugs. Plos ONE 2010; 5(11): e13977
References
Aspinall SL, Good CB, Jiang R, et al. Severe dysglycemia with the fluoroquinolones: a class effect? Clin Infect Dis 2009; 49(3): 402–8
Garber SM, Pound MW, Miller SM. Hypoglycemia associated with the use of levofloxacin. Am J Health Syst Pharm 2009; 66(11): 1014–9
Mohr JF, Peymann PJ, Troxell E, et al. Risk factors for hyperglycemia in hospitalized adults receiving gatifloxacin: a retrospective, nested case-controlled analysis. Clin Ther 2008; 30(1): 152–7
Onyenwenyi AJ, Winsterstein AG, Hatton RC. An evaluation of the effects of gatifloxacin on glucose homeostasis. Pharm World Sci 2008; 30(5): 544–9
References
Amerson AB, Harper G. Introduction to the concept of medical information. In: Malone PM, Mosdell KW KL, editors. Drug Information, A Guide for Pharmacists. 2nd ed. Mc Graw Companies, 2001: 1–18
Anum P, Hedidor G, Ackon A, et al. Report on Ghana’s Drug Information System. National Drug Information Journal 2006; 1: 6–9
Beena G, Padama GMR. Assesment and evaluation of drug in information services provided in a South Indian Teaching Hospital [online]. Available from URL: http://medind.nic.in. [Accessed 2008 Aug 30]
Joshi MP. Drug Information Service in a developing country [online]. Available from URL: http://www.springerlink.com [Accessed 2008 Sep 3]
Avijit H, Amitava S, Sushanta R. Indian Journal of Pharmacology 2001; 33: 44–45 [online]. Available from URL: http://medind.nic.in [Accessed 2008 Sep 3]
References
Caudron JM, Frod N, Henkens M, et al. Substandard medicines in resource-poor setting: A problem that can no longer be ignored. Trop Med Int Health 2008 Aug; 13(8): 1062–72
Senior K. Global health-care implementations of substandard medicines. Lancet Infect Dis 2008 Nov; 8(11): 666
Newton PN, Green MD, Fernandez FM. Impact of poor-quality medicines in the ‘developing’ world. Trends Pharmacol Sci 2010 Mar; 31(3): 99–101
Lindquist M. VigiBase, the WHO global ICSR database system: basic facts. Drug Information Journal 2008; 42(5): 409–19
Norén GN, Hopstadius J, Bate A. Shrinkage observed-to-expected ratios for robust and transparent large-scale pattern discovery. Stat Methods Med Res. Epub 2011 Jun 24
References
Brooks K. Leveraging Expertise for Innovation. Contract Pharma 2011; May
Mozzicato P. MedDRA: An Overview of the Medical Dictionary for Regulatory Activities. Pharmaceutical Medicine 2009; 23(2): 65–75
References
American College of Obstetricians and Gynaecologists. Intrauterine devices and Adolescents 2007
Deans EI, Grimes DA. Intrauterine devices for adolescents: a systematic review. Contraception 2009 Jun; 79(6): 418–23
Harrison-Woolrych M, Coulter DM. PEM in New Zealand. In: Mann R, Andrews EB, editor. Pharmacovigilance. Second Edition ed. Chichester: John Wiley & Sons Ltd, 2006: 313–28
Paterson H, Ashton J, Harrison-Woolrych M. A nationwide cohort study of the use of the levonorgestrel intrauterine device in New Zealand adolescents. Contraception 2009 Jun; 79(6): 433–8
Sivin I, el Mahgoub S, McCarthy T, et al. Long-term contraception with the levonorgestrel 20 mcg/day (LNg 20) and the copper T 380Ag intrauterine devices: a five-year randomized study. Contraception 1990 Oct; 42(4): 361–78
Andersson K, Odlind V, Rybo G. Levonorgestrel-releasing and copper-releasing (Nova T) IUDs during five years of use: a randomized comparative trial. Contraception 1994 Jan; 49(1): 56–72
References
