Abstract
Background
The purpose of this article was to determine the impact of time to undetectable prostate-specific antigen (PSA) for predicting biochemical recurrence (BCR) in patients with a positive surgical margin (PSM) following radical prostatectomy (RP). A PSM is an independent predictor of BCR; however, not all patients develop BCR later on.
Methods
A retrospective analysis was conducted on 1,117 consecutive prostate cancer patients who underwent RP without neoadjuvant or adjuvant therapy from July 2005 to December 2009. Of these, 516 (46.2 %) patients without PSMs, and 214 (19.2 %) patients with PSMs who later achieved undetectable PSA, defined as <0.01 ng/ml, were identified. Patients with PSMs were stratified according to time to undetectable PSA dichotomized at 6 weeks and compared with patients without PSMs. Patients with PSMs who did not achieve undetectable PSA were excluded. BCR was defined as two consecutive increases of post-undetectable PSA ≥0.2 ng/ml.
Results
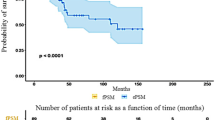
During the median follow-up of 58.2 months, patients with PSMs who achieved undetectable PSA in <6 weeks had comparable 5-year BCR-free survival rates to those without PSMs; however, patients with PSMs who achieved undetectable PSA in ≥6 weeks showed significantly lower rates compared with both patients without PSMs (59.2 vs 74.3 %; p < 0.001) and patients with PSMs who achieved undetectable PSA in <6 weeks (59.2 vs 78.8 %; p = 0.004). Among patients with PSMs, multivariate analysis revealed time to undetectable PSA at ≥6 weeks and seminal vesicle invasion to be independent predictors of BCR. No perioperative factors were associated with undetectable PSA at ≥6 weeks.
Conclusions
Patients with PSMs who achieve undetectable PSA in <6 weeks show comparable risks of BCR to patients with negative surgical margins.

Similar content being viewed by others
References
Ko J, Falzarano SM, Walker E, Streator Smith K, Stephenson AJ, Klein EA, et al. Prostate cancer patients older than 70 years treated by radical prostatectomy have higher biochemical recurrence rate than their matched younger counterpart. Prostate. 2013;73:897–903.
Bivalacqua TJ, Pierorazio PM, Su LM. Open, laparoscopic and robotic radical prostatectomy: optimizing the surgical approach. Surg Oncol. 2009;18:233–41.
Nakamura M, Hasumi H, Miyoshi Y, Sugiura S, Fujinami K, Yao M, et al. Usefulness of ultrasensitive prostate-specific antigen assay for early detection of biochemical failure after radical prostatectomy. Int J Urol. 2005;12:1050–4.
Briganti A, Wiegel T, Joniau S, Cozzarini C, Bianchi M, Sun M, et al. Early salvage radiation therapy does not compromise cancer control in patients with pT3N0 prostate cancer after radical prostatectomy: results of a match-controlled multi-institutional analysis. Eur Urol. 2012;62:472–87.
Shinghal R, Yemoto C, McNeal JE, Brooks JD. Biochemical recurrence without PSA progression characterizes a subset of patients after radical prostatectomy. Prostate-specific antigen. Urology. 2003;61:380–5.
Doherty AP, Bower M, Smith GL, Miano R, Mannion EM, Mitchell H, et al. Undetectable ultrasensitive PSA after radical prostatectomy for prostate cancer predicts relapse-free survival. Br J Cancer. 2000;83:1432–6.
Cooperberg MR, Hilton JF, Carroll PR. The CAPRA-S score: A straightforward tool for improved prediction of outcomes after radical prostatectomy. Cancer. 2011;117:5039–46.
Ploussard G, Staerman F, Pierrevelcin J, Saad R, Beauval JB, Roupret M, et al. Predictive factors of oncologic outcomes in patients who do not achieve undetectable prostate specific antigen after radical prostatectomy. J Urol. 2013;190:1750–6.
American Joint Committee on Cancer (AJC) (2010) Prostate In: Edge SB, Byrd , Compton CC, Fritz AG, Greene FL, Trotti A (Eds.) AJCC cancer staging manual 7. Springer, New York pp 457–468.
