Abstract
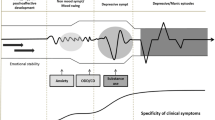
Bipolar disorder is a chronic and typically recurring illness with significant psychosocial morbidity. Although the aetiological factors that contribute to the onset of mania, and by definition bipolar I disorder, are poorly understood, it most commonly occurs during the adolescent period. Putative risk factors for developing bipolar disorder include having a first-degree relative with a mood disorder, physical/sexual abuse and other psychosocial stressors, substance use disorders, psychostimulant and antidepressant medication exposure and omega-3 fatty acid deficiency. Prominent prodromal clinical features include episodic symptoms of depression, anxiety, hypomania, anger/irritability and disturbances in sleep and attention. Because prodromal mood symptoms precede the onset of mania by an average of 10 years, and there is low specificity of risk factors and prodromal features for mania, interventions initiated prior to onset of the disorder (primary prevention) or early in the course of the disorder (early or secondary prevention) must be safe and well tolerated upon long-term exposure. Indeed, antidepressant and psychostimulant medications may precipitate the onset of mania. Although mood stabilizers and atypical antipsychotic medications exhibit efficacy in youth with bipolar I disorder, their efficacy for the treatment of prodromal mood symptoms is largely unknown. Moreover, mood stabilizers and atypical antipsychotics are associated with prohibitive treatment-emergent adverse effects. In contrast, omega-3 fatty acids have neurotrophic and neuroprotective properties and have been found to be efficacious, safe and well tolerated in the treatment of manic and depressive symptoms in children and adolescents. Together, extant evidence endorses a clinical staging model in which subjects at elevated risk for developing mania are treated with safer interventions (i.e. omega-3 fatty acids, familyfocused therapy) in the prodromal phase, followed by pharmacological agents with potential adverse effects for nonresponsive cases and secondary prevention. This approach warrants evaluation in prospective longitudinal trials in youth determined to be at ultra-high risk for bipolar I disorder.

Similar content being viewed by others
References
Kessler RC, Merikangas KR, Wang PS. Prevalence, comorbidity, and service utilization for mood disorders in the United States at the beginning of the twenty-first century. Annu Rev Clin Psychol 2007; 3: 137–58
Chengappa KN, Kupfer DJ, Frank E, et al. Relationship of birth cohort and early age at onset of illness in a bipolar disorder case registry. Am J Psychiatry 2003; 160: 1636–42
Goodwin FK, Jamison KR. Manic-depressive illness. New York: Oxford University Press, 1990: 134–6
Perlis RH, Miyahara S, Marangell LB, et al., STEP-BD Investigators. Long-term implications of early onset in bipolar disorder: data from the first 1000 participants in the Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD). Biol Psychiatry 2004; 55: 875–81
Perlis RH, Dennehy EB, Miklowitz DJ, et al. Retrospective age at onset of bipolar disorder and outcome during twoyear follow-up: results from the STEP-BD study. Bipolar Disord 2009; 11: 391–400
Brent DA, Perper JA, Goldstein CE, et al. Risk factors for adolescent suicide: a comparison of adolescent suicide victims with suicidal inpatients. Arch Gen Psychiatry 1988; 45: 581–8
Brent DA, Perper JA, Moritz G, et al. Psychiatric risk factors for adolescent suicide: a case-control study. J Am Acad Child Adolesc Psychiatry 1993; 32: 521–9
Craney JL, Geller B. A prepubertal and early adolescent bipolar disorder-I phenotype: review of phenomenology and longitudinal course. Bipolar Disord 2003; 5: 243–56
Goodwin FK. Rationale for long-term treatment of bipolar disorder and evidence for long-term lithium treatment. J Clin Psychiatry 2002; 63 Suppl. 10: 5–12
Tohen M, Waternaux CM, Tsuang MT. Outcome in mania: a 4-year prospective follow-up of 75 patients utilizing survival analysis. Arch Gen Psychiatry 1990 Dec; 47: 1106–11
Post RM, Leverich GS, Altshuler LL, et al. An overview of recent findings of the Stanley Foundation Bipolar Network (Part I). Bipolar Disord 2003; 5: 310–9
