Abstract
Objective
We investigated the relation between response to neoadjuvant chemotherapy and overall survival (OS) in patients with colorectal liver metastases (CLM).
Background
It has previously been reported that patients with synchronous CLM whose disease progresses while receiving neoadjuvant chemotherapy or who do not receive neoadjuvant chemotherapy experience worse survival than patients whose disease responds to neoadjuvant chemotherapy.
Methods
By means of a prospectively maintained surgical database, between 1995 and 2003, we identified 111 patients with a synchronous CLM who received neoadjuvant chemotherapy before hepatic resection. The disease of all 111 patients was deemed resectable, and patients underwent hepatic resection with curative intent.
Results
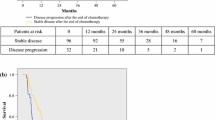
The median OS after liver resection was 62 months, with a median follow-up of 63 months. Median OS was similar between the three study groups classified by response to neoadjuvant chemotherapy (complete or partial response, 58 months; stable disease, 65 months; and disease progression, 61 months; P = .98). By univariate analysis, carcinoembryonic antigen level after liver resection of <5 ng/dL, size of metastatic lesion of ≤5 cm, lymph node–negative primary tumor, and disease-negative margins were associated with improved survival. Patients in the disease progression group had more positive margins and metastases >5 cm in size than patients in the complete or partial response group and the stable disease group. Patients whose tumor progressed but who received postoperative hepatic arterial infusion had a trend toward improved survival compared with those who did not receive hepatic arterial infusion (70% vs. 50% at 3 years, permutation log rank test P = .12).
Conclusions
Response to neoadjuvant chemotherapy did not correlate with OS even after controlling for margins, stage of primary tumor, and postoperative carcinoembryonic antigen level. Postoperative salvage treatment may have helped the survival of some patients.


Similar content being viewed by others
Reference
Fong Y, Fortner J, Sun RL, Brennan MF, Blumgart LH. Clinical score for predicting recurrence after hepatic resection for metastatic colorectal cancer: analysis of 1001 consecutive cases. Ann Surg. 1999;230:309–18.
Beckurts KT, Hölscher AH, Thorban S, Bollschweiler E, Siewert JR. Significance of lymph node involvement at the hepatic hilum in the resection of colorectal liver metastases. Br J Surg. 1997;84:1081–4.
Gayowski TJ, Iwatsuki S, Madariaga JR, et al. Experience in hepatic resection for metastatic colorectal cancer: analysis of clinical and pathologic risk factors. Surgery. 1994;703–10.
Minagawa M, Yamamoto J, Miwa S, et al. Selection criteria for simultaneous resection in patients with synchronous liver metastasis. Arch Surg 2006;141:1006–12.
Nordlinger B, Guiguet M, Vaillant JC, et al. Surgical resection of colorectal carcinoma metastases to the liver. A prognostic scoring system to improve case selection, based on 1568 patients. Association Francaise de Chirurgie. Cancer. 1996;77:1254–62.
Scheele J, Altendorf-Hofmann A. Resection of colorectal liver metastases. Langenbecks Arch Surg 1999;384:313–27.
Bengtsson G, Carlsson G, Hafström L, Jönsson PE. Natural history of patients with untreated liver metastases from colorectal cancer. Am J Surg 1981;141:586–9.
Tomlinson JS, Jarnagin WR, DeMatteo RP, et al. Actual 10-year survival after resection of colorectal liver metastases defines cure. J Clin Oncol 2007;25:4575–80.
Choti MA, Sitzmann JV, Tiburi MF, et al. Trends in long-term survival following liver resection for hepatic colorectal metastases. Ann Surg 2002;235:759–66.
Abdalla EK, Adam R, Bilchik AJ, Jaeck D, Vauthey JN, Mahvi D. Improving resectability of hepatic colorectal metastases: expert consensus statement. Ann Surg Oncol. 2006;13:1271–80.
Stangl R, Altendorf-Hofmann A, Charnley RM, Scheele J. Factors influencing the natural history of colorectal liver metastases. Lancet. 1994;343(8910):1405–10.
Sugihara K, Hojo K, Moriya Y, Yamasaki S, Kosuge T, Takayama T. Pattern of recurrence after hepatic resection for colorectal metastases. Br J Surg. 1993;80:1032–5.
Adam R, Bismuth H, Castaing D, et al. Repeat hepatectomy for colorectal liver metastases. Ann Surg. 1997;225:51–60.
Harmon KE, Ryan JA Jr, Biehl TR, Lee FT. Benefits and safety of hepatic resection for colorectal metastases. Am J Surg. 1999;177:402–4.
Schindl M, Wigmore SJ, Currie EJ, Laengle F, Garden OJ. Prognostic scoring in colorectal cancer liver metastases: development and validation. Arch Surg. 2005;140:183–9.
Petrelli NJ, Nambisan RN, Herrera L, Mittelman A. Hepatic resection for isolated metastasis from colorectal carcinoma. Am J Surg. 1985;149:205–9.
Schlag P, Hohenberger P, Herfarth C. Resection of liver metastases in colorectal cancer—competitive analysis of treatment results in synchronous versus metachronous metastases. Eur J Surg Oncol. 1990;16:360–5.
