Summary
Abstract
Risedronate is a novel orally administered pyridinyl bisphosphonate indicated for the prevention or treatment of postmenopausal and glucocorticoid-induced osteoporosis and Paget’s disease. The drug reduces bone turnover and decreases resorption chiefly through osteoclastic effects, with no undesirable effects on cortical porosity or thickness or on cancellous bone volume.
Four randomised, double-blind trials have been carried out in 4873 patients with postmenopausal osteoporosis. In 2 of these studies, the primary end-point of vertebral fracture incidence was reduced by risedronate 5mg once daily by up to 65 and 49% relative to placebo after 1 and 3 years, respectively. Across all 4 trials, risedronate improved lumbar spine, femoral neck and femoral trochanter bone mineral density (BMD) statistically significantly relative to placebo. The drug also prevented bone loss in a study in 383 women with recent menopause, and reduced the risk of hip fracture in elderly women with confirmed osteoporosis in a trial involving a total of 9331 patients. Risedronate 5 mg/day plus estrogen has been shown to be superior to estrogen alone in a 12-month double-blind study in 524 women with at least 1-year’s history of menopause.
Two randomised, double-blind and placebo-controlled 12-month studies in a total of 518 patients have shown risedronate 5 mg/day to prevent or reverse bone loss in patients receiving glucocorticoid therapy.
Risedronate 30 mg/day was associated with statistically significant reductions in mean serum levels of alkaline phosphatase (ALP) in noncomparative studies in patients with Paget’s disease. ALP normalisation rates ranged from 53.8 to 65% across two 84-day treatment cycles in 2 of these trials in 180 patients. In a randomised, double-blind study in 123 patients, risedronate 30 mg/day for 2 months evoked significantly greater serum ALP responses than etidronate 400 mg/day for 6 months.
The overall tolerability profile of risedronate was similar to that of placebo in clinical studies, with no evidence of acute-phase reactions or mineralisation defects, or excess incidence of upper GI lesions, in patients receiving the drug.
Conclusions: Risedronate is an effective and well tolerated novel bisphosphonate that is suitable for first-line therapy in Paget’s disease. The rapid and sustained reductions in vertebral fracture incidence and BMD changes seen in patients with postmenopausal and glucocorticoid-induced osteoporosis indicate the drug to be a valuable treatment option with first-line potential, particularly in patients for whom hormonal therapy is inappropriate. The effects of the drug on hip fracture incidence in elderly women with confirmed osteoporosis point to a particular role in older patients, or those with more advanced disease.
Pharmacological Profile
Risedronate inhibits bone resorption by interfering with the recruitment and activity of osteoclasts. As with other bisphosphonates, the drug is believed also to inhibit osteoclastic adhesion to mineralised bone matrix and to shorten the osteoclastic life span.
Risedronate 5 mg/day (all dosages quoted are oral unless stated otherwise) reduces bone turnover as shown consistently in clinical studies in postmenopausal women and patients with Paget’s disease by statistically significant reductions relative to placebo in serum levels of bone-specific ALP. Maximal reductions are typically obtained after 6 months’ treatment and are accompanied by reductions in urinary markers of bone resorption (e.g. N-telopeptide and deoxypyridinoline).
Histomorphometric analysis in patients receiving risedronate for corticosteroid-induced osteoporosis showed decreased resorption depth with unchanged rates of resorption (resulting in a net decrease in bone resorption) with the drug. There were no undesirable effects on cortical porosity or thickness or on cancellous bone volume. Trabecular width and rates of mineralisation remained unchanged, and bone turnover decreased, in patients with skeletal deterioration caused by multiple myeloma who received risedronate.
Risedronate undergoes rapid absorption and shows a dose-proportional pharmacokinetic profile after oral administration. Mean peak serum concentrations (Cmax) of risedronate were 0.41, 0.94 and 5.1 μg/L after single doses of 1.5, 5 and 30mg, respectively, in healthy volunteers. Mean times to Cmaxranged from 0.81 to 0.87 hours. GI absorption of the drug is impaired by the presence of food, and by calcium-, magnesium- or aluminium-containing compounds.