World Health Organization Collaborating Center for International Drug Monitoring. The importance of pharmacovigilance. Safety monitoring of medicinal products. Geneva: World Health Organization, 2002
Striker B, Psaty B. Detection, verification, and quantification of adverse drug reactions. BMJ 2004; 329: 44–7
Elland I, Belton K, van Grootheest A, et al. Attitudinal survey of voluntary reporting of adverse drug reactions. British Journal of Clinical Pharmacology 1999; 48: 623–7
References
National cholesterol education program (NCEP). Expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (adult treatment panel III). Third report of the national cholesterol education program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III). Final Report 2002; 106: 3143–21
AlRazzaq HAA, Abd Aziz N, Hassan Y, et al. Dyslipidemia control and contributing factors in cardiac clinic of Malaysia. HealthMED 2009; 3(4): 343–51
Avorn J, Monette J, Lacour A, et al. Persistence of use of lipid-lowering medications: a cross-national study. JAMA 1998; 279: 1458–62
National cardiovascular disease database (NCVD). Malaysia, 2006
AHFS. HMG-CoA Reductase Inhibitors (Statins) — safety overview. Drug information service, University of Utah, 2007
References
de Vries TW, de Langen-Wouterse JJ, van Puijenbroek E, et al. Reported adverse drug reactions during the use of inhaled steroids in children with asthma in the Netherlands. Eur J Clin Pharmacol 2006; 62: 343–6
Dalan D. Clinical data mining and research in the allergy office. Curr Opin Allergy Clin Immunol 2010; 10: 171–7
Jamali AN, Aqil M, Alam MS, et al. A pharmacovigilance study on patients of bronchial asthma in a teaching hospital. J Pharm Bioallied Sci 2010; 2: 333–6
References
Gill SS, Bronskill SE, Normand S-LT, et al. Antipsychotic drug use and mortality in older adults with dementia. Annals of Internal Medicine 2007; 146: 775–86
Banerjee S. The use of antipsychotic medication for people with dementia: Time for action. A report for the Minister of State for Care Services. October 2009
References
Wadzinski J, Franks R, Roane D, et al. Valproate-associated Hyperammonemic Encephalopathy. JABFM 2007; 20(5): 499–502
Mittal V, Muralee S, Tampi R. Valproic acid-induced hyperammonemia in the elderly: a review of the literature. Case Report Med 2009
References
Chandy SJ, Mathew BS. Patient information and medication labelling: an area of concern. Indian Journal of Medical Ethics 2006; 3(2): 58–60
Napke E, Stevens DGH. Excipients and additives: hidden hazards in drug products and in product substitution. Canadian medical Association Journal 1984; 131: 1449–52
DeMerlis CC. Excipient Development for Pharmaceutical, Biotechnology, and Drug Delivery Systems. Chapter 6 The Use of Food Additive Safety Evaluation Procedures as a Basis for Evaluating the Safety of New Pharmaceutical Excipients. Informa healthcare, US, Taylor & Francis Group, LLC. 2006, page 74
Harding G, Taylor KMG. Pharmacy’s strength lies in its blend of clinical, scientific and social skills. Pharmaceutical Journal 2004; 273: 126
Anderson M., Opawale F., Rao M. and Delmarre D., Anyarambhatla G. Development for Pharmaceutical, Biotechnology, and Drug Delivery Systems. Chapter 11 Excipients for Oral Liquid Formulations. Informa healthcare, US, Taylor & Francis Group, LLC, 2006, 106
Reference
Maintz L, Schwarzer V, Bieber T, et al. Effects of histamine and diamine oxidase activities on pregnancy: a critical review. Hum Reprod Update 2008; 14: 485–95
References
