Abstract
Background
Childhood under-nutrition is far-reaching in low and middle-income nations. Undernutrition is one of the major open wellbeing concerns among newborn children and youthful children in Ethiopia. The present study aimed to explore the potential risk factors of undernutrition among children under 5 years of age in Somali Region, Ethiopia.
Methods
The data for this study was extricated from the Ethiopian Demographic and Health Survey (EDHS) 2016. The data collected from 1339 children born 5 years before was considered within the analysis. A multivariable binary logistic regression analysis was utilized at a 5% level of significance to decide the individual and community-level variables related to childhood malnutrition.
Results
The prevalence of stunting, underweight and wasting were 27.4, 28.7 and 22.7%, respectively. About 16.1% of children were both stunted and underweight; the extent of both being underweight and wasted was 11.7%, the prevalence of both stunted and wasted children was 5.5%, and all three malnutrition conditions were 4.7% children. Among the variables considered in this study, age of the child in months, type of birth, anemia level, size of child at birth, sex of the child, mothers’ BMI and sources of drinking water were significantly related to stunting, underweight and wasting in Somali Region.
Conclusions
The prevalence of stunting, underweight and wasting was relatively high. Undernutrition is one of the major open wellbeing concerns among children in Somali region. The impact of these variables ought to be considered to develop strategies for decreasing the lack of healthy sustenance due to undernutrition in the study areas. Hence, intercession should be centered on making strides for the under-nutrition determinant variables of the children to be solid, to improve the child’s wholesome status, and decrease child mortality quickly.
Similar content being viewed by others
Background
Adequate nutrition is essential in early childhood to ensure healthy growth, proper organ formation and function, a strong immune system, and neurological and cognitive development. Economic growth and human development require well-nourished populations who can learn new skills, think critically and contribute to their communities. Child malnutrition impacts cognitive function and contributes to poverty by impeding individuals’ ability to lead productive lives. In addition, it is estimated that more than one-third of under-five deaths are attributable to undernutrition [1, 2].
Nutrition has increasingly been recognized as a basic pillar for social and economic development. The reduction of infant and young child malnutrition is essential to the achievement of the Millennium Development Goals (MDGs) particularly those related to the eradication of extreme poverty and hunger (MDG 1) and child survival (MDG 4). Improving children’s nutrition requires effective and sustained multi-sectoral nutrition programming over the long term, and many countries are moving in the right direction [3].
Globally, an estimated 165 million children under 5 years of age, or 26%, were stunted, 101 million children under 5 years of age, or 16%, were underweight and 52 million children under 5 years of age, or 8%, were wasted. High prevalence levels of stunting among children under 5 years of age in Africa (36% in 2011) and Asia (27% in 2011) remain a public health problem, one which often goes unrecognized. More than 90% of the world’s stunted children live in Africa and Asia. Although the prevalence of stunting, underweight and wasting among children under 5 years of age worldwide has decreased since 1990, overall progress is insufficient and millions of children remain at risk [3].
Childhood under-nutrition is broad in low and middle-income nations. In these nations, it is an imperative and backhanded cause of child mortality. Around the world, stunting and wasting besides intrauterine development limitations are mindful of about 2.1 million deaths in under-five children that contain 21% of all deaths [2].
Undernutrition in children occurs due to the interplay of several factors, which include variables related to the maternal age, maternal education, poor feeding practice, maternal nutritional status, parity and multiple births, sex of the child, illness, birth interval and immunization status, poor wealth status, large families, water and sanitation, place of residence, and other factors relating to health services utilization [4,5,6,7]. Child under-nutrition and mortality rates are sensible reactions to both wellbeing programs and financial conditions such as pay, unemployment, and lack of education [8]. In Ethiopia, the predominance of under-nutrition is high [9,10,11,12,13] which ranges from 14.6% in Addis Ababa to 46.3% in Amhara region for stunting, 3.5% in Addis Ababa to 22.5% in Somalia region for wasting and 5% in Addis Ababa to 35.5% in Somali region for underweight [14].
Although a few studies have been carried out on the identification of factors that are associated with children under 5 years old of undernutrition in the Somali region, none of them uses the nationally representative data for the Somali region. The exertion made in decreasing under-five children’s undernutrition in the region is still high, and more effort is required to move forward the obstructions for advance diminishment. More research studies are, subsequently, required to inform policymakers to execute suitable mediation programs. To address these gaps, an all-inclusive cross-sectional analysis of the recent 2016 Ethiopian Demographic Health Survey (EDHS) was done, to explore the potential risk factors of undernutrition among under-five children in Somali region, Ethiopia.
