Abstract
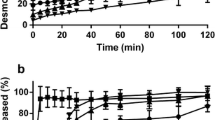
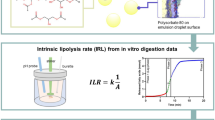
The impact of pancreatin and calcium addition on a wide array of lipid-based formulations (LBFs) during in vitro lipolysis, with regard to digestion rates and distribution of the model drug danazol, was investigated. Pancreatin primarily affected the extent of digestion, leaving drug distribution somewhat unaffected. Calcium only affected the extent of digestion slightly but had a major influence on drug distribution, with more drug precipitating at higher calcium levels. This is likely to be caused by a combination of removal of lipolysis products from solution by the formation of calcium soaps and calcium precipitating with bile acids, events known to reduce the solubilizing capacity of LBFs dispersed in biorelevant media. Further, during the digestion of hydrophilic LBFs, like IIIA-LC, the un-ionized–ionized ratio of free fatty acids (FFA) remained unchanged at physiological calcium levels. This makes the titration curves at pH 6.5 representable for digestion. However, caution should be taken when interpreting lipolysis curves of lipophilic LBFs, like I-LC, at pH 6.5, at physiological levels of calcium (1.4 mM); un-ionized–ionized ratio of FFA might change during digestion, rendering the lipolysis curve at pH 6.5 non-representable for the total digestion. The ratio of un-ionized–ionized FFAs can be maintained during digestion by applying non-physiological levels of calcium, resulting in a modified drug distribution with increased drug precipitation. However, as the main objective of the in vitro digestion model is to evaluate drug distribution, which is believed to have an impact on bioavailability in vivo, a physiological level (1.4 mM) of calcium is preferred.








Similar content being viewed by others
References
Araya H, Nagao S, Tomita M, Hayashi M. The novel formulation design of self-emulsifying drug delivery systems (SEDDS) type O/W microemulsion I: enhancing effects on oral bioavailability of poorly water soluble compounds in rats and beagle dogs. Drug Metab Pharmacokinet. 2005;20(4):244–56.
Araya H, Tomita M, Hayashi M. The novel formulation design of self-emulsifying drug delivery systems (SEDDS) type O/W microemulsion II: stable gastrointestinal absorption of a poorly water soluble new compound, ER-1258 in bile-fistula rats. Drug Metab Pharmacokinet. 2005;20(4):257–67.
Kang BK, Lee JS, Chon SK, et al. Development of self-microemulsifying drug delivery systems (SMEDDS) for oral bioavailability enhancement of simvastatin in beagle dogs. Int J Pharm. 2004;274(1–2):65–73.
Larsen AT, Ohlsson AG, Polentarutti B, et al. Oral bioavailability of cinnarizine in dogs: relation to SNEDDS droplet size, drug solubility and in vitro precipitation. Eur J Pharm Sci. 2013;48(1–2):339–50.
Di Maio S, Carrier RL. Gastrointestinal contents in fasted state and post-lipid ingestion: in vivo measurements and in vitro models for studying oral drug delivery. J Control Release. 2011;151(2):110–22.
Zangenberg NH, Mullertz A, Kristensen HG, Hovgaard L. A dynamic in vitro lipolysis model. I. Controlling the rate of lipolysis by continuous addition of calcium. Eur J Pharm Sci. 2001;14(2):115–22.
Carriere F, Grandval P, Renou C, et al. Quantitative study of digestive enzyme secretion and gastrointestinal lipolysis in chronic pancreatitis. Clin Gastroenterol Hepatol. 2005;3(1):28–38.
Ville E, Carriere F, Renou C, Laugier R. Physiological study of pH stability and sensitivity to pepsin of human gastric lipase. Digestion. 2002;65(2):73–81.
Johnston N, Dettmar PW, Bishwokarma B, et al. Activity/stability of human pepsin: implications for reflux attributed laryngeal disease. Laryngoscope. 2007;117(6):1036–9.
