Abstract
Background
We sought to determine whether lymph node ratio (LNR; defined as number of positive nodes/number of nodes dissected) provides additional prognostic information in node-positive breast cancer patients.
Methods
Data from a cohort of 319 node-positive breast cancer patients diagnosed between 1956 and 1982 were analyzed for overall survival (OS) on the basis of current American Joint Committee on Cancer (AJCC) nodal staging versus LNR.
Results
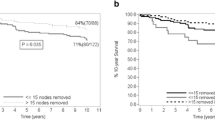
In terms of AJCC categorization, 157 patients (49.2%) were pN1 (1–3 positive nodes), 97 (30.4%) were pN2 (4–9 positive nodes), and 65 (20.4%) were pN3 (≥10 positive nodes). In terms of LNR, 90 (28.2%) were low risk (LNR = 0.01–0.20), 119 (38.3%) were intermediate risk (LNR = 0.21–0.65), and 110 (34.5%) were high risk (LNR > 0.65). The median follow-up was 68.7 months. AJCC nodal status correlated with OS (median OS 85.9, 70.4, and 48.4 months for pN1–3, respectively, P = 0.018). LNR also correlated with OS (median OS 105.8, 72.2, and 48.4 months for the low-, intermediate-, and high-risk groups, respectively, P < 0.005). On multivariate analysis, LNR predicted OS independent of pN status (P < 0.001). Stratifying by pN status, LNR could discriminate distinct subpopulations of patients with significantly different OS rates. In a multivariate model controlling for clinicopathologic factors (tumor size, grade, estrogen receptor, progesterone receptor, and her-2-neu status), LNR remained a significant predictor of OS (P < 0.001).
Conclusions
LNR has the ability to discriminate populations with different OS rates within traditional AJCC node classification groups and predicts OS independent of traditional clinicopathologic factors. These results should be validated and considered for future incorporation into the breast cancer staging system.





Similar content being viewed by others
References
American Joint Committee on Cancer. Breast. In: Edge SB, Byrd DR, Compton CC, et al., editors. AJCC cancer staging handbook. 7th ed. New York: Springer Verlag; 2010. p. 417–60.
Fisher B, Jeong JH, Anderson S, Bryant J, Fisher ER, Wolmark N. Twenty-five-year follow-up of a randomized trial comparing radical mastectomy, total mastectomy, and total mastectomy followed by irradiation. N Engl J Med. 2002;347:567–75.
Saha S, Farrar WB, Young DC, Ferrara JJ, Burak WE Jr. Variation in axillary node dissection influences the degree of nodal involvement in breast cancer patients. J Surg Oncol. 2000;73:134–7.
Schaapveld M, Otter R, de Vries EG, et al. Variability in axillary lymph node dissection for breast cancer. J Surg Oncol. 2004;87:4–12.
Harris JR, Halpin-Murphy P, McNeese M, Mendenhall NP, Morrow M, Robert NJ. Consensus statement on postmastectomy radiation therapy. Int J Radiat Oncol Biol Phys. 1999;44:989–90.
Giuliano AE, McCall L, Beitsch P, et al. Locoregional recurrence after sentinel lymph node dissection with or without axillary dissection in patients with sentinel lymph node metastases: the American College of Surgeons Oncology Group Z0011 randomized trial. Ann Surg. 2010;252:426–32.
Chang GJ, Rodriguez-Bigas MA, Skibber JM, Moyer VA. Lymph node evaluation and survival after curative resection of colon cancer: systematic review. J Natl Cancer Inst. 2007;99:433–41.
Chagpar AB, Scoggins CR, Martin RC, et al. Factors determining adequacy of axillary node dissection in breast cancer patients. Breast J. 2007;13:233–7.
Axillary dissection. The Steering Committee on Clinical Practice Guidelines for the Care and Treatment of Breast Cancer. CMAJ. 1998;158(Suppl 3):S22–6.
Voordeckers M, Vinh-Hung V, Van de Steene J, Lamote J, Storme G. The lymph node ratio as prognostic factor in node-positive breast cancer. Radiother Oncol. 2004;70:225–30.
Vinh-Hung V, Joseph SA, Coutty N, Ly BH, Vlastos G, Nguyen NP. Age and axillary lymph node ratio in postmenopausal women with T1-T2 node positive breast cancer. Oncologist. 2010;15:1050–62.
van der Wal BC, Butzelaar RM, van der Meij S, Boermeester MA. Axillary lymph node ratio and total number of removed lymph nodes: predictors of survival in stage I and II breast cancer. Eur J Surg Oncol. 2002;28:481–9.
Truong PT, Lesperance M, Li KH, MacFarlane R, Speers CH, Chia S. Micrometastatic node-positive breast cancer: long-term outcomes and identification of high-risk subsets in a large population-based series. Ann Surg Oncol. 2010;17:2138–46.
Oven Ustaalioglu BB, Bilici A, Kefeli U, et al. Does the metastatic lymph node ratio influence the disease-free survival of patients with breast cancer: single-center experiences. Oncology. 2010;79:105–11.
Martinez-Ramos D, Escrig-Sos J, Alcalde-Sanchez M, Torrella-Ramos A, Salvador-Sanchis JL. Disease-free survival and prognostic significance of metastatic lymph node ratio in T1-T2N positive breast cancer patients. A population registry-based study in a European country. World J Surg. 2009;33:1659–64.
Ibrahim EM, Elkhodary TR, Zekri JM, et al. Prognostic value of lymph node ratio in poor prognosis node-positive breast cancer patients in Saudi Arabia. Asia Pac J Clin Oncol. 2010;6:130–7.
Danko ME, Bennett KM, Zhai J, Marks JR, Olson JA Jr. Improved staging in node-positive breast cancer patients using lymph node ratio: results in 1,788 patients with long-term follow-up. J Am Coll Surg. 2010;210:797–805.
Chagpar AB, Scoggins CR, Martin RC, et al. Predicting patients at low probability of requiring postmastectomy radiation therapy. Ann Surg Oncol. 2007;14:670–7.
Chagpar AB, Scoggins CR, Martin RC, et al. Prediction of sentinel lymph node-only disease in women with invasive breast cancer. Am J Surg. 2006;192:882–7.
Degnim AC, Reynolds C, Pantvaidya G, et al. Nonsentinel node metastasis in breast cancer patients: assessment of an existing and a new predictive nomogram. Am J Surg. 2005;190:543–50.
NCCN clinical practice guidelines in oncology: breast cancer. National Comprehensive Cancer Network. 2011. http://www.nccn.com/.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chagpar, A.B., Camp, R.L. & Rimm, D.L. Lymph Node Ratio Should Be Considered for Incorporation into Staging for Breast Cancer. Ann Surg Oncol 18, 3143–3148 (2011). https://doi.org/10.1245/s10434-011-2012-9
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-011-2012-9