Abstract
Allergic disease is an increasing problem worldwide. Allergic rhinitis, an inflammatory response to an allergen, affects an estimated 20–40 million people in the US, while chronic idiopathic urticaria is a dermatoallergic condition that affects 0.1–3% of people in the US and Europe. The primary goals of treatment for allergic rhinitis are to reduce symptoms, which include sneezing, rhinorrhoea and nasal congestion, improve quality of life and prevent the sequelae associated with this disease, while the goal for chronic idiopathic urticaria is the rapid and prolonged control of symptoms. Quantitatively, histamine is the most abundant mediator present during an allergic episode — thus, antihistamines (historically called histamine H1 receptor antagonists, now called H1 receptor inverse agonists) are a first-line defense against allergic rhinitis and chronic idiopathic urticaria. Although first-generation antihistamines can cause sedation and cognitive impairment, second-generation antihistamines are relatively nonsedating and free of such adverse events owing to their comparative inability to penetrate the blood-brain barrier. Desloratadine is one such second-generation antihistamine and is indicated for the treatment of allergic diseases, including allergic rhinitis and chronic idiopathic urticaria. It has proven efficacy against the symptoms associated with seasonal and perennial allergic rhinitis, including nasal congestion, and chronic idiopathic urticaria. As a result, it has been shown to improve patients’ quality of life. The safety and efficacy profiles of desloratadine are well established, and published postmarketing analyses have assessed >54 000 patients. Although earlier second-generation antihistamines have been associated with cardiovascular adverse effects, desloratadine has been shown to be safe and well tolerated at nine times the recommended dose. In addition, it has been shown to not interact with concomitantly administered drugs and food. Overall, current data indicate that desloratadine is a safe and effective treatment for allergic diseases.
Similar content being viewed by others
The aim of this review was to provide a comprehensive review of the available data on the safety and efficacy of desloratadine in the treatment of allergic disease, including allergic rhinitis (both seasonal and perennial) and chronic idiopathic urticaria. The literature was initially searched for key references discussing the preclinical characterisation of desloratadine and establishing the safety and efficacy of this agent in allergen-challenge studies, clinical trials and postmarketing surveillance studies. The literature search was then broadened; the PubMed online citation database was searched from 1 January 1993 to 4 April 2005, using the keywords ‘desloratadine’, ‘loratadine’ and ‘descarboethoxyloratadine’ to identify all papers discussing desloratadine, and using combinations of the terms ‘allergic rhinitis’, ‘seasonal allergic rhinitis’, ‘perennial allergic rhinitis’, ‘chronic idiopathic urticaria’, ‘H1-antihistamine’, ‘inhaled corticosteroids’, ‘leukotriene receptor antagonist’, ‘anti-IgE antibody therapy’, ‘allergen immunotherapy’ and the generic names of other antihistamines and corticosteroids to identify key references containing information on the prevalence, epidemiology, economic burden, immunopathology and treatments for allergic rhinitis and chronic idiopathic urticaria. Desloratadine references were selected on the basis of their inclusion of data and information on the development, safety and efficacy of the agent in allergic rhinitis and chronic idiopathic urticaria. Other references were included or excluded in order to provide a representative, up-to-date overview of currently available data on the diseases and alternative agents.
1. Allergic Disease
1.1 Epidemiology
Allergic rhinitis is a major respiratory disorder affecting 10–25% of the world’s population, a prevalence that is increasing.[1] In addition to bothersome symptoms, allergic rhinitis results in decreases in work productivity, cognitive performance and quality of life.[2–4] Allergic rhinitis affects an estimated 20–40 million people in the US[2] (approximately 20% of adults and >40% of children), with the incidence of allergic disease in the paediatric population increasing at an alarming rate.[5] The estimated prevalence of allergic rhinitis in adults in Europe is approximately 23%.[6] Allergic rhinitis is classified as either seasonal or perennial, depending on the pattern of symptom occurrence.[7] Symptoms of seasonal allergic rhinitis occur during the spring and autumn in response to exposure to outdoor allergens, such as pollens and moulds. In contrast, perennial allergic rhinitis is a persistent disorder that occurs throughout the year. Perennial allergens include dust mites and animal dander. Symptoms of seasonal and perennial allergic rhinitis can be nasal or non-nasal but usually include nasal itching, sneezing, rhinorrhoea and nasal congestion.[8]
Another allergic disorder is chronic urticaria, which is known as chronic idiopathic urticaria when there are no known causal agents. Chronic idiopathic urticaria is a dermatoallergic condition that affects 0.1–3% of people in the US and Europe, and that accounts for almost 75% of cases of chronic urticaria.[9–12] Symptoms include hives or wheals and pruritis, and the disease can have a severely negative effect on quality of life. Owing to this, it is frequently a disabling disease.[9,11,13–15]
1.2 Morbidity
Chronic nasal congestion and stuffiness are perhaps the most troubling symptoms of allergic rhinitis.[7] Night-time nasal congestion can cause sleep impairment,[16] which can contribute to daytime irritability and fatigue, lack of concentration, decreased productivity and an overall reduction in quality of life.[17] One controlled trial investigated the impact of unmedicated allergic rhinitis on vigilance (i.e. sustained attention over time) and cognitive function in patients with ragweed-induced allergic rhinitis.[18] A comprehensive series of cognitive performance tests was administered at baseline and after allergen priming. Compared with asymptomatic patients, those with symptomatic allergic rhinitis demonstrated divided attention, longer response times and decreased efficiency in working memory, psychomotor speed, and reasoning and computation.
Allergic rhinitis is associated with long-term complications, such as chronic sinusitis, otitis media and asthma.[17] Epidemiological studies have revealed that up to 38% of patients with allergic rhinitis have a diagnosis of asthma and that up to 78% of patients with asthma have a diagnosis of rhinitis.[7] Epidemiological data suggest that these two diseases have many common characteristics[17] and a number of studies have suggested that they may be manifestations of a common underlying pathology, but many questions remain to be answered.[19]
For patients with chronic idiopathic urticaria, pruritis is often the most distressing symptom;[13] this is associated with the late-phase allergic response. The itchy, erythematous wheals seen in patients are a result of the early-phase allergic response and are chiefly the effects of histamine.[13] The disease can cause sleep disruption, fatigue, social isolation, energy loss and emotional or sexual disturbances.[11,12]
1.3 Economic Burden
Although allergic rhinitis typically is not a severe disease, it accounts for a substantial number of doctor visits.[20] Subsequently, the economic burden associated with allergic rhinitis is high; more than $4.5 billion of the total direct costs for allergic rhinitis spent annually in the US[20] is accounted for by easily identifiable expenditures, such as physician office visits, laboratory tests and treatment.[21] This figure does not include treatment costs for associated medical conditions (e.g. antibacterial treatment for chronic sinusitis, costs associated with worsening asthma) or the tremendous impact of reduced productivity and days lost from work or school (an estimated 3.8 million days are lost each year in the US).[22] The rising prevalence of allergic rhinitis will only increase its economic burden.
1.4 Immunopathology
Allergic rhinitis is well established as an IgE-mediated systemic inflammatory response to a particular allergen.[23,24] The complexity of this immune response is evident in the numerous cell types, cytokines and inflammatory mediators involved in the process. The allergic cascade is a series of immunological events comprising: (i) the early-phase response of IgE-induced mast cell degranulation; (ii) the subsequent release of preformed mediators; and (iii) the rapid synthesis of leukotrienes and prostaglandins. During the late-phase response, the release of cytokines from mast cells (e.g. interleukin [IL]-4, IL-13) advances the inflammatory process by activating eosinophils and basophils. Cytokines and chemokines (e.g. regulated on activation normal T cell expressed and secreted [RANTES], eotaxin) cause eosinophils and basophils to migrate to allergically activated tissue. Upregulation of adhesion molecules (P-selectin, intercellular adhesion molecule-1 [ICAM-1]) facilitates the migration of these cells into the mucosa, where they continue to release inflammatory agents and mediators. Because each phase of the allergic cascade is unique, the symptoms associated with each phase may vary (figure 1).
The allergic inflammatory response: specific immune mediators involved in early- and late-phase reactions, and their association with symptoms. GM-CSF = granulocyte-macrophage colony-stimulating factor; ICAM = intercellular adhesion molecule; IL = interleukin; LTC 4 = leukotriene C4; PGD 2 = prostaglandin D2; RANTES = regulated on activation normal T cell expressed and secreted; TNF = tumor necrosis factor; VCAM = vascular cell adhesion molecule.
The pathophysiology of chronic idiopathic urticaria remains unclear in a large proportion of patients. It has been identified that the condition has an autoimmune basis in 30–50% of patients, with these patients possessing autoantibodies against the Fee receptor 1 or IgE that result in histamine release.[25,26] However, in the remaining 50% of patients the condition is truly idiopathic. Nevertheless, histamine is one of the major mediators in all forms of urticaria.
