Abstract
Purpose
To evaluate the protection of the urogenital function after robot-assisted total mesorectal excision (R-TME) for rectal cancer compared to those of laparoscopic TME (L-TME).
Methods
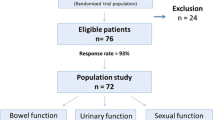
69 patients who underwent L-TME (n = 39) or R-TME (n = 30) were prospectively enrolled. Their urogenital function was evaluated by uroflowmetry, a standard questionnaire of the international prostate symptom score (IPSS) and the international index of erectile function (IIEF) before surgery and 1, 3, 6, and 12 months after surgery. The pre- and postoperative IPSS and IIEF scores were compared to detect functional deterioration by paired t test for each group. How postoperative IPSS and IIEF scores and uroflowmetry data deviated from the preoperative values (Δ) were statistically compared between the two groups.
Results
The IPSS score significantly increased 1 month after surgery; the recovery from decreased urinary function took 6 months for patients in the L-TME group (8.2 ± 6.3; P = 0.908) but 3 months in the R-TME group (8.36 ± 5.5; P = 0.075). The ΔIPSS scores were significantly different between the two groups at 3 months (P = 0.036). In male patients (L-TME 20, R-TME 18), the total IIEF score in R-TME and L-TME significantly decreased 1 month after surgery, L-TME gradually recovered over 12 months (46.00 ± 16.9; P = 0.269), but R-TME recovered within 6 months (44.61 ± 13.76; P = 0.067). The ΔIIEF score value was not significantly different at any time between the two groups, but in an itemized analysis of the change in erectile function and sexual desire, there were significant differences at 3 months between the two groups.
Conclusions
R-TME for rectal cancer is associated with earlier recovery of normal voiding and sexual function compared to patients who underwent L-TME, although this result needs to be verified by larger prospective comparative studies.





Similar content being viewed by others
References
Heald RJ, Husband EM, Ryall RD. The mesorectum in rectal cancer surgery—the clue to pelvic recurrence? Br J Surg. 1982;69:613–6.
Kim NK, Aahn TW, Park JK, et al. Assessment of sexual and voiding function after total mesorectal excision with pelvic autonomic nerve preservation in males with rectal cancer. Dis Colon Rectum. 2002;45:1178–85.
Chang PL, Fan HA. Urodynamic studies before and/or after abdominoperineal resection of the rectum for carcinoma. J Urol. 1983;130:948–51.
Santangelo ML, Romano G, Sassaroli C. Sexual function after resection for rectal cancer. Am J Surg. 1987;154:502–4.
Kinn AC, Ohman U. Bladder and sexual function after surgery for rectal cancer. Dis Colon Rectum. 1986;29:43–8.
Fazio VW, Fletcher J, Montague D. Prospective study of the effect of resection of the rectum on male sexual function. World J Surg. 1980;32 4:149–52.
Havenga K, DeRuiter MC, Enker WE, et al. Anatomical basis of autonomic nerve-preserving total mesorectal excision for rectal cancer. Br J Surg. 1996;83:384–8.
Heald RJ. The “holy plane” of rectal surgery. Royal Society of Medicine (Great Britain). J R Soc Med. 1988;81:503–8.
Masui H, Ike H, Yamaguchi S, et al. Male sexual function after autonomic nerve-preserving operation for rectal cancer. Dis Colon Rectum. 1996;39:1140–5.
Maas CP, Moriya Y, Steup WH, et al. Radical and nerve-preserving surgery for rectal cancer in The Netherlands: a prospective study on morbidity and functional outcome. Br J Surg. 1998;85:92–7.
Nesbakken A, Nygaard K, Bull-Njaa T, et al. Bladder and sexual dysfunction after mesorectal excision for rectal cancer. Br J Surg. 2000;87:206–10.
Jayne DG, Brown JM, Thorpe H, et al. Bladder and sexual function following resection for rectal cancer in a randomized clinical trial of laparoscopic versus open technique. Br J Surg. 2005;92:1124–32.
Asoglu O, Matlim T, Karanlik H, et al. Impact of laparoscopic surgery on bladder and sexual function after total mesorectal excision for rectal cancer. Surg Endosc. 2009;23:296–303.
Liang J, Lai H, Lee P. Laparoscopic pelvic autonomic nerve-preserving surgery for patients with lower rectal cancer after chemoradiation therapy. Ann Surg Oncol. 2007;14:1285–7.
Morino M, Parini U, Allaix ME, et al. Male sexual and urinary function after laparoscopic total mesorectal excision. Surg Endosc. 2009;23:1233–40.
Quah HM, Jayne DG, Eu KW, et al. Bladder and sexual dysfunction following laparoscopically assisted and conventional open mesorectal resection for cancer. Br J Surg. 2002;89:1551–6.
Weber PA, Merola S, Wasielewski A, et al. Telerobotic-assisted laparoscopic right and sigmoid colectomies for benign disease. Dis Colon Rectum. 2002;45:1689–94.
Lanfranco AR, Castellanos AE, Desai JP, et al. Robotic surgery: a current perspective. Ann Surg. 2004;239:14–21.
Baik SH, Lee WJ, Rha KH, et al. Robotic total mesorectal excision for rectal cancer using four robotic arms. Surg Endosc. 2008;22:792–7.
D’Annibale A, Morpurgo E, Fiscon V, et al. Robotic and laparoscopic surgery for treatment of colorectal diseases. Dis Colon Rectum. 2004;47:2162–8.
Hellan M, Anderson C, Ellenhorn JD, et al. Short-term outcomes after robotic-assisted total mesorectal excision for rectal cancer. Ann Surg Oncol. 2007;14:3168–73.
Pigazzi A, Ellenhorn JDI, Ballantyne GH, et al. Robotic-assisted laparoscopic low anterior resection with total mesorectal excision for rectal cancer. Surg Endosc. 2006;20:1521–5.
Spinoglio G, Summa M, Priora F, et al. Robotic colorectal surgery: first 50 cases experience. Dis Colon Rectum. 2008;51:1627–32.
Kim NK. Anatomic basis of sharp pelvic dissection for curative resection of rectal cancer Yonsei Med J. 2005;46:737–49.
Nagtegaal ID, van de Velde CJ, van der Worp E, et al. Macroscopic evaluation of rectal cancer resection specimen: clinical significance of the pathologist in quality control. J Clin Oncol. 2002;20:1729–34.
Kim NK, Kim YW, Min BS, et al. Operative safety and oncologic outcomes of anal sphincter-preserving surgery with mesorectal excision for rectal cancer: 931 consecutive patients treated at a single institution. Ann Surg Oncol. 2009;16:900–9.
Enker WE, Havenga K, Polyak T, et al. Abdominoperineal resection via total mesorectal excision and autonomic nerve preservation for low rectal cancer. World J Surg. 1997;21:715–20.
Acknowledgment
This study was supported by the Good Health R&D Project (A090733), Ministry of Health and Welfare, Korea. J.Y.K. and N.K.K. have conflicts of interest or financial ties to disclosure.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kim, J.Y., Kim, NK., Lee, K.Y. et al. A Comparative Study of Voiding and Sexual Function after Total Mesorectal Excision with Autonomic Nerve Preservation for Rectal Cancer: Laparoscopic Versus Robotic Surgery. Ann Surg Oncol 19, 2485–2493 (2012). https://doi.org/10.1245/s10434-012-2262-1
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-012-2262-1