Centers for Disease Control and Prevention. Renal insufficiency and failure associated with immunoglobulin intravenous therapy-United States, 1985–1998. MMWR Morb Mortal Wkly Rep 1999; 48: 518–22
Gras V, Andrejak M, Decocq G. Acute renal failure associated with intravenous immunoglobulins. Pharmacoepidemiol Drug Safety 1999; 8 Suppl. 1: S73–8
Orbach H, Katz U, Sherer Y, et al. Intravenous immunoglobulin: adverse effects and safe administration. Clin Rev Allergy Immunol 2005; 29: 173–84
References
Giezen TJ, Mantel-Teeuwisse AK, Leufkens HG. Pharmacovigilance of biopharmaceuticals: challenges remain. Drug Saf 2009; 32(10): 811–7
Schellekens H, Jiskoot W. Erythropoietin-Associated PRCA: Still an Unsolved Mystery. J Immunotoxicol 2006 Sep 1; 3(3): 123–30
Declerck PJ. Biotherapeutics in the era of biosimilars: what really matters is patient safety. Drug Saf 2007; 30(12): 1087–92
Crommelin DJA, Storm G, Verrijk R, et al. Shifting paradigms: biopharmaceuticals versus low molecular weight drugs. Int J Pharm 2003 11/6; 266(1-2): 3–16
References
National Research Council. Networking Health: Prescriptions for the Internet. Washington DC: National Academy Press; 2000
Arıkan Y, Benker T. Use of Internet and Social Media for Healthcare and Drug Side Effect information Among Turkish Patients [poster]. 1 1th ISOP, Istanbul, 2011
References
Giordano C, Giordana C. Health professions students’ use of social media. J Allied Health 2011 Summer; 40(2): 78–81
Arıkan Y, Benker T. Use of Internet and Social Media for Healthcare and Drug Side Effect information Among Turkish Patients [poster]. 1 1th. ISOP. 2011 Istanbul
References
Lazarou J, Pomeranz BH, Corey PN. Incidence of adverse reactions in hospitalized patients. A meta-analysis of prospective studies. JAMA 1998; 279: 1200–5
Pirmohamed M, James S, Meakin S, et al. Adverse drug reactions as cause of admission to hospital: prospective analysis of 18 820 patients. Br Med J 2004; 329: 15–9
Oshikoya KA. Adverse drug reaction in children: types, incidence and risk factors. Nig J Paediatr 2006; 33: 29–35
Lexchin J. Is there a role for spontaneous reporting of adverse drug reactions? CMAJ 2006; 174: 191–2
References
Strandell J, Caster O, Bate A, et al. Reporting Patterns Indicative of Adverse Drug Interactions: A Systematic Evaluation in VigiBase. Drug Safety 2011 Mar 1; 34(3): 253–66
Horn JR, Hansten PD, Chan LN. Proposal for a new tool to evaluate drug interaction cases. Annals of Pharmacotherapy 2007 Apr; 41(4): 674–80
Lindquist M. VigiBase, the WHO Global ICSR Database system: basic facts. Drug Information Journal 2008; 42(5): 409–19
Reference
Passier A, ten Napel M, van Grootheest K, et al. Reporting of adverse drug reactions by general practitioners: a questionnaire-based study in the Netherlands. Drug Saf 2009; 32(10): 851–8
Reference
IHI Global Trigger tool for measuring Adverse Events (UK version revised 2008). A resource from the Institute for Healthcare Improvement [online]. Available from URL: http://www.ihi.org [Accessed 2011 Jun 30]
References
Choonara IA. Sodium valproate and enuresis. Lancet 1985; I: 1276
Panayiotopoulos CP. Nocturnal enuresis associated with sodium valproate. Lancet 1985; I: 980–1
Reference
Bégaud B, Evreux JC, Jouglard J, et al. FrImputabilité des effets inattendus ou toxiques des médicaments. Thérapie 1985; 40: 111–8
References
Pirmohamed M, James S, Meakin S, et al. Adverse drug reactions as cause of admission to hospital: prospective analysis of 18 820 patients. BMJ 2004 Jul 3; 329(7456): 15–9