1.5 Treatment
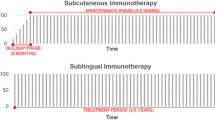
The primary goals of treatment for allergic rhinitis are to reduce the symptoms associated with the condition, improve quality of life, and prevent associated complications. Appropriate skin testing and/or IgE testing is performed to identify specific allergens responsible for the onset of symptoms. Following the identification of the causative allergen, treatment strategies include allergen avoidance, immunotherapy and pharmacotherapy. Strategies are used in a stepwise fashion; symptom severity and the timing of presentation often guide treatment choices. Allergen avoidance is a first-line treatment strategy, the success of which depends on the specific allergen involved and the practical measures used to avoid allergen contact.[8] Unfortunately, it may take considerable time before significant benefit is noted and certain avoidance strategies may not be practical for some patients. Pharmacotherapy is usually the next approach taken to reduce disease severity; however, immunotherapy should be considered early in the disease because it can significantly alleviate symptoms and lessen the need for drug treatment.[27]
The aim of chronic idiopathic urticaria treatment is to bring symptoms under control rapidly and for a prolonged period, thus enabling the patient to resume social activities.[11,12] Treatment is generally targeted to individual symptoms until a diagnosis of chronic idiopathic urticaria has been established, whereupon antihistamines are the primary therapy.[11,12,28–30]
1.5.1 Antihistamines (Histamine H1 Receptor Inverse Agonists)
Oral antihistamines, historically called histamine H1 receptor antagonists, now known as H1 receptor inverse agonists, are first-line pharmacotherapeutic agents in the treatment of allergic diseases including allergic rhinitis and chronic idiopathic urticaria. Antihistamines are commonly categorised as sedating or nonsedating.[8,31] Certain over-the-counter and first-generation antihistamines (e.g. chlorphenamine [chlorpheniramine], diphenhydramine) can relieve the symptoms of allergic disease, but they may cause sedation, cognitive impairment and anticholinergic adverse effects.[32] Second-generation antihistamines (e.g. loratadine, desloratadine, cetirizine, levocetirizine, fexofenadine, azelastine) are preferred because of their greater tolerability compared with the sedating antihistamines. In general, these agents are nonsedating except for cetirizine, which can cause mild sedation,[33] with the incidence of somnolence having been shown in some clinical studies to be dose dependent.[34] Azelastine has also been shown to be sedating when taken systemically;[35] however, it is also available in an intranasal formulation that is only mildly sedating.[36] The second-generation antihistamines show less potential for sedation than the first-generation antihistamines owing to their comparative inability to penetrate the blood-brain barrier and occupy H1 receptors in the CNS; occupation of such receptors ranges from none for fexofenadine to 30% for cetirizine.[37] These agents are clinically effective for the treatment of the symptoms of allergic disease and are most effective when administered consistently.
The clinical efficacy of the older antihistamines is often overshadowed by their adverse event profile, including sedation and decrements in cognitive function. In one retrospective analysis, nearly 6000 employees demonstrated changes in work productivity that were associated with antihistamines that cause sedation.[38] Within the first 3 days of taking a prescribed sedating antihistamine, employee production decreased 8%, whereas it increased 5% after the employees began taking a prescribed nonsedating antihistamine. Older antihistamines are also associated with anticholinergic adverse effects, such as dry mouth, dry eyes, constipation and urinary retention.[31] These effects may be especially problematic for elderly patients, patients with prostatic hypertrophy or bladder outlet obstruction and patients with increased intraocular pressure.[31]
The pharmacological properties of early nonsedating antihistamines (terfenadine, astemizole) were associated with adverse cardiovascular effects, including tachycardia and corrected QT (QTc) interval prolongation leading to torsades de pointes, which is a potentially fatal arrhythmia.[31] Patients with hepatic dysfunction and those taking drugs that inhibit the metabolism of the antihistamines (e.g. macrolide antibacterials or antifungals) appeared to be at the greatest risk for this complication.[39] Terfenadine and astemizole were subsequently withdrawn from the US market.[40] Second-generation antihistamines, including loratadine, cetirizine and fexofenadine, are not associated with significant QTc interval prolongation.[41]
Clinical trials of nonsedating antihistamines have demonstrated that these agents rapidly reduce the symptoms of seasonal and perennial allergic rhinitis, including rhinorrhoea, sneezing and nasal pruritus.[34,36,37,42–57] Antihistamines work through inverse agonism of the H1 receptor, via ligand-dependent stabilisation of the inactive form of the receptor.[37] This results in decreased capillary permeability, reduced mucus production, relaxation of the smooth muscle and reduced vasodilation, thus lessening allergy-related symptoms.[58]
As a class, the newer antihistamines have demonstrated efficacy in reducing nasal congestion, which is considered the most bothersome symptom of allergic rhinitis. Desloratadine and fexofenadine have demonstrated significant improvements in peak nasal inspiratory flow (PNIF) and nasal congestion when compared with placebo in a double-blind, crossover study (p < 0.05),[59] and a study of levocetirizine in patients with seasonal allergic rhinitis showed that it improved nasal obstruction.[60] In addition, desloratadine, fexofenadine and levocetirizine have been shown to be equally effective in attenuating the response to nasal adenosine monophosphate challenge in patients with perennial allergic rhinitis, in terms of the maximum value and the area under the concentration-time curve (AUC) for the percentage fall in PNIF.[46] Studies of desloratadine in the Vienna Challenge Chamber (an environmental exposure unit) have shown this antihistamine to be significantly more effective than placebo in reducing the symptom of nasal congestion induced by grass pollen exposure in patients with seasonal allergic rhinitis.[61,62] Meanwhile, a single-dose study comparing cetirizine 10mg and fexofenadine 120mg conducted in the Vienna Challenge Chamber demonstrated that both agents were significantly more effective than placebo at reducing the symptom of nasal congestion in patients with seasonal allergic rhinitis, although neither agent significantly improved nasal air flow as measured by active anterior rhinomanometry.[52] Other studies of fexofenadine have also shown clinical efficacy in reducing nasal congestion in patients with perennial allergic rhinitis.[63] However, a single-dose study conducted in an environmental exposure unit showed that fexofenadine 60–120mg significantly reduced sneezing, itchy nose, palate or throat and itchy, watery, red eyes compared with placebo, but had no significant effect on rhinorrhoea or nasal congestion.[51]
Drug-drug and drug-food interactions may complicate the use of some of the newer antihistamines. These interactions are commonly mediated by the well known cytochrome P450 (CYP) enzyme system and the less well understood active drug transporters, organic anion transport polypeptide (OATP) and P-glycoprotein. The actions of these drug transport systems have been well characterised for cancer and immunosuppressive therapies, but investigation into their role in the disposition of antihistamines is just beginning. Many drugs that are metabolised by CYP3A4 are also affected by P-glycoprotein. P-glycoprotein is an adenosine triphosphate-dependent transporter that can facilitate the removal of drugs from a cell against a concentration gradient.[64] P-glycoprotein is present in many tissues, including immune cells, biliary canaliculi, kidney, adrenal glands and the intestinal wall, where it can limit the absorption of certain drugs. OATP mediates the absorption of specific drugs into the intestinal lumen.[64]
Fexofenadine is associated with several drug-drug interactions mediated by the CYP system and the drug transporters P-glycoprotein and OATP.[31,65] Several studies have shown that drug-drug and drug-food interactions reduce the bioavailability of fexofenadine at pharmacologically relevant doses. Aluminum- and magnesium-containing antacids administered within 15 minutes of fexofenadine 120mg decreased the maximum concentration (Cmax) and the AUC of fexofenadine by approximately 40%.[66] A high-salt diet has been shown to reduce the bioavailability of fexofenadine 180mg by approximately 30% compared with a low-salt diet.[67] Full-strength grapefruit, orange and apple juices reduced the bioavailability of fexofenadine 120mg to approximately 70%.[68]
Antihistamines are also first-line therapy for chronic idiopathic urticaria, with the newer, nonsedating antihistamines such as desloratadine, fexofenadine, levocetirizine and mizolastine being the first-choice treatment.[14] Clinical studies have shown these agents to be highly effective for reducing and inhibiting wheal, flare and itch, controlling pruritis and consequently improving quality of life in patients with chronic idiopathic urticaria.[11–13,28,29,69–72] The older, sedating antihistamines may be useful in patients with sleep disturbances caused by chronic idiopathic urticaria symptoms.[14]
1.5.2 Topical Corticosteroids
Topical corticosteroids can be used to manage symptoms in patients with allergic rhinitis and are the recommended first-line treatment for moderate to severe allergic rhinitis.[8,45] These drugs have potent anti-inflammatory properties, including the inhibition of cytokine and chemokine production and of cellular infiltration within the nasal mucosa.[73] These properties are believed to contribute to the efficacy of corticosteroids in reducing nasal congestion, rhinorrhoea, itching and sneezing. Indeed, corticosteroids are generally acknowledged to be more effective than antihistamines,[73,74] particularly for the reduction of nasal blockage.[75,76] They are most effective when started a number of days prior to allergen exposure. In addition, they may need to be used more regularly than on an as-needed basis for their maximum effectiveness to be realised.[77] However, a study comparing fluticasone propionate and loratadine for as-needed treatment in patients with seasonal allergic rhinitis found that the corticosteroid was more effective.[78] Because corticosteroids treat not only the early-phase reactions but also the late-phase reactions, maximum symptom relief after intranasal corticosteroid therapy is commonly reported several days after the initial dose. If the nose is extremely congested, the delivered drug may not easily reach the mucosa and it may be advisable to use a topical decongestant.[8]
1.5.3 Other Pharmacological Therapies
Sodium cromoglicate (cromolyn sodium) is a mast cell stabiliser that prevents the release of inflammatory mediators involved in the allergic response. It is less effective than antihistamines or topical corticosteroids, and patient compliance can be a problem because of the need for multiple daily doses.[8] Sodium cromoglicate is most effective when it is started several weeks before allergen exposure and then used regularly.
