Abstract
Background
Bilateral breast cancer (BBC) may present as synchronous (SBC) or metachronous breast cancer (MBC). Optimal surgical management of BBC patients is not well-defined. In this study, we report on histopathology, treatment, and outcomes in BBC patients.
Methods
Upon Institutional Review Board approval, we identified BBC patients diagnosed and treated for invasive breast cancer between 1999 and 2007. Retrospective chart review for demographics, histopathology, treatment, and outcomes was performed, and factors associated with BCS choice were collected. Contraindication to BCS was defined as any of the following one-breast findings: multicentric disease, tumor considered too large for BCS, and a patient without a nominal breast size for acceptable cosmetic results. McNemar’s test for matched pairs (binary variables) or the paired t test (continuous variables) were used to examine if a pathologic characteristic differed within a cancer pair. Kaplan–Meier methods estimated overall survival (OS).
Results
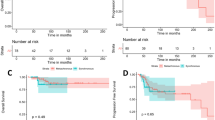
A total of 203 BBC patients (119 SBC, 84 MBC) comprised our study group. Histopathologic characteristics of the first and second cancers diagnosed in both the SBC and MBC patients were very similar in histologic type and molecular profiles. Overall, 57 % of MBC patients underwent breast-conserving surgery (BCS) at initial diagnosis versus 34 % of patients with SBC. BCS contraindications were similar in both groups: 16 (34 %) MBC patients and 28 (36 %) SBC patients. Kaplan–Meier OS estimates at 5 and 10 years were 86 and 78 % for MBC, and 87 and 77 % for SBC patients, respectively.
Conclusions
OS was excellent for both the MBC and SBC groups. Contraindications to BCS did not differ between groups. However, patients with SBC were less likely to undergo BCS compared with patients with MBC at the time of initial diagnosis.

Similar content being viewed by others
References
Lu W, Schaapveld M, Jansen L, et al. The value of surveillance mammography of the contralateral breast in patients with a history of breast cancer. Eur J Cancer. 2009;45(17):3000–7.
Schmid SM, Pfefferkorn C, Myrick ME, et al. Prognosis of early-stage synchronous bilateral invasive breast cancer. Eur J Surg Oncol. 2011;37(7):623–8.
Samant RS, Olivotto IA, Jackson JS, et al. Diagnosis of metachronous contralateral breast cancer. Breast J. 2001;7(6):405–10.
Diaz R, Munarriz B, Santaballa A, et al. Synchronous and metachronous bilateral breast cancer: a long-term single-institution experience. Med Oncol. 2012;29(1):16–24.
Heron DE, Komarnicky LT, Hyslop T, et al. Bilateral breast carcinoma: risk factors and outcomes for patients with synchronous and metachronous disease. Cancer. 2000;88(12):2739–50.
Kheirelseid EA, Jumustafa H, Miller N, et al. Bilateral breast cancer: analysis of incidence, outcome, survival and disease characteristics. Breast Cancer Res Treat. 2011;126(1):131–40.
Michowitz M, Noy S, Lazebnik N, et al. Bilateral breast cancer. J Surg Oncol. 1985;30(2):109–12.
Fung MC, Schultz DJ, Solin LJ. Early-stage bilateral breast cancer treated with breast-conserving surgery and definitive irradiation: the University of Pennsylvania experience. Int J Radiat Oncol Biol Phys. 1997;38(5):959–67.
9. Jobsen JJ, van der Palen J, Ong F, et al. Synchronous, bilateral breast cancer: prognostic value and incidence. Breast. 2003;12(2):83-8.
Wapnir IL, Dignam JJ, Fisher B, et al. Long-term outcomes of invasive ipsilateral breast tumor recurrences after lumpectomy in NSABP B-17 and B-24 randomized clinical trials for DCIS. J Natl Cancer Inst. 2011;103(6):478–8.
Hartman M, Czene K, Reilly M, et al. Genetic implications of bilateral breast cancer: a population based cohort study. Lancet Oncol. 2005;6(6):377–82.
Dawson PJ, Maloney T, Gimotty P, et al. Bilateral breast cancer: one disease or two? Breast Cancer Res Treat. 1991;19(3):233–44.
Baker B, Morcos B, Daoud F, et al. Histo-biological comparative analysis of bilateral breast cancer. Med Oncol. 2013;30(4):711.
Bouganim N, Tsvetkova E, Clemons M, et al. Evolution of sites of recurrence after early breast cancer over the last 20 years: implications for patient care and future research. Breast Cancer Res Treat. 2013;139(2):603–6.
Huo D, Melkonian S, Rathouz PJ, et al. Concordance in histological and biological parameters between first and second primary breast cancers. Cancer. 2011;117(5):907–15.
Baretta Z, Olopade OI, Huo D. Heterogeneity in hormone-receptor status and survival outcomes among women with synchronous and metachronous bilateral breast cancers. Breast. 2015;24(2):131–6.
Sandberg ME, Hartman M, Klevebring D, et al. Prognostic implications of estrogen receptor pattern of both tumors in contralateral breast cancer. Breast Cancer Res Treat. 2012;134(2):793–800.
Sighoko D, Liu J, Hou N, et al. Discordance in hormone receptor status among primary, metastatic, and second primary breast cancers: biological difference or misclassification? Oncologist. 2014;19(6):592–601.
Hartman M, Czene K, Reilly M, et al. Incidence and prognosis of synchronous and metachronous bilateral breast cancer. J Clin Oncol. 2007;25(27):4210–6.
Nichol AM, Yerushalmi R, Tyldesley S, et al. A case-match study comparing unilateral with synchronous bilateral breast cancer outcomes. J Clin Oncol. 2011;29(36):4763–8.
Carmichael AR, Bendall S, Lockerbie L, et al. The long-term outcome of synchronous bilateral breast cancer is worse than metachronous or unilateral tumours. Eur J Surg Oncol. 2002;28(4):388–91.
Londero AP, Bernardi S, Bertozzi S, et al. Synchronous and metachronous breast malignancies: a cross-sectional retrospective study and review of the literature. Biomed Res Int. 2014;2014:250727.
Disclosures
Julie A. O’Brien, Alice Ho, G. Paul Wright, Michelle Stempel, Sujata Patil, Kate Krause, Monica Morrow, and Mary L. Gemignani have no disclosures to report. This study, presented in poster format at the 15th Annual Meeting of the American Society of Breast Surgeons, 30 April–4 May 2014, was funded in part by National Institutes of Health/National Cancer Institute (NIH/NCI) Cancer Center Support Grant P30 CA008748.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
O’Brien, J.A., Ho, A., Wright, G.P. et al. Breast-Conserving Surgery in Bilateral Breast Cancer. Ann Surg Oncol 22, 3389–3396 (2015). https://doi.org/10.1245/s10434-015-4746-2
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-015-4746-2