Gargouri Y, Pieroni G, Riviere C, et al. Kinetic assay of human gastric lipase on short- and long-chain triacylglycerol emulsions. Gastroenterology. 1986;91(4):919–25.
Carriere F, Barrowman JA, Verger R, Laugier R. Secretion and contribution to lipolysis of gastric and pancreatic lipases during a test meal in humans. Gastroenterology. 1993;105(3):876–88.
Armand M, Borel P, Pasquier B, et al. Physicochemical characteristics of emulsions during fat digestion in human stomach and duodenum. Am J Physiol. 1996;271(1 Pt 1):G172–83.
Capolino P, Guérin C, Paume J, et al. In vitro gastrointestinal lipolysis: replacement of human digestive lipases by a combination of rabbit gastric and porcine pancreatic extracts. Food Dig. 2011;2:43–51.
Fernandez S, Jannin V, Rodier JD, et al. Comparative study on digestive lipase activities on the self emulsifying excipient Labrasol, medium chain glycerides and PEG esters. Biochim Biophys Acta. 2007;1771(5):633–40.
Armand M. Lipases and lipolysis in the human digestive tract: where do we stand? Curr Opin Clin Nutr Metab Care. 2007;10(2):156–64.
Xiao X, Ross LE, Sevilla WA, et al. Porcine pancreatic lipase related protein 2 has high triglyceride lipase activity in the absence of colipase. Biochim Biophys Acta. 2013;1831(9):1435–41.
Alvarez FJ, Stella VJ. The role of calcium ions and bile salts on the pancreatic lipase-catalyzed hydrolysis of triglyceride emulsions stabilized with lecithin. Pharm Res. 1989;6(6):449–57.
Patton JS, Carey MC. Watching fat digestion. Science. 1979;204(4389):145–8.
Lindahl A, Ungell AL, Knutson L, Lennernas H. Characterization of fluids from the stomach and proximal jejunum in men and women. Pharm Res. 1997;14(4):497–502.
Hofmann AF, Mysels KJ. Bile acid solubility and precipitation in vitro and in vivo: the role of conjugation, pH, and Ca2+ ions. J Lipid Res. 1992;33(5):617–26.
Williams HD, Sassene P, Kleberg K, et al. Toward the establishment of standardized in vitro tests for lipid-based formulations, part 1: method parameterization and comparison of in vitro digestion profiles across a range of representative formulations. J Pharm Sci. 2012;101(9):3360–80.
Williams HD, Anby MU, Sassene P, et al. Toward the establishment of standardized in vitro tests for lipid-based formulations. 2. The effect of bile salt concentration and drug loading on the performance of type I, II, IIIA, IIIB, and IV formulations during in vitro digestion. Mol Pharm. 2012;9(11):3286–300.
Williams HD, Sassene P, Kleberg K, et al. Toward the establishment of standardized in vitro tests for lipid-based formulations, part 3: understanding supersaturation versus precipitation potential during the in vitro digestion of type I, II, IIIA, IIIB and IV lipid-based formulations. Pharm Res. 2013;30:3059–76.
Carriere F, Moreau H, Raphel V, et al. Purification and biochemical characterization of dog gastric lipase. Eur J Biochem. 1991;202(1):75–83.
Fernandez S, Rodier JD, Ritter N, et al. Lipolysis of the semi-solid self-emulsifying excipient Gelucire 44/14 by digestive lipases. Biochim Biophys Acta. 2008;1781(8):367–75.
Kanicky JR, Shah DO. Effect of degree, type, and position of unsaturation on the pKa of long-chain fatty acids. J Colloid Interface Sci. 2002;256(1):201–7.
Cistola DP, Hamilton JA, Jackson D, Small DM. Ionization and phase behavior of fatty acids in water: application of the Gibbs phase rule. Biochemistry. 1988;27(6):1881–8.