Studies with leukotriene receptor antagonists have also suggested the use of this class of drugs as treatments for allergic disease.[79] Leukotriene receptor antagonists, such as montelukast, are commonly prescribed for asthma therapy. Several large placebo-controlled studies have shown that montelukast alone or in combination with loratadine produces significant improvements in daytime and night-time nasal symptoms, ocular symptoms and total symptom score (TSS) and better quality of life for patients with allergic rhinitis; single-agent efficacy was comparable to that of loratadine in these studies.[80–82] Data from a nasal challenge model have also shown comparable in vivo efficacy between the antihistamine fexofenadine and montelukast.[83] In addition, a study of desloratadine and montelukast in patients with seasonal allergic rhinitis and asthma showed that both agents significantly and comparably improved asthma symptoms and reduced β2-adrenoceptor agonist use.[84]
Anti-IgE antibody therapy with omalizumab, a recombinant humanised murine monoclonal antibody, is another promising approach for the treatment of allergic rhinitis, having been shown to reduce nasal symptom scores in patients with seasonal allergic rhinitis in response to ragweed[85] and perennial allergic rhinitis.[86] Omalizumab works by reducing the level of circulating IgE and reducing Fcε receptor 1 expression on mast cells and basophils; omalizumab-induced reductions in IgE have been shown to correlate with symptom improvement.[87–89] Allergen immunotherapy is another approach for the treatment of allergic rhinitis; this works by reducing circulating IgE levels. The therapy acts to build up the patient’s immune responses, thereby desensitising the patient to the allergen and preventing increases in IgE levels.[45,90] Immunotherapy for grass pollen allergy has been shown to be effective and vaccination with genetically engineered allergens and hybrid molecules has been proven to be active in preventing the progression of allergic disease.[91–93]
2. Desloratadine
Desloratadine is a long-acting, novel, nonsedating H1 receptor inverse agonist that is the primary active metabolite of loratadine.[58] Desloratadine undergoes less extensive first-pass metabolism than loratadine and has a mean elimination half-life of 27 hours[94] compared with 12–15 hours for loratadine.[95] It is indicated for the relief of the nasal and non-nasal symptoms of seasonal and perennial allergic rhinitis and for the relief of symptoms associated with chronic idiopathic urticaria.[58] It is approved in the US for paediatric use in perennial allergic rhinitis and chronic idiopathic urticaria from 6 months of age and in seasonal allergic rhinitis from 2 years of age. The standard recommended adult dosage is 5mg given once daily; for 6- to 11-year-olds the dose is 2.5mg; for 1- to 5-year-olds it is 1.25mg; and for infants aged 6–11 months it is 1.0mg (all given once daily). The clinical development programme for desloratadine included >2300 patients between the ages of 12 and 75 years with allergic disease[94] and published postmarketing analyses have described the safety and efficacy of desloratadine in an additional ~54 000 patients.[96,97]
2.1 Antihistaminic and Anti-inflammatory Effects
In vitro studies have documented that desloratadine is a potent peripheral H1 receptor inverse agonist with an increased affinity and avidity for H1 receptors compared with other second-generation agents.[98–100] Radioligand-receptor binding studies have demonstrated that desloratadine is 15- to 20-fold more potent than loratadine and terfenadine[98] and has 50- to 194-fold greater affinity than cetirizine, loratadine and fexofenadine.[99] Furthermore, desloratadine failed to bind to dopamine, bradykinin or GABA receptors, illustrating that it has enhanced receptor specificity. Collectively, these studies suggest that the increased specificity of desloratadine over that of older antihistamines, which cause CNS impairment, may reduce its potential for adverse effects.[99]
In vitro studies demonstrate that desloratadine, like all H1 receptor antagonists, has anti-inflammatory properties that inhibit various mediators associated with early- and late-phase allergic responses. Kleine-Tebbe and colleagues[101] reported that desloratadine provided dose-dependent inhibition of both IgE- and non-IgE-induced leucocyte histamine release from mast cells and basophils. Desloratadine has been shown to inhibit IgE-mediated release of tryptase, leukotriene C4 (LTC4) and prostaglandin D2 from mast cells and basophils.[102] H1 receptor inverse agonists have also been shown to downregulate transcription factors activated by H1 receptors, such as nuclear factor κB (NF-κB), which are considered to play an important role in inflammatory processes.[103]
Inhibition of late-phase mediators of the allergic cascade can subsequently reduce mucinous secretions and nasal congestion.[104,105] Desloratadine inhibited the release of cytokines, chemokines and adhesion molecules associated with the late-phase response. Schroeder and colleagues[106] reported that pretreatment of basophil-enriched preparations with desloratadine significantly blocked anti-IgE-induced IL-4 and IL-13 secretion; histamine release and LTC4 generation were also inhibited. Desloratadine also dose dependently inhibited IL-6 and IL-8 production by histamine-treated human umbilical vein endothelial cells[107] and by human mast cells and basophils stimulated by phorbol myristate acetate or calcium ionophore.[108] Desloratadine reduced the release of IL-3, IL-6, tumour necrosis factor (TNF)-α and granulocyte-macrophage colony-stimulating factor from stimulated mast cells and basophils to an extent similar to that for dexamethasone but greater than that for cetirizine.[109] Additionally, desloratadine reduced TNFα-induced release of the chemokine RANTES from nasal polyp epithelial cells[110] and inhibited up regulation of the adhesion molecules ICAM-1 and P-selectin.[107,111] The ability of desloratadine to exert its anti-inflammatory and anti-allergic effects on early- and late-phase responses may contribute to its efficacy in the treatment of allergic disease. To date, the putative anti-inflammatory activity of desloratadine has not been fully demonstrated in vivo in patients with allergic rhinitis.
Desloratadine has a long half-life (~27 hours), which allows for once-daily administration, and it provides full 24-hour symptom relief.[42,53,112] A significantly greater reduction from baseline in instantaneous TSS at 24 hours after the first dose was seen with desloratadine compared with placebo in studies in patients with seasonal and perennial allergic rhinitis and this was maintained for the durations of the studies.[42,112] Desloratadine also has a rapid onset of action; the drug exhibits an antihistaminic effect by 1 hour postadministration in human histamine skin wheal testing.[94] In the Vienna Challenge Chamber studies carried out by Horak et al.[61] patients treated with desloratadine showed significant symptom reduction compared with those given placebo within 30 minutes of allergen exposure. A study by Day et al.[49] in patients with seasonal allergic rhinitis in an environmental exposure unit showed that the onset of action of desloratadine was 3 hours. The pharmacokinetic profile of desloratadine is not significantly influenced by patient age, sex or race,[113,114] which suggests that dose requirements do not vary from person to person; these characteristics may simplify prescribing practices for physicians. However, dose reduction is required for patients with hepatic or renal insufficiency. In patients with renal impairment, plasma concentrations were shown to be increased compared with those in patients with normal renal function. In hepatically impaired patients, there was a 2.4-fold increase in the AUC of desloratadine compared with that in patients with normal liver function and the mean elimination half-life was increased.[94]
2.2 Clinical Efficacy
2.2.1 Allergic Rhinitis
Clinical studies have shown that once-daily doses of desloratadine ranging from 5 to 20mg are similarly effective and safe in patients with seasonal allergic rhinitis.[53] Dosages of 5mg once daily rapidly and effectively reduced nasal and non-nasal symptoms during the spring and autumn allergy seasons.[42] Reductions in reflective and instantaneous TSS have been observed as early as day 2 of treatment and were maintained for the duration of therapy. Recently, the Allergic Rhinitis and its Impact on Asthma (ARIA) panel of the WHO put forth a set of guidelines describing the link between allergic rhinitis and asthma; these guidelines suggested that optimal treatment should be effective against symptoms in both the upper and lower airways.[115] Indeed, desloratadine has demonstrated beneficial effects in relieving symptoms affecting both of these areas. Berger and colleagues[116] evaluated the efficacy of desloratadine 5mg once daily in a 4-week, double-blind, placebo-controlled trial of 331 patients with mild asthma, seasonal allergic rhinitis and nasal congestion. Improvements in total nasal and non-nasal seasonal allergic rhinitis symptom scores were observed and pulmonary effects were apparent, in that total asthma symptom scores improved and the use of inhaled bronchodilator for rescue decreased after desloratadine administration. Meanwhile, studies have shown similar efficacies in perennial allergic rhinitis and asthma for desloratadine and various second-generation antihistamines.[46,117] However, it should be noted that desloratadine is not indicated for relief of asthma symptoms.
Clinical studies of antihistamines in patients with perennial allergic rhinitis are limited compared with those addressing the efficacy of therapy in patients with seasonal allergic rhinitis. Results obtained from two independent research groups have demonstrated the efficacy of desloratadine in patients with perennial allergic rhinitis.[112,118] Simons and colleagues[112] reported that desloratadine significantly reduced the TSS associated with perennial allergic rhinitis; nasal symptoms, including rhinorrhoea, nasal itching, sneezing and postnasal drip, were also reduced compared with placebo. Symptom relief was observed after the first dose of desloratadine; adverse events were similar for desloratadine- and placebo-treated patients. Another study confirmed and extended the results of the previous group by providing subjective and objective (i.e. PNIF) measurements, which demonstrated the effectiveness of desloratadine in patients with perennial allergic rhinitis.[118] Collectively, the results of the study demonstrated that desloratadine is an effective and safe therapy for reducing nasal and non-nasal symptoms associated with this chronic condition.
