Abstract
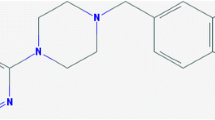
Objectives: Cabergoline is an ergoline derivative with a very long half-life that allows once-daily administration and the potential for more continuous stimulation of dopaminergic receptors than is possible with other dopamine receptor agonists (DAs). The aim of this study was to evaluate whether the possible advantage resulting from a more sustained dopaminergic effect of cabergoline would translate into delayed onset of motor complications, compared with levodopa, in patients with newly diagnosed Parkinson’s disease.
Study design and methods: This study was a double-blind, multicentre trial that compared cabergoline and levodopa as initial therapy for Parkinson’s disease. A total of 419 levodopa-, DA-and selegiline-naive patients with newly diagnosed Parkinson’s disease were randomised to receive either cabergoline (n = 211) or levodopa (n = 209). Treatment was titrated to an optimal dose over a period of up to 24 weeks and then continued at this dose until the study endpoint (confirmed motor complications) or up to a maximum of 5 years. At years 1–5, the cabergoline group was receiving cabergoline at average daily doses ranging from 2.8–2.9mg, with added levodopa at mean daily doses ranging from 322mg at year 1 to 431mg at year 5; over the same period, the levodopa group was receiving daily levodopa doses of 784mg. Thus, patients in the cabergoline group received >50% levodopa than patients in the levodopa group.
Results: Motor complications were significantly delayed (p = 0.0175) and occurred less frequently in cabergoline-treated patients than in levodopa-treated patients (22.3% vs 33.7%). Cox model proportional hazards regression analysis showed that the relative risk of developing such complications was >50% lower (0.46; p < 0.001) in the cabergoline group compared with the levodopa group. In particular, development of dyskinesias was markedly delayed in the cabergoline group and occurred in 9.5% of patients compared with 21.2% in the levodopa group (p < 0.001).
Among patients not requiring supplemental levodopa, the frequency of motor complications was three times higher with levodopa (15.5% of 110 patients) than with cabergoline (5.3% of 76 patients). Among patients who did need supplemental levodopa, motor complications were more frequent in the levodopa arm (54.1% of 98 patients) than in the cabergoline arm (31.9% of 135 patients).
Consistent improvements relative to baseline in average Unified Parkinson’s Disease Rating Scale (UPDRS) daily living activities and motor function sections, and in Clinical Global Impression severity of illness and physician-and patient-rated global improvement scores, were seen in both treatment groups, with maximal effects occurring within 2 years. However, levodopa treatment was associated with a significantly (p < 0.001) greater improvement in motor disability (as measured by the UPDRS motor score) over time, with mean values of 13.8 versus 12.9 in the cabergoline versus levodopa arm recorded at 1 year, 18.6 versus 17.2 at 3 years and 19.2 versus 16.3 at 5 years, respectively.
While the overall frequency of adverse events was similar in the two groups, the cabergoline-treated group experienced marginally, but not significantly, higher frequencies of nausea, vomiting, dyspepsia and gastritis (37.4% vs 32.2% in the levodopa group) and of dizziness and postural hypotension (31.3% vs 24% in the levodopa group). Cabergoline-treated patients also experienced a significantly higher frequency of peripheral oedema (16.1% vs 3.4%, respectively; p < 0.0001). The cabergoline and levodopa groups had similar rates of sleepiness (17.5% vs 18.3%, respectively) and hallucinations (4.8% vs 4.4%, respectively); in an elderly population subset, hallucinations were reported in 7.1% and 6.5% of patients taking cabergoline and levodopa, respectively. Adverse events generally occurred more frequently in female patients (with the exception of dyskinesias, hyperkinesias and hallucinations, which occurred more frequently in men) and in the elderly.
Conclusion: This study showed that, compared with levodopa, initial therapy with cabergoline in patients with Parkinson’s disease is associated with a lower risk of response fluctuations at the cost of a marginally reduced symptomatic improvement and some tolerability disadvantages that are mostly limited to a significantly higher frequency of peripheral oedema.











