Abstract
Background
Melanoma patients with lymph node (LN) metastases have variable survival after lymphadenectomy. This study investigates whether lymphadenectomy at different times in the course of disease progression influences disease-free survival (DFS; time from primary diagnosis to first recurrence after lymphadenectomy), post recurrence survival (PRS; time from first recurrence after lymphadenectomy to death), and overall survival (OS; time from diagnosis to death).
Methods
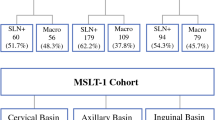
Between 1992 and 2010, a total of 1,704 patients underwent lymphadenectomy; 502 underwent immediate completion lymphadenectomy (ICL) after positive sentinel node biopsy (SNB), 214 had delayed completion lymphadenectomy (DCL) for regional recurrence after positive SNB with no ICL or after an earlier false-negative SNB, 709 had no SNB and later required delayed therapeutic lymphadenectomy (DTL) for clinically evident metastasis, and 279 had immediate therapeutic lymphadenectomy (ITL) for clinically positive LNs at primary melanoma diagnosis.
Results
Median DFS for ICL, DCL, DTL, and ITL was 68, 48, 82, and 16 months, respectively (p < 0.001). Median PRS for ICL, DCL, DTL, and ITL was 14, 8, 9, and 9 months, respectively (p < 0.001). Median OS for ICL was not reached whilst for DCL, DTL, and ITL it was 71, 101, and 29 months, respectively (p < 0.001). Extranodal spread and tumor, node, metastasis classification system N stage were the only significant prognostic factors for OS within each group. ICL patients had significantly improved DFS (p = 0.005) and OS (p = 0.012) beyond 5 years compared to DTL patients.
Conclusions
Variable outcomes after lymphadenectomy were observed with different timing of surgery and LN tumor burden. ICL patients had the best outcome.



Similar content being viewed by others
References
National Comprehensive Cancer Network. NCCN: clinical practice guidelines in oncology: melanoma.
Australian Cancer Network Melanoma Guidelines Revision Working Party. Clinical practice guidelines for the management of melanoma in Australia and New Zealand. Wellington: Cancer Council Australia and Australian Cancer Network, Sydney and New Zealand Guidelines Group; 2008.
Marsden JR, Newton-Bishop JA, Burrows L, et al. Revised UK guidelines for the management of cutaneous melanoma, 2010. Br J Dermatol. 2010;163:238–56.
Garbe C, Peris K, Hauschild A, et al. Diagnosis and treatment of melanoma: European consensus-based interdisciplinary guideline. Eur J Cancer. 2010;46:270–83.
Balch CM, Gershenwald JE, Soong SJ, et al. Multivariate analysis of prognostic factors among 2,313 patients with stage III melanoma: comparison of nodal micrometastases versus macrometastases. J Clin Oncol. 2010;28:2452–9.
Spillane AJ, Cheung BL, Stretch JR, et al. Proposed quality standards for regional lymph node dissections in patients with melanoma. Ann Surg. 2009;249:473–80.
Spillane AJ, Haydu L, McMillan W, Stretch JR, Thompson JF. Quality assurance parameters and predictors of outcome for ilioinguinal and inguinal dissection in a contemporary melanoma patient population. Ann Surg Oncol. 2011;18:2521–8.
Pasquali S, Haydu LE, Scolyer RA, et al. The importance of adequate primary tumor excision margins and sentinel node biopsy in achieving optimal locoregional control for patients with thick primary melanomas. Ann Surg. 2013;258:152–7.
Balch CM, Gershenwald JE, Soong SJ, et al. Final version of. 2009 AJCC melanoma staging and classification. J Clin Oncol. 2009;27:6199–206.
Nieto FJ, Coresh J. Adjusting survival curves for confounders: a review and a new method. Am J Epidemiol. 1996;143:1059–68.
Makuch RW. Adjusted survival curve estimation using covariates. J Chronic Dis. 1982;35:437–43.