2.2.2 Chronic Idiopathic Urticaria
Desloratadine has also shown efficacy in patients with chronic idiopathic urticaria. In clinical trials, desloratadine significantly lessened the severity of pruritus, the number and size of hives, and the frequency of the sleep disturbances associated with chronic idiopathic urticaria.[12,13,29,72] In one double-blind, placebo-controlled study assessing the effects of treatment with once-daily desloratadine 5mg for up to 6 weeks in 190 patients with chronic idiopathic urticaria, desloratadine therapy reduced pruritis scores from baseline by 74% compared with 48.7% in the placebo group at 6 weeks and also conferred a significant first-dose effect, with pruritis, the number of hives and the size of the largest hive being reduced from baseline by 35–45% and the TSS being reduced by 41.6%, compared with 10.6% in the placebo group.[13,29] In another double-blind, placebo-controlled trial of desloratadine 5mg once daily, the drug was again shown to significantly improve the TSS, pruritis, number of hives and the size of the largest hive compared with placebo. Global chronic idiopathic urticaria status improved significantly with desloratadine, and sleep disruption was reduced. Significant improvements were seen within the first 24 hours of therapy and these were sustained for the duration of the study.[72] Meanwhile, in a 4-week open-label study of desloratadine in patients with chronic idiopathic urticaria, symptoms of chronic idiopathic urticaria were completely eradicated in approximately 50% of patients by the end of the study and 71.7% of patients reported no evening pruritis, compared with 12.9% of patients at baseline.[13] Desloratadine, along with other antihistamines, has also been shown to have 24-hour activity against histamine-induced wheal, flare and itch in the skin in a number of clinical studies.[69–71] Finally, clinical studies have shown that desloratadine in combination with montelukast is highly effective as a treatment for chronic idiopathic urticaria,[11,28] with Nettis et al.[11] finding that the combination regimen improved patients’ symptoms and quality of life significantly more than desloratadine alone.
2.2.3 Quality-of-Life Issues
Treatment with desloratadine has been associated with improvements in quality of life in patients with allergic rhinitis and chronic urticaria or chronic idiopathic urticaria. These improvements in quality of life are owing to decreases in symptom severity and also to reductions in adverse events compared with other therapies. In a randomised, double-blind study of desloratadine and budesonide in seasonal allergic rhinitis patients, Bhatia et al.[76] showed that both treatments caused a significant increase in PNIF compared with baseline and resulted in clinically significant reductions in the individual domains and overall scores on the Rhinoconjunctivitis Quality of Life Questionnaire. In chronic urticaria, desloratadine alone and in combination with montelukast improved patients’ quality of life, which was assessed using a quality of life questionnaire derived from the Dermatology Life Quality Index.[11] In addition, two surveys by Glass and Harper[119,120] have shown that patient satisfaction with their antiallergy treatment is, on average, increased upon switching to desloratadine from loratadine, cetirizine or fexofenadine.
2.3 Decongestant Effects
Relief of nasal congestion is an important element in allergic rhinitis therapy because of its association with snoring and with sleep-disordered breathing,[16] both of which can lead to impaired performance of daytime activities. Selected newer, nonsedating antihistamines are generally effective in reducing symptoms of nasal congestion[36,37,44,46,49,52,59,63,116,121] and can be used in combination with an oral decongestant for increased symptom relief.[54,122–124] Desloratadine has several anti-inflammatory actions that affect the pathophysiology of nasal congestion and it has been shown in several clinical trials to significantly reduce nasal congestion.[61,62,112,118,125–127]
In a double-blind, placebo-controlled trial, 346 patients with a history of intermittent allergic rhinitis and symptoms of nasal congestion at baseline received desloratadine 5mg once daily for 2 weeks.[125] At baseline, most patients had moderately severe symptoms of nasal congestion or stuffiness. During the 2-week treatment period, desloratadine significantly reduced mean morning/afternoon nasal congestion scores compared with placebo (p < 0.05). Nasal congestion scores were significantly reduced with the first dose of desloratadine, as determined by the instantaneous morning score on day 2; reductions were maintained for the 2-week study. Additionally, other nasal and non-nasal symptom scores and the TSS were significantly reduced from baseline for the 2-week study.
Horak and colleagues[126] reported the effects of desloratadine on objective and subjective measures of nasal airflow and symptoms of seasonal allergic rhinitis in patients exposed to grass pollen in the Vienna Challenge Chamber. In this open-label trial, 28 patients received desloratadine 5mg for 3 days following an allergen challenge on day 1. Patients rapidly experienced significant resolution of nasal congestion or obstruction on day 1. On day 4, between 21 and 24 hours after the last dose of desloratadine, patients underwent a second allergen challenge. Mean nasal stuffiness scores were mild or reduced for 2 hours, which suggested that the decongestant effects of desloratadine were maintained for 24 hours. In three separate double-blind, placebo-controlled studies,[127] single doses of desloratadine 5mg significantly resolved nasal blockage after administration and reduced the nasal stuffiness score from baseline by approximately 20% to nearly 40% (p ≤ 0.02 vs placebo). In another double-blind, crossover, placebo-controlled study, pretreatment with desloratadine 5mg daily for 7 days resulted in significantly less severe reductions in nasal air flow compared with placebo during a 6-hour allergen exposure in the Vienna Challenge Chamber.[61] Desloratadine was also associated with significantly lower nasal congestion symptom severity scores, lower volumes of nasal secretions and reduced seasonal allergic rhinitis symptoms compared with placebo. Total nasal and non-nasal seasonal allergic rhinitis symptom scores were significantly reduced.
2.4 Safety and Tolerability of Desloratadine
In clinical studies of treatment for both allergic rhinitis and chronic idiopathic urticaria, desloratadine exhibited an adverse event profile similar to that for placebo.[11,13,28,29,42,53,72,84,112,116,125] Most adverse events were of mild to moderate severity and occurred with similar frequency among patients treated with desloratadine and placebo. The most commonly reported adverse events included headache, dry mouth, somnolence and gastrointestinal events. Adverse event-related study discontinuations were minimal. Similar results were found in paediatric studies[128] and the US FDA concluded that there were no new safety concerns regarding the use of desloratadine in the paediatric population following a 1-year postexclusivity adverse event review.[129] In a large postmarketing study, 99% of patients and physicians rated the tolerability and safety of desloratadine as excellent, good or moderate.[96]
2.4.1 CNS Safety
Impairment of CNS function after the administration of first-generation antihistamines can result in sedation and severe decrements in cognitive function.[33,130] For example, it has been shown that these drugs significantly impair driving performance.[131] Therefore, allergic rhinitis is better managed with the relatively nonimpairing second-generation antihistamines; some of these drugs may cause differing levels of drowsiness or impairment, especially at higher-than-recommended doses.[132] In vitro and in vivo analyses have demonstrated that desloratadine does not cause CNS effects, even at higher-than-recommended doses.[133] These findings have been confirmed in clinical studies. In two crossover, placebo-controlled studies, a single dose of desloratadine 7.5mg, diphenhydramine 50mg or placebo was administered to a total of 44 healthy volunteers;[134] the primary endpoints were the effects of treatments on daytime somnolence and psychomotor performance. The Maintenance of Wakefulness Test (MWT), which describes the minimum time to stage 1 or rapid eye movement sleep when the subject is trying to stay awake, and the Multiple Sleep Latency Test (MSLT), which assesses the presence and severity of daytime somnolence and the time to falling asleep, were used to detect treatment effects. Desloratadine was not significantly different from placebo for mean changes from baseline in the MWT or the MSLT. In contrast, diphenhydramine significantly impaired performance and increased daytime somnolence compared with placebo and desloratadine. In another crossover, placebo-controlled study using promethazine 25mg as an active control, the effects of desloratadine 5mg on psychomotor performance, daytime sleep latencies, subjective sleepiness and memory were studied in nine volunteers.[135] Assessments were made at 1 hour predose and 0.5–8 hours post-dose. While promethazine impaired tracking, choice reaction time, digit symbol substitution and attention, and increased subjective sleepiness and fatigue, desloratadine was shown to be free of adverse effects on psychomotor performance, daytime sleep latencies and subjective sleepiness.[135] Meanwhile, Wilken et al.[136] compared the effects of diphenhydramine 50mg and desloratadine 5mg on vigilance and cognitive function in patients with ragweed-induced allergic rhinitis. Patients were assessed using a range of neuropsychological tests before treatment and at 90 minutes postdose. It was found that desloratadine improved allergic rhinitis symptoms without adversely affecting performance, whereas diphenhydramine improved symptoms but caused significant decreases in vigilance and cognitive function, and significantly greater sleepiness.
Because CNS effects may impair a patient’s ability to operate a vehicle, several studies have investigated the effects of desloratadine on driving and flying performance. Vuurman and colleagues[137] reported the results of a double-blind, crossover study of driving performance in 18 healthy volunteers who were administered single doses of desloratadine 5mg, diphenhydramine 50mg or placebo, with at least a 5-day washout between treatments. In a 90-minute test starting 2 hours after administration, no significant increase in weaving while driving was noted when desloratadine therapy was compared with placebo. In contrast, diphenhydramine significantly increased weaving compared with both desloratadine and placebo. Brake reaction time was significantly faster following desloratadine treatment than treatment with placebo or diphenhydramine.
Effects on flying ability under simulated cabin pressure conditions were evaluated in a double-blind, crossover study of 21 healthy men who were also given a single dose of desloratadine 5mg, diphenhydramine 50mg or placebo.[138] At least a 7-day washout was required between treatments and patients were evaluated for 6 hours after drug administration. Desloratadine did not cause any significant changes compared with placebo in tracking performance or vigilance task performance, measures of complex task performance or sleepiness. As in the previous study, diphenhydramine caused significant impairment by reducing tracking performance and resource management parameters, and increasing sleepiness.