The volume of distribution at steady state of risedronate was 6.3 L/kg after intravenous administration in 1 study. The terminal elimination half-life is long (480 hours), and the drug is excreted unchanged largely via the kidneys, with renal clearance (CLR) accounting for 87% of total clearance. CLR and volume of distribution are related linearly to creatinine clearance (CLCR). Risedronate is known not to interfere with the function of hepatic microsomal cytochrome P450 enzymes.
Therapeutic Use
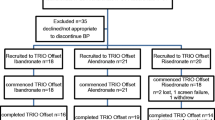
Postmenopausal Osteoporosis. Following the demonstration of efficacy relative to placebo of risedronate in women with postmenopausal osteoporosis in phase II studies, the drug was compared with placebo in a series of 6 randomised, double-blind phase III clinical trials. Four of these studies involved risedronate treatment of 4873 patients with low bone mass; vertebral fracture incidence was measured as the primary end-point in 2 of these, which involved women with established osteoporosis at baseline. The other studies focused on prevention of osteoporosis (i.e. maintenance of baseline bone mass) in women with recent menopause, and reduction of risk of hip fracture in elderly women.
Statistically significant improvements relative to placebo in vertebral fracture incidence and/or in lumbar spine, femoral neck and femoral trochanter BMD were seen consistently with risedronate 5mg once daily. In the 2 vertebral fracture studies, significant (61 and 65%; p ≤ 0.001 vs placebo) reductions in vertebral fracture risk were evident with risedronate treatment by the end of the first year. The risk of new fractures was reduced over 3 years by 41 (p = 0.003) and 49% (p < 0.001) relative to placebo. There were also substantial (39 and 33%) reductions in the risk of nonvertebral fracture (the first of these 2 results was also statistically significant).
Statistically significant improvements relative to placebo in BMD were noted from 6 months onwards with risedronate 5 mg/day in the vertebral fracture studies. After 3 years, mean treatment differences of 5.9, 6.4, 3.1 and 2.1% were reported for the lumbar spine, femoral trochanter, femoral neck and midshaft radius, respectively (all p < 0.001 vs placebo), in 1 trial.
In the 2 studies in patients with low baseline bone mass in which BMD was the primary end-point, mean lumbar spine BMD increased from baseline by 4.1% over 2 years (p < 0.001 vs placebo) in 1 trial and by 4.7% over 18 months (p < 0.05 vs placebo) in the other with risedronate 5 mg/day.
Statistically significant increases relative to both baseline and placebo with risedronate 5 mg/day in spinal and hip BMD were reported from as early as 3 months after starting treatment in a preliminary report of the bone loss prevention study in 383 women with a history of recent (6 to 36 months) menopause.
Risedronate treatment reduced the risk of the primary end-point of hip fracture in elderly women with established osteoporosis as confirmed by low BMD in a 3-year study in which 9331 patients were randomised within 2 strata to risedronate 2.5 or 5mg daily or placebo. In group 1 (patients aged 70 to 79 years with confirmed osteoporosis at baseline), hip fracture incidences were 1.9% with risedronate and 3.2% with placebo (relative risk 0.6; p = 0.009). The relative risk of hip fracture associated with risedronate treatment in 1703 women in group 1 with evidence of at least 1 vertebral fracture at baseline was 0.4 (p = 0.003 vs placebo). The corresponding relative risk in 2648 group 1 women with no history of vertebral fracture was 0.6 (p = 0.14).
There was no significant effect of risedronate treatment on hip fracture risk in group 2 (patients aged 80 years and over, most of whom were recruited on the basis of presence of clinical risk factors only): hip fracture incidences of 4.2 and 5.1% were reported for the risedronate and placebo groups, respectively (p = 0.35). Further analysis suggested that the majority of patients in group 2 did not have osteoporosis. Overall, incidences of hip fracture were 2.8% in all women who received risedronate and 3.9% in those who received placebo in this study (relative risk 0.7; p = 0.02).
BMD measurements indicated superiority of risedronate 5 mg/day plus estrogen therapy (n = 261) over estrogen alone (n = 263) in a 12-month double-blind placebo-controlled study in women with at least 1 year’s history of menopause. Improvements with risedronate plus estrogen were significantly greater than those with estrogen alone at 6 months for the lumbar spine and at 12 months for the femoral neck and midshaft radius.
