Abstract
Background
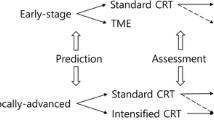
Locally advanced rectal cancer is frequently treated with neoadjuvant chemoradiotherapy to reduce local recurrence and possibly improve survival. The tumor response to chemoradiotherapy is variable and may influence the prognosis after surgery. This study assessed tumor regression and its influence on survival in patients with rectal cancer treated with chemoradiotherapy followed by curative surgery.
Methods
One hundred twenty-six patients with locally advanced rectal cancer (T3/T4 or N1/N2) were treated with chemoradiotherapy followed by total mesorectal excision. Patients received long-course radiotherapy (50 Gy in 25 fractions) in combination with 5-flourouracil over 5 weeks. By means of a standardized approach, tumor regression was graded in the resection specimen using a 3-point system related to tumor regression grade (TRG): complete or near-complete response (TRG1), partial response (TRG2), or no response (TRG3).
Results
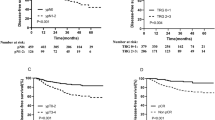
The 5-year disease-free survival was 72% (median follow-up 37 months), and 7% of patients had local recurrence. Chemoradiotherapy produced downstaging in 60% of patients; 21% of patients experienced TRG1. TRG1 correlated with a pathological T0/1 or N0 status. Five-year disease-free survival after chemoradiotherapy and surgery was significantly better in TRG1 patients (100%) compared with TRG2 (71%) and TRG3 (66%) (P = .01).
Conclusion
Tumor regression grade measured on a 3-point system predicts outcome after chemoradiotherapy and surgery for locally advanced rectal cancer.



Similar content being viewed by others
References
Jemal A, Siegel R, Ward E, et al. Cancer statistics, 2006. CA Cancer J Clin 2006; 56:106–30.
Cancer Facts and Figures 2002. Atlanta, GA: American Cancer Society
Adam IJ, Mohamdee MO, Martin IG, et al. Role of circumferential margin involvement in the local recurrence of rectal cancer. Lancet 1994; 344:707–11.
Quirke P, Durdey, Dixon MF, et al. Local recurrence of rectal adenocarcinoma due to inadequate surgical resection. Histopathological study of lateral tumour spread and surgical excision. Lancet 1986; 1:996–8
Balslev I, Pedersen M, Teglbjaerg PS, et al. Postoperative radiotherapy in Dukes B and C carcinoma of rectum and recto-sigmoid. A randomized multicenter study. Cancer 1986; 58:22–8.
Heald RJ, Ryall RDH. Recurrence and survival after total mesorectal excision for rectal cancer. Lancet 1986; 28:1479–82.
Glimelius B. Radiotherapy in rectal cancer. Br Med Bull 2002; 64:141–57.
Gerald A, Buyse M, Nordlinger B, et al. Preoperative radiotherapy as adjuvant treatment in rectal cancer. Final results of a randomized study of the European Organisation for Research and Treatment of Cancer (EORTC). Ann Surg 1988; 208:606–14.
Stockholm Colorectal Cancer Study Group. Preoperative short-term radiation therapy in operable rectal carcinoma. A prospective randomized trial. Cancer 1990; 66:49–55.
Stockholm Colorectal Cancer Study Group. Randomized study on preoperative radiotherapy in rectal carcinoma. Ann Surg Oncol 1996; 3:423–30.
Swedish Rectal Cancer Trial. Improved survival with preoperative radiotherapy in resectable rectal cancer. N Engl J Med 1997; 336:980–7.
Guillem J, Chessin D, Cohen A, et al. Long-term oncologic outcome following preoperative combined modality therapy and total mesorectal excision of locally advanced rectal cancer. Ann Surg 2005; 241:829–38.
Osti MF, Valeriani M, Masoni L, et al. Neoadjuvant chemoradiation for locally advanced carcinoma of the rectum. Tumori 2004; 90:303–9.
Wheeler JM, Warren BF, Mortensen NJ, et al. Quantification of histological regression of rectal cancer after irradiation: a proposal for a modified staging system. Dis Colon Rectum 2002; 45:1051–6.
Habr-Gama A, de Souza PM, Ribeiro U Jr, et al. Low rectal cancer: impact of radiation and chemotherapy on surgical treatment. Dis Colon Rectum 1998; 41:1087–96.
Hiotis SP, Weber SM, Cohen AM, et al. Assessing the predictive value of clinical complete response to neoadjuvant therapy for rectal cancer: an analysis of 488 patients. J Am Coll Surg 2002; 194:131–5.
Mandard AM, Dalibard F, Mandard JC et al. Pathologic assessment of tumour regression after preoperative chemoradiotherapy of oesophageal carcinoma. Clinicopathologic correlations. Cancer 1994; 73:2680–6.
Ryan R, Gibbons D, Hyland JMP, et al. Pathological response following long-course neo-adjuvant chemoradiotherapy for locally advanced rectal cancer. Histopathology 2005; 47:141–6.
Wang LM, Sheahan K. Pathological assessment of post-treatment gastrointestinal and hepatic resection specimens. Curr Diag Pathol 2007; 13:222–31.
Dworak O, Keilholz L, Hoffmann A. Pathological features of rectal cancer after preoperative radiochemotherapy. Int J Colorectal Dis 1997; 12:19–23.