Methods
Description of study design and area
A cross-sectional study design was used for this study. The study was conducted in Somali regional state which is located in the east and southeast of Ethiopia. According to the 2007 Census, the state’s population was 4,439,147 of which 1,970,363 were males. The urban residents of the region were 621,210 and its rural residents 3,817,937 [15].
Data sources
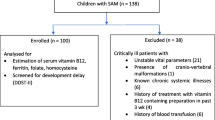
The data for this study was extracted from the Ethiopian Demographic and Health Survey (EDHS) 2016. The Central Statistics Agency (CSA), the Ministry of Health (MOH), and the Ethiopian Public Health Institute together surveyed from January 18, 2016–June 27, 2016, where the United States Agency for International Development (USAID) funded the project. The authors have got permission from the ICF-DHS program to use the EDHS data and access it through https://www.dhsprogram.com/data/dataset_admin/login_main.cfm. The 2016 EDHS used a two-stage stratified sampling to select households. In the first stage, there were 645 enumeration areas (202 in urban and 443 in rural areas). 1339 (700 males and 639 females) under-five children from Somali region were considered for this study. This study considered live children age 0–59 months with anthropometry data in the analysis of determinants of nutritional status among children under age 5 in Somali region. Missing values in the 2016 EDHS dataset were not included in the analyses.
Variables of the study
The subordinate factors for this consideration were the malnutrition status of under-5 year children (stunting, underweight and wasting). Children whose height-for-age Z-score is below minus two standard deviations (− 2SD) from the median of the reference population is considered as stunted. If the weight-for-age Z-score is below minus two standard deviations (− 2 SD) from the medium of reference population then the child is underweight. Children whose weight for height Z-score is below minus two standard deviations (−2SD) from the median of the reference population are considered as wasted [16]. Illustrative factors were chosen after conducting a point-by-point writing survey [16,17,18,19,20,21] additionally accessible with complete data in the EDHS, 2016 data set was included within the current investigation. Selected illustrative factors were divided into two levels which included socio-demographic-maternal and child-level variables. Socio demographic-maternal variables chosen were types of residence, household wealth index, mother’s educational level, mother’s body mass index (BMI), religion, and type of toilet facility, sex of household head and sources of drinking water. Child-level components were the sex of the child, child age, type of birth, number of living children and child size at birth. Malnutrition indicators were defined using the WHO child growth standards [22].
Statistical data analysis
The data was extracted, edited, and analyzed by using SPSS version 23 for Windows. Descriptive statistics such as frequencies and proportions were used to summarize the distribution of selected background characteristics of the sample. Bivariate logistic regression was performed to analyze the crude odds ratio and a variable with a P-value of less than 0.25 was transported into multivariable binary logistic regression analyses to analyze adjusted odds ratio and to identify the determinants of undernutrition of children under 5 years old. The dependent variables for bivariate and multivariable logistic regression analyses were stunting, wasting and underweight. Finally, variables with P-values < 0.05 in the multivariable logistic regression model were taken as statistically significant.
Results
In this study, a total of 1339 under-five children were included. In the Somali region, the prevalence of stunting, underweight and wasting were 27.4, 28.7 and 22.7%, respectively. Almost 16.1% of children were both stunted and underweight; the prevalence of underweight and wasting was 11.7%, the prevalence of stunted and wasted was 5.5%, and all three malnutrition conditions were only 4.7% children. Among the total participants, 555 children (41.4%) were 0–24 months old, 501 (37.4%) were 25–47 months old and 283 (21.1%) were 48–59 months old. From the total participants, male children constituted 700 of the sample population (52.3%), and nearly 1069 (79.8%) of the children were taken from rural areas while. The majority of the children (62.4%) were anemic; most children were born in single birth type (98.2%). The majority of children (56.5%) were born from overweight mothers, 24.6% of children were from normal-weight mothers and only 18.8% of children were from underweight mothers. Regarding the educational status of the household, 85.4% of households did not attend at all, 10.7% of households attended primary school and 3.8% of households attended secondary and higher education. The majority (63.8%) of the children were born at normal size, 32.3% were large and 24.6% of the children were born in small size at birth. More than half (63.8%) of the respondents had no toilet facilities; from the total participants, one thousand ninety-seven (81.9%) children were from the household who used unimproved water sources. The majority of children (75.8%) were born from poor wealth index families, 18.4% of children were from rich wealth index family and the rest 5.8% of children were from medium wealth index families. The number of children who lived in household members of 1–2, 3–4 and > 4 was 20.9, 30.4 and 48.7%, respectively. More than half of the respondents (67.8%) were male household-headed.