Berk M, Conus P, Lucas N, et al. Setting the stage: from prodrome to treatment resistance in bipolar disorder. Bipolar Disord 2007; 9: 671–8
Conus P, Ward J, Hallam KT, et al. The proximal prodrome to first episode mania: a new target for early intervention. Bipolar Disord 2008; 10: 555–65
DelBello MP, Geller B. Review of studies of child and adolescent offspring of bipolar parents. Bipolar Disord 2001; 3: 325–34
Miklowitz DJ, Chang KD. Prevention of bipolar disorder in at-risk children: theoretical assumptions and empirical foundations. Dev Psychopathol 2008; 20: 881–97
Salvadore G, Drevets WC, Henter ID, et al. Early intervention in bipolar disorder, part I: clinical and imaging findings. Early Interv Psychiatry 2008; 2: 122–35
Tsuchiya KJ, Byrne M, Mortensen PB. Risk factors in relation to an emergence of bipolar disorder: a systematic review. Bipolar Disord 2003; 5: 231–42
McGorry PD, Hickie IB, Yung AR, et al. Clinical staging of psychiatric disorders: a heuristic framework for choosing earlier, safer and more effective interventions. Aust N Z J Psychiatry 2006; 40: 616–22
Cannon TD, van Erp TG, Bearden CE, et al. Early and late neurodevelopmental influences in the prodrome to schizophrenia: contributions of genes, environment, and their interactions. Schizophr Bull 2003; 29: 653–69
Maier W, Cornblatt BA, Merikangas KR. Transition to schizophrenia and related disorders: toward a taxonomy of risk. Schizophr Bull 2003; 29: 693–701
Hill AB. The environment and disease: association or causation? Proc R Soc Med 1965; 58: 295–300
Alda M. Bipolar disorder: from families to genes. Can J Psychiatry 1997; 42: 378–87
Craddock N, Jones I. Genetics of bipolar disorder. J Med Genet 1999; 36: 585–94
Kieseppä T, Partonen T, Haukka J, et al. High concordance of bipolar I disorder in a nationwide sample of twins. Am J Psychiatry 2004; 161: 1814–21
Faraone SV, Glatt SJ, Tsuang MT. The genetics of pediatriconset bipolar disorder. Biol Psychiatry 2003; 53: 970–7
Smoller JW, Finn CT. Family, twin, and adoption studies of bipolar disorder. Am J Med Genet C Semin Med Genet 2003; 123C(1): 48–58
Gershon ES, Hamovit J, Guroff JJ, et al. A family study of schizoaffective, bipolar I, bipolar II, unipolar, and normal control probands. Arch Gen Psychiatry 1982; 39: 1157–67
Lapalme M, Hodgins S, LaRoche C. Children of parents with bipolar disorder: a metaanalysis of risk for mental disorders. Can J Psychiatry 1997; 42: 623–31
Carlson GA, Weintraub S. Childhood behavior problems and bipolar disorder: relationship or coincidence? J Affect Disord 1993; 28: 143–53
Chang KD, Steiner H, Ketter TA. Psychiatric phenomenology of child and adolescent bipolar offspring. J Am Acad Child Adolesc Psychiatry 2000; 39: 453–60
Singh MK, DelBello MP, Stanford KE, et al. Psychopathology in children of bipolar parents. J Affect Disord 2007; 102: 131–6
Chang K, Steiner H, Dienes K, et al. Bipolar offspring: a window into bipolar disorder evolution. Biol Psychiatry 2003; 53: 945–51
Dwyer JT, DeLong GR. A family history study of twenty probands with childhood manic-depressive illness. J Am Acad Child Adolesc Psychiatry 1987; 26: 176–80
Strober M, Morrell W, Burroughs J, et al. A family study of bipolar I disorder in adolescence: early onset of symptoms linked to increased familial loading and lithium resistance. J Affect Disord 1988; 15: 255–68
Todd RD, Reich W, Petti TA, et al. Psychiatric diagnoses in the child and adolescent members of extended families identified through adult bipolar affective disorder probands. J Am Acad Child Adolesc Psychiatry 1996; 35: 664–71
Post RM, Leverich GS. The role of psychosocial stress in the onset and progression of bipolar disorder and its comorbidities: the need for earlier and alternative modes of therapeutic intervention. Dev Psychopathol 2006; 18: 1181–211
Agid O, Shapira B, Zislin J, et al. Environment and vulnerability to major psychiatric illness: a case control study of early parental loss in major depression, bipolar disorder and schizophrenia. Mol Psychiatry 1999; 4: 163–72
Brown GR, McBride L, Bauer MS, et al., Cooperative Studies Program 430 Study Team. Impact of childhood abuse on the course of bipolar disorder: a replication study in U.S. veterans. J Affect Disord 2005; 89: 57–67