Glucocorticoid-Induced Osteoporosis. In a randomised, double-blind, placebo-controlled phase III study in 228 patients starting glucocorticoid therapy, lumbar spine, femoral neck and femoral trochanter BMD decreased from baseline by around 3% over 12 months in patients receiving placebo. In contrast, BMD was maintained at the lumbar spine and femoral neck, and was increased at the femoral trochanter, with risedronate 5 mg/day. Least squares mean differences from placebo were 3.8, 4.1 and 4.6%, respectively (all p < 0.001). BMD was also maintained in recipients of risedronate 2.5 mg/day, but effects were less marked than with the 5 mg/day dosage. Distal and midshaft radius BMD did not change significantly relative to baseline in any group, and there were no statistically significant differences from placebo with either active treatment.
Risedronate 5 mg/day significantly increased BMD relative to placebo at the lumbar spine and the femoral neck and trochanter in 290 patients on glucocorticoid therapy and with low BMD at baseline in another 12-month randomised double-blind study.
Although neither trial was designed to detect differences between treatment groups with respect to incidence of vertebral fracture, combined results from the 2 studies nevertheless indicated an encouraging overall 70% reduction in this end-point (p = 0.01 vs placebo).
Paget’s Disease. In 2 noncomparative studies in which risedronate 30mg was given once daily for 84 days (with additional 112-day follow-up) in 20 and 160 patients with moderate to severe Paget’s disease, mean serum ALP levels were reduced from the first post-baseline measurement (day 29) onwards (p < 0.001 vs baseline for both studies). Patients whose serum ALP levels did not normalise received a second cycle of treatment; ALP normalisation rates were 65 and 53.8% across both cycles in these 2 studies. All patients were free from pain by day 56 of the second cycle in the smaller study; in the larger trial, 42% of 154 evaluable patients were pain-free on day 196 (p < 0.001 vs baseline).
Risedronate 30mg once daily for 2 months has been compared with etidronate 400mg daily for 6 months in 123 patients with Paget’s disease in a randomised double-blind trial with 12- and 18-month follow-up. Both drugs were associated with reductions from baseline (p < 0.01) in serum levels of ALP from 1 month onwards, but risedronate evoked greater responses than etidronate (p < 0.001 between treatments). Maximum mean changes from baseline in ALP were seen at 6 months and were 69 and 33% for risedronate and etidronate, respectively. Biochemical remission was achieved in 77 and 11% of patients by month 6 (p < 0.001). After 18 months, 53 and 14% of evaluable risedronate and etidronate recipients, respectively, had serum ALP levels within the normal range. There was no statistically significant difference between treatments in mean pain scores, and no significant improvements in other quality-of-life measures (Short Form Health Survey) were reported with either drug.
Tolerability
Adverse event reporting rates were 92.1% with risedronate 5mg daily and 92.8% with placebo in patients below 80 years of age in an analysis of tolerability results from 10 068 individuals included in an assessment of 15 066 patients enrolled in placebo-controlled clinical studies. Corresponding rates in patients aged 80 years and over were 87.9 and 88.3%. Withdrawal rates were also similar between treatment groups for both age categories.
According to collated data from over 5700 patients in phase III osteoporosis studies, overall incidences of serious adverse events were 24.9% with placebo and 26.3% with risedronate 5 mg/day; rates of withdrawal from treatment were 14.4 and 13.5%, respectively. Risedronate 10 to 30 mg/day was well tolerated by 392 patients with Paget’s disease who participated in clinical trials. Similar tolerability profiles between treatment groups were apparent in a clinical trial comparing risedronate 30 mg/day with etidronate 400 mg/day, with the most commonly reported adverse events possibly or probably related to study medication (both drugs) being arthralgia, diarrhoea, headache, abdominal pain and skin rash.
Tolerability data from the analysis of 15 066 patients randomised in clinical studies to risedronate or placebo treatment have shown no excess incidence relative to placebo of upper GI lesions in patients receiving risedronate 5 mg/day. Similarity between groups was maintained in patients with a history of upper GI disease, those receiving NSAID or aspirin treatment, and those using histamine H2-receptor antagonists or proton pump inhibitors.
