Abstract
Introduction
Outcome after hepatic resection for colorectal cancer liver metastases (CRLM) is heterogeneous and accurate predictors of survival are lacking. This study analyzes the prognostic relevance of pathologic details of the primary colorectal tumor in patients undergoing hepatic resection for CRLM.
Methods
Retrospective review of a prospective database identified patients who underwent resection for CRLM. Clinicopathological variables were investigated and their association with outcome was analyzed.
Results
From 1997–2007, 1,004 patients underwent hepatic resection for CRLM. The median follow-up was 59 months with a 5-year survival of 47 %. Univariate analysis identified nine factors associated with poor survival; three of these related to the primary tumor: lymphovascular invasion (LVI, p < 0.0001), perineural invasion (p = 0.005), and degree of regional lymph node involvement (N0 vs. N1 vs. N2, p < 0.0001). Multivariate analysis identified seven factors associated with poor survival, two of which related to the primary tumor: LVI (hazard ratio (HR) 1.3, 95 % confidence interval (CI) 1.06–1.64, p = 0.01) and degree of regional lymph node involvement [N1 (HR 1.3, 95 % CI 1.04–1.69, p = 0.02) vs. N2 (HR 1.7, 95 % CI 1.27–2.21, p < 0.0005)]. A significant decrease in survival along the spectrum of patients ranging from LVI negative/N0 to LVI positive/N2 was present. Patients who were LVI-positive/N2 had a median survival of 40 months compared with 74 months for patients who were LVI-negative/NO (p < 0.0001).
Conclusions
Histopathologic details of the primary colorectal tumor, particularly LVI and the detailed assessment of the degree of lymph node involvement, are strong predictors of survival. Future biomarker studies should consider exploring factors related to the primary colorectal tumor.
Similar content being viewed by others
Resection of colorectal cancer liver metastases (CRLM) has become the standard of care for patients with resectable disease and is the only potentially curative treatment. At diagnosis 20–25 % of patients with colorectal cancer will have synchronous liver metastases, and an additional 50–60 % of patients with colorectal cancer will develop metachronous liver metastases.1 , 2 Among patients with metastases isolated to the liver, approximately 10–20 % are candidates for hepatic resection. Complete resection of CRLM is associated with 5-year actuarial survival rates up to and greater than 50 % in most modern series and is curative in approximately 20 % of patients, as evidenced by 10-year disease-free survival.3 , 4
Numerous studies evaluating the outcome after hepatectomy for CRLM have identified a plethora of statistically significant single prognostic factors. However, the predictive value of these factors has not been consistent across studies, and although these factors can be associated with significant differences in survival, they do not necessarily impact decisions on resectability. In the absence of robust and effective single biomarkers, clinical and pathological factors often have been combined into grading systems and have proven to be reasonable predictors of outcome.5 Perhaps the most well-known study is by Fong et al.,6 which identified a clinical risk score based on five preoperative prognostic factors independently associated with long-term survival. However, when these factors were applied to a group of patients with actual 10-year follow-up, the highest clinical risk scores did not preclude the possibility of long-term survival or cure.4 In addition, this scoring system is not always an accurate predictor of outcome when applied to databases from other institutions.7 , 8
It is clear that novel and more effective prognostic factors are needed to help clinicians manage patients with potentially resectable CRLM. With better prognostic scoring systems that can accurately predict early postoperative death from disease and/or long-term cure, we may ultimately be able to better select patients for specific treatment protocols and to stratify patients in randomized, prospective trials. The past decade has seen numerous advancements in the management of patients with CRLM. Improvements in preoperative cross-sectional and functional imaging, patient selection, operative technique, perioperative management, and systemic and regional chemotherapies have improved outcomes and expanded our criteria for resectability.3 Therefore, periodic reassessment of prognostic factors and modification of scoring systems is warranted.
