Abstract
Background and objective: Subcutaneous treprostinil is an effective treatment for pulmonary arterial hypertension (PAH). A previous pivotal study indicated that infusion site pain was dose dependent and resulted in suboptimal dose escalation by week 12 and a reduced clinical benefit. We hypothesized that a rapid-escalation treprostinil dosing regimen would be as safe and effective as a slow-escalation dosing regimen.
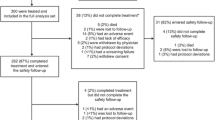
Methods: Twenty-three patients received treprostinil to treat PH of various aetiologies and were randomized into two groups. Group 1 (11 patients: seven females and four males, aged 51.7 ± 15.4 years) received a slowescalation regimen, and group 2 (12 patients: ten females and two males, aged 51.3 ± 16.7 years) were exposed to rapid dose escalation. The dose escalation, exercise capacity (a 6-minute walk test [6WT] or a shuttle walk test [SWT]), WHO classification, blood pressure, heart rate, respiration rate, baseline haemodynamics and adverse events were followed up for 12 weeks.
Results: Baseline haemodynamics did not differ significantly between the treatment groups. At follow-up, the treprostinil dose reached 12.9 ± 2.7 ng/kg/min in group 1 and 20.3 ± 5.8 ng/kg/min in group 2 (p < 0.01). The patients’ WHO classification improved significantly (p < 0.05), with no difference between the groups. Improvement of exercise capacity was greater in group 2 (6WT and SWT, p < 0.05). Infusion site pain occurred in 81.8% of group 1 and in 58.3% of group 2 (p < 0.05) patients. Other adverse events and changes in the heart rate, respiration rate and blood pressure were similar in both groups.
Conclusion: The rapid-dosing regimen is as safe and effective as the slow-escalation regimen and may be associated with even better clinical outcomes. Infusion site pain is not dose dependent.








Similar content being viewed by others
Notes
The use of trade names is for product identification purposes only and does not imply endorsement.
References
Moncada S, Gryglewski R, Bunting S, et al. An enzyme isolated from arteries transforms Prostaglandin endoperoxides to an unstable substance that inhibits platelet aggregation. Nature 1976; 263: 663–5
Tuder RM, Cool CD, Geraci MW, et al. Prostacyclin synthase expression is decreased in lungs from patients with severe pulmonary hypertension. Am J Respir Crit Care Med 1999; 159(6): 1925–32
Badesch DB, McLaughlin VV, et al. Prostanoid therapy for pulmonary arterial hypertension. J Am Coll Cardiol 2004; 43: 56S–61S
Barst RJ, Rubin LJ, Long WA, et al. A comparison of continuous intravenous epoprostenol (prostacyclin) with conventional therapy for primary pulmonary hypertension. The Primary Pulmonary Hypertension Study Group. N Engl J Med 1996; 334: 296–302
McNulty MJ, Sailstad JM, Steffen RP. The pharmacokinetics and pharmacodynamics of the prostacyclin analog 15au81 in the anesthetized beagle dog. Prostaglandins Leukot Essent Fatty Acids 1993; 48: 159–66
Voswinckel R, Enke B, Reichenberger F, et al. Favorable effects of inhaled treprostinil in severe pulmonary hypertension: results from randomized controlled pilot studies. J Am Coll Cardiol 2006; 48: 1672–81
Simonneau G, Barst RJ, Galie N, et al. Continuous subcutaneous infusion of treprostinil, a prostacyclin analogue, in patients with pulmonary arterial hypertension: a double-blind, randomized, placebo-controlled trial. Am J Respir Crit Care Med 2002; 165: 800–4
Lang I, Gomez-Sanchez M, Kneussl M, et al. Efficacy of long-term subcutaneous treprostinil sodium therapy in pulmonary hypertension. Chest 2006; 129: 1636–43
Barst RJ, Galie N, Naeije R, et al. Long-term outcome in pulmonary arterial hypertension patients treated with subcutaneous treprostinil. Eur Respir J 2006; 28: 1195–203
Skoro-Sajer N, Bonderman D, Wiesbauer F, et al. Treprostinil for severe inoperable chronic thromboembolic pulmonary hypertension. J Thromb Haemost 2007; 5: 483–9
Vachiery JL, Hill N, Zwicke D, et al. Transitioning from IV epoprostenol to subcutaneous treprostinil in pulmonary arterial hypertension. Chest 2002; 121: 1561–5
Rubenfire M, McLaughlin VV, Allen RP, et al. Transition from IV epoprostenol to subcutaneous treprostinil in pulmonary arterial hypertension: a controlled trial. Chest 2007; 132: 757–63
McGoon M, Gutterman D, Steen V, et al. Screening, early detection, and diagnosis of pulmonary arterial hypertension: ACCP evidence-based clinical practice guidelines. Chest 2004; 126: 14S–34S
McLaughlin VV, Presberg KW, Doyle RL, et al. Prognosis of pulmonary arterial hypertension: ACCP evidence-based clinical practice guidelines. Chest 2004; 126: 78S–92S
Galie N, Torbicki A, Barst R, et al. Guidelines on diagnosis and treatment of pulmonary arterial hypertension. The Task Force on Diagnosis and Treatment of Pulmonary Arterial Hypertension of the European Society of Cardiology. Eur Heart J 2004; 25: 2243–78
Acknowledgements
This study/research project received financial support from the European Commission under the 6th Framework Programme (Contract no.: LSHM-CT-2005-018725, PULMOTENSION). This publication reflects only the authors’ views, and the European Community is in no way liable for any use that may be made of the information contained therein.
Wendy Gin Sing has received honoraria for lecturing from United Therapeutics, Actelion Pharmaceuticals and Encysive Pharmaceuticals, and travel grants for educational meetings from United Therapeutics, Actelion Pharmaceuticals, Encysive Pharmaceuticals, Schering Healthcare, GlaxoSmithKline (GSK) and Pfizer. Simon Gibbs has received honoraria from Actelion Pharmaceuticals, GSK, Encysive Pharmaceuticals, Pfizer and Schering. The Hammersmith Pulmonary Hypertension Service has received funding from United Therapeutics, Actelion Pharmaceuticals and Encysive Pharmaceuticals. The other authors have no conflicts of interest that are directly relevant to the content of this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Skoro-Sajer, N., Lang, I.M., Harja, E. et al. A Clinical Comparison of Slow- and Rapid-Escalation Treprostinil Dosing Regimens in Patients with Pulmonary Hypertension. Clin Pharmacokinet 47, 611–618 (2008). https://doi.org/10.2165/00003088-200847090-00004
Published:
Issue Date:
DOI: https://doi.org/10.2165/00003088-200847090-00004