Factors associated with stunting
According to the multivariable logistic regression analysis, age of the child, type of birth, toilet facility and anemia level was significantly associated with being stunted. The risk of being stunted was 1.94 times more likely among children that were aged 25–47 months as compared to those aged 0–24 months (AOR = 1.94; 95% CL: 1.41–2.69). The risk of being stunted was 1.66 times more likely among children that were aged 48–59 months as compared to those aged 0–24 months (AOR = 1.66; 95% CL: 1.12–2.46). The odds of stunting among children who were born in multiple-birth types were 2.86 times higher as compared to those born in single birth type (AOR = 2.86; 95% CL: 1.10–7.37). Children from the household who had not toilet facility were 1.45 times more likely to be stunted as compared to the children household who had a toilet facility (AOR = 1.45; 95% CL: 1.12–1.87). Being stunted of anemic children was 2.36 times more likely to be stunted as compared to non-anemic children (AOR = 2.36; 95% CL: 1.55–3.61) (Table 1).
Factors associated with underweight
Results of the multivariable binary logistic regression model revealed that the age of a child, size of child at birth, and anemia level were significantly associated with underweight. The children who were 25–47 months aged groups were 1.67 times more likely to develop underweight as compared to those who were 0–24 months aged groups (AOR = 1.67; 95% CL: 1.22–2.28). The children who were 48–59 months aged groups were 1.70 times more likely to develop underweight as compared to those who were 0–24 months aged groups (AOR = 1.70; 95% CL: 1.17–2.46). Compared to children of a large size at birth, the odds of underweight among children in the small size at birth was 1.55 times higher (AOR = 1.55; 95% CL: 1.08–2.21). The anemic children were 1.65 times more likely to be underweight as compared to non-anemic children (AOR = 1.65; 95% CL: 1.12–2.43) (Table 2).
Factors associated with wasting
Based on multivariable logistic regression analysis, sex of the child, Mothers’ BMI, size of child at birth and sources of drinking water were significantly associated with wasting. The results of the adjusted odds ratio showed that male children were 0.35 times less likely to be wasting compared to female children (AOR = 0.65; 95% CL: 0.48–0.88). The risk of being wasted among children who were born from underweight mothers was 1.64 times higher compared to those born from overweight mothers (AOR = 1.64; 95% CL: 1.03–2.64). The children who had small size at birth were 1.58 times more likely to be wasting compared to those who had large size at birth (AOR = 1.58; 95% CL: 1.07–2.31). Children whose household used unimproved water were 1.66 times more likely to be wasted as compared to the children household used improved water (AOR = 1.66; 95% CL: 1.44–3.98) (Table 3).
Discussion
In this study, the prevalence of stunting in the present study was 27.4%. This prevalence is lower than the previous studies conducted in in Ethiopia (38.3%) [16], in Shabelle zone, in Shinille District (33.4%) [23], in Tigray region 39.1% [24], Takusa District (36.5%) [25], in rural Ethiopia (41.2%) [26], in east Gojjam Zone (44.7%) [27], in Tigray region (46.9%) [11] and in Hidabu Abote District (47.6%) [28], but it was higher than the study conducted in the Bure Town of West Gojjam Zone (24.9%) [29]. Similar studies conducted in Nairobi Peri-Urban Slum and Nigeria reported a higher prevalence of stunting (30.2%) [30] and (47.6%) [31], respectively. The variation might be due to socioeconomic, geographical characteristics of the study area, cultural differences in dietary habits and care practices.
In the present study, the prevalence of underweight was 28.7%. The prevalence of underweight in this finding is higher than the studies conducted in Ethiopia (23.3%) [16], in Tigray (23.9%) [24], Dale district (19%) [32], Takusa District (19.5%) [25], in rural Ethiopia (27%) [26], in east Gojjam Zone (15.30%) [27] and the Bure Town of West Gojjam Zone (14.30%) [29], but it is lower than the study conducted in Hidabu Abote District (30.9%) [28]. The lower prevalence of underweight was reported in Nairobi Peri-Urban Slum (14.9%) [30] and Nigeria (25.6%) [31]. This could be because the households lack knowledge, attitude and practices (KAP) on how to feed their children and themselves [33].
