Abstract
The concept of ‘continuity of care’ or ‘seamless care’ refers to the transition that occurs when a patient is discharged from an acute care setting to an outpatient community environment. In order to prevent errors and to ensure appropriate follow-up during this transition, communication between all healthcare disciplines is required to guarantee the implementation of an appropriate, successful treatment plan following hospital discharge. Major accrediting organizations now require the process of medication reconciliation upon hospital admission and the provision of a comprehensive list of the patient’s medications to the next healthcare provider following hospital discharge.
While the process of medication reconciliation is an important step toward improving the transfer of information from an acute care environment to the community care setting, it is limited in scope and generally only involves the primary care physician. Unfortunately, consistent infrastructures for the provision of continuity of care are lacking when a patient transitions from the acute care environment to the community care setting. The community pharmacist is often not provided with any information regarding the patient’s recent hospitalization or changes that may have been made to their medications. Comprehensive review of the patient’s medications in both the inpatient and community settings, as well as the communication that would need to occur among healthcare providers, requires a significant time commitment by pharmacists.
Medication therapy management programs, which are starting to grow within the community pharmacy setting, may assist with continuity of care by providing patients with a personal medication record that can be shared with their healthcare providers, as well as presented at admission to the hospital to assist with medication reconciliation efforts. While it is evident that identification and resolution of drug-related problems can have a significant impact on healthcare cost and patient safety, the issue of compensation for the provision of these types of services still needs to be addressed.
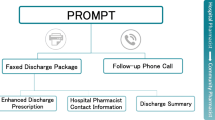
Upon discharge, a minimum set of information should be provided by discharging institutions to community pharmacies to ensure continuity of care. Information provided to the community pharmacy at discharge should include patient demographics, third-party prescription insurance information, new medications and associated indications, along with the name of the prescribing physician, changes to pre-admission medications (including dose changes and discontinuations), the reason for hospitalization, and follow-up plan formulated in association with the healthcare providers. Ideally, this information would be provided in a means that is easily readable, preferably electronic or printed as opposed to handwritten in order to reduce errors.
The success of continuity of care in optimizing the transition of the patient from the inpatient setting to the community setting is highly dependent on the effective cooperation and communication between all components of the healthcare system. More studies are needed to evaluate the impact of cost due to the additional resources needed to appropriately implement an effective continuity of care system.
Similar content being viewed by others
References
ASHP Continuity of Care Task Force. Continuity of care in medication management: review of issues and considerations for pharmacy. Am J Health Syst Pharm 2005 Aug; 62: 1714–20
Proceedings of the Seamless Care Workshop; 2000 Sep 29–Oct 1; Val Morin (QC): Canadian Society of Hospital Pharmacists and Canadian Pharmacists Association, 2001
The Joint Commission. National patient safety goals: facts about the national patient safety goals [online]. Available from URL: http://www.jointcommission.org/PatientSafety/NationalPatientSafetyGoals/07_npsg_facts.htm [Accessed 2007 Aug 12]
Canadian Council on Health Services Accreditation. CCHSA patient safety goals and required organizational practices [online]. Available from URL: http://www.cchsa.ca/default.aspx?page=139 [Accessed 2008 Apr 13]
Kliethermes MA. Continuity of care: the significance of the pharmacist’s role. Am J Health Syst Pharm 2003; 60: 1787–90
American Pharmacists Association — Academy of Pharmacy Research and Science. Continuity of care: can the whole health care team be linked together?. J Am Pharm Assoc 2006; 46(4): 427–30
Munday A, Kelly B, Forrester JWE, et al. Do general practitioners and community pharmacists want information on the reasons for drug therapy changes implemented in secondary care?. Br J Gen Prac 1997 Sep; 47(422): 563–6
Nickerson A, MacKinnon NJ, Roberts N, et al. Drug therapy problems, inconsistencies and omissions identified during a medication reconciliation and seamless care service. Healthc Q 2005; 8 Suppl.: 65–72
Paulino EI, Bouvy ML, Gastelurrutia MA, et al. Drug related problems identified by European community pharmacists in patients discharged from hospital. Pharm World Sci 2004 Dec; 26(6): 353–60
Dvorak SR, McCoy RA, Voss GD. Continuity of care from acute to ambulatory care setting. Am J Health Syst Pharm 1998 Dec; 55(23): 2500–4
Brookes K, Scott MG, McConnell JB, et al. Benefits of a hospital based community services liaison pharmacist. Pharm World Sci 2000; 22(2): 33–8
Moving toward a patient-centered integrated medication-use system. In: Aspden P, Wolcott JA, Bootman JL, et al., editors. Preventing medication errors. Washington, DC: The National Academies Press, 2007: 143–50
Bodeheimer T. Coordinating care: a major (unreimbursed) task of primary care [editorial]. Ann Int Med 2007 Nov; 147(10): 730–1
Action agenda for health care organizations. In: Aspden P, Wolcott JA, Bootman JL, et al., editors. Preventing medication errors. Washington, DC: The National Academies Press, 2007: 221–65
Coleman EA. Falling through the cracks: challenges and opportunities for improving transitional care for persons with continuous complex care needs. J Am Geratr Soc 2003 Apr; 51(4): 549–55
American Pharmacists Association and National Association of Chain Drug Stores Foundation. Medication therapy management in pharmacy practice: core elements of an MTM service model. Version 2.0. 2008 Mar [online]. Available from URL: http://www.pharmacist.com/mtm/coreelements2 [Accessed 2008 Apr 13]
Acknowledgments
No sources of funding were used to assist in the preparation of this article. The authors have no conflicts of interest that are directly relevant to the content of this article.
The authors would like to thank Robert Michocki, PharmD, BCPS, for his assistance in the development of this current opinion paper.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Layson-Wolf, C., Morgan, J.A. Pharmacy Continuity of Care. Dis-Manage-Health-Outcomes 16, 199–203 (2008). https://doi.org/10.2165/00115677-200816040-00001
Published:
Issue Date:
DOI: https://doi.org/10.2165/00115677-200816040-00001