Cuine JF, McEvoy CL, Charman WN, et al. Evaluation of the impact of surfactant digestion on the bioavailability of danazol after oral administration of lipidic self-emulsifying formulations to dogs. J Pharm Sci. 2008;97(2):995–1012.
Devraj R, Williams HD, Warren DB, et al. In vitro digestion testing of lipid-based delivery systems: calcium ions combine with fatty acids liberated from triglyceride rich lipid solutions to form soaps and reduce the solubilization capacity of colloidal digestion products. Int J Pharm. 2013;441(1–2):323–33.
Zangenberg NH, Mullertz A, Kristensen HG, Hovgaard L. A dynamic in vitro lipolysis model. II: evaluation of the model. Eur J Pharm Sci. 2001;14(3):237–44.
Bodansky O. Are the phosphatases of bone, kidney, intestine, and serum identical? The use of bile acids in their differentiation. J Biol Chem. 1937;118(2):341–62.
Salentinig S, Sagalowicz L, Glatter O. Self-assembled structures and pK(a) value of oleic acid in systems of biological relevance. Langmuir. 2010;26(14):11670–9.
Salentinig S, Sagalowicz L, Leser ME, et al. Transitions in the internal structure of lipid droplets during fat digestion. Soft Matter. 2011;7(2):650–61.
Fatouros DG, Bergenstahl B, Mullertz A. Morphological observations on a lipid-based drug delivery system during in vitro digestion. Eur J Pharm Sci. 2007;31(2):85–94.
Jenkins TC, Palmquist DL. Effect of added fat and calcium on in vitro formation of insoluble fatty-acid soaps and cell-wall digestibility. J Anim Sci. 1982;55(4):957–63.
Marounek M, Skrivanova E, Rada V. Susceptibility of Escherichia coli to C2–C18 fatty acids. Folia Microbiol (Praha). 2003;48(6):731–5.
Sassene PJ, Knopp MM, Hesselkilde JZ, et al. Precipitation of a poorly soluble model drug during in vitro lipolysis: characterization and dissolution of the precipitate. J Pharm Sci. 2010;99(12):4982–91.
Winkler FK, D’Arcy A, Hunziker W. Structure of human pancreatic lipase. Nature. 1990;343(6260):771–4.
Thomas N, Holm R, Mullertz A, Rades T. In vitro and in vivo performance of novel supersaturated self-nanoemulsifying drug delivery systems (super-SNEDDS). J Control Release. 2012;160(1):25–32.
Thomas N, Holm R, Garmer M, et al. Supersaturated self-nanoemulsifying drug delivery systems (Super-SNEDDS) enhance the bioavailability of the poorly water-soluble drug simvastatin in dogs. Aaps J. 2013;15(1):219–27.
Stillhart C, Durr D, Kuentz M. Toward an improved understanding of the precipitation behavior of weakly basic drugs from oral lipid-based formulations. J Pharm Sci. 2014;103(4):1194–203.
Thomas N, Richter K, Pedersen TB, et al. In vitro lipolysis data does not adequately predict the in vivo performance of lipid-based drug delivery systems containing fenofibrate. Aaps J. 2014;16(3):539–49.
Griffin BT, Kuentz M, Vertzoni M, et al. Comparison of in vitro tests at various levels of complexity for the prediction of in vivo performance of lipid-based formulations: case studies with fenofibrate. Eur J Pharm Biopharm. 2014;86(3):427–37.
Acknowledgments
This study results from a joint collaboration between members of the LFCS Consortium, which received funding from Capsugel, Gattefosse, Sanofi, Merck Serono, NiCox, Roche, Bristol-Myers Squibb, and Actelion.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sassene, P., Kleberg, K., Williams, H.D. et al. Toward the Establishment of Standardized In Vitro Tests for Lipid-Based Formulations, Part 6: Effects of Varying Pancreatin and Calcium Levels. AAPS J 16, 1344–1357 (2014). https://doi.org/10.1208/s12248-014-9672-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1208/s12248-014-9672-x