Recently, there have been improvements in the routine pathologic reporting of resected primary colorectal specimens.9 Pathologic details such as tumor grade, extent of locoregional lymph node involvement, and the presence of lymphovascular invasion (LVI) and/or perineural invasion (PNI) are now consistently reported. These pathologic details of the primary colorectal tumor have been only minimally studied as they pertain to the outcome after potentially curative resection for CRLM.10 , 11
The routine reporting of these pathologic factors began at the turn of the 21st century and we now have sufficient data and follow-up to analyze these factors in the context of outcome after hepatic resection with curative intent for CRLM. The purpose of our study was to analyze the prognostic relevance of pathologic details of the colorectal primary tumor in patients undergoing hepatic resection of CRLM.
Patients and Methods
Patients and Pretreatment Evaluation
Patients who underwent hepatic resection, with curative intent, for colorectal liver metastases between 1997 and 2007 were identified from a prospectively maintained surgical database at Memorial Sloan-Kettering Cancer Center (MSKCC). The MSKCC Institutional Review Board and Privacy Board, according to the institutional policy for protected health information, approved the study design. The study population only included patients with metastatic colon or rectal adenocarcinoma. Patients were selected for liver resection if they had: (1) appropriate medical fitness for a major operation; (2) no evidence of widely disseminated disease on preoperative evaluation or at laparotomy; and (3) an adequate future liver remnant free of metastatic disease. Preoperative staging consisted of cross-sectional imaging to evaluate the extent of intrahepatic disease and exclude extrahepatic disease. Imaging primarily consisted of contrast-enhanced computed tomography of the chest, abdomen, and pelvis. Colonoscopy was required within a year of the hepatic resection. Positron emission tomography, magnetic resonance imaging, and/or transabdominal ultrasound were used at the discretion of the treating physician(s). Intraoperative hepatic ultrasound was used routinely. Patients who were undergoing hepatectomy for recurrent CRLM, had extrahepatic metastatic disease, were treated with local ablative techniques exclusively, or underwent a two-stage hepatectomy were excluded. A specific review of patient demographics, clinicopathological factors related to the pathology of the primary colorectal tumor, the colorectal cancer liver metastases, and extent of hepatic resection was performed, and outcome data were analyzed.
Pathology of the Primary Colorectal Tumor
Specifically, the data with regards to the pathology of the primary colorectal tumor were obtained by a detailed review of pathology reports and specific pathologic re-review was not routinely performed. Pathologic staging was reported according to the American Joint Committee on Cancer (AJCC) staging guidelines (6th edition). The AJCC 6th edition was used, instead of the 7th edition, due to the more practical representation of nodal involvement for the purposes of statistical analysis. Histological grade of the primary tumor was characterized as: well, moderately, or poorly differentiated. There were very few cases of well-differentiated tumors and therefore well and moderately differentiated tumors were grouped together for purposes of analysis. Colorectal wall infiltration was characterized by T stage: T1 tumors invade the submucosa; T2 tumors invade the muscularis propria; T3 tumors invade through the muscularis propria into the subserosa or into nonperitonealized pericolic tissues; and T4 tumors perforate the visceral peritoneum or directly invade other organs. Locoregional lymph node involvement was analyzed as N0 (negative lymph nodes), N1 (1–3 positive lymph nodes), and N2 (>3 positive lymph nodes). In addition, the presence or absence of LVI and PNI were assessed. LVI is defined as present if cancer cells were identified within an epithelial-lined channel thought to represent either a lymphatic or small blood vessel.
Pathology of the Colorectal Liver Metastases
Specific factors related to the pathology of the liver metastases included the number of metastatic tumors, size of the largest tumor, and resection margin. In addition, prehepatectomy carcinoembryonic antigen (CEA) levels were measured and disease-free interval, defined as the time from presentation of the primary colorectal tumor to the time of presentation of colorectal liver metastases, was determined. Minor liver resections were defined as resection of <3 Couinaud segments and major liver resections were defined as resection of ≥3 Couinaud segments. R0 resection was defined has having a negative microscopic margin and R1 resection was defined has having a positive microscopic margin on histopathological examination.
Systemic and Regional Therapy
Neoadjuvant chemotherapy was defined as systemic therapy administered within 6 months before liver resection with the specific intent of treating the metastatic disease. Adjuvant chemotherapy, systemic or regional, was defined as therapy administered after potentially curative liver resection.