Dienes KA, Hammen C, Henry RM, et al. The stress sensitization hypothesis: understanding the course of bipolar disorder. J Affect Disord 2006; 95: 43–9
Garno JL, Goldberg JF, Ramirez PM, et al. Impact of childhood abuse on the clinical course of bipolar disorder. Br J Psychiatry 2005; 186: 121–5
Leverich GS, McElroy SL, Suppes T, et al. Early physical and sexual abuse associated with an adverse course of bipolar illness. Biol Psychiatry 2002; 51: 288–97
Hillegers MH, Burger H, Wals M, et al. Impact of stressful life events, familial loading and their interaction on the onset of mood disorders: study in a high-risk cohort of adolescent offspring of parents with bipolar disorder. Br J Psychiatry 2004; 185: 97–101
Wals M, Hillegers MH, Reichart CG, et al. Stressful life events and onset of mood disorders in children of bipolar parents during 14-month follow-up. J Affect Disord 2005; 87: 253–63
Kennedy S, Thompson R, Stancer HC, et al. Life events precipitating mania. Br J Psychiatry 1983; 142: 398–403
Ellicott A, Hammen C, Gitlin M, et al. Life events and the course of bipolar disorder. Am J Psychiatry 1990; 147: 1194–8
Post RM. Kindling and sensitization as models for affective episode recurrence, cyclicity, and tolerance phenomena. Neurosci Biobehav Rev 2007; 31: 858–73
Kessler RC, Crum RM, Warner LA, et al. Lifetime cooccurrence of DSM-III-R alcohol abuse dependence with other psychiatry disorders in the National Comorbidity Survey. Arch Gen Psychiatry 1997; 54: 313–21
Regier DA, Farmer ME, Rae DS, et al. Comorbidity of mental disorders with alcohol and other drug abuse: results from the Epidemiologic Catchment Area ECA Study. JAMA 1990; 264: 2511–8
West SA, Strakowski SM, Sax KW, et al. Phenomenology and comorbidity of adolescents hospitalized for the treatment of acute mania. Biol Psychiatry 1996; 39: 458–60
Wilens TE, Biederman J, Mick E, et al. Attention deficit hyperactivity disorder (ADHD) is associated with early onset substance use disorders. J Nerv Ment Dis 1997; 185: 475–82
Wilens TE, Biederman J, Millstein RB, et al. Risk for substance use disorders in youths with child- and adolescentonset bipolar disorder. J Am Acad Child Adolesc Psychiatry 1999; 37: 680–5
Wilens TE, Biederman J, Kwon A, et al. Risk of substance use disorders in adolescents with bipolar disorder. J Am Acad Child Adolesc Psychiatry 2004; 43: 1380–6
Salloum IM, Thase ME. Impact of substance abuse on the course and treatment of bipolar disorder. Bipolar Disord 2000; 2: 269–80
Strakowski SM, DelBello MP. The co-occurrence of bipolar and substance use disorders. Clin Psychol Rev 2000; 20: 191–206
Goldstein BI, Strober MA, Birmaher B, et al. Substance use disorders among adolescents with bipolar spectrum disorders. Bipolar Disord 2008; 10: 469–78
Tohen M, Vieta E, Gonzalez-Pinto A, et al., European Mania in Bipolar Longitudinal Evaluation of Medication (EMBLEM) Advisory Board. Baseline characteristics and outcomes in patients with first episode or multiple episodes of acute mania. J Clin Psychiatry 2010; 71: 255–61
Wilens TE, Biederman J, Abrantes AM, et al. Clinical characteristics of psychiatrically referred adolescent out-patients with substance use disorder. J Am Acad Child Adolesc Psychiatry 1997; 36: 941–7
Goldstein BI, Bukstein OG. Comorbid substance use disorders among youth with bipolar disorder: opportunities for early identification and prevention. J Clin Psychiatry 2010; 71: 348–58
Mayes R, Bagwell C, Erkulwater J. ADHD and the rise in stimulant use among children. Harv Rev Psychiatry 2008; 16: 151–66
Reichart CG, Nolen WA. Earlier onset of bipolar disorder in children by antidepressants or stimulants? An hypothesis. J Affect Disord 2004; 78: 81–4
Moreno C, Laje G, Blanco C, et al. National trends in the outpatient diagnosis and treatment of bipolar disorder in youth. Arch Gen Psychiatry 2007; 64: 1032–9
Baumer FM, Howe M, Gallelli K, et al. A pilot study of antidepressant-induced mania in pediatric bipolar disorder: characteristics, risk factors, and the serotonin transporter gene. Biol Psychiatry 2006; 60: 1005–12
Biederman J, Mick E, Prince J, et al. Systematic chart review of the pharmacologic treatment of comorbid attention deficit hyperactivity disorder in youth with bipolar disorder. J Child Adolesc Psychopharmacol 1999; 9: 247–56