INFARMED. Notificação de Reacções Adversas a Medicamentos em 2009. Boletim de Farmacovigilância, Volume 14, N∘2, 2∘Trimestre de 2010
Inman W. Attitudes to adverse drug reaction reporting. British Journal of Clinical Pharmacology 1996; 41(5): 434
Herdeiro MT, Figueiras A, Polonia J, et al. Influence of pharmacists’ attitudes on adverse drug reaction reporting: a case-control study in Portugal. Drug Saf 2006; 29(4): 331–40
Reference
TUFAM’s database 2008, 2009,2010
Reference
TUFAM’sData
Reference
TUFAM’s data
Reference
TUFAM’s data
Reference
Safety of Medicines A guide to detecting and reporting adverse drug reactions. Geneva: World Health Organization, 2002
Reference
Reeves RR, Ladner ME. Antidepressant-induced suicidality: an update. CNS Neuroscience & Therapeutic 2010 Aug; 16(4): 227–34
Stone M, et al. Risk of suicidality in clinical trials of antidepressants in adults: analysis of proprietary data submitted to US Food and Drug Administration. BMJ 2009 Aug 11; 339: b2880
Barbui C, Esposito E, Cipriani A. Selective serotonin reuptake inhibitors and risk of suicide: a systematic review of observational studies. CMAJ 2009 Feb 3; 180(3): 291–7
Brent DA, et al. Predictors of spontaneous and systematically assessed suicidal adverse events in the treatment of SSRI-resistant depression in adolescents (TORDIA) study. Am J Psychiatry. 2009 Apr; 166(4): 418–26
Reference
Kambu, K.O. et al. Pharmacopée Traditionnelle de la République Démocratique du Congo, 2010
Plantes toxiques. Végétaux dangereux pour l’homme et les animaux. Lavoisier TEC 1 DOC. Londres, 1996
Reference
Lilly Turkey Pharmacovigilance data in 2009–2010
Reference
Diane K. Wysowski, PhD; Lynette Swartz, MEd, MBA. (2005). Adverse Drug Event Surveillance and Drug Withdrawals in the United States 1969–2002. The Importance of Reporting Suspected Reactions. Arch Intern Med, 165: 1363–1369
Reference
Moen M. Indacaterol. In chronic obstructive pulmonary disease. Drugs 2010; 70(17): 2269–80
References
Toklu HZ, Uysal MK. The knowledge and attitude of the Turkish community pharmacists toward pharmacovigilance in the Kadikoy district of Istanbul. Pharm World Sci 2008; 30: 556–62
Green CF, Mottram DR, Raval D, et al. Community pharmacists’attitudes to adverse drug reaction reporting. Int J Pharm Pract 1999; 7: 92–9
Reference
Hedenmalm K, Spigset O. Agranulocytosis and other blood dyscrasias associated with dipyrone (metamizole). Eur J Clin Pharmacol 2002; 58: 265–74
Reference
Ghosh S, Ali S, Chhabra L, et al. Investigation of attitude and perception of medical practitioners on adverse drug reaction reporting — a pilot study. The Pharma Research 2010; 3: 1–9
Beard K, Lee A. Introduction. In: Lee A, editor. Adverse drug reactions. 2nd edition. London: Pharmaceutical Press, 2006: 4: 1–22
van Grootheest K, Olsson S, Couper M, et al. Pharmacists’ role in reporting adverse drug reactions in an international perspective. Pharmacoepidemiology and drug safety 2004; 13: 457–464
WHO (2002) Safety of Medicines: A guide to detecting and reporting adverse drug reactions;Why health professionals need to take action. World Health Organization
Zolezzi M, Parsotam N. Adverse drug reaction reporting in New Zealand: implications for pharmacists. Therapeutics and Clinical Risk Management 2005; 1: 181–8
Bawazir S, Al-Sultan M. To study hospital pharmacists attitude and behavior toward reporting of adverse drug reactions (ADRs) in different hospitals throughout Saudi Arabia. Saudi Pharmaceutical Journal, 17 2009