Outcome Data
Follow-up and overall survival were calculated from the date of liver resection to the date of last clinical encounter captured by the MSKCC medical record system or the date of death. Ninety-day morbidity and mortality were determined. Complications were graded on a 1-to-5 scale according to a previously published grading system12: Grade 1 complications require minor or no intervention; Grade 2 complications require moderate interventions; Grade 3 complications require hospital readmission, surgical intervention, or radiologic intervention; Grade 4 complications produce chronic disability, organ resection, or enteral diversion; and Grade 5 complications result in death.
Statistics
Statistical analyses were performed with SPSS software version 12.0 for Windows (Statistical Package for the Social Sciences, Chicago, IL). Categorical variable were compared using a Chi-square test. The log-rank test was used to make univariate comparisons. Multivariable analyses of survival were performed with a Cox regression analysis method with incorporated factors which reached significance of p < 0.1 on univariate analysis, and we have used the standard approach of excluding from the multivariable analyses any patient with missing values. Survival probabilities were estimated using the Kaplan–Meier method and compared with a log-rank test.
Results
Patient and Primary Colorectal Tumor Characteristics
A total of 1,363 patients underwent hepatic resection for CRLM between 1997 and 2007, and 359 patients (26 %) were excluded because they were undergoing hepatectomy for recurrent CRLM, had extrahepatic metastatic disease, were treated with local ablative techniques exclusively, or underwent a two-stage hepatectomy. Therefore, the study cohort consisted of 1,004 patients (74 %) who underwent primary hepatic resection with curative intent. Table 1 summarizes the patient and primary colorectal tumor characteristics. Seventy-seven percent of the patients were ≤70 years of age and 584 (58 %) were men. The majority of patients (72 %) had a primary tumor of the colon, presented with a locoregionally advanced primary tumor with regards to T and N stage, and presented with metachronous disease (58 %). Approximately 90 % of primary tumors were well or moderately differentiated. The median number of harvested lymph nodes was 12 (data not shown). LVI and PNI were present in 331 (33 %) and 181 (18 %) of cases but were not reported in 223 (23 %) and 329 (33 %) of cases, respectively.
Colorectal Liver Metastases and Treatment Characteristics
Table 2 summarizes the characteristics of the CRLM and their treatment; 522 patients (58 %) underwent a major hepatic resection, whereas the other 425 patients (42 %) underwent minor segmental, wedge, or atypical resections. The majority of patients had smaller (≤5 cm) and multiple tumors (>1). Perioperative, systemic and/or regional, chemotherapy was administered to 924 patients (92 %); specifically, 464 (46 %) received neoadjuvant therapy, 842 (84 %) received adjuvant therapy, and 343 (34 %) patients received regional hepatic artery infusional therapy. Eighty-six percent of patients had an R0 resection. In addition, there was no association between LVI and degree of lymph node involvement with regards to the size of the CRLM, number of CRLM, presence of bilateral hepatic disease, or the need for major hepatectomy (data not shown).
Outcome
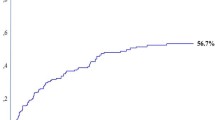
The median follow-up for survivors was 59 months with an overall median survival of 56 months and a predicted 5 and 10-year survival rate of 47 and 28 %, respectively (Fig. 1). The rate of 90-day postoperative complications was 33.5 %; minor complications (grade 1–2) occurred in 22 %, and major complications (grade 3–4) occurred in 11.5 % of cases. Perioperative 90-day mortality occurred in 22 (2 %) patients (data not shown).