The prevalence of wasting was 22.7%. The prevalence of wasting in the present study is higher compared to the study conducted in Ethiopia (10.1%) [16], in Haramaya district (10.7%) [34], in Tigray region (11.6%) [11], in Dale district (14%) (32), in Pakistan (10.7%) [33], Nairobi Peri-Urban slum (4.5%) [30], and (16.7%) [28], in the Bure Town of West Gojjam Zone (11.1%) [29] and in east Gojjam Zone (10%) [27]. In general, this high prevalence of wasting could be due to repeated attacks of drought and famine in the study area.
According to the multivariable logistic regression analysis, age of the child, type of birth, toilet facility and anemia level was significantly associated with being stunted. The risk of being stunted was 1.94 and 1.66 times more likely among children that were aged 25–47 and 48–59 as compared to those aged 0–24 months, respectively. This finding is in line with the studies conducted in Ethiopia [16], in Haramaya district [34], in Pakistan [33], in Amhara region [35] and Kilimanjaro Region, Tanzania [36]. This could be because younger children are more likely to receive more attention and feeding effort from their parents as compared to older children [37]. It could also be due to the inappropriate and late introduction of low nutritional quality supplementary food [38]. The risk of being stunted among children who were born in multiple-birth types was 2.86 times higher as compared to those born in single birth types. This finding is consistent with the study carried out in Tigray region [24]. The reason behind might be in multiple birth types, there could be food competition between children and it leads to malnutrition; and the mothers’ breast may not produce enough milk for both children. Children from the household who had not toilet facility were 1.45 times more likely to be stunted compared to the children household that had a toilet facility. This result is in contradiction to the studies conducted in Tigray region [24] and in Bule Hora district, South Ethiopia [39]. This might be because lack of toilet facility is the main cause for intestinal parasites and microorganisms which leads to loss of appetite leading to poor nutritional status; this might repeated infection causes depressed immunity and making the severity and duration of disease more severe contributing to the poor nutritional status of the children. Being stunted of anemic children was 2.36 times more likely to be stunted as compared to non-anemic children. This finding has supported the study conducted in Ethiopia [16]. Undernourished children are more suffered from inadequate bioavailability of micronutrients such as iron, B12 and folate in their body which are important for the formation of blood cells. Therefore, those children who are undernourished cannot form adequate blood cells as much as required; consequently the this leads to the development of nutritional deficiency anemia which is common especially in developing countries [40].
The children who were 25–47 and 48–59 aged groups were 1.67 and 1.70 times more likely to develop underweight as compared to those who were 0–24 aged groups. This finding is supported by the study conducted in Ethiopia [16], but in contradiction to the study conducted in Tigray region [24] and in Pakistan [33]. This might be due to the fact that as children grow older, they may have less access to attention and not provide sufficient food by their families. It might be due to a large portion of guardians in rural areas are ignoring to meet their children’s optimal food requirements like the age of the child increases [41]. Compared to children of a large size at birth, the odds of underweight among children in the small size at birth was 1.55 times higher. This study is in line with the study conducted in Tigray region [24] and in Pakistan [33]. Children with low birth sizes are often disadvantaged in terms of physical growth and are also more vulnerable to infections compared to children born with normal birth sizes [42]. The anemic children were 1.65 times more likely to be underweight as compared to non-anemic children. This might be due to the fact that the communities in the study area consume cereals that have low iron content [43].