Tsai MS, Su YH, Ho MC, Liang JT, Chen TP, Lai HS, Lee PH. Clinicopathological features and prognosis in resectable synchronous and metachronous colorectal liver metastases. Ann Surg Oncol. 2007;14:786–94.
Folprecht G, Grothey A, Alberts S, Raab HR, Köhne CH. Neoadjuvant treatment of unresectable colorectal liver metastases: correlation between tumour response and resection rates. Ann Oncol. 2005;16:1311–9.
Adam R, Pascal G, Castaing D, et al. Tumor progression while on chemotherapy: a contraindication to liver resection for multiple colorectal metastases? Ann Surg. 2004;240:1052–61.
Allen PJ, Kemeny N, Jarnagin W, DeMatteo R, Blumgart L, Fong Y. Importance of response to neoadjuvant chemotherapy in patients undergoing resection of synchronous colorectal liver metastases. J Gastrointest Surg. 2003;7:109–15.
Heller G, Venkatraman ES. Resampling procedures to compare two survival distributions in the presence of right-censored data. Biometrics. 1996;52(4):1204–13.
Adam R, Delvart V, Pascal G, et al. Rescue surgery for unresectable colorectal liver metastases downstaged by chemotherapy: a model to predict long-term survival. Ann Surg. 2004;240:644–57.
Cummings LC, Payes JD, Cooper GS, Survival after hepatic resection in metastatic colorectal cancer: a population-based study. Cancer. 2007;109:718–26.
Iwatsuki S, Dvorchik I, Madariaga JR, et al. Hepatic resection for metastatic colorectal adenocarcinoma: a proposal of a prognostic scoring system. J Am Coll Surg. 1999;189:291–9.
Lise M, Bacchetti S, Da Pian P, Nitti D, Pilati P. Patterns of recurrence after resection of colorectal liver metastases: prediction by models of outcome analysis. World J Surg. 2001;25:638–44.
Ueno H, Mochizuki H, Hashiguchi Y, Hase K. Prognostic determinants of patients with lateral nodal involvement by rectal cancer. Ann Surg. 2001;234:190–7.
Portier G, Elias D, Bouche O, et al. Multicenter randomized trial of adjuvant fluorouracil and folinic acid compared with surgery alone after resection of colorectal liver metastases: FFCD ACHBTH AURC 9002 trial. J Clin Oncol. 2006;24:4976–82.
Parks R, Gonen M, Kemeny N, et al. Adjuvant chemotherapy improves survival after resection of hepatic colorectal metastases: analysis of data from two continents. J Am Coll Surg. 2007;204:753–61.
Tanaka K, Shimada H, Ueda M, Matsuo K, Endo I, Togo S. Role of hepatectomy in treating multiple bilobar colorectal cancer metastases. Surgery 2008;143:259–70.
Nordlinger B, Sorbye H, Collette L, et al. Final results of the EORTC Intergroup randomized phase III study 40983 [EPOC] evaluating the benefit of peri-operative FOLFOX4 chemotherapy for patients with potentially resectable colorectal cancer liver metastases. J Clin Oncol 2007;25(18S):LBA5.
Mitry E, Fields AL, Bleiberg H, et al. Adjuvant chemotherapy after potentially curative resection of metastases from colorectal cancer: a pooled analysis of two randomized trials. J Clin Oncol. 2008;26:4906–11.
Petrelli NJ. Perioperative or adjuvant therapy for resectable colorectal hepatic metastases. J Clin Oncol. 2008;26:4862–3.
Reddy SK, Morse MA, Hurwitz HI, et al. Addition of bevacizumab to irinotecan- and oxaliplatin-based preoperative chemotherapy regimens does not increase morbidity after resection of colorectal liver metastases. J Am Coll Surg. 2008;206:96–106.
Falcone A, Ricci S, Brunetti I, et al, Gruppo Oncologico Nord Ovest. Phase III trial of infusional fluorouracil, leucovorin, oxaliplatin, and irinotecan (FOLFOXIRI) compared with infusional fluorouracil, leucovorin, and irinotecan (FOLFIRI) as first-line treatment for metastatic colorectal cancer: the Gruppo Oncologico Nord Ovest. J Clin Oncol 2007;25:1670–6.
Giantonio BJ, Catalano PJ, Meropol NJ, et al. Eastern Cooperative Oncology Group Study E3200 Bevacizumab in combination with oxaliplatin, fluorouracil, and leucovorin (FOLFOX4) for previously treated metastatic colorectal cancer: results from the Eastern Cooperative Oncology Group Study E3200. J Clin Oncol 2007;25:1539–44.
Sobrero AF, Maurel J, Fehrenbacher L, et al. EPIC: phase III trial of cetuximab plus irinotecan after fluoropyrimidine and oxaliplatin failure in patients with metastatic colorectal cancer. J Clin Oncol 2008;26:2311–9.
Acknowledgments
We thank Dr. Rebecca White and Tracy Mak for their help in gathering data for this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gallagher, D.J., Zheng, J., Capanu, M. et al. Response to Neoadjuvant Chemotherapy Does Not Predict Overall Survival for Patients With Synchronous Colorectal Hepatic Metastases. Ann Surg Oncol 16, 1844–1851 (2009). https://doi.org/10.1245/s10434-009-0348-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-009-0348-1