Bouzorenne H, Bosman FT, Seelentag W, et al. Importance of tumour regression assessment in predicting the outcome in patients with locally advanced rectal carcinoma who is treated with preoperative radiotherapy. Cancer 2002; 94:1121–30.
Suarez J, Vera R, Balen E, et al. Pathologic response assessed by Mandard grade is a better prognostic factor than down staging for disease-free survival after preoperative radiochemotherapy for advanced rectal cancer. Colorectal Dis 2007; 10:563–8.
Kuo LJ, Liu MC, Jian J, et al. Is final TNM staging a predictor for survival in locally advanced rectal cancer after preoperative chemoradiation therapy? Ann Surg Oncol 2007; 14:2766–72.
Quah HM, Chou JF, Gonen M, et al. Pathologic stage is most prognostic of disease-free survival in locally advanced rectal cancer patients after preoperative chemoradiation. Cancer 2008; 113:57–64.
Capirci C, Valentini V, Cionini L, et al. Prognostic value of pathologic complete response after neoadjuvant therapy in locally advanced rectal cancer: long term analysis of 566 ypCR patients. Int J Radiat Oncol Biol Phys 2008; 72:99–107.
Habr-Gama A, Perez RO, Nadalin W, et al. Operative versus nonoperative treatment for stage 0 distal cancer following chemoradiation therapy- long term results. Ann Surg 2004; 240:711–7.
Capirci C, Rubello D, Chierichetti F, et al. Restaging after neoadjuvant chemoradiotherapy for rectal adenocarcinoma: role of F18-FDG PET. Biomed Pharmacother 2004; 58:451–7.
Stipa F, Zernecke A, Moore HG, et al. Residual mesorectal lymph node involvement following neo-adjuvant combined modality therapy: rationale for radical resection? Ann Surg Oncol 2004; 11:187–91.
Hughes R, Glynne-Jones R, Grainger J, et al. Can pathological response in the primary tumour following pre-operative pelvic chemoradiotherapy for T3-T4 rectal cancer predict for sterilisation of pelvic lymph nodes, a low risk of recurrence and the appropriateness of local excision? Int J Colorectal Dis 2006; 21:11–7.
Lindebjerg J, Garm Spindler K, Ploen J, et al. The prognostic value of lymph node metastases and tumour regression grade in rectal cancer patients treated with long-course preoperative chemoradiotherapy. Colorectal Dis (in press). doi:10.1111/j.1463-1318.2008.01599.x
Birgisson H, Pahlman L, Gunnarson U, et al. Adverse effects of preoperative radiation therapy for rectal cancer: long term follow-up of the Swedish Rectal Cancer Trial. J Clin Oncol 2005; 23:8697–705.
Swedish Rectal Cancer Trial. Preoperative irradiation followed by surgery vs. surgery alone in respectable rectal carcinoma- postoperative morbidity and mortality in a Swedish multicentre trial. Br J Surg 1993; 80:1333–6.
Kapiteijn E, Marijnen CAM, Nagtegaal ID. Preoperative radiotherapy in combination with total mesorectal excision improves local control in resectable rectal cancer. Report from a multicentre randomised trial. For the Dutch Colorectal Cancer Group and other cooperative investigators. N Engl J Med 2001; 345:638–46.
Marijinen CA, van de Velde CJ, Putter H, et al. Impact of short term preoperative radiotherapy on health-related quality of life and sexual functioning in primary rectal cancer: report of a multicenter randomised trial. J Clin Oncol 2005; 23:1847–58.
Baxter N, Hartman LK, Tepper JE, et al. Postoperative irradiation for rectal cancer increases the risk of small bowel obstruction after surgery. Ann Surg 2007; 245:553–9.
Pollack J, Holm T, Cedermark B, et al. Late adverse effects of short-course preoperative radiotherapy in rectal cancer. Br J Surg 2006; 93:1519–25.
Kobayashi H, Hashiguchi Y, Ueno H, et al. Absence of cyclooxygenase-2 protein expression is a predictor of tumour regression in rectal cancer treated with preoperative short-term chemoradiotherapy. Dis Colon Rectum 2007; 50:1354–62.
Willet CG, Hagan M, Daley W, et al. Changes in tumour proliferation of rectal cancer induced by preoperative 5-fluorouracil and irradiation. Dis Colon Rectum 1998; 41:62–7.
Bertolini F, Bengala C, Losi L, et al. Prognostic and predictive value of baseline and post treatment molecular marker expression in locally advanced rectal cancer treated with neoadjuvant chemoradiotherapy. Int J Radiat Oncol Biol Phys 2007; 68:1455–61.
Smith FM, Gallagher WM, Fox E, et al. Combination of SELDI-TOF-MS and data mining provides early-stage response prediction for rectal tumours undergoing multimodal neoadjuvant therapy. Ann Surg 2007; 245:259–66.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Beddy, D., Hyland, J.M.P., Winter, D.C. et al. A Simplified Tumor Regression Grade Correlates with Survival in Locally Advanced Rectal Carcinoma Treated with Neoadjuvant Chemoradiotherapy. Ann Surg Oncol 15, 3471–3477 (2008). https://doi.org/10.1245/s10434-008-0149-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-008-0149-y