Rates of gastric ulceration after endoscopic examination on days 8 and 15 in a recent 2-week study in 448 healthy postmenopausal women were 4.1% with risedronate 5 mg/day and 13.2% with alendronate 10 mg/day (p < 0.001). Another study in 235 patients has shown similar mean gastric erosion scores after 28 days’ therapy with risedronate 30 mg/day or alendronate 40 mg/day. There have been no reports of any acute-phase reactions, age-related increases in adverse event reporting or mineralisation defects in patients receiving risedronate therapy.
Dosage and Administration
Risedronate tablets should be taken once daily at least 30 minutes before the first meal or drink (other than water) of the day, and should be swallowed with a full glass of water by patients in an upright position. Patients should not lie down for at least 30 minutes after taking risedronate. Supplemental calcium and calciferol should be prescribed for those whose dietary intake is inadequate.
The recommended daily dosage of risedronate for the prevention or treatment of postmenopausal and glucocorticoid-induced osteoporosis is 5mg. Patients with Paget’s disease should receive 30mg daily for 2 months, with a second course after an additional 2-month treatment-free observation period if serum ALP levels do not normalise or disease relapse is seen.
There are no data on the use of risedronate in pregnant or nursing women. No dosage adjustment is necessary in elderly patients or in those with mild to moderate renal impairment (CLCR≥1.8 L/h). The drug is not recommended in patients with CLCR below 1.8 L/h, however.










Similar content being viewed by others
References
Watson JE, editor. Medical-surgical nursing and related physiology. 2nd ed. Eastbourne: W.B. Saunders, 1979
Golden BD. The prevention and treatment of osteoporosis. Arthritis Care Res 1998; 11(2): 124–34
Gatti D, Adami S. New bisphosphonates in the treatment of bone diseases. Drugs Aging 1999 Oct; 15: 285–96
Johansen A, Stone M, Rawlinson F. Bisphosphonates and the treatment of bone disease in the elderly. Drugs Aging 1996 Feb; 8: 113–26
Ali SY, Sajdera SW, Anderson HC. Isolation and characterization of calcifying matrix vesicles from epiphyseal cartilage. Proc Natl Acad Sci U S A 1970; 67: 1513–20
Fleisch H, Russell RG, Francis MD. Diphosphonates inhibit hydroxyapatite dissolution in vitro and bone resorption in tissue culture and in vivo. Science 1969; 165: 1261–4
Reynolds JJ, Morgan DB. A combined in vivo and in vitro study of the effects of diphosphonates on bone resorption. J Bone Joint Surg Br 1970; 52B: 796
Strates BS, Firschein HE, Urist MR. Alkaline phosphatase and failure of calcification under the influence of a diphosphonate. Biochim Biophys Acta 1971; 244: 121–4
Dunn CJ, Fitton A, Sorkin EM. Etidronic acid: a review of its pharmacological properties and therapeutic efficacy in resorptive bone disease. Drugs Aging 1994; 5(6): 446–74
Kylstra JW, Bekker PJ, Axelrod DW, et al. Risedronate in Paget’s disease: preliminary results of a multi-center study. Semin Arthritis Rheum 1994; 23(4): 272
Fleisch H. Bisphosphonates: mechanisms of action. Endocr Rev 1998; 19(1): 80–100
Licata AA. Bisphosphonate therapy. Am J Med Sci 1997 Jan; 313: 17–22
Hughes DE, Wright KR, Uy HL, et al. Bisphosphonates promote apoptosis in murine osteoclasts in vitro and in vivo. J Bone Miner Res 1995 Oct; 10: 1478–87
Luckman SP, Hughes DE, Coxon FP, et al. Nitrogen-containing bisphosphonates inhibit the mevalonate pathway and prevent post-translational prenylation of GTP-binding proteins, including RAS. J Bone Miner Res 1998; 13(4): 581–9
Harris ST, Watts NB, Genant HK, et al. Effects of risedronate treatment on vertebral and nonvertebral fractures in women with postmenopausal osteoporosis: a randomized controlled trial. JAMA 1999 Oct 13; 282: 1344–52