Alcohol can impair performance, especially when administered with antihistamines that cause sedation. However, desloratadine does not potentiate alcohol-induced performance impairment, even at a higher-than-recommended dose.[139] In a crossover, placebo-controlled study, alcohol administration significantly increased sleepiness, decreased the number of substitutions in a digit symbol substitution test and increased reaction time compared with no alcohol administration in 25 healthy volunteers.[139] However, performance measures were not significantly different following a single dose of desloratadine 7.5mg than they were after placebo, regardless of whether alcohol was administered.
2.4.2 Cardiovascular Safety
Preclinical and clinical studies have demonstrated that desloratadine, like other later second-generation antihistamines, is not associated with cardiovascular toxicity. Unlike terfenadine and quinidine, desloratadine at concentrations of up to 10 μmol/L does not affect the cardiac K+ human ether-a-go-go-related gene (HERG) channel, when this is expressed in Xenopus oocytes.[133] Blockade of this potassium channel in humans is associated with QTc interval prolongation, torsades de pointes and sudden cardiac death.[140] Furthermore, studies in laboratory animals have shown that desloratadine does not appreciably affect blood pressure, heart rate or ECG parameters, including the QRS and QTc intervals.[133]
Even at very high concentrations, desloratadine is not associated with cardiovascular adverse events. In a double-blind, crossover, placebo-controlled study, desloratadine 45mg (nine times the recommended dose) was administered to 24 healthy volunteers for 10 days, followed by a 14-day washout period before crossover.[141] Serial ECGs were recorded at baseline and throughout the study. No clinically relevant differences in cardiovascular parameters and no prolongation of the QTc interval were evident from baseline or within 10 days of administration of high-dose desloratadine.
2.5 Improved Drug-Drug and Drug-Food Interaction Profile
Desloratadine does not interact with concomitantly administered drugs and foods. Clinical studies have examined the coadministration of desloratadine with several known inhibitors of the CYP system, the enzyme system by which desloratadine is metabolised. In a study of 36 healthy volunteers, desloratadine 5mg once daily was administered alone and in combination with cimetidine (an inhibitor of CYP3A4, 2D6, 1A2 and 2C19) every 12 hours.[142] At steady state, no clinically relevant changes in the mean AUC24 and Cmax of desloratadine or 3-OH desloratadine (the primary metabolite of desloratadine) were seen with the combination compared with desloratadine alone. In addition, no clinically relevant ECG changes were observed. Administration of desloratadine 7.5mg once daily with the CYP3A4 inhibitors ketoconazole or erythromycin in two separate studies also confirmed that coadministration does not induce clinically relevant alterations in ECG or pharmacokinetic parameters.[143,144] In vitro analyses indicate that neither desloratadine nor 3-OH desloratadine is an inhibitor of other agents metabolised by the CYP isoenzymes 1A2, 2C9, 2C19, 2D6 or 3A4.[145]
In vitro studies have demonstrated that desloratadine is neither an inhibitor nor a significant substrate of P-glycoprotein.[146,147] These findings were reinforced by clinical interaction studies performed with desloratadine. Coadministration of desloratadine and azithromycin failed to cause clinically relevant changes in AUC or Cmax values or in the ECG.[65] In addition, desloratadine is devoid of drug-food interactions.[148,149] Gupta and colleagues[148] reported that, in an open-label, single-dose, crossover study of 18 healthy volunteers who received desloratadine 7.5mg under fed and fasted conditions, the plasma concentration-time profiles were similar between fed and fasted conditions, and the relative bioavailability of desloratadine was also comparable. Administration of a high-fat meal had no effect on the oral bioavailability of desloratadine, which indicates that desloratadine may be taken with meals or without meals.[148] Additionally, administration with grapefruit juice, a known inhibitor of CYP3A4 and OATP, did not alter the absorption or bioavailability of desloratadine 5mg.[149]
The results of these studies indicate that desloratadine is not prone to drug-drug and drug-food interactions. For this reason, clinicians can prescribe desloratadine with confidence that its bioavailability will not be complicated by changes in diet or drug therapy.
2.6 Postmarketing Studies: ‘Real-World’ Efficacy of Desloratadine
Postmarketing surveillance studies provide an opportunity for a drug to be evaluated in a real-world clinical practice setting. These studies use objective and subjective measures to evaluate safety and efficacy, and to confirm the results obtained in controlled clinical trials. Bachert and colleagues[96] reported the results of an open-label, postmarketing surveillance study conducted in 47 953 patients in Germany. Patients were treated by general practitioners or allergists for symptoms of seasonal allergic rhinitis. Patients and physicians completed study questionnaires at enrolment and at the end of treatment, which lasted a mean duration of 38 days. Patients assessed nasal (nasal congestion, runny nose, sneezing/itching), ocular (watery eyes, burning/itching, redness), asthma (wheezing, breathlessness, chest tightness, cough), and dermal (itching, hives/pustules, dryness) symptoms. Significant reductions from baseline, which ranged from 72% to 81%, were observed for nasal, ocular and dermal symptoms, and the TSS. Before treatment, 67% of patients had moderate to severe symptoms of nasal congestion; however, only 6% had moderate to severe congestion after treatment with desloratadine. The proportion of patients who reported no nasal congestion increased from 14% to 55% (p = 0.0001). Approximately 93% of patients rated their symptoms of congestion, rhinorrhoea or itching/sneezing after treatment as none or mild. More than 19 500 patients had at least one symptom of asthma at baseline and treatment with desloratadine significantly reduced the mean asthma TSS (p = 0.0001). Of these patients, 51% reported a reduction in their need for asthma medication. Overall, 91% of patients and 93% of physicians rated the global efficacy of desloratadine treatment as good or excellent. Global safety/tolerability was rated as good/excellent by 98.9% of physicians and 98.5% of patients, and the adverse event rate was very low at 0.44%. No single adverse event was experienced by >0.1% of the population; the most common probable/possible treatment-related adverse events were fatigue, headache, nausea, dry mouth and diarrhoea, and the majority of adverse events were of mild or moderate severity.[96]
In a preliminary report of a patient experience trial conducted in the US, 6064 patients with seasonal allergic rhinitis responded to questionnaires regarding their worst seasonal allergic rhinitis symptom before and after desloratadine therapy.[97] After desloratadine therapy, 85% of patients reported relief from their worst symptom regardless of what it was. The area of greatest improvement was sleep interruption because of seasonal allergic rhinitis. Collectively, the results obtained in these real-world studies confirmed those from clinical trials of desloratadine.
3. Conclusion
Antihistamines are a first-line pharmacotherapy for the treatment of allergic disorders such as allergic rhinitis and chronic idiopathic urticaria. Desloratadine, a second-generation antihistamine, effectively manages the symptoms of allergic disease, including nasal congestion. In addition, quality of life assessments have demonstrated significant improvements in daily activities and reduced sleep impairment. Desloratadine can be confidently administered once daily in patients regardless of age, sex or race, and can also be administered in paediatric patients. Dose reductions are required for patients with renal or hepatic impairment. The risks associated with desloratadine are minimal; no significant CNS-related or cardiovascular adverse effects have been associated with treatment in clinical studies. Desloratadine has no known drug-drug or drug-food interactions of clinical relevance and does not potentiate the effects of alcohol. Large postmarketing studies, which have confirmed the results obtained in clinical trials, demonstrate the efficacy and safety of desloratadine in a real-world setting.