Boerlin HL, Gitlin MJ, Zoellner LA, et al. Bipolar depression and antidepressant-induced mania: a naturalistic study. J Clin Psychiatry 1998; 59: 374–9
Bond DJ, Noronha MM, Kauer-Sant’Anna M, et al. Antidepressant-associated mood elevations in bipolar II disorder compared with bipolar I disorder and major depressive disorder: a systematic review and meta-analysis. J Clin Psychiatry 2008; 69: 1589–601
Cicero D, El-Mallakh RS, Holman J, et al. Antidepressant exposure in bipolar children. Psychiatry 2003; 66: 317–22
DelBello MP, Soutullo CA, Hendricks W, et al. Prior stimulant treatment in adolescents with bipolar disorder: association with age at onset. Bipolar Disord 2001; 3: 53–7
Faedda GL, Baldessarini RJ, Glovinsky IP, et al. Treatment-emergent mania in pediatric bipolar disorder: a retrospective case review. J Affect Disord 2004; 82: 149–58
Koehler-Troy C, Strober M, Malenbaum R. Methylphenidate-induced mania in a prepubertal child. J Clin Psychiatry 1986; 47: 566–7
Pagano ME, Demeter CA, Faber JE, et al. Initiation of stimulant and antidepressant medication and clinical presentation in juvenile bipolar I disorder. Bipolar Disord 2008; 10: 334–41
Post RM, Altshuler LL, Leverich GS, et al. Mood switch in bipolar depression: comparison of adjunctive venlafaxine, bupropion and sertraline. Br J Psychiatry 2006; 189: 124–31
Soutullo CA, DelBello MP, Ochsner JE, et al. Severity of bipolarity in hospitalized manic adolescents with history of stimulant or antidepressant treatment. J Affect Disord 2002; 70: 323–7
Goldberg JF, Whiteside JE. The association between substance abuse and antidepressant-induced mania in bipolar disorder: a preliminary study. J Clin Psychiatry 2002; 63: 791–5
Lieberman DZ, Kolodner G, Massey SH, et al. Antidepressant-induced mania with concomitant mood stabilizer in patients with comorbid substance abuse and bipolar disorder. J Addict Dis 2009; 28: 348–55
Goldstein BI, Shamseddeen W, Axelson DA, et al. Clinical, demographic, and familial correlates of bipolar spectrum disorders among offspring of parents with bipolar disorder. J Am Acad Child Adolesc Psychiatry 2010; 49: 388–96
Tillman R, Geller B. Controlled study of switching from attention-deficit/hyperactivity disorder to a prepubertal and early adolescent bipolar I disorder phenotype during 6-year prospective follow-up: rate, risk, and predictors. Dev Psychopathol 2006; 18: 1037–53
Noaghiul S, Hibbeln JR. Cross-national comparisons of seafood consumption and rates of bipolar disorders. Am J Psychiatry 2003; 160: 2222–7
Hibbeln JR. Fish consumption and major depression [letter]. Lancet 1998; 351(9110): 1213
Peet M. International variations in the outcome of schizophrenia and the prevalence of depression in relation to national dietary practices: an ecological analysis. Br J Psychiatry 2004; 184: 404–8
Colangelo LA, He K, Whooley MA, et al. Higher dietary intake of long-chain omega-3 polyunsaturated fatty acids is inversely associated with depressive symptoms in women. Nutrition 2009; 25: 1011–9
Golding J, Steer C, Emmett P, et al. High levels of depressive symptoms in pregnancy with low omega-3 fatty acid intake from fish. Epidemiology 2009; 20: 598–603
Kamphuis MH, Geerlings MI, Tijhuis MA, et al. Depression and cardiovascular mortality: a role for n-3 fatty acids? Am J Clin Nutr 2006; 84: 1513–7
Rees AM, Austin MP, Owen C, et al. Omega-3 deficiency associated with perinatal depression: case control study. Psychiatry Res 2009; 166: 254–9
Freeman MP, Hibbeln JR, Wisner KL, et al. Omega-3 fatty acids: evidence basis for treatment and future research in psychiatry. J Clin Psychiatry 2006; 67: 1954–67
Lin PY, Su KP. A meta-analytic review of double-blind, placebo-controlled trials of antidepressant efficacy of omega-3 fatty acids. J Clin Psychiatry 2007; 68: 1056–61
Cao J, Schwichtenberg KA, Hanson NQ, et al. Incorporation and clearance of omega-3 fatty acids in erythrocyte membranes and plasma phospholipids. Clin Chem 2006; 52: 2265–72
Sands SA, Reid KJ, Windsor SL, et al. The impact of age, body mass index, and fish intake on the EPA and DHA content of human erythrocytes. Lipids 2005; 40: 343–7
Itomura M, Fujioka S, Hamazaki K, et al. Factors influencing EPA+DHA levels in red blood cells in Japan. In Vivo 2008; 22: 131–5
Chiu CC, Huang SY, Su KP, et al. Polyunsaturated fatty acid deficit in patients with bipolar mania. Eur Neuropsychopharmacol 2003; 13: 99–103