Fogelman I, Ribot C, Smith R, et al. Risedronate reverses bone loss in postmenopausal women with low bone mass: results from a multinational, double-blind, placebo-controlled trial. J Clin Endocrinol Metab 2000; 85(5): 1895–900
Reginster J-Y, Minne HW, Sorensen OH, et al. Randomized trial of the effects of risedronate on vertebral fractures in women with established postmenopausal osteoporosis. Osteoporosis Int 2000; 11: 83–91
Hosking DJ, Eusebio RA, Chines AA. Paget’s disease of bone: reduction of disease activity with oral risedronate. Bone 1998; 22(1): 51–5
Siris ES, Chines AA, Altaian RD, et al. Risedronate in the treatment of Paget’s disease of bone: an open label, multicenter study. J Bone Miner Res 1998 Jun; 13: 1032–8
Brown JP, Hosking DJ, Ste-Marie L-G, et al. Risedronate, a highly effective, short-term oral treatment for Paget’ s disease: a dose-response study. Calcif Tissue Int 1999; 64(2): 93–9
Miller PD, Brown JP, Siris ES, et al. A randomized, double-blind comparison of risedronate and etidronate in the treatment of Paget’s disease of bone. Am J Med 1999 May; 106: 513–20
Goa KL, Balfour JA. Risedronate. Drugs Aging 1998 Jul; 13: 83–91
Eriksen EF, Brown JP, Boling E, et al. Beneficial effects of risedronate in corticosteroid-treated patients: histology and histomorphometry [abstract]. Bone 1998; 23 (5 Suppl.): S403
Roux C, Ravaud P, Cohen-Solal M, et al. Biologic, histologic and densitometric effects of oral risedronate on bone in patients with multiple myeloma. Bone 1994 Jan-Feb; 15: 41–9
Mitchell DY, Eusebio RA, Sacco-Gibson NA, et al. Dose-proportional pharmacokinetics of risedronate on single-dose oral administration to healthy volunteers. J Clin Pharmacol 2000 Mar; 40: 258–65
Mitchell DY, Barr WH, Eusebio RA, et al. Determination of intravenous pharmacokinetics, absolute and relative bioavailability, and intra- and intersubject variability of risedronate using a four period replicate study design [abstract no. 3444]. Pharm Res 1997; 14: S–610
Mitchell DY, Heise MA, Pallone KA, et al. The effect of dosing regimen on the pharmacokinetics of risedronate. Br J Clin Pharmacol 1999 Oct; 48: 536–42
Aventis Pharmaceuticals Inc. Actonel (risedronate sodium tablets) prescribing information. Kansas City (MO: Aventis Pharmaceuticals Inc, Apr 2000
Mitchell DY, Eusebio R, Axelrod DW, et al. Risedronate pharmacokinetics following single and multiple dose intravenous administration [abstract no. P321]. Bone 1997; 20: 100S
Mitchell DY, St Peter JV, Eusebio RA, et al. Effect of renal function on risedronate pharmacokinetics after a single oral dose. Br J Clin Pharmacol 2000 Mar; 49: 215–22
Melton III LJ, Chrischilles EA, Cooper C, et al. Perspective: how many women have osteoporosis? J Bone Miner Res 1992; 7: 1005–10
Rubin CD. Southwestern Internal Medicine Conference: age-related osteoporosis. Am J Med Sci 1991; 301: 281–98
Ullrich I. Osteoporosis. West Virginia Med J 1991; 87: 347–50
Cummings S, Black D, Nevitt M, et al. Bone density at various sites for prediction of hip fractures. Lancet 1993; 341: 72–5
Lindsay R, Silverman SL, Cooper C, et al. Risk of new vertebral fracture in the year following a fracture. JAMA 2001; 285(3): 320–3
Adami S, Kanis JA. Assessment of involutional bone loss: methodological and conceptual problems. J Bone Miner Res 1995; 10: 511–7
National Osteoporosis Foundation. Physician’s guide to prevention and treatment of osteoporosis [online]. NOF; 2000. Available from: URL: http://www.nof.org/physguide [accessed 2001 Mar 30]
Consensus Statements (NIH Consensus Development Program): 111. Osteoporosis prevention, diagnosis, and therapy. National Institutes of Health Consensus Development Conference Statement. March 27–29, 2000. Available from URL: http://odp.od.nih.gOv/consensus/cons/111/111_statement.htm#4 [Accessed 2000 Sep 16]