Univariate and Multivariate Analysis of Factors Associated with Overall Survival
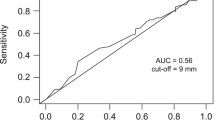
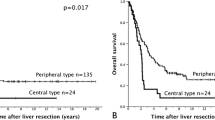
Univariate analysis identified nine factors associated with poor survival (Table 3). Three of these related to the pathology of the primary colorectal tumor: LVI (p < 0.0001), PNI (p = 0.005), and degree of regional lymph node involvement (N0 vs. N1 vs. N2, p < 0.0001). Multivariate analysis identified seven factors associated with poor survival (Table 4). Two of these related to the pathology of the primary tumor: LVI (HR 1.3, 95 % CI 1.06–1.64, p = 0.01) and degree of regional lymph node involvement where an increase in the number of metastatic regional lymph nodes from N1 (HR 1.3, 95 % CI 1.04–1.69, p = 0.02) to N2 (HR 1.7, 95 % CI 1.27–2.21, p < 0.0005) was associated with a worse survival. Specifically, LVI-positive patients had a median survival of 48 months compared with 69 months for LVI-negative patients (p < 0.0001), and N0 patients had a median survival of 74 months compared with 54 and 40 months for N1 and N2 patients, respectively (p < 0.0001). Furthermore, Table 5 depicts the significant decrease in survival along the spectrum of patients ranging from LVI-negative/N0 to LVI-positive/N2 (p < 0.0001) such that patients who were LVI-positive with N2 nodal disease had a median survival of 40 months compared with 74 months for patients who were LVI-negative with no nodal disease (p < 0.0001).
Discussion
As evidenced by the favorable 5- and 10-year predicted survival of 47 and 28 % in this modern cohort of patients, resection of CRLM is associated with long-term survival and the potential for cure in well-selected patients. These outcomes are comparable to recent institutional and multi-institutional studies where reported 5-year survival rates ranged from 36 to 58 %.8 , 13 – 16 However, outcome after hepatic resection for CRLM is still heterogeneous and many patients still do poorly even after careful selection and a successful operation. Ultimately recurrence of disease occurs in 60–80 % of patients and a significant proportion (approximately 20 %) die within 2 years of operation. Most importantly, accurate and clinically meaningful predictors of the extremes of outcome (early death vs. long-term survival) are lacking.
To this end, novel prognostic factors are needed to help clinicians manage patients with potentially resectable CRLM. The last decade has seen numerous advancements in the assessment and management of patients with CRLM and therefore, the need for periodic reassessment of prognostic factors and modification of scoring systems also is warranted.5 We hypothesized that factors in the primary colorectal tumor may help discern the biological behavior of resected CRLM, which would result in better predictors of outcome.
Specifically, LVI, which has not previously been reported or proposed as a prognostic factor for outcome after hepatic resection for CRLM, has been shown to be a predictor of poor outcome in patients with primary nonmetastatic colorectal cancer and other primary malignancies (i.e., cholangiocarcinoma, breast, and melanoma).17 – 20 In our study, the presence of LVI in the primary colorectal tumor was a poor prognostic indicator based on Cox regression analysis in patients with LVI positive primary colorectal tumors having a median survival of 48 months compared with 69 months for patients with no evidence of LVI in their primary colorectal tumor (p < 0.0001).
Involvement of regional lymph nodes from the primary colorectal tumor has been shown in various studies to be a significant prognostic factor for outcome in patients undergoing hepatic resection of CRLM 6 , 21 , 22; however, these studies have primarily taken into consideration only whether the regional lymph nodes were negative or positive. More recently, two nomograms for estimating survival in patients with CRLM have been published where the degree of regional lymph node involvement was evaluated.23 , 24 Both of these studies indicated that an increase in the number of metastatic regional lymph nodes was associated with a worse outcome; however, the specific effect of the degree of nodal involvement (N0 vs. N1 vs. N2) was not comprehensively analyzed or reported. In our study, an increase in the degree of regional lymph node involvement was independently associated with a reduced survival on Cox regression analysis such that the risk of death with N1 (HR 1.3) or N2 (HR 1.7) nodal disease was significantly increased compared with N0 nodal disease.
