Abstract
Background
The ACOSOG Z0011 trial demonstrated that axillary dissection (ALND) is not necessary for local control or survival in women with T1/2cN0 cancer undergoing breast-conserving therapy. There is concern about applying these results to triple-negative (TN) cancers secondary to their high local-recurrence (LR) rate. We examined the frequency of lymphovascular invasion (LVI) and nodal metastases in TN cancers to determine whether ALND can be safely avoided in this subtype.
Methods
Data were obtained from a database of patients with invasive breast cancer treated at Memorial Sloan Kettering Cancer Center from January 1998 to December 2010. A total of 11,596 tumors were classifiable into clinical surrogates for molecular subtype by immunohistochemical analysis: hormone receptor (HR)+/HER2+, HR+/HER2−, HR−/HER2+, and TN (HR−/HER2−). Multivariable logistic regression analysis (MVA) was used to determine associations between clinicopathologic variables and subtype.
Results
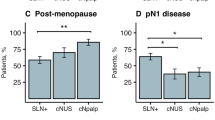
There were differences in age, tumor size, LVI, grade, and nodal involvement among groups. On MVA controlling for size, grade, and age, ER, PR, and HER2 status were significantly associated with LVI (p < 0.0001). Relative to TN tumors, HR+/HER2−, HR+/HER2+, and HR−/HER2+ tumors had higher odds of demonstrating LVI of 1.8 (odds ratio 1.8; 95 % confidence interval 1.6–2.1), 2.5 (2.5; 2.0–3.0), and 1.7 (1.7; 1.4–2.1), respectively. On MVA adjusting for size, grade, LVI, and age, TN tumors had the lowest odds of having any or high-volume nodal involvement (≥4 nodes, p < 0.0001).
Conclusions
LVI and nodal metastases were least frequent in TN cancers compared with other subtypes, despite the uniformly worse prognosis and increased LR rate in TN tumors. This suggests TN cancers spread via lymphatics less frequently than other subtypes and ALND may be avoided in TN patients meeting Z0011 eligibility criteria.
Similar content being viewed by others
References
Perou CM, Sorlie T, Eisen MB, et al. Molecular portraits of human breast tumours. Nature. 2000;406(6797):747–52.
Sorlie T, Perou CM, Tibshirani R, et al. Gene expression patterns of breast carcinomas distinguish tumor subclasses with clinical implications. Proc Natl Acad Sci USA. 2001;98:10869–74.
Sorlie T, Tibshirani R, Parker J, et al. Repeated observation of breast tumor subtypes in independent gene expression data sets. Proc Natl Acad Sci USA. 2003;100:8418–23.
Alvarenga CA, Paravidino PI, Alvarenga M, et al. Reappraisal of immunohistochemical profiling of special histological types of breast carcinomas: a study of 121 cases of eight different subtypes. J Clin Pathol. 2012;65:1066–71.
Carey LA, Perou CM, Livasy CA, et al. Race, breast cancer subtypes, and survival in the Carolina Breast Cancer Study. JAMA. 2006;295:2492–502.
Harvey JM, Clark GM, Osborne CK, et al. Estrogen receptor status by immunohistochemistry is superior to the ligand-binding assay for predicting response to adjuvant endocrine therapy in breast cancer. J Clin Oncol. 1999;17:1474–81.
Kraeima J, Siesling S, Vliegen IM, et al. Individual risk profiling for breast cancer recurrence: towards tailored follow-up schemes. Br J Cancer. 2013;109:866–71.
Nguyen PL, Taghian AG, Katz MS, et al. Breast cancer subtype approximated by estrogen receptor, progesterone receptor, and HER-2 is associated with local and distant recurrence after breast-conserving therapy. J Clin Oncol. 2008;26:2373–8.
Lowery AJ, Kell MR, Glynn RW, et al. Locoregional recurrence after breast cancer surgery: a systematic review by receptor phenotype. Breast Cancer Res Treat. 2012;133:831–41.
Metzger-Filho O, Sun Z, Viale G, et al. Patterns of Recurrence and outcome according to breast cancer subtypes in lymph node-negative disease: results from international breast cancer study group trials VIII and IX. J Clin Oncol. 2013;31:3083–90.
Romond EH, Perez EA, Bryant J, et al. Trastuzumab plus adjuvant chemotherapy for operable HER2-positive breast cancer. N Engl J Med. 2005;353:1673–84.
Giuliano AE, Hunt KK, Ballman KV, et al. Axillary dissection vs no axillary dissection in women with invasive breast cancer and sentinel node metastasis: a randomized clinical trial. JAMA. 2011;305:569–75.
Giuliano AE, McCall L, Beitsch P, et al. Locoregional recurrence after sentinel lymph node dissection with or without axillary dissection in patients with sentinel lymph node metastases: the American College of Surgeons Oncology Group Z0011 randomized trial. Ann Surg. 2010;252:426–32.
Wiechmann L, Sampson M, Stempel M, et al. Presenting features of breast cancer differ by molecular subtype. Ann Surg Oncol. 2009;16:2705–10.
Crabb SJ, Cheang MC, Leung S, et al. Basal breast cancer molecular subtype predicts for lower incidence of axillary lymph node metastases in primary breast cancer. Clin Breast Cancer. 2008;8:249–56.
Dent R, Trudeau M, Pritchard KI, et al. Triple-negative breast cancer: clinical features and patterns of recurrence. Clin Cancer Res. 2007;13(15 Pt 1):4429–34.
Voduc KD, Cheang MC, Tyldesley S, et al. Breast cancer subtypes and the risk of local and regional relapse. J Clin Oncol. 2010;28:1684–91.