Edwards R, Peet M, Shay J, et al. Omega-3 polyunsaturated fatty acid levels in the diet and in red blood cell membranes of depressed patients. J Affect Disord 1998; 48: 149–55
McNamara RK, Jandacek R, Rider T, et al. Selective deficits in erythrocyte docosahexaenoic acid composition in adult patients with bipolar disorder and major depressive disorder. J Affect Disord 2010; 126: 303–11
Peet M, Murphy B, Shay J, et al. Depletion of omega-3 fatty acid levels in red blood cell membranes of depressive patients. Biol Psychiatry 1998; 43: 315–9
Ranjekar PK, Hinge A, Hegde MV, et al. Decreased antioxidant enzymes and membrane essential polyunsaturated fatty acids in schizophrenic and bipolar mood disorder patients. Psychiatry Res 2003; 121: 109–22
Clayton EH, Hanstock TL, Hirneth SJ, et al. Long-chain omega-3 polyunsaturated fatty acids in the blood of children and adolescents with juvenile bipolar disorder compared to healthy controls. Lipids 2008; 43: 1031–8
McNamara RK, Sullivan J, Richtand NM. Omega-3 fatty acid deficiency augments the development of behavioral sensitization in adult mice: prevention by chronic lithium treatment. J Psychiatric Res 2008; 42: 458–68
McNamara RK, Sullivan J, Richtand NM, et al. Omega-3 fatty acid deficiency augments amphetamine-induced behavioral sensitization in adult DBA/2J mice: relationship with ventral striatum dopamine concentrations. Synapse 2008; 62: 725–35
Arvindakshan M, Ghate M, Ranjekar PK, et al. Supplementation with a combination of omega-3 fatty acids and antioxidants (vitamins E and C) improves the outcome of schizophrenia. Schizophr Res 2003; 62: 195–204
Fava M, Mischoulon D. Folate in depression: efficacy, safety, differences in formulations, and clinical issues. J Clin Psychiatry 2009; 70 Suppl. 5: 12–7
Folstein M, Liu T, Peter I, et al. The homocysteine hypothesis of depression. Am J Psychiatry 2007; 164: 861–7
Frazier EA, Fristad MA, Arnold LE. Multinutrient supplement as treatment: literature review and case report of a 12-year-old boy with bipolar disorder. J Child Adolesc Psychopharmacol 2009; 19: 453–60
Kilbourne AM, Rofey DL, McCarthy JF, et al. Nutrition and exercise behavior among patients with bipolar disorder. Bipolar Disord 2007; 9: 443–52
Kinney DK, Teixeira P, Hsu D, et al. Relation of schizophrenia prevalence to latitude, climate, fish consumption, infant mortality, and skin color: a role for prenatal vitamin D deficiency and infections? Schizophr Bull 2009; 35: 582–95
Lakhan SE, Vieira KF. Nutritional therapies for mental disorders. Nutr J 2008; 7: 2
Blumberg HP, Krystal JH, Bansal R, et al. Age, rapidcycling, and pharmacotherapy effects on ventral prefrontal cortex in bipolar disorder: a cross-sectional study. Biol Psychiatry 2006; 59: 611–8
Haznedar MM, Roversi F, Pallanti S, et al. Fronto-thalamostriatal gray and white matter volumes and anisotropy of their connections in bipolar spectrum illnesses. Biol Psychiatry 2005; 57: 733–42
Lopez-Larson MP, DelBello MP, Zimmerman ME, et al. Regional prefrontal gray and white matter abnormalities in bipolar disorder. Biol Psychiatry 2002; 52: 93–100
Lyoo IK, Kim MJ, Stoll AL, et al. Frontal lobe gray matter density decreases in bipolar I disorder. Biol Psychiatry 2004; 55: 648–51
Stanfield AC, Moorhead TW, Job DE, et al. Structural abnormalities of ventrolateral and orbitofrontal cortex in patients with familial bipolar disorder. Bipolar Disord 2009; 11: 135–44
Adler CM, DelBello MP, Jarvis K, et al. Voxel-based study of structural changes in first-episode patients with bipolar disorder. Biol Psychiatry 2007; 61: 776–81
Gogtay N, Ordonez A, Herman DH, et al. Dynamic mapping of cortical development before and after the onset of pediatric bipolar illness. J Child Psychol Psychiatry 2007; 48: 852–62
Kalmar JH, Wang F, Spencer L, et al. Preliminary evidence for progressive prefrontal abnormalities in adolescents and young adults with bipolar disorder. J Int Neuropsychol Soc 2009; 15: 476–81
Cotter D, Hudson L, Landau S. Evidence for orbitofrontal pathology in bipolar disorder and major depression, but not in schizophrenia. Bipolar Disord 2005; 7: 358–69
Rajkowska G. Postmortem studies in mood disorders indicate altered numbers of neurons and glial cells. Biol Psychiatry 2000; 48: 766–77