Lindsay R. Estrogen deficiency. In: Riggs BL, Melton LJ, editors. Osteoporosis: etiology, diagnosis, and management. 2nd ed. Philadelphia (PA): Lippincott-Raven, 1995: 133–60
Kanis JA, Melton III LJ, Christiansen C, et al. Perspective: the diagnosis of osteoporosis. J Bone Miner Res 1994;9: 1137–41
Watts NB, Harris ST, Genant HK, et al. Intermittent cyclical etidronate treatment of postmenopausal osteoporosis. N Engl J Med 1990; 323: 73–9
Storm T, Thamsborg G, Steiniche T, et al. Effect of intermittent cyclical etidronate therapy on bone mass and fracture rate in women with postmenopausal osteoporosis. N Engl J Med 1990; 322: 1265–71
McClung MR, Bensen W, Bolognese MA, et al. Risedronate increases BMD at the hip, spine and radius in postmenopausal women with low bone mass [abstract no. P269]. J Bone Miner Res 1997 Aug; 12 Suppl. 1: S169
Ebeling P, Roberts A, D’Emden M, et al. Risedronate prevents bone loss in early postmenopausal women [abstract no. SA377]. J Bone Miner Res 1999; 14 Suppl. 1: S403
McClung MR, Geusens P, Miller PD, et al. Effect of risedronate on the risk of hip fracture in elderly women. N Engl J Med 2001; 344(5): 333–40
Hooper M, Hanley DA, Eastell R, et al. Sustained effect of risedronate in the prevention of the first vertebral fracture in women [abstract]. J Bone Miner Res 2000 Sep; 15 Suppl. 1: S428
Brown J-P, Hosking D, Josse R, et al. Risedronate rapidly and consistently reduces risk of further vertebral fracture in women with multiple vertebral fractures [abstract]. J Bone Miner Res 2000 Sep; 15 Suppl. 1: 150
Harris ST, Wasnich R, Ettinger M, et al. The effects of risedronate plus estrogen compared with estrogen alone in postmenopausal women [abstract]. J Bone Miner Res 1999 Sep; 14 Suppl.: 29
Adinoff AD, Hollister JR. Steroid-induced fractures and bone loss in patients with asthma. N Engl J Med 1983; 309: 265–8
Hamdy RC. Iatrogenic osteoporosis. South Med J 1999 Nov; 92: 1131–3
van Staa TP, Leufkens HG, Abenhaim L, et al. Use of oral corticosteroids and risk of fractures. J Bone Miner Res 2000; 15(6): 993–1000
Cushing H. The basophil adenomas of the pituitary body and their clinical manifestations (pituitary basophilism). Bull Johns Hopkins Hosp 1932; 50: 137–95
Curtiss Jr PH, Clark WS, Herndon CH, et al. Vertebral fractures resulting from prolonged cortisone and corticotrophin therapy. JAMA 1954; 156: 467–9
Laan RFJM, van Riel PLCM, van de Putte LBA, et al. Low-dose prednisone induces rapid reversible axial bone loss in patients with rheumatoid arthritis: a randomized controlled study. Ann Intern Med 1993; 119. 963–968
Lukert BP, Raisz LG. Glucorticoid-induced osteoporosis: pathogenesis and management. Ann Intern Med 1990; 112: 352–64
Montemurro L, Fraioli P, Riboldi A, et al. Bone loss in prednisone treated sarcoidosis: a two-year follow-up. Ann Ital Med Interna 1990; 5: 164–8
Nordborg E, Hansson T, Jonson R, et al. Bone mineral content of the third lumbar vertebra during 18 months of prednisolone treatment for giant cell arteritis. Clin Rheumatol 1993; 12: 455–60
Als OS, Gotfredsen A, Christiansen C. The effect of glucocorticoids on bone mass in rheumatoid arthritis patients: influence of menopausal state. Arthritis Rheum 1985; 28: 369–75
Pons F, Peris P, Guanabens N, et al. The effect of systemic lupus erythematosus and long-term steroid therapy on bone mass in premenopausal women. Br J Rheumatol 1995; 34: 742–6
Eggelmeijer F. Prevention and treatment of glucocorticoid-induced osteoporosis. Pharm World Sci 1998; 20(5): 193–7
Homik JE, Cranney A, Shea B, et al. A metaanalysis on the use of bisphosphonates in corticosteroid induced osteoporosis. J Rheumatol 1999; 26(5): 1148–57