Kyndi M, Sorensen FB, Knudsen H, et al. Estrogen receptor, progesterone receptor, HER-2, and response to postmastectomy radiotherapy in high-risk breast cancer: the Danish Breast Cancer Cooperative Group. J Clin Oncol. 2008;26:1419–26.
Giuliano AE, Hawes D, Ballman KV, et al. Association of occult metastases in sentinel lymph nodes and bone marrow with survival among women with early-stage invasive breast cancer. JAMA. 2011;306:385–93.
Dengel LT, Van Zee KJ, King TA, et al. Axillary dissection can be avoided in the majority of clinically node-negative patients undergoing breast-conserving therapy. Ann Surg Oncol. 2014;21:22–7.
Grills IS, Kestin LL, Goldstein N, et al. Risk factors for regional nodal failure after breast-conserving therapy: regional nodal irradiation reduces rate of axillary failure in patients with four or more positive lymph nodes. Int J Radiat Oncol Biol Phys. 2003;56:658–70.
Yates L, Kirby A, Crichton S, et al. Risk factors for regional nodal relapse in breast cancer patients with one to three positive axillary nodes. Int J Radiat Oncol Biol Phys. 2012;82:2093–103.
Barth A, Craig PH, Silverstein MJ. Predictors of axillary lymph node metastases in patients with T1 breast carcinoma. Cancer. 1997;79:1918–22.
Gajdos C, Tartter PI, Bleiweiss IJ. Lymphatic invasion, tumor size, and age are independent predictors of axillary lymph node metastases in women with T1 breast cancers. Ann Surg. 1999;230:692–6.
Greer LT, Rosman M, Charles Mylander W, et al. A prediction model for the presence of axillary lymph node involvement in women with invasive breast cancer: a focus on older women. Breast J. 2014. doi:10.1111/tbj.12233.
Olivotto IA, Jackson JS, Mates D, et al. Prediction of axillary lymph node involvement of women with invasive breast carcinoma: a multivariate analysis. Cancer. 1998;83:948–55.
Viale G, Zurrida S, Maiorano E, et al. Predicting the status of axillary sentinel lymph nodes in 4351 patients with invasive breast carcinoma treated in a single institution. Cancer. 2005;103:492–500.
Abdulkarim BS, Cuartero J, Hanson J, et al. Increased risk of locoregional recurrence for women with T1–2N0 triple-negative breast cancer treated with modified radical mastectomy without adjuvant radiation therapy compared with breast-conserving therapy. J Clin Oncol. 2011;29:2852–8.
Kim RG, Kim EK, Kim HA, et al. Prognostic significance of molecular subtype in T1N0M0 breast cancer: Korean experience. Eur J Surg Oncol. 2011;37:629–34.
Lin PH, Yeh MH, Liu LC, et al. Clinical and pathologic risk factors of tumor recurrence in patients with node-negative early breast cancer after mastectomy. J Surg Oncol. 2013;108:352–7.
Kiess AP, McArthur HL, Mahoney K, et al. Adjuvant trastuzumab reduces locoregional recurrence in women who receive breast-conservation therapy for lymph node-negative, human epidermal growth factor receptor 2–positive breast cancer. Cancer. 2012;118:1982–8.
Lanning RM, Riaz N, Morrow M, et al. Effect of adjuvant trastuzumab on locoregional recurrence in human epidermal growth factor receptor 2-positive breast cancer treated with post-mastectomy radiation therapy. J Clin Oncol. 2013;31(suppl 26):61.
Clarke M, Collins R, Darby S, et al. Effects of radiotherapy and of differences in the extent of surgery for early breast cancer on local recurrence and 15-year survival: an overview of the randomised trials. Lancet. 2005;366(9503):2087–106.
Mannino M, Yarnold JR. Local relapse rates are falling after breast conserving surgery and systemic therapy for early breast cancer: can radiotherapy ever be safely withheld? Radiother Oncol. 2009;90:14–22.
Pilewskie M, Olcese C, Eaton A, et al. Perioperative breast MRI is not associated with lower locoregional recurrence rates in DCIS patients treated with or without radiation. Ann Surg Oncol. 2014. doi:10.1245/s10434-013-3424-5.
Adkins FC, Gonzalez-Angulo AM, Lei X, et al. Triple-negative breast cancer is not a contraindication for breast conservation. Ann Surg Oncol. 2011;18:3164–73.
Zumsteg ZS, Morrow M, Arnold B, et al. Breast-conserving therapy achieves locoregional outcomes comparable to mastectomy in women with T1–2N0 triple-negative breast cancer. Ann Surg Oncol. 2013;20:3469–76.
McCarty KS Jr, Miller LS, Cox EB, et al. Estrogen receptor analyses. Correlation of biochemical and immunohistochemical methods using monoclonal antireceptor antibodies. Arch Pathol Lab Med. 1985;109:716–21.
Taylor CR, Levenson RM. Quantification of immunohistochemistry—issues concerning methods, utility and semiquantitative assessment II. Histopathology. 2006;49:411–24.
Acknowledgment
Supported in part through NIH/NCI Cancer Center Support Grant P30CA008748 and the Breast Cancer Alliance.
Disclosure
The authors declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ugras, S., Stempel, M., Patil, S. et al. Estrogen Receptor, Progesterone Receptor, and HER2 Status Predict Lymphovascular Invasion and Lymph Node Involvement. Ann Surg Oncol 21, 3780–3786 (2014). https://doi.org/10.1245/s10434-014-3851-y
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-014-3851-y