WU T, et al. Ten-year trends in hospital admissions for adverse drug reactions in England 1999–2009. Journal of the Royal Society of Medicine 2010; 103: 239
Reference
Popova M, Historical Overview and Gained Experience in the Field of Pharmacovigilance in Bulgaria, Fifth National Pharmaceutical Congress, Pharmacia, Supplement/2011 volume LVIII, ISSN 0428-0296
Bulgarian Drug Agency, 2007, History of Medicinal Products Regulation in Bulgaria [online]. Available from URL: http://www.bda.bg [Accessed 2011 Mar 25]
Law for Medicinal Products in Human Medicine. State Gazette No 31/2007. Amendments in No 19/2008; Resolution No 5/2008 of the Bulgarian Constitutional Court promulgated in State Gazette No 65/2008; amendments in No 71/2008, Nos 10, 23, 41, 88 and 102/2009, Nos 59 and 102/2010., Nos 9 and 12/2011
WHO. The Importance of Pharmacovigilance, Safety Monitoring of Medical Products. Geneva: WHO, 2002
Reference
The US FDA. Safety information on Leukotriene inhibitors. 2009 [online]. Available from URL: http://www.fda.gov
Wallerstedt SM, Brunlöf G, Sundström A, et al. Montelukast and psychiatric disorders in children. Pharmacoepidemiol Drug Saf 2009 Sep; 18(9): 858–64
Reference
Report of an independent review of access to the Yellow Card scheme. The Stationary Office, 2004
Reference
Friedman DS, Wolfs RC, O’Colmain BJ, et al. Eye Diseases Prevalence Research Group Prevalence of open-angle glaucoma among adults in the United States. Arch Ophthalmol 2004; 122(4): 532–8
Reference
Trifirò G, Calogero G, Ippolito FM, et al. Adverse drug events in emergency department population: a prospective Italian study. Pharmaco-epidemiol Drug Saf 2005; 14(5): 333–40
Queneau P, Bannwarth B, Carpentier F, et al. Emergency department visits caused by adverse drug events: results of a French survey. Drug Saf 2007; 30(1): 81–8
Reference
Pharmacovigilance: The French System. Drug Saf 1990; 5 Suppl.1: 137–40
Fraunhofer Institute for Systems and Innovation Research: Assessment of the European Community System of Pharmacovigilance, Final Report November 2005
Vallano A, Cereza G, Pedrós C, et al. Obstacles and solutions for spontanoues adverse drug reactions in the hospital. Br J Clin Pharmacol 2005; 60: 653–8
Reference
American Society of Health-System Pharmacists (AHFS) Drug Information. American Society of Health-System Pharmacists. Printed in the United States of America, 2007: 2961
Reference
World Health Organization. Promoting safety of medicines for children. Geneva: WHO, 2007
Reference
TUFAM Database
Reference
Valeyrie L, Bastuji-Garin S, Revus J. Adverse cutaneous reactions to imatinib (STI571) in philadelphia chromosome-positive leukemias: A prospective study of 54 patients. J Am Acad Dermatol 2003; 48: 201–6
Reference
Munir Pirmohamed et al. Pharmacovigilance in developing countries [editorial]; BMJ 335, 6 September 2007
Reference
Boudal P. Bleedings induced by oral anticoagulants: a study of adverse drug reactions reported to Midi Pyrénées PharmacoVigilance Centre between 2003 and 2006. Therapie 2010; 65: 567–9
Reference
Chiang YY, Tseng KF, Lih YW, et al. Lidocaine-induced CNS toxicity: a case report. Acta Anaesthesiol Sin 1996; 34: 243–6
Rights and permissions
About this article
Cite this article
International Society of Pharmacovigilance Abstracts 11th ISoP Annual Meeting ‘Next Stop: Istanbul — Bridging the Continents!’ Istanbul, Turkey 26–28 October 2011. Drug-Safety 34, 883–1026 (2011). https://doi.org/10.2165/11596230-000000000-00000
Published:
Issue Date:
DOI: https://doi.org/10.2165/11596230-000000000-00000