References
Salib RJ, Drake-Lee A, Howarth PH. Allergic rhinitis: past, present and the future. Clin Otolaryngol 2003; 28(4): 291–303
D’Alonzo G. Scope and impact of allergic rhinitis. J Am Osteopath Assoc 2002; 102(6 Suppl. 2): S2–6
Schoenwetter WF, Dupclay Jr L, Appajosyula S, et al. Economic impact and quality-of-life burden of allergic rhinitis. Curr Med Res Opin 2004; 20(3): 305–17
Reed SD, Lee TA, McCrory DC. The economic burden of allergic rhinitis: a critical evaluation of the literature. Pharmacoeconomics 2004; 22(6): 345–61
Brunton SA. Allergy management strategies: an update. Patient Care 2002; Suppl. (Spring): 16–25
Bauchau V, Durham SR. Prevalence and rate of diagnosis of allergic rhinitis in Europe. Eur Respir J 2004; 24: 758–64
Bronsky E. The burden of allergic disease. Patient Care 2002; Suppl. (Spring): 1–6
van Cauwenberge P, Bachert C, Passalacqua G, et al. Consensus statement on the treatment of allergic rhinitis. Allergy 2000; 55(2): 116–34
Sabroe RA, Greaves MW. The pathogenesis of chronic idiopathic urticaria. Arch Dermatol 1997; 133(8): 1003–8
Champion RH. Urticaria: then and now. Br J Dermatol 1988; 119(4): 427–36
Nettis E, Colanardi MC, Paradiso MT, et al. Desloratadine in combination with montelukast in the treatment of chronic urticaria: a randomized, double-blind, placebo-controlled study. Clin Exp Allergy 2004; 34(9): 1401–7Z
Ring J, Hein R, Gauger A. Desloratadine in the treatment of chronic idiopathic urticaria. Allergy 2001; 56Suppl. 65: 28–32
Ring J, Gauger A, Hein R. Clinical efficacy of desloratadine in chronic urticaria. Clin Drug Invest 2002; 22Suppl. 2: 33–41
Kozel MM, Sabroe RA. Chronic urticaria: aetiology, management and current and future treatment options. Drugs 2004; 64(22): 2515–36
Ring J, Brockow K, Ollert M, et al. Antihistamines in urticaria. Clin Exp Allergy 1999; 29Suppl. 1: 31–7
Young T, Finn L, Kim H. Nasal obstruction as a risk factor for sleep-disordered breathing: the University of Wisconsin Sleep and Respiratory Research Group. J Allergy Clin Immunol 1997; 99(2): S757–62
Settipane RA. Complications of allergic rhinitis. Allergy Asthma Proc 1999; 20(4): 209–13
Wilken JA, Berkowitz R, Kane R. Decrements in vigilance and cognitive functioning associated with ragweed-induced allergic rhinitis. Ann Allergy Asthma Immunol 2002; 89(4): 372–80
Meltzer EO, Szwarcberg J, Pill MW. Allergic rhinitis, asthma, and rhinosinusitis: diseases of the integrated airway. J Manag Care Pharm 2004; 10(4): 310–7
Santos R, Cifaldi M, Gregory C, et al. Economic outcomes of a targeted intervention program: the costs of treating allergic rhinitis patients. Am J Manag Care 1999; 5(4 Suppl.): S225–34
Blaiss MS. Cognitive, social, and economic costs of allergic rhinitis. Allergy Asthma Proc 2000; 21(1): 7–13
American Academy of Allergy Asthma & Immunology (AAAAI). The allergy report. Volume I: overview of allergic diseases: diagnosis, management, and barriers to care. Milwaukee (WI): AAAAI, 2000
Pearlman DS. Pathophysiology of the inflammatory response. J Allergy Clin Immunol 1999; 104(4 Pt 1): S132–7
Baraniuk JN. Pathogenesis of allergic rhinitis. J Allergy Clin Immunol 1997; 99(2): S763–72
Greaves MW. Pathophysiology of chronic urticaria. Int Arch Allergy Immunol 2002; 127(1): 3–9
Greaves MW. Chronic idiopathic urticaria. Curr Opin Allergy Clin Immunol 2003; 3(5): 363–8
Fell WR, Mabry RL, Mabry CS. Quality of life analysis of patients undergoing immunotherapy for allergic rhinitis. Ear Nose Throat J 1997; 76(8): 528–32, 34-6
Di Lorenzo G, Pacor ML, Mansueto P, et al. Randomized placebo-controlled trial comparing desloratadine and montelukast in monotherapy and desloratadine plus montelukast in combined therapy for chronic idiopathic urticaria. J Allergy Clin Immunol 2004; 114(3): 619–25
Ring J, Hein R, Gauger A, et al. Once-daily desloratadine improves the signs and symptoms of chronic idiopathic urticaria: a randomized, double-blind, placebo-controlled study. Int J Dermatol 2001; 40(1): 72–6
Greaves M. Chronic urticaria. J Allergy Clin Immunol 2000; 105(4): 664–72
DuBuske LM. Safety and efficacy in allergy management. Patient Care 2002; Suppl. (Spring): 26–33
Bender BG, Berning S, Dudden R, et al. Sedation and performance impairment of diphenhydramine and second-generation antihistamines: a meta-analysis. J Allergy Clin Immunol 2003; 111(4): 770–6
Gengo FM, Gabos C. Antihistamines, drowsiness, and psychomotor impairment: central nervous system effect of cetirizine. Ann Allergy 1987; 59(6 Pt 2): 53–7
Day JH, Briscoe M, Widlitz MD. Cetirizine, loratadine, or placebo in subjects with seasonal allergic rhinitis: effects after controlled ragweed pollen challenge in an environmental exposure unit. J Allergy Clin Immunol 1998; 101(5): 638–45
Mabry R. Recent advances in pharmacotherapy of allergic rhinitis. Curr Opin Otolaryngol Head Neck Surg 1999; 7: 375–8
Golden SJ, Craig TJ. Efficacy and safety of azelastine nasal spray for the treatment of allergic rhinitis. J Am Osteopath Assoc 1999; 99(7 Suppl.): S7–12
Simons FE. Advances in H1-antihistamines. N Engl J Med 2004; 351(21): 2203–17
Cockburn IM, Bailit HL, Berndt ER, et al. Loss of work productivity due to illness and medical treatment. J Occup Environ Med 1999; 41(11): 948–53
Kelloway JS, Pongowski MA, Schoenwetter WF. Additional causes of torsades de pointes. Mayo Clin Proc 1995; 70(2): 197
DuBuske LM. Second-generation antihistamines: the risk of ventricular arrhythmias. Clin Ther 1999; 21(2): 281–95
Barbey JT, Anderson M, Ciprandi G, et al. Cardiovascular safety of second-generation antihistamines. Am J Rhinol 1999; 13(3): 235–43
Meltzer EO, Prenner BM, Nayak A, et al. Efficacy and tolerability of once-daily 5mg desloratadine, an H1-receptor antagonist, in patients with seasonal allergic rhinitis. Clin Drug Invest 2001; 21(1): 25–32
Charpin D, Godard P, Garay RP, et al. A multicenter clinical study of the efficacy and tolerability of azelastine nasal spray in the treatment of seasonal allergic rhinitis: a comparison with oral cetirizine. Eur Arch Otorhinolaryngol 1995; 252(8): 455–8
Wilson AM, Orr LC, Coutie WJ, et al. A comparison of once daily fexofenadine versus the combination of montelukast plus loratadine on domiciliary nasal peak flow and symptoms in seasonal allergic rhinitis. Clin Exp Allergy 2002; 32(1): 126–32
Willsie SK. Improved strategies and new treatment options for allergic rhinitis. J Am Osteopath Assoc 2002; 102(6 Suppl. 2): S7–14
Lee DK, Gardiner M, Haggart K, et al. Comparative effects of desloratadine, fexofenadine, and levocetirizine on nasal adenosine monophosphate challenge in patients with perennial allergic rhinitis. Clin Exp Allergy 2004; 34(4): 650–3
Passalacqua G, Guerra L, Compalati E, et al. Comparison of the effects in the nose and skin of a single dose of desloratadine and levocetirizine over 24 hours. Int Arch Allergy Immunol 2004; 135(2): 143–7
Deruaz C, Leimgruber A, Berney M, et al. Levocetirizine better protects than desloratadine in a nasal provocation with allergen. J Allergy Clin Immunol 2004; 113(4): 669–76
Day JH, Briscoe MP, Rafeiro E, et al. Comparative clinical efficacy, onset and duration of action of levocetirizine and desloratadine for symptoms of seasonal allergic rhinitis in subjects evaluated in the Environmental Exposure Unit (EEU). Int J Clin Pract 2004; 58(2): 109–18
Day JH, Briscoe MP, Rafeiro E, et al. Randomized double-blind comparison of cetirizine and fexofenadine after pollen challenge in the environmental exposure unit: duration of effect in subjects with seasonal allergic rhinitis. Allergy Asthma Proc 2004; 25(1): 59–68
Day JH, Briscoe MP, Welsh A, et al. Onset of action, efficacy, and safety of a single dose of fexofenadine hydrochloride for ragweed allergy using an environmental exposure unit. Ann Allergy Asthma Immunol 1997; 79(6): 533–40
Horak F, Stubner P, Zieglmayer R, et al. Controlled comparison of the efficacy and safety of cetirizine 10mg o.d. and fexofenadine 120mg o.d. in reducing symptoms of seasonal allergic rhinitis. Int Arch Allergy Immunol 2001; 125(1): 73–9
Salmun LM, Lorber R. 24-hour efficacy of once-daily desloratadine therapy in patients with seasonal allergic rhinitis [ISRCTN32042139]. BMC Fam Pract 2002; 3(1): 14
Sussman GL, Mason J, Compton D, et al. The efficacy and safety of fexofenadine HCl and pseudoephedrine, alone and in combination, in seasonal allergic rhinitis. J Allergy Clin Immunol 1999; 104(1): 100–6
Potter PC. Levocetirizine is effective for symptom relief including nasal congestion in adolescent and adult (PAR) sensitized to house dust mites. Allergy 2003; 58(9): 893–9
Stubner P, Zieglmayer R, Horak F. A direct comparison of the efficacy of antihistamines in SAR and PAR: randomised, placebo-controlled studies with levocetirizine and loratadine using an environmental exposure unit — the Vienna Challenge Chamber (VCC). Curr Med Res Opin 2004; 20(6): 891–902