Bradburn MJ, Clark TG, Love SB, Altman DG. Survival analysis, part III: multivariate data analysis—choosing a model and assessing its adequacy and fit. Br J Cancer. 2003;89:605–11.
Hosmer DW, Lemeshow S. Applied survival analysis: regression modeling of time to event data. 2nd edition. New York: John Wiley & Sons; 2008.
Morton DL, Thompson JF, Cochran AJ, et al. Sentinel-node biopsy or nodal observation in melanoma. N Engl J Med. 2006;355:1307–17.
Pasquali S, Mocellin S, Campana LG, et al. Early (sentinel lymph node biopsy-guided) versus delayed lymphadenectomy in melanoma patients with lymph node metastases:personal experience and literature meta-analysis. Cancer. 2010;116:1201–9.
Balch CM, Soong SJ, Gershenwald JE, et al. Prognostic factors analysis of 17,600 melanoma patients: validation of the American Joint Committee on Cancer melanoma staging system. J Clin Oncol. 2001;19:3622–34.
Eggermont AM, Robert C. New drugs in melanoma: it’s a whole new world. Eur J Cancer. 2011;47:2150–7.
Hodi FS, O’Day SJ, McDermott DF, et al. Improved survival with ipilimumab in patients with metastatic melanoma. N Engl J Med. 2010;363:711–23.
Robert C, Thomas L, Bondarenko I, et al. Ipilimumab plus dacarbazine for previously untreated metastatic melanoma. N Engl J Med. 2011;364:2517–26.
Arkenau HT, Kefford R, Long GV. Targeting BRAF for patients with melanoma. Br J Cancer. 2011;104:392–8.
Chapman PB, Hauschild A, Robert C, et al. Improved survival with vemurafenib in melanoma with BRAF V600E mutation. N Engl J Med. 2011;364:2507–16.
Kirkwood JM, Butterfield LH, Tarhini AA, Zarour H, Kalinski P, Ferrone S. Immunotherapy of cancer in 2012. CA Cancer J Clin. 2012;62:309–35.
Calabro A, Singletary SE, Balch CM. Patterns of relapse in 1001 consecutive patients with melanoma nodal metastases. Arch Surg. 1989;124:1051–5.
Dalal KM, Patel A, Brady MS, Jaques DP, Coit DG. Patterns of first-recurrence and post-recurrence survival in patients with primary cutaneous melanoma after sentinel lymph node biopsy. Ann Surg Oncol. 2007;14:1934–42.
Nathansohn N, Schachter J, Gutman H. Patterns of recurrence in patients with melanoma after radical lymph node dissection. Arch Surg. 2005;140:1172–7.
Pidhorecky I, Lee RJ, Proulx G, et al. Risk factors for nodal recurrence after lymphadenectomy for melanoma. Ann Surg Oncol. 2001;8:109–15.
Warso MA, Das Gupta TK. Melanoma recurrence in a previously dissected lymph node basin. Arch Surg. 1994;129:252–5.
White RR, Stanley WE, Johnson JL, Tyler DS, Seigler HF. Long-term survival in 2,505 patients with melanoma with regional lymph node metastasis. Ann Surg. 2002;235:879–87.
Acknowledgment
A.J.S.’s research is supported by the Friends of the Mater Foundation, North Sydney, NSW, Australia. S.P. was a research fellow at Melanoma Institute Australia and was supported by the University of Padova, Padova, Italy. J.F.T.’s research is supported by the Melanoma Foundation of the University of Sydney.
Disclosure
The authors declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Spillane, A.J., Pasquali, S., Haydu, L.E. et al. Patterns of Recurrence and Survival After Lymphadenectomy in Melanoma Patients: Clarifying the Effects of Timing of Surgery and Lymph Node Tumor Burden. Ann Surg Oncol 21, 292–299 (2014). https://doi.org/10.1245/s10434-013-3253-6
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-013-3253-6