ABSTRACT
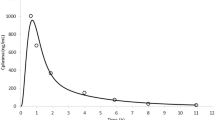
In a recent food effect clinical study, the authors concluded that a meal consisting of ≥500 kcal, regardless of fat content, produced the maximal bioavailability for ziprasidone. Using GastroPlus™, a commercially available pharmacokinetic simulation software, a semiphysiological model—a kind of physiologically based pharmacokinetic (PBPK) absorption model—was developed that could predict the concentration-time profiles when ziprasidone was administered with any one of the five test meals or fasting. Ziprasidone intravenous pharmacokinetics and oral absorption permeability were determined from clinical studies following the intravenous and duodenal infusion of ziprasidone to volunteers. From the detailed dietary information of each meal provided in the previously published food effect study, the stomach pH, volume, and gastric emptying could be predicted. Incorporating these meal-specific parameters into the model improved the predictions beyond the default fed/fasted parameters commonly used in the software. Compared to the default models, the improved models resulted in an improved prediction of the average ziprasidone concentration-time profile for each meal. Using this type of semiphysiological absorption model, we have shown that the dietary contents of the meals should be taken into account to predict food effects for ziprasidone and perhaps other BCS class I or II compounds.








Similar content being viewed by others
Notes
pKa was determined by SCS at UNE College of Pharmacy.
The ASF models are the best fits of experimental data across a diverse set of compounds (GastroPlus™ Manual, August 2013, Version 8.5, p. 168). The data could also be fitted to the Optimized logD Model by adjusting percent volume in the small and large intestines.
The ASF model used in reference [16] was “Opt logD”, whereas in this work, the model used as “Opt logD Model SA/V 6.1”.
REFERENCES
Welling PG. Effects of food on drug absorption. Annual Review of Nutrition. 1996;16(1):383–415.
Harvey PD, Bowie CR. Ziprasidone: efficacy, tolerability, and emerging data on wide-ranging effectiveness. Expert Opinion on Pharmacotherapy. 2005;6(2):337–46.
Amidon G, Lennernas H, Shah V, Crison J. A theoretical basis for a biopharmaceutic drug classification: correlation of in vitro drug product dissolution and in vivo bioavailability. Pharm Res. 1995;12:413–20.
Hamelin BA, Allard S, Laplante L, Miceli J, Wilner KD, Tremblay J, Lebel M. The effect of timing of a standard meal on the pharmacokinetics and pharmacodynamics of the novel atypical antipsychotic agent ziprasidone. Pharmacotherapy. 1998;18(1):9–15.
Gandelman K, Alderman JA, Lombardo I, LaBadie RR, Versavel M, Preskorn SH. The impact of calories and fat content of meals on oral ziprasidone absorption: a randomized, open-label, crossover trial. J Clin Psychiatry. 2009;70(1):58–62.
Thombre A, Herbig S, Alderman J. Improved ziprasidone formulations with enhanced bioavailability in the fasted state and a reduced food effect. Pharmaceutical Research. 2011;28(12):3159–70.
Yasuda M. Dissociation constants of some carboxylic acids in mixed aqueous solvents. Bulletin of the Chemical Society of Japan. 1959;32(5):429–32.
Shedlovsky T, Kay RL. The ionization constant of acetic acid in water-methanol mixtures at 25° from conductance measurements. The Journal of Physical Chemistry. 1956;60(2):151–5.
Fiese EF. General pharmaceutics—the new physical pharmacy. J Pharm Sci. 2003;92:1331–42.
Thombre AG, Caldwell WB, Friesen DT, McCray SB, Sutton SC. Solid nanocrystalline dispersions of ziprasidone with enhanced bioavailability in the fasted state. Molecular Pharmaceutics. 2012;9:3526–34.
Mithani SD, Bakatselou V, TenHoor CN, Dressman JB. Estimation of the increase in solubility of drugs as a function of bile salt concentration. Pharmaceutical Research. 1996;13(1):163–7.
Agoram B, Woltosz WS, Bolger MB. Predicting the impact of physiological and biochemical processes on oral drug bioavailability. Advanced Drug Delivery Reviews. 2001;50(Supplement 1):S41–67.
Parrott N, Lukacova V, Fraczkiewicz G, Bolger M. Predicting pharmacokinetics of drugs using physiologically based modeling—application to food effects. The AAPS Journal. 2009;11(1):45–53.
Hunt J, Stubbs D. The volume and energy content of meals as determinants of gastric emptying. J Physiol (Lond). 1975;245:209–25.
Akaike, H. Information theory and the extension of the maximum likelihood principle. in Proceedings of the Second International Symposium on Information Theory. 1973. Budapest Akailseoniai-Kiudo.
Sutton S. Role of physiological intestinal water in oral absorption. The AAPS Journal. 2009;11(2):277–85.
Fleisher D, Li C, Zhou Y, Pao LH, Karim A. Drug, meal and formulation interactions influencing drug absorption after oral administration. Clinical implications. Clin Pharmacokinet. 1999;36:233–54.
Festi D, Colecchia A, Larocca A, Villanova N, Mazzella G, Petroni ML, Romano F, Roda E. Review: low caloric intake and gall-bladder motor function. Alimentary Pharmacology & Therapeutics. 2000;14:51–3.
Fox M, Barr C, Nolan S, Lomer M, Anggiansah A, Wong T. The effects of dietary fat and calorie density on esophageal acid exposure and reflux symptoms. Clinical gastroenterology and hepatology : the official clinical practice journal of the American Gastroenterological Association. 2007;5(4):439–44. e1
Kotrba C, Code C. Gastric acid secretory responses to some purified foods and to additions of sucrose or olive oil. The American Journal of Digestive Diseases. 1969;14(1):1–8.
Colombo P, Mangano M, Bianchi PA, Penagini R. Effect of calories and fat on postprandial gastro-oesophageal reflux. Scandinavian Journal of Gastroenterology. 2002;37(1):3–5.
Ikonen T, Morri S, Tyrisevä AM, Ruottinen O, Ojala M. Genetic and phenotypic correlations between milk coagulation properties, milk production traits, somatic cell count, casein content, and pH of milk. Journal of dairy science. 2004;87(2):458–67.
FDA, Guidance for industry: food-effect bioavailability and fed bioequivalence studies, CDER. 2002: Washington, DC.
Author information
Authors and Affiliations
Corresponding author
ELECTRONIC SUPPLEMENTARY MATERIAL
ESM 1
(PDF 508 kb)
Rights and permissions
About this article
Cite this article
Sutton, S.C., Nause, R. & Gandelman, K. The impact of gastric pH, volume, and emptying on the food effect of ziprasidone oral absorption. AAPS J 19, 1084–1090 (2017). https://doi.org/10.1208/s12248-017-0065-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1208/s12248-017-0065-9