Cohen S, Levy RM, Keller M, et al. Risedronate therapy prevents corticosteroid-induced bone loss: a twelve-month, multicenter, randomized, double-blind, placebo-controlled, parallel-group study. Arthritis Rheum 1999 Nov; 42: 2309–18
Reid DM, Hughes RA, Laan RFJM, et al. Efficacy and safety of daily risedronate in the treatment of corticosteroid-induced osteoporosis in men and women: a randomized trial. J Bone Miner Res 2000; 15(6): 1006–13
Wallach S, Cohen S, Reid DM, et al. Effects of risedronate treatment on bone density and vertebral fracture in patients on corticosteroid therapy. Calcif Tissue Int 2000; 67: 277–85
Maricic M, Weryha G, Emkey R, et al. Risedronate increases bone mass in men receiving glucocorticoid therapy [abstract]. Arthritis Rheum 2000 Sep; 43 (9 Suppl.): S203
Frame B, Marel GM. Paget disease: a review of current knowledge. Radiology 1981; 141: 21–4
Wallach S. Treatment of Paget’s disease. In: Advances in internal medicine. v. 27. Chicago (IL): Year Book Medical Publishers, 1982: 1–43
Merkow RL, Lane JM. Paget’s disease, part II. In: Sculco TP, editor. Orthopedic care of the geriatric patient. St Louis (MO): CV Mosby, 1985: 253–68
Case records of the Massachusetts General Hospital. Weekly clinicopathological exercises. Normal reference laboratory values. N Engl J Med 1992; 327(10): 718–24
Young DS. Implementation of SI units for clinical laboratory data. Style specifications and conversion tables. Ann Intern Med 1987; 106(1): 114–29
Deal C, Piette F, Olszynski W, et al. Risedronate is well-tolerated in osteoporotic patients, including those over 80 years of age. Arthritis Rheum 2000 Sep; 43 Suppl.: S203
Eastell R, Watts N, McClung M, et al. Integrated safety analyses of risedronate in postmenopausal women [abstract]. 81st Annual Meeting, Endocrine Society 1999 Jun 12: 443
Brown JP, Singer FR, Siris FS, et al. A safety review of the use of risedronate in the treatment of Paget’ s disease of bone [abstract]. J Rheumatol 1998 Jun; 25 Suppl. 52: 53
Singer FR, Minoofar PN. Bisphosphonates in the treatment of disorders of mineral metabolism. Adv Endocrinol Metab 1995; 6: 259–88
Zysset E, Ammann P, Jenzer A, et al. Comparison of a rapid (2-h) versus a slow (24-h) infusion of alendronate in the treatment of hypercalcemia of malignancy. Bone Miner 1992 Sep; 18(3): 237–49
Adami S, Bhalla AK, Dorizzi R, et al. The acute-phase response after bisphosphonate administration. Calcif Tissue Int 1987 Dec; 41(6): 326–31
Ward C, Sacco-Gibson N, Mitchell DY, et al. Single dose risedronate (pyridinyl-bisphosphonate) does not induce acute phase reaction in healthy subjects [abstract no. M660]. J Bone Miner Res 1996; 11 Suppl. 1: S346
Sacco-Gibson N, Mitchell DY, Eusebio RA, et al. Risedronate (a pyridinyl bisphosphonate) does not induce acute phase reaction after single and multiple dose intravenous administration [abstract no. P329]. Bone 1997; 20: 102S
Fogelman I, Moreland L, Woodson G, et al. Gastrointestinal side effects and endoscopic findings similar between risedronate and placebo-treated patients. Osteoporosis Int 2000; 11 Suppl. 2: S179
Hosking D, Bockman R, Glowinski J, et al. Similar gastrointestinal side effects and endoscopic findings between risedronate and placebo-treated patients. J Bone Miner Res 2000 Sep; 15 Suppl. 1: S428
Lanza FL, Hunt RH, Thomson ABR, et al. Endoscopic comparison of esophageal and gastroduodenal effects of risedronate and alendronate in postmenopausal women. Gastroenterology 2000; 119: 631–8
Adachi JD, Adami S, Miller PD, et al. Risedronate is well-tolerated in alendronate-intolerant postmenopausal women [abstract]. J Bone Miner Res 2000 Sep; 15 Suppl. 1: S429
Lanza F, Schwartz H, Sahba B, et al. An endoscopic comparison of the effects of alendronate and risedronate on upper gastrointestinal mucosae. Am J Gastroenterol 2000; 95: 3112–7