Hampel F, Ratner P, Mansfield L, et al. Fexofenadine hydrochloride, 180mg, exhibits equivalent efficacy to cetirizine, 10mg, with less drowsiness in patients with moderate-to-severe seasonal allergic rhinitis. Ann Allergy Asthma Immunol 2003; 91(4): 354–61
Limon L, Kockler DR. Desloratadine: a nonsedating antihistamine. Ann Pharmacother 2003; 37(2): 237–46
Wilson AM, Haggart K, Sims EJ, et al. Effects of fexofenadine and desloratadine on subjective and objective measures of nasal congestion in seasonal allergic rhinitis. Clin Exp Allergy 2002; 32(10): 1504–9
Ciprandi G, Cirillo I, Vizzaccaro A, et al. Levocetirizine improves nasal obstruction and modulates cytokine pattern in patients with seasonal allergic rhinitis: a pilot study. Clin Exp Allergy 2004; 34(6): 958–64
Horak F, Stubner P, Zieglmayer R, et al. Effect of desloratadine versus placebo on nasal airflow and subjective measures of nasal obstruction in subjects with grass pollen-induced allergic rhinitis in an allergen-exposure unit. J Allergy Clin Immunol 2002; 109(6): 956–61
Horak F, Stubner P, Zieglmeyer R, et al. Comparison of the effects of desloratadine 5-mg daily and placebo on nasal airflow and seasonal allergic rhinitis symptoms induced by grass pollen exposure. Allergy 2003; 58(6): 481–5
Ciprandi G, Cosentino C, Milanese M, et al. Fexofenadine reduces nasal congestion in perennial allergic rhinitis. Allergy 2001; 56(11): 1068–70
DuBuske LM. Drug transport systems. Pharm Perspect 2001: 3–14
Gupta S, Banfield C, Kantesaria B, et al. Pharmacokinetic and safety profile of desloratadine and fexofenadine when coadministered with azithromycin: a randomized, placebo-controlled, parallel-group study. Clin Ther 2001; 23(3): 451–66
Allegra (fexofenadine) prescribing information. Kansas City (MO): Aventis Pharmaceuticals, 2000
Dresser GK, Schwarz UI, Wilkinson GR, et al. Fexofenadine bioavailability modulated by dietary salt [abstract]. Clin Pharmacol Ther 2001; 69(2): 23
Dresser GK, Bailey DG, Leake BF, et al. Fruit juices inhibit organic anion transporting polypeptide-mediated drug uptake to decrease the oral availability of fexofenadine. Clin Pharmacol Ther 2002; 71(1): 11–20
Purohit A, Melac M, Pauli G, et al. Comparative activity of cetirizine and desloratadine on histamine-induced wheal-and-flare responses during 24 hours. Ann Allergy Asthma Immunol 2004; 92(6): 635–4092 (6)
Denham KJ, Boutsiouki P, Clough GF, et al. Comparison of the effects of desloratadine and levocetirizine on histamine-induced wheal, flare and itch in human skin. Inflamm Res 2003; 52(10): 424–7
Purohit A, Melac M, Pauli G, et al. Twenty-four-hour activity and consistency of activity of levocetirizine and desloratadine in the skin. Br J Clin Pharmacol 2003; 56(4): 388–94
Monroe E, Finn A, Patel P, et al. Efficacy and safety of desloratadine 5mg once daily in the treatment of chronic idiopathic urticaria: a double-blind, randomized, placebo-controlled trial. J Am Acad Dermatol 2003; 48(4): 535–41
Nelson HS. Mechanisms of intranasal steroids in the management of upper respiratory allergic diseases. J Allergy Clin Immunol 1999; 104(4 Pt 1): S138–43
Nielsen LP, Dahl R. Comparison of intranasal corticosteroids and antihistamines in allergic rhinitis: a review of randomized, controlled trials. Am J Respir Med 2003; 2(1): 55–65
Weiner JM, Abramson MJ, Puy RM. Intranasal corticosteroids versus oral H1 receptor antagonists in allergic rhinitis: systematic review of randomised controlled trials. BMJ 1998; 317(7173): 1624–9
Bhatia S, Baroody FM, deTineo M, et al. Increased nasal airflow with budesonide compared with desloratadine during the allergy season. Arch Otolaryngol Head Neck Surg 2005; 131(3): 223–8
Dupclay Jr L, Doyle J. Assessment of intranasal corticosteroid use in allergic rhinitis: benefits, costs, and patient preferences. Am J Manag Care 2002; 8(13 Suppl.): S335–40
Kaszuba SM, Baroody FM, deTineo M, et al. Superiority of an intranasal corticosteroid compared with an oral antihistamine in the as-needed treatment of seasonal allergic rhinitis. Arch Intern Med 2001; 161(21): 2581–7
Meltzer EO. Clinical evidence for antileukotriene therapy in the management of allergic rhinitis. Ann Allergy Asthma Immunol 2002; 88(4 Suppl. 1): 23–9
Meltzer EO, Malmstrom K, Lu S, et al. Concomitant montelukast and loratadine as treatment for seasonal allergic rhinitis: a randomized, placebo-controlled clinical trial. J Allergy Clin Immunol 2000; 105(5): 917–22
Nayak AS, Philip G, Lu S, et al. Efficacy and tolerability of montelukast alone or in combination with loratadine in seasonal allergic rhinitis: a multicenter, randomized, double-blind, placebo-controlled trial performed in the fall. Ann Allergy Asthma Immunol 2002; 88(6): 592–600
Philip G, Malmstrom K, Hampel FC, et al. Montelukast for treating seasonal allergic rhinitis: a randomized, double-blind, placebo-controlled trial performed in the spring. Clin Exp Allergy 2002; 32(7): 1020–8
Lee DKC, Jackson CM, Soutar PC, et al. Effects of single or combined histamine H-1-receptor and leukotriene CysLT (1)-receptor antagonism on nasal adenosine mono phosphate challenge in persistent allergic rhinitis. Br J Clin Pharmacol 2004; 57(6): 714–9
Baena-Cagnani CE, Berger WE, DuBuske LM, et al. Comparative effects of desloratadine versus montelukast on asthma symptoms and use of beta 2-agonists in patients with seasonal allergic rhinitis and asthma. Int Arch Allergy Immunol 2003; 130(4): 307–13
Casale TB, Condemi J, LaForce C, et al. Effect of omalizumab on symptoms of seasonal allergic rhinitis: a randomized controlled trial. JAMA 2001; 286(23): 2956–67
Chervinsky P, Casale T, Townley R, et al. Omalizumab, an anti-IgE antibody, in the treatment of adults and adolescents with perennial allergic rhinitis. Ann Allergy Asthma Immunol 2003; 91(2): 160–7
D’Amato G, Oldani V, Donner CF. Anti-IgE monoclonal antibody: a new approach to the treatment of allergic respiratory diseases. Monaldi Arch Chest Dis 2003; 59(1): 25–9
Casale TB. Anti-immunoglobulin E (omalizumab) therapy in seasonal allergic rhinitis. Am J Respir Crit Care Med 2001; 164(8 Pt 2): S18–21
Brownell J, Casale TB. Anti-IgE therapy. Immunol Allergy Clin North Am 2004; 24(4): 551–68, v
Li JT. Immunotherapy for allergic rhinitis. Immunol Allergy Clin North Am 2000; 20(2): 383–400
Durham SR, Walker SM, Varga EM, et al. Long-term clinical efficacy of grass-pollen immunotherapy. N Engl J Med 1999; 341(7): 468–75
Niederberger V, Horak F, Vrtala S, et al. Vaccination with genetically engineered allergens prevents progression of allergic disease. Proc Natl Acad Sci U S A 2004; 101Suppl. 2: 14677–82
Linhart B, Jahn-Schmid B, Verdino P, et al. Combination vaccines for the treatment of grass pollen allergy consisting of genetically engineered hybrid molecules with increased immunogenicity. FASEB J 2002; 16(10): 1301–3
Schering Plough. Clarinex (desloratadine) product information. Kenilworth (NJ): Schering Plough, 2004
Claritin (loratadine) prescribing information. Kenilworth (NJ): Schering-Plough, 2000
Bachert C, Virchow JC, Plenker A. Desoloratadine in the treatment of seasonal allergic rhinitis: results of a large observatinal study. Clin Drug Invest 2002; 22Suppl. 2: 43–52
Kerney D. Real world treatment with desloratadine in seasonal allergic rhinitis (SAR) patients [abstract]. Ann Allergy Asthma Immunol 2003; 90: 123
Kreutner W, Hey JA, Anthes J, et al. Preclinical pharmacology of desloratadine, a selective and nonsedating histamine H1 receptor antagonist. 1st communication: receptor selectivity, antihistaminic activity, and antiallergenic effects. Arzneimittelforschung 2000; 50(4): 345–52
Anthes JC, Gilchrest H, Richard C, et al. Biochemical characterization of desloratadine, a potent antagonist of the human histamine H (1) receptor. Eur J Pharmacol 2002; 449(3): 229–37
Agrawal DK. Anti-inflammatory properties of desloratadine. Clin Exp Allergy 2004; 34(9): 1342–8
Kleine-Tebbe J, Josties C, Frank G, et al. Inhibition of IgE- and non-IgE-mediated histamine release from human basophil leukocytes in vitro by a histamine H1-antagonist, desethoxycarbonyl-loratadine. J Allergy Clin Immunol 1994; 93(2): 494–500
Genovese A, Patella V, De Crescenzo G, et al. Loratadine and desethoxylcarbonyl-loratadine inhibit the immunological release of mediators from human Fc epsilon RI+ cells. Clin Exp Allergy 1997; 27(5): 559–67
Bakker RA, Schoonus SB, Smit MJ, et al. Histamine H (1)-receptor activation of nuclear factor-kappa B: roles for G beta gamma- and G alpha (q/11)-subunits in constitutive and agonist-mediated signaling. Mol Pharmacol 2001; 60(5): 1133–42
Scadding GK. Desloratadine in the treatment of nasal congestion in seasonal allergic rhinitis: preclinical and clinical evidence. Clin Drug Invest 2002; 22Suppl. 2: 21–32
Greiff L, Persson CG, Andersson M. Desloratadine reduces allergen challenge-induced mucinous secretion and plasma exudation in allergic rhinitis. Ann Allergy Asthma Immunol 2002; 89(4): 413–8