Adler CM, Adams J, DelBello MP, et al. Evidence of white matter pathology in bipolar disorder adolescents experiencing their first episode of mania: a diffusion tensor imaging study. Am J Psychiatry 2006; 163: 322–4
Beyer JL, Taylor WD, MacFall JR, et al. Cortical white matter microstructural abnormalities in bipolar disorder. Neuropsychopharmacology 2005; 30: 2225–9
Mahon K, Wu J, Malhotra AK, et al. A voxel-based diffusion tensor imaging study of white matter in bipolar disorder. Neuropsychopharmacology 2009; 34: 1590–600
Kafantaris V, Kingsley P, Ardekani B, et al. Lower orbital frontal white matter integrity in adolescents with bipolar I disorder. J Am Acad Child Adolesc Psychiatry 2009; 48: 79–86
Kringelbach ML, Rolls ET. The functional neuroanatomy of the human orbitofrontal cortex: evidence from neuroimaging and neuropsychology. Prog Neurobiol 2004; 72: 341–72
Quirk GJ, Likhtik E, Pelletier JG, et al. Stimulation of medial prefrontal cortex decreases the responsiveness of central amygdala output neurons. J Neurosci 2003; 23: 8800–7
Monk CS, Telzer EH, Mogg K, et al. Amygdala and ventrolateral prefrontal cortex activation to masked angry faces in children and adolescents with generalized anxiety disorder. Arch Gen Psychiatry 2008; 65: 568–76
Nomura M, Ohira H, Haneda K, et al. Functional association of the amygdala and ventral prefrontal cortex during cognitive evaluation of facial expressions primed by masked angry faces: an event-related fMRI study. Neuroimage 2004; 21: 352–63
Ohira H, Nomura M, Ichikawa N, et al. Association of neural and physiological responses during voluntary emotion suppression. Neuroimage 2006; 29: 721–33
Urry HL, van Reekum CM, Johnstone T, et al. Amygdala and ventromedial prefrontal cortex are inversely coupled during regulation of negative affect and predict the diurnal pattern of cortisol secretion among older adults. J Neurosci 2006; 26: 4415–25
Rich BA, Vinton DT, Roberson-Nay R, et al. Limbic hyperactivation during processing of neutral facial expressions in children with bipolar disorder. Proc Natl Acad Sci U S A 2006; 103: 8900–5
Yurgelun-Todd DA, Gruber SA, Kanayama G, et al. fMRI during affect discrimination in bipolar affective disorder. Bipolar Disord 2000; 2 (3 Pt 2): 237–48
Kalmar JH, Wang F, Chepenik LG, et al. Relation between amygdala structure and function in adolescents with bipolar disorder. J Am Acad Child Adolesc Psychiatry 2009; 48: 636–42
Pavuluri MN, O’Connor MM, Harral E, et al. Affective neural circuitry during facial emotion processing in pediatric bipolar disorder. Biol Psychiatry 2007; 62: 158–67
Altshuler L, Bookheimer S, Proenza MA, et al. Increased amygdala activation during mania: a functional magnetic resonance imaging study. Am J Psychiatry 2005; 162: 1211–3
Altshuler LL, Bookheimer SY, Townsend J, et al. Blunted activation in orbitofrontal cortex during mania: a functional magnetic resonance imaging study. Biol Psychiatry 2005; 58: 763–9
Blumberg HP, Stern E, Ricketts S, et al. Rostral and orbital prefrontal cortex dysfunction in the manic state of bipolar disorder. Am J Psychiatry 1999; 156: 1986–8
Elliott R, Ogilvie A, Rubinsztein JS, et al. Abnormal ventral frontal response during performance of an affective go/no go task in patients with mania. Biol Psychiatry 2004; 55: 1163–70
Pfeifer JC, Welge J, Strakowski SM, et al. Meta-analysis of amygdala volumes in children and adolescents with bipolar disorder. J Am Acad Child Adolesc Psychiatry 2008; 47: 1289–98
Findling RL, Youngstrom EA, McNamara NK, et al. Early symptoms of mania and the role of parental risk. Bipolar Disord 2005; 7: 623–34
Birmaher B, Axelson D, Strober M, et al. Clinical course of children and adolescents with bipolar spectrum disorders. Arch Gen Psychiatry 2006; 63: 175–83
Egeland JA, Hostetter AM, Pauls DL, et al. Prodromal symptoms before onset of manic-depressive disorder suggested by first hospital admission histories. J Am Acad Child Adolesc Psychiatry 2000; 39: 1245–52
Biederman J, Monuteaux MC, Mick E, et al. Psychopathology in females with attention-deficit/hyperactivity disorder: a controlled, five-year prospective study. Biol Psychiatry 2006; 60: 1098–105
Carlson GA. Mania and ADHD: comorbidity or confusion. J Affect Disord 1998; 51: 177–87