The results of the adjusted odds ratio showed that the sex of the child was significantly associated with wasting. Wasting is a relatively short-term condition, which means that an individual child can be affected more than once in a year [44]. Male children were 0.35 times less likely to be wasting compared to female children. This finding is consistent with finding in Tigray region [24], but previous studies indicated that boys had a significantly worse nutritional status than girls [24]. This could probably be due to the value and cultural preferences placed on the male child. As such, they are likely to be better fed as compared to the girl child. This has also been shown in other Sub-Saharan African countries [45]. The risk of being wasting among children who were born from underweight mothers was 1.64 times higher compared to those born from overweight mothers. This study is in line with findings in Pakistan [33], Ethiopia [16], India [46] and Vietnam [47]. This finding is also similar to other previously conducted studies [34, 48]. This could be explained by the presence of an intergenerational link between maternal and child nutrition means a small mother will have small babies who in turn grow to become small mothers [49]. Maternal BMI is also an important determinant of child under-nutrition and is influenced by maternal nutrition, to improve child growth, proper nutrition is essential for the mothers during the prenatal and postnatal period. Healthier mothers have less risk of having undernourished children [18]. The children who had small sizes at birth were 1.58 times more likely to be wasting compared to those who had large sizes at birth. This result is supported by the study conducted in Tigray region [24]. Children whose households used unimproved water were 1.66 times more likely to be wasting as compared to the children household used improved water. This finding is supported by finding in Haramaya District, Eastern Ethiopia [34]. This might be due to the fact that impure water is a vehicle for intestinal parasites which leads to loss of appetite leading to poor nutritional status; this might repeated infection causes depressed immunity and making the severity and duration of disease more severe contributing to the poor nutritional status of the children.
Conclusion
This study revealed individual- and community-level factors that determined childhood malnutrition in Somali region children. Among the factors considered in this study, age of the child in months, type of birth, anemia level, size of child at birth, sex of the child, mothers’ BMI and sources of drinking water were significantly associated with stunting, underweight and wasting. The authors concluded that under-nutrition among under-five children was one of the public health problems in the study area. Thus, interventions should be focused on 25–59 months age of children, multiple birth type, anemic children, and small size of child at birth, female children, underweight mothers and improving access to improved drinking water to get better health care, to enhance the child’s nutritional status, and reduce child mortality more rapidly.
Availability of data and materials
Data will be available upon request from the corresponding author.
Abbreviations
- AOR:
-
Adjusted odds ratio
- BMI:
-
Body mass index
- COR:
-
Crude odds ratio
- CSA:
-
Central Statistical Agency
- SPSS:
-
Statistical Package for Social Science
- DHS:
-
Demographic and Health Surveys
- EDHS:
-
Ethiopian Demographic and Health Survey
References
Liu L, Johnson HL, Cousens S, Perin J, Scott S, Lawn JE, et al. Global, regional, and national causes of child mortality: an updated systematic analysis for 2010 with time trends since 2000. Lancet. 2012;379(9832):2151–61. https://doi.org/10.1016/S0140-6736(12)60560-1.
Black RE, Allen LH, Bhutta ZA, Caulfield LE, de Onis M, Ezzati M, et al. Maternal and child undernutrition: global and regional exposures and health consequences. Lancet. 2008;371(9608):243–60. https://doi.org/10.1016/S0140-6736(07)61690-0.
United Nations Children's Fund, WHO, The World Bank, UNICEF-WHO. World Bank joint child malnutrition estimates. New York: UNICEF; 2012.
Black RE, Allen LH, Bhutta ZA, Caulfield LE, de Onis M, Ezzati M, Mathers C, Rivera J; Maternal and Child Undernutrition Study Group. Maternal and child undernutrition: global and regional exposures and health consequences. Lancet. 2008;371(9608):243-60. https://doi.org/10.1016/S0140-6736(07)61690-0.
Müller, O, M. Krawinkel. Malnutrition and health in developing countries. CMAJ. 2005; 173(3): p. 279–286, DOI: https://doi.org/10.1503/cmaj.050342.
Younis K, Ahmad S, Badpa A. Malnutrition: causes and strategies. J Food Process Technol. 2015;6(434):2.
Younis K, Ahmad S, Badpa A. Malnutrition: Causes and Strategies. J Food Process Technol. 2015;6:434.https://doi.org/10.4172/2157-7110.1000434.
El-Ghannam AR. The global problems of child malnutrition and mortality in different world regions. J Health Soc Policy. 2003;16(4):1–26. https://doi.org/10.1300/J045v16n04_01.
Mulugeta A, Hagos F, Kruseman G, Linderhof V, Stoecker B, Abraha Z, et al. Child malnutrition in Tigray, northern Ethiopia. East Afr Med J. 2010;87(6):248–54. https://doi.org/10.4314/eamj.v87i6.63083.
Edris M. Assessment of nutritional status of preschool children of Gumbrit, north West Ethiopia. Ethiop J Health Dev. 2007;21(2):125–9.
Wollo E. Risk factors for child under-nutrition with a human rights edge in rural villages of North Wollo, Ethiopia. East Afr Med J. 2005;82(12):625–30.