Moreover, based on these two significant prognostic factors, we are able to identify a subgroup of patients who appear to have biologically more aggressive tumors given that survival was significantly reduced in the presence of these factors. Patients whose primary tumors were LVI-positive and had N2 nodal disease had an overall survival of 40 months compared with 74 months for patients who were LVI-negative with no nodal disease (p < 0.0001). This worse outcome was evident regardless of whether patients presented with synchronous or metachronous disease as depicted by the fact that disease-free interval did not impact the prognostic significance of LVI or degree of regional lymph node involvement on multivariate analysis. It is important to highlight that this high-risk group still had the potential for long-term survival and therefore should still be considered for hepatic resection. However, these findings provide us with further insight on the biology of a patient’s tumor and can help to identify a subgroup of patients with more aggressive tumors where one may consider alternative (neo)adjuvant treatment regimens, allow for stratification within a clinical trial, or consider a different surveillance regimen.
Furthermore, although this was not the primary goal of our study, we identified various significant prognostic factors on Cox regression analysis that were related to the hepatic metastasis and treatment, specifically: (1) size of liver metastasis (>5 cm), (2) number of liver metastasis (>1), (3) CEA level (>200 pg/ml), (4) R0 versus R1 hepatic resection, and (5) utilization of regional hepatic artery infusion therapy. Several of these factors (size, number, and CEA) are similar to the preoperative prognostic factors identified previously by our group in a prior cohort of 1,001 patients undergoing hepatic resection with curative intent 6 and have maintained their prognostic significance in this modern cohort of patients.
Limitations of this retrospective study include the lack of pathological re-review of all pathology specimens of the primary colorectal tumor and thus the absence of LVI and PNI status in approximately 20 and 30 % of patients in our series, respectively. Furthermore, although the median number of harvested lymph nodes in our study population was 12; approximately 16 % of the study population had inadequate lymph node sampling (data not shown). Due to the retrospective nature of the study and the fact that not all patients received the treatment for the primary tumor at our institution, we cannot definitively comment on how these patients were managed in a uniform manner, and because this comprised only a small percentage of our study population, it was not feasible for us to study this issue in depth statistically. In addition, we did not evaluate for the presence of LVI within the CRLM and, therefore, did not determine the correlation of its presence to the presence of LVI within the primary colorectal tumor and its association with outcome. Recently, two, small, single-institution series have associated the presence of LVI within the CLRM with a significantly poor outcome, and future studies in the area are required.25 , 26
Conclusions
Resection of CLRM is associated with long-term survival. Pathologic details of the primary colorectal tumor, particularly LVI and the degree of lymph node involvement, are strong predictors of survival although the presences of these factors do not preclude long-term survival and cure. It is clear that novel and more effective prognostic factors are still needed to help clinicians manage patients with potentially resectable CRLM. Future biomarker studies should consider exploring factors related to the primary colorectal tumor.
References
Fong Y, Kemeny N, Paty P, et al. Treatment of colorectal cancer: hepatic metastasis. Semin Surg Oncol. 1996;12:219–52.
Kemeny N. Management of liver metastases from colorectal cancer. Oncology (Williston Park). 2006;20:1161–76, 1179; discussion 1179–80, 1185–6.
House MG, Ito H, Gonen M, et al. Survival after hepatic resection for metastatic colorectal cancer: trends in outcomes for 1,600 patients during two decades at a single institution. J Am Coll Surg. 2010;210:744–52, 752–5.
Tomlinson JS, Jarnagin WR, DeMatteo RP, et al. Actual 10-year survival after resection of colorectal liver metastases defines cure. J Clin Oncol. 2007;25:4575–80.
Jarnagin WR. Clinical scoring systems for stratifying risk after resection of hepatic colorectal metastases: still relevant? Ann Surg Oncol. 2011;18:2711–3.
Fong Y, Fortner J, Sun RL, et al. Clinical score for predicting recurrence after hepatic resection for metastatic colorectal cancer: analysis of 1001 consecutive cases. Ann Surg 1999;230:309–18; discussion 318–21.
Nanashima A, Sumida Y, Abo T, et al. A modified grading system for post-hepatectomy metastatic liver cancer originating from colorectal carcinoma. J Surg Oncol. 2008;98:363–70.
Zakaria S, Donohue JH, Que FG, et al. Hepatic resection for colorectal metastases: value for risk scoring systems? Ann Surg. 2007;246:183–91.
Compton CC, Fielding LP, Burgart LJ, et al. Prognostic factors in colorectal cancer. College of American Pathologists Consensus Statement 1999. Arch Pathol Lab Med. 2000;124:979–94.