West SA, Strakowski SM, Sax KW, et al. The comorbidity of attention-deficit hyperactivity disorder in adolescent mania: potential diagnostic and treatment implications. Psychopharmacol Bull 1995; 31: 347–51
Singh MK, DelBello MP, Kowatch RA, et al. Co-occurrence of bipolar and attention-deficit hyperactivity disorders in children. Bipolar Disord 2006; 8: 710–20
Reddy JYC, Srinath S, Jairam R. Pediatric bipolar disorder: from the perspective of India. In: Diler RS, editor. Pediatric bipolar disorder: a global perspective. New York: Nova Science Publishers, 2007: 91–106
Bock N, Quentin DJ, Hüther G, et al. Very early treatment with fluoxetine and reboxetine causing long-lasting change of the serotonin but not the noradrenaline transporter in the frontal cortex of rats. World J Biol Psychiatry 2005; 6: 107–12
LaRoche RB, Morgan RE. Adolescent fluoxetine exposure produces enduring, sex-specific alterations of visual discrimination and attention in rats. Neurotoxicol Teratol 2007; 29: 96–107
Youngs RM, Chu MS, Meloni EG, et al. Lithium administration to preadolescent rats causes long-lasting increases in anxiety-like behavior and has molecular consequences. J Neurosci 2006; 26: 6031–9
McPherson CS, Lawrence AJ. Exposure to amphetamine in rats during periadolescence establishes behavioural and extrastriatal neural sensitization in adulthood. Int J Neuropsychopharmacol 2006; 9: 377–92
Colom F, Vieta E. A perspective on the use of psychoeducation, cognitive-behavioral therapy and interpersonal therapy for bipolar patients. Bipolar Disord 2004; 6: 480–6
West AE, Pavuluri MN. Psychosocial treatments for childhood and adolescent bipolar disorder. Child Adolesc Psychiatr Clin N Am 2009; 18: 471–82
Nandagopal JJ, DelBello MP, Kowatch R. Pharmacologic treatment of pediatric bipolar disorder. Child Adolesc Psychiatr Clin N Am 2009; 18: 455–69
Geller B, Cooper TB, Zimerman B, et al. Lithium for prepubertal depressed children with family history predictors of future bipolarity: a double-blind, placebo-controlled study. J Affect Disord 1998; 51: 165–75
Chang KD, Dienes K, Blasey C, et al. Divalproex monotherapy in the treatment of bipolar offspring with mood and behavioral disorders and at least mild affective symptoms. J Clin Psychiatry 2003; 64: 936–42
Saxena K, Howe M, Simeonova D, et al. Divalproex sodium reduces overall aggression in youth at high risk for bipolar disorder. J Child Adolesc Psychopharmacol 2006; 16: 252–9
Findling RL, Frazier TW, Youngstrom EA, et al. Double-blind, placebo-controlled trial of divalproex monotherapy in the treatment of symptomatic youth at high risk for developing bipolar disorder. J Clin Psychiatry 2007; 68: 781–8
DelBello MP, Adler CM, Whitsel RM, et al. A 12-week single-blind trial of quetiapine for the treatment of mood symptoms in adolescents at high risk for developing bipolar I disorder. J Clin Psychiatry 2007; 68: 789–95
Nemets H, Nemets B, Apter A, et al. Omega-3 treatment of childhood depression: a controlled, double-blind pilot study. Am J Psychiatry 2006; 163: 1098–100
Clayton EH, Hanstock TL, Hirneth SJ, et al. Reduced mania and depression in juvenile bipolar disorder associated with long-chain omega-3 polyunsaturated fatty acid supplementation. Eur J Clin Nutr 2009; 63: 1037–40
Wozniak J, Biederman J, Mick E, et al. Omega-3 fatty acid monotherapy for pediatric bipolar disorder: a prospective open-label trial. Eur Neuropsychopharmacol 2007; 17: 440–7
Amminger GP, Schäfer MR, Papageorgiou K, et al. Longchain omega-3 fatty acids for indicated prevention of psychotic disorders: a randomized, placebo-controlled trial. Arch Gen Psychiatry 2010; 67: 146–54
Beltz BS, Tlusty MF, Benton JL, et al. Omega-3 fatty acids upregulate adult neurogenesis. Neurosci Lett 2007; 415: 154–8
Kawakita E, Hashimoto M, Shido O. Docosahexaenoic acid promotes neurogenesis in vitro and in vivo. Neuroscience 2006; 139: 991–7
Coti Bertrand P, O’Kusky JR, Innis SM. Maternal dietary (n-3) fatty acid deficiency alters neurogenesis in the embryonic rat brain. J Nutr 2006; 136: 1570–5
Yavin E, Himovichi E, Eilam R. Delayed cell migration in the developing rat brain following maternal omega 3 alpha linolenic acid dietary deficiency. Neuroscience 2009; 162: 1011–122