Hoedemaeker RF, Ruijter ETG, Ruizeveld-de Winter JA, van der Kaa CA, van der Kwast TH. The Biomed II MPC Study group. Processing radical prostatectomy specimens. J Urol Pathol. 1998;9:211–22.
Eisenberg ML, Davies BJ, Cooperberg MR, Cowan JE, Carroll PR. Prognostic implications of an undetectable ultrasensitive prostate-specific antigen level after radical prostatectomy. Eur Urol. 2010;57:622–9.
Shen S, Lepor H, Yaffee R, Taneja SS. Ultrasensitive serum prostate specific antigen nadir accurately predicts the risk of early relapse after radical prostatectomy. J Urol. 2005;173:777–80.
Huang SP, Bao BY, Wu MT, Choueiri TK, Goggins WB, Huang CY, et al. Impact of prostate-specific antigen (PSA) nadir and time to PSA nadir on disease progression in prostate cancer treated with androgen-deprivation therapy. Prostate. 2011;71:1189–97.
Choueiri TK, Xie W, D’Amico AV, Ross RW, Hu JC, Pomerantz M, et al. Time to prostate-specific antigen nadir independently predicts overall survival in patients who have metastatic hormone-sensitive prostate cancer treated with androgen-deprivation therapy. Cancer. 2009;115:981–7.
Cookson MS, Aus G, Burnett AL, Canby-Hagino ED, D’Amico AV, Dmochowski RR, et al. Variation in the definition of biochemical recurrence in patients treated for localized prostate cancer: the American Urological Association Prostate Guidelines for Localized Prostate Cancer Update Panel report and recommendations for a standard in the reporting of surgical outcomes. J Urol. 2007;177:540–5.
Han M, Partin AW, Pound CR, Epstein JI, Walsh PC. Long-term biochemical disease-free and cancer-specific survival following anatomic radical retropubic prostatectomy. The 15-year Johns Hopkins experience. Urol Clin North Am. 2001;28:555–65.
Swindle P, Eastham JA, Ohori M, Kattan MW, Wheeler T, Maru N, et al. Do margins matter? The prognostic significance of positive surgical margins in radical prostatectomy specimens. J Urol. 2005;174:903–7.
Siddiqui SA, Boorjian SA, Inman B, Bagniewski S, Bergstralh EJ, Blute ML. Timing of androgen deprivation therapy and its impact on survival after radical prostatectomy: a matched cohort study. J Urol. 2008;179:1830–7.
Freedland SJ, Moul JW. Prostate specific antigen recurrence after definitive therapy. J Urol. 2007;177:1985–91.
Yoshida T, Matsuzaki K, Kobayashi Y, Takeda K, Nakayama M, Arai Y, et al. Usefulness of postoperative nadir prostate-specific antigen value by ultrasensitive assay as a predictor of prostate-specific antigen relapse for pathological T3 or positive surgical margins after radical prostatectomy for prostate cancer. Int Urol Nephrol. 2012;44:479–85.
Epstein JI. Incidence and significance of positive margins in radical prostatectomy specimens. Urol Clin North Am. 1996;23:651–63.
Yossepowitch O, Briganti A, Eastham JA, Epstein J, Graefen M, Montironi R, et al. Positive surgical margins after radical prostatectomy: a systematic review and contemporary update. Eur Urol. 2014;65:303–13.
Ward JF, Blute ML, Slezak J, Bergstralh EJ, Zincke H. The long-term clinical impact of biochemical recurrence of prostate cancer 5 or more years after radical prostatectomy. J Urol. 2003;170:1872–6.
Disclosures
This work was supported by the National Research Foundation of Korea(NRF) grant funded by the Korea government (MEST) (2011-0029348).
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Koo, K.C., Tuliao, P., Komninos, C. et al. Prognostic Impact of Time to Undetectable Prostate-Specific Antigen in Patients with Positive Surgical Margins Following Radical Prostatectomy. Ann Surg Oncol 22, 693–700 (2015). https://doi.org/10.1245/s10434-014-4057-z
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-014-4057-z