Similar content being viewed by others
References
Jankovic J. Levodopa strengths and weaknesses. Neurology 2002; 58: S19–32
Rinne UK. Recent advances in research on parkinsonism. Acta Neurol Scand 1978; 57: 77–113
Bravi D, Mouradian MM, Roberts JW, et al. Wearing-off fluctuations in Parkinson’s disease: contribution of postsynaptic mechanisms. Ann Neurol 1994; 36: 27–31
Leenders KL, Palmer AJ, Quinn N, et al. Brain dopamine metabolism in patients with Parkinson’s disease measured with positron emission tomography. J Neurol Neurosurg Psychiatry 1986; 49: 853–60
Rodriguez M, Lera G, Vaamonde J, et al. Motor response to apomorphine and levodopa in asymmetric Parkinson’s disease. J Neurol Neurosurg Psychiatry 1994; 57: 562–6
Hubble JP, Koller WC, Cutler NR, et al. Pramipexole in patients with early Parkinson’s disease. Clin Neuropharmacol 1995; 18: 338–47
Tanner CM. Dopamine agonists in early therapy for Parkinson disease. JAMA 2000; 284: 1971–3
Montastruc JL, Rascol O, Senard JM, et al. A randomised controlled study comparing bromocriptine to which levodopa was later added, with levodopa alone in previously untreated patients with Parkinson’s disease: a five year follow up. J Neurol Neurosurg Psychiatry 1994; 57: 1034–8
Rinne UK, Bracco F, Chouza C, et al. Cabergoline in the treatment of early Parkinson’s disease: results of the first year of treatment in a double-blind comparison of cabergoline and levodopa. Neurology 1997; 48: 363–8
Wiseman LR, Fitton A. Cabergoline: a review of its efficacy in the treatment of Parkinson’s disease. CNS Drugs 1999; 12: 485–97
Barone P, Bravi D, Bermejo-Pareja F, et al. Pergolide monotherapy in the treatment of early PD: a randomized, controlled study. Neurology 1999; 53: 573–9
Parkinson Study Group. Pramipexole vs levodopa as initial treatment for Parkinson disease. JAMA 2000; 284: 1931–8
Rascol O, Brooks DJ, Korczyn AD, et al. A five-year study of the incidence of dyskinesia in patients with early Parkinson’s disease who were treated with ropinirole or levodopa. N Engl J Med 2000; 342: 1484–91
Rascol O. Dopamine agonists: what is the place of the newer compounds in the treatment of Parkinson’s disease? J Neural Transm Suppl 1999; 55: 33–45
Rinne UK, Bracco F, Chouza C, et al. Early treatment of Parkinson’s disease with cabergoline delays the onset of motor complications: results of a double-blind levodopa controlled trial. Drugs 1998; 55 Suppl. 1: 20–3
Marubini E, Valsecchi MG. Analyzing survival data from clinical trials and observational studies. New York: John Wiley & Sons, 1995
Everitt BS. The analysis of repeated measures: a practical review with examples. Statistician 1995; 44: 113–35
Block G, Liss C, Reines S, et al. Comparison of immediate-release and controlled release carbidopa/levodopa in Parkinson’s disease: a multicenter 5-year study. The CR First Study Group. Eur Neurol 1997; 37: 23–7
Miyasaki JM, Martin W, Suchowersky O, et al. Practice parameter: initiation of treatment for Parkinson’s disease: an evidence-based review. Report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology 2002; 58: 11–7
Ahlskog JE. Slowing Parkinson’s disease progression: recent dopamine agonist trials. Neurology 2003; 60(3): 381–9
Albin RL, Frey KA. Initial agonist treatment of Parkinson disease: a critique. Neurology 2003; 60(3): 390–4
Acknowledgements
The authors thank Adriana Dubini and Bruno Musch for their cooperation in the preparation of the manuscript. The study was funded by Farmitalia Carlo Erba as part of the Cabergoline phase III Parkinson’s Disease clinical development programme.
Author information
Authors and Affiliations
Consortia
Corresponding author
Rights and permissions
About this article
Cite this article
Bracco, F., Battaglia, A., Chouza, C. et al. The Long-Acting Dopamine Receptor Agonist Cabergoline in Early Parkinson’s Disease. CNS Drugs 18, 733–746 (2004). https://doi.org/10.2165/00023210-200418110-00003
Published:
Issue Date:
DOI: https://doi.org/10.2165/00023210-200418110-00003