Calderon F, Kim HY. Docosahexaenoic acid promotes neurite growth in hippocampal neurons. J Neurochem 2004; 90: 979–88
Ikemoto A, Nitta A, Furukawa S, et al. Dietary n-3 fatty acid deficiency decreases nerve growth factor content in rat hippocampus. Neurosci Lett 2000; 285: 99–102
Rao JS, Ertley RN, Lee HJ, et al. n-3 polyunsaturated fatty acid deprivation in rats decreases frontal cortex BDNF via a p38 MAPK-dependent mechanism. Mol Psychiatry 2007; 12: 36–46
Belayev L, Khoutorova L, Atkins KD, et al. Robust docosahexaenoic acid-mediated neuroprotection in a rat model of transient, focal cerebral ischemia. Stroke 2009; 40: 3121–6
Bazan NG. Cellular and molecular events mediated by docosahexaenoic acid-derived neuroprotectin D1 signaling in photoreceptor cell survival and brain protection. Prostaglandins Leukot Essent Fatty Acids 2009; 81: 205–11
Blondeau N, Widmann C, Lazdunski M, et al. Polyunsaturated fatty acids induce ischemic and epileptic tolerance. Neuroscience 2002; 109: 231–41
Green P, Glozman S, Weiner L, et al. Enhanced free radical scavenging and decreased lipid peroxidation in the rat fetal brain after treatment with ethyl docosahexaenoate. Biochim Biophys Acta 2001; 1532: 203–12
Högyes E, Nyakas C, Kiliaan A, et al. Neuroprotective effect of developmental docosahexaenoic acid supplement against excitotoxic brain damage in infant rats. Neuroscience 2003; 119: 999–1012
Ozyurt B, Sarsilmaz M, Akpolat N, et al. The protective effects of omega-3 fatty acids against MK-801-induced neurotoxicity in prefrontal cortex of rat. Neurochem Int 2007; 50: 196–202
Conklin SM, Gianaros PJ, Brown SM, et al. Long-chain omega-3 fatty acid intake is associated positively with corticolimbic gray matter volume in healthy adults. Neurosci Lett 2007; 421: 209–12
Frangou S, Lewis M, Wollard J, et al. Preliminary in vivo evidence of increased N-acetyl-aspartate following eicosapentanoic acid treatment in patients with bipolar disorder. J Psychopharmacol 2007; 21: 435–9
McNamara RK, Able J, Jandacek R, et al. Docosahexaenoic acid supplementation increases prefrontal cortex activation during sustained attention in healthy boys: a placebo-controlled, dose-ranging, functional magnetic resonance imaging study. Am J Clin Nutr 2010; 91: 1060–7
Yung AR, Nelson B, Thompson AD, et al. Should a “risk syndrome for psychosis” be included in the DSMV? Schizophr Res 2010; 120: 7–15
Acknowledgements
The work was supported in part by National Institutes of Health (NIH) grants MH080973 to M.P.D., MH083924 to R.K.M. and M.P.D., and MH077138 to S.M.S. R.K.M. has received research support from Martek Biosciences Inc., Inflammation Research Foundation, Ortho-McNeil Janssen, AstraZeneca, Eli Lilly, National Alliance for Research on Schizophrenia And Depression (NARSAD), National Institute of Mental Health (NIMH) and National Institute on Aging (NIA). J.J.N. has received research support from AstraZeneca, BMS/Otsuka, Eli Lilly, GlaxoSmithKline, Pfizer, Johnson & Johnson, Shire, Abbott, Janssen, Martek Biosciences Inc., Somerset, Repligen, Sumitomo, National Institute on Drug Abuse (NIDA), NIMH, National Institute on Alcohol Abuse and Alcoholism (NIAAA) and NARSAD. S.M.S. has received research grant support from Eli Lilly, Janssen, AstraZeneca, Nutrition 21, Martek Biosciences Inc., Repligen, NIDA, NIAAA, NARSAD, NIMH and Thrasher Foundation, and is a consultant for Pfizer. M.P.D. has received research support from AstraZeneca, Eli Lilly, Martek, Johnson & Johnson, Shire, Ortho-McNeil, Janssen, Pfizer, Bristol Myers Squibb, Repligen, Somerset, Sumitomo, Thrasher Foundation, GlaxoSmithKline, NARSAD, NIMH, NIDA and NIAAA, and is a consultant for GlaxoSmithKline, Eli Lilly, France Foundation, Kappa Clinical, Pfizer, Medical Communications Media, Schering-Plough and Merck.
GlaxoSmithKline, Martek Biosciences Inc. and the Inflammation Research Foundation market omega-3 fatty acid preparations. None of these funding sources had any role in the design, implementation or writing of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
McNamara, R.K., Nandagopal, J.J., Strakowski, S.M. et al. Preventative Strategies for Early-Onset Bipolar Disorder. CNS Drugs 24, 983–996 (2010). https://doi.org/10.2165/11539700-000000000-00000
Published:
Issue Date:
DOI: https://doi.org/10.2165/11539700-000000000-00000