Schroeder JT, Schleimer RP, Lichtenstein LM, et al. Inhibition of cytokine generation and mediator release by human basophils treated with desloratadine. Clin Exp Allergy 2001; 31(9): 1369–77
Molet S, Gosset P, Lassalle P, et al. Inhibitory activity of loratadine and descarboxyethoxyloratadine on histamine-induced activation of endothelial cells. Clin Exp Allergy 1997; 27(10): 1167–74
Lippert U, Kruger-Krasagakes S, Moller A, et al. Pharmacological modulation of IL-6 and IL-8 secretion by the H1-antagonist decarboethoxy-loratadine and dexamethasone by human mast and basophilic cell lines. Exp Dermatol 1995; 4(4 Pt 2): 272–6
Lippert U, Moller A, Welker P, et al. Inhibition of cytokine secretion from human leukemic mast cells and basophils by H1- and H2-receptor antagonists. Exp Dermatol 2000; 9(2): 118–24
Lebel B, Bousquet J, Czarlewski W, et al. Loratadine (L) reduces RANTES release by an epithelial cell line [abstract]. J Allergy Clin Immunol 1997; 99(1 Pt 2 Suppl. S): 1802
Papi A, Papadopoulos NG, Stanciu LA, et al. Effect of desloratadine and loratadine on rhinovirus-induced intercellular adhesion molecule 1 upregulation and promoter activation in respiratory epithelial cells. J Allergy Clin Immunol 2001; 108(2): 221–8
Simons FE, Prenner BM, Finn Jr A. Efficacy and safety of desloratadine in the treatment of perennial allergic rhinitis. J Allergy Clin Immunol 2003; 111(3): 617–22
Affrime M, Gupta S, Banfield C, et al. A pharmacokinetic profile of desloratadine in healthy adults, including elderly. Clin Pharmacokinet 2002; 41 Suppl. 1: 13–9
Affrime M, Banfield C, Gupta S, et al. Effect of race and sex on single and multiple dose pharmacokinetics of desloratadine. Clin Pharmacokinet 2002; 41Suppl. 1: 21–8
Bousquet J, Van Cauwenberge P, Khaltaev N. ARIA Workshop Group, World Health Organization. Allergic Rhinitis and its Impact on Asthma. J Allergy Clin Immunol 2001; 108Suppl. 5: S147–334
Berger WE, Schenkel EJ, Mansfield LE. Safety and efficacy of desloratadine 5mg in asthma patients with seasonal allergic rhinitis and nasal congestion. Ann Allergy Asthma Immunol 2002; 89(5): 485–91
Lee DK, Bates CE, Currie GP, et al. Comparative in vivo bioactivity of modern H1-antihistamines on AMP challenge in atopic asthma. J Allergy Clin Immunol 2003; 111(2): 337–41
Kim KT, Sussman GL, Herbert J, et al. Effect of once daily desloratadine in patients with perennial allergic rhinitis (PAR): a double-blind, placebo-controlled study. J Allergy Clin Immunol 2003; 111: S76–7
Glass DJ, Harper AS. Assessing satisfaction with desloratadine and fexofenadine in allergy patients who report dissatisfaction with loratadine. BMC Fam Pract 2003; 4(1): 10
Glass DJ, Harper AS. Assessing patient satisfaction with desloratadine after conversion from loratadine, fexofenadine, or cetirizine. Manag Care Interface 2004; 17: 29–34
Wang DY, Hanotte F, De Vos C, et al. Effect of cetirizine, levocetirizine, and dextrocetirizine on histamine-induced nasal response in healthy adult volunteers. Allergy 2001; 56(4): 339–43
Corren J, Harris AG, Aaronson D, et al. Efficacy and safety of loratadine plus pseudoephedrine in patients with seasonal allergic rhinitis and mild asthma. J Allergy Clin Immunol 1997; 100(6 Pt 1): 781–8
Bertrand B, Jamart J, Marchal JL, et al. Cetirizine and pseudoephedrine retard alone and in combination in the treatment of perennial allergic rhinitis: a double-blind multicentre study. Rhinology 1996; 34(2): 91–6
Schenkel E, Corren J, Murray JJ. Efficacy of once-daily desloratadine/pseudoephedrine for relief of nasal congestion. Allergy Asthma Proc 2002; 23(5): 325–30
Nayak AS, Schenkel E. Desloratadine reduces nasal congestion in patients with intermittent allergic rhinitis. Allergy 2001; 56(11): 1077–80
Horak F, Stubner P, Zieglmayer R, et al. Onset and duration of action of desloratadine after controlled pollen challenges in patients with seasonal allergic rhinitis [abstract no. 1000]. Allergy 2000; 55Suppl. 63: 279
Horak F, Stubner P. Decongestant activity of desloratadine in controlled allergen-exposure trials. Clin Drug Invest 2002; 22Suppl. 2: 13–20
Bloom M, Staudinger H, Herron J. Safety of desloratadine syrup in children. Curr Med Res Opin 2004; 20(12): 1959–65
Filie J. One year post exclusivity adverse event review: desloratadine [online]. Presented at the FDA Pediatric Advisory Committee meeting, 2004 Sep 15 Available from URL: http://www.fda.gov/ohrms/dockets/ac/04/slides/2004-4067s1_03_Filie%20Final.pdf [Accessed 2005 Apr 4 ]
Bower E, Moore J, Moss M, et al. Effects of a single-dose fexofenadine, diphenhydramine, and placebo on cognitive and psychomotor performance in naval flight personnel in a double-blind, crossover, randomised study [abstract]. Allergy 2000; 55Suppl. 63: 254
Verster JC, Volkerts ER. Antihistamines and driving ability: evidence from on-the-road driving studies during normal traffic. Ann Allergy Asthma Immunol 2004; 92(3): 294–303
Casale TB, Blaiss MS, Gelfand E, et al. First do no harm: managing antihistamine impairment in patients with allergic rhinitis. J Allergy Clin Immunol 2003; 111(5): S835–42
Kreutner W, Hey JA, Chiu P, et al. Preclinical pharmacology of desloratadine, a selective and nonsedating histamine H1 receptor antagonist. 2nd communication: lack of central nervous system and cardiovascular effects. Arzneimittelforschung 2000; 50(5): 441–8
Scharf MB, Kay G, Rikken G, et al. Desloratadine has no effect on wakefulness or psychomotor performance [abstract]. Allergy 2000; 55Suppl. 63: 280
Nicholson AN, Handford ADF, Turner C, et al. Studies on performance and sleepiness with the H-1-antihistamine, desloratadine. Aviat Space Environ Med 2003; 74(8): 809–15
Wilken JA, Kane RL, Ellis AK, et al. A comparison of the effect of diphenhydramine and desloratadine on vigilance and cognitive function during treatment of ragweed-induced allergic rhinitis. Ann Allergy Asthma Immunol 2003; 91(4): 375–85
Vuurman EF, Rikken GH, Muntjewerff ND, et al. Effects of desloratadine, diphenhydramine, and placebo on driving performance and psychomotor performance measurements. Eur J Clin Pharmacol 2004; 60(5): 307–13
Valk PJ, Van Roon DB, Simons RM, et al. Desloratadine shows no effect on performance during 6h at 8,000 ft simulated cabin altitude. Aviat Space Environ Med 2004; 75(5): 433–8
Data on file, Schering-Plough, 2005
Dumaine R, Roy ML, Brown AM. Blockade of HERG and Kv1.5 by ketoconazole. J Pharmacol Exp Ther 1998; 286(2): 727–35
Marino M, Glue P, Herron JM. Lack of electrocardiographic effects of multiple high doses of desloratadine [abstract]. Allergy 2000; 55Suppl. 63: 279
Khalilieh S, Krishna G, Marino M, et al. Lack of interaction with coadministration of desloratadine and cimetide [abstract]. Ann Allergy Asthma Immunol 2002; 88: 110
Banfield C, Herron J, Keung A, et al. Desloratadine has no clinically relevant electrocardiographic or pharmacodynamic interactions with ketoconazole. Clin Pharmacokinet 2002; 41Suppl. 1: 37–44
Banfield C, Hunt T, Reyderman L, et al. Lack of clinically relevant interaction between desloratadine and erythromycin. Clin Pharmacokinet 2002; 41Suppl. 1: 29–35
Barecki ME, Casciano CN, Johnson WW, et al. In vitro characterization of the inhibition profile of loratadine, desloratadine, and 3-OH-desloratadine for five human cytochrome P-450 enzymes. Drug Metab Dispos 2001; 29(9): 1173–5
Hwang K, Offord S, Correll M. Evaluation of P-gp substrate potential of desloratadine [abstract]. Ann Allergy Asthma Immunol 2001; 86: 111
Wang EJ, Casciano CN, Clement RP, et al. Evaluation of the interaction of loratadine and desloratadine with P-glycoprotein. Drug Metab Dispos 2001; 29(8): 1080–3
Gupta S, Banfield C, Affrime M, et al. Oral bioavailability of desloratadine is unaffected by food. Clin Pharmacokinet 2001; 41Suppl. 1: 7–12
Banfield C, Gupta S, Marino M, et al. Grapefruit juice reduces the oral bioavailability of fexofenadine but not desloratadine. Clin Pharmacokinet 2002; 41(4): 311–8
Acknowledgements
Funding for the preparation of this review was provided by Schering Plough Corporation. The author would Like to thank Steve Hill and Meera Nathan for their assistance in the drafting of this review. Steve Hill is a Medical Writer with Thomson Gardiner-Caldwell London and Meera Nathan is a Medical Writer with Apothecom.
The author has not received income from patents, royalties or stocks, or received any other financial or material gains, that are directly related to the subject matter of this review. The author has received research grants from and been involved with the advisory boards and speaking bureaus of the following companies: Altana, Aventis, Sepracor, Merck, Pfizer, Schering, Novartis, Genentech, AstraZeneca, Inspire, Alcon, MedPointe, GlaxoSmithKline and Fujisawa.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Berger, W.E. The Safety and Efficacy of Desloratadine for the Management of Allergic Disease. Drug-Safety 28, 1101–1118 (2005). https://doi.org/10.2165/00002018-200528120-00005
Published:
Issue Date:
DOI: https://doi.org/10.2165/00002018-200528120-00005