Aventis Pharma Pty Ltd. Product information: Actonel® (risedronate disodium). Lane Cove, NSW: Aventis Pharma Pty Ltd, Aug 2000
Procter and Gamble Pharmaceuticals. Actonel®: risedronate sodium tablets 5 and 30 mg (as the hemi-pentahydrate). Toronto, Ontario, Canada, Jul 2000
Hoechst Marion Roussel SA. Package insert leaflet: Actonel® 30 mg. Maroussi, Greece, Dec 2000
Aventis Pharmaceuticals. Actonel 30 mg film-coated tablets. Costa Rica, Oct 1999
Cranney A, Welch V, Tugwell P, et al. Responsiveness of end-points in osteoporosis clinical trials — an update. J Rheumatol 1999; 26(1): 222–8
Chrischilles EA, Butler CD, Davis CS, et al. A model of lifetime osteoporosis impact. Arch Intern Med 1991; 151: 2026–32
Adis meeting report: osteoporosis becoming a disease of the past? Drugs RD 1999 Mar; 1: 231–2
Eastell R. Treatment of postmenopausal osteoporosis. N Engl J Med 1998; 338(11): 736–46
Francis RM. Management of established osteoporosis. Br J Clin Pharmacol 1998; 45(2): 95–9
Barman Balfour JA, Goa KL. Intranasal salcatonin (salmon calcitonin): an updated review of its pharmacological properties and therapeutic use in the management of postmenopausal osteoporosis. Drugs Aging (In press)
Eastell R, Reid DM, Compston J, et al. A UK Consensus Group on management of glucocorticoid-induced osteoporosis: an update. J Intern Med 1998 Oct; 244: 271–92
Torgerson DJ, Reid DM. The economics of osteoporosis and its prevention: a review. Pharmacoeconomics 1997 Feb; 11: 126–38
Roux C, Dougados M. Treatment of patients with Paget’s disease of bone. Drugs 1999 Nov; 58: 823–30
Author information
Authors and Affiliations
Corresponding author
Additional information
Various sections of the manuscript reviewed by: M.A. Ankrom, Johns Hopkins Geriatrics Center, Baltimore, Maryland, USA; S.B. Cohen, Rheumatology Associates, Dallas, Texas, USA; ; F. Eggelmeijer, Department of Rheumatology, Ziekenhuiscentrum Apeldoorn, Apeldoorn, The Netherlands; A.A. Licata, The Cleveland Clinic Foundation, Cleveland, Ohio, USA; L. Mortensen, Department of Endocrinology and Metabolism, Aarhus Amtssygehus, Aarhus, Denmark; C. Roux, Centre d’Évaluation des Maladies Osseuses, Paris, France.
Data Selection
Sources: Medical literature published in any language since 1983 on risedronate, identified using AdisBase (a proprietary database of Adis International, Auckland, New Zealand), Medline and EMBASE. Additional references were identified from the reference lists of published articles. Bibliographical information, including contributory unpublished data, was also requested from the company developing the drug.
Search strategy: AdisBase search terms were ‘risedronate’ or ‘NE-58095’. Medline search terms were ‘risedronate’ or ‘NE-58095’. EMBASE search terms were ‘risedronate’ or ‘NE 58095’. Searches were last updated 4 Apr 2001.
Selection: Studies in patients with postmenopausal or glucocorticoid-induced osteoporosis or Paget’s disease who received risedronate. Inclusion of studies was based mainly on the methods section of the trials. When available, large, well controlled trials with appropriate statistical methodology were preferred. Relevant pharmacodynamic and pharmacokinetic data are also included.
Index terms: Risedronate, bisphosphonates, resorptive bone disease, osteoporosis, postmenopausal, glucocorticoid-induced, Paget’s disease, pharmacodynamics, pharmacokinetics, therapeutic use, tolerability, dosage and administration, review.
Rights and permissions
About this article
Cite this article
Dunn, C.J., Goa, K.L. Risedronate. Drugs 61, 685–712 (2001). https://doi.org/10.2165/00003495-200161050-00013
Published:
Issue Date:
DOI: https://doi.org/10.2165/00003495-200161050-00013