Tan MC, Castaldo ET, Gao F, et al. A prognostic system applicable to patients with resectable liver metastasis from colorectal carcinoma staged by positron emission tomography with [18F]fluoro-2-deoxy-d-glucose: role of primary tumor variables. J Am Coll Surg. 2008;857–68; discussion 868–9.
Malafosse R, Penna C, Sa Cunha A, Nordlinger B. Surgical management of hepatic metastases from colorectal malignancies. Ann Oncol. 2001;12:887–94.
Martin RC, 2nd, Brennan MF, Jaques DP. Quality of complication reporting in the surgical literature. Ann Surg. 2002;235:803–13.
de Haas RJ, Wicherts DA, Andreani P, et al. Impact of expanding criteria for resectability of colorectal metastases on short- and long-term outcomes after hepatic resection. Ann Surg. 2011;253:1069–79.
Rees M, Tekkis PP, Welsh FK, et al. Evaluation of long-term survival after hepatic resection for metastatic colorectal cancer: a multifactorial model of 929 patients. Ann Surg. 2008;247:125–35.
Malik HZ, Prasad KR, Halazun KJ, et al. Preoperative prognostic score for predicting survival after hepatic resection for colorectal liver metastases. Ann Surg. 2007;246:806–14.
Nathan H, de Jong MC, Pulitano C, et al. Conditional survival after surgical resection of colorectal liver metastasis: an international multi-institutional analysis of 949 patients. J Am Coll Surg. 2010;210:755–64, 764–6.
Lim SB, Yu CS, Jang SJ, et al. Prognostic significance of lymphovascular invasion in sporadic colorectal cancer. Dis Colon Rectum. 2010;53:377–84.
Patel SH, Kooby DA, Staley CA 3rd, et al. The prognostic importance of lymphovascular invasion in cholangiocarcinoma above the cystic duct: a new selection criterion for adjuvant therapy? HPB (Oxford). 2011;13:605–11.
Schoppmann SF, Bayer G, Aumayr K, et al. Prognostic value of lymphangiogenesis and lymphovascular invasion in invasive breast cancer. Ann Surg. 2004; 240:306–312.
Dadras SS, Paul T, Bertoncini J, et al. Tumor lymphangiogenesis: a novel prognostic indicator for cutaneous melanoma metastasis and survival. Am J Pathol. 2003;162:1951–60.
Nordlinger B, Guiguet M, Vaillant JC, et al. Surgical resection of colorectal carcinoma metastases to the liver. A prognostic scoring system to improve case selection, based on 1,568 patients. Association Francaise de Chirurgie. Cancer. 1996;77:1254–62.
Jaeck D, Bachellier P, Guiguet M, et al. Long-term survival following resection of colorectal hepatic metastases. Association Francaise de Chirurgie. Br J Surg. 1997;84:977–80.
Kattan MW, Gonen M, Jarnagin WR, et al. A nomogram for predicting disease-specific survival after hepatic resection for metastatic colorectal cancer. Ann Surg. 2008;247:282–7.
Kanemitsu Y, Kato T. Prognostic models for predicting death after hepatectomy in individuals with hepatic metastases from colorectal cancer. World J Surg. 2008;32:1097–107.
Sasaki A, Aramaki M, Kawano K, et al. Prognostic significance of intrahepatic lymphatic invasion in patients with hepatic resection due to metastases from colorectal carcinoma. Cancer. 2002;95:105–11.
Korita PV, Wakai T, Shirai Y, et al. Intrahepatic lymphatic invasion independently predicts poor survival and recurrences after hepatectomy in patients with colorectal carcinoma liver metastases. Ann Surg Oncol. 2007;14:3472–80.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cardona, K., Mastrodomenico, P., D’Amico, F. et al. Detailed Pathologic Characteristics of the Primary Colorectal Tumor Independently Predict Outcome after Hepatectomy for Metastases. Ann Surg Oncol 20, 148–154 (2013). https://doi.org/10.1245/s10434-012-2540-y
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-012-2540-y