Tarekegn SM, Lieberman LS, Giedraitis V. Determinants of maternal health service utilization in Ethiopia: analysis of the 2011 Ethiopian Demographic and Health Survey. BMC Pregnancy Childbirth. 2014;14(1):161.
Muchie KF. Quality of antenatal care services and completion of four or more antenatal care visits in Ethiopia: a finding based on a demographic and health survey. BMC Pregnancy Childbirth. 2017;17(1):1–7.
Wolde HF, Gonete KA, Akalu TY, Baraki AG, Lakew AM. Factors affecting neonatal mortality in the general population: evidence from the 2016 Ethiopian demographic and health survey (EDHS)—multilevel analysis. BMC Res Notes. 2019;12(1):610. https://doi.org/10.1186/s13104-019-4668-3.
Edris, M. Assessment of nutritional status of preschool children of Gumbrit, North West Ethiopia. Ethiopian Journal of Health Development. African Journals Online. 2007;21(2):125-9.
Tekile AK, Woya AA, Basha GW. Prevalence of malnutrition and associated factors among under-five children in Ethiopia: evidence from the 2016 Ethiopia demographic and health survey. BMC Res Notes. 2019;12(1):391. https://doi.org/10.1186/s13104-019-4444-4.
Tariq J, Sajjad A, Zakar R, Zakar M, Fischer F. Factors associated with undernutrition in children under the age of two years: secondary data analysis based on the Pakistan demographic and health survey 2012–2013. Nutrients. 2018;10(6):676. https://doi.org/10.3390/nu10060676.
Talukder A. Factors associated with malnutrition among under-five children: illustration using Bangladesh demographic and health survey, 2014 data. Children. 2017;4(10):88. https://doi.org/10.3390/children4100088.
Asim M, Nawaz Y. Child malnutrition in Pakistan: evidence from literature. Children. 2018;5(5):60.
Das S, Gulshan J. Different forms of malnutrition among under five children in Bangladesh: a cross sectional study on prevalence and determinants. BMC Nutr. 2017;3(1):1–12. https://doi.org/10.1186/s40795-016-0122-2.
Akombi BJ, Agho K, Merom D, Hall J, Renzaho A. Multilevel analysis of factors associated with wasting and underweight among children under-five years in Nigeria. Nutrients. 2017;9(1):44. https://doi.org/10.3390/nu9010044.
Tekile AK, Woya AA, Basha GW. Prevalence of malnutrition and associated factors among under-five children in Ethiopia: evidence from the 2016 Ethiopia demographic and health survey. BMC Res Notes. 2019;12(1):1–6.
Ma’alin A, et al. Magnitude and factors associated with malnutrition in children 6–59 months of age in Shinille Woreda, Ethiopian Somali regional state: a cross-sectional study. BMC Nutr. 2016;2(1):1–12.
Woldeamanuel BT, Tesfaye TT. Risk factors associated with under-five stunting, wasting, and underweight based on Ethiopian demographic health survey datasets in Tigray region, Ethiopia. J Nutr Metab. 2019;2019:1–11. https://doi.org/10.1155/2019/6967170.
Nigatu G, Assefa Woreta S, Akalu TY, Yenit MK. Prevalence and associated factors of underweight among children 6–59 months of age in Takusa district, Northwest Ethiopia. Int J Equity Health. 2018;17(1):106. https://doi.org/10.1186/s12939-018-0816-y.
Endris N, Asefa H, Dube L. Prevalence of malnutrition and associated factors among children in rural Ethiopia. Biomed Res Int. 2017.
Zeray A, Kibret GD, Leshargie CT. Prevalence and associated factors of undernutrition among under-five children from model and non-model households in east Gojjam zone, Northwest Ethiopia: a comparative cross-sectional study. BMC Nutr. 2019;5(1):27.
Mengistu K, Alemu K, Destaw B. Prevalence of malnutrition and associated factors among children aged 6–59 months at Hidabu Abote District, North Shewa, Oromia Regional State. J Nutr Disorders Ther. 2013;1:1–15.
Wollo, E. Risk factors for child under-nutrition with a human rights edge in rural villages of North Wollo, Ethiopia. East African medical journal. 2005;82(12):625-30.
Chesire E, et al. Determinants of under nutrition among school age children in a Nairobi peri-urban slum. East Afr Med J. 2008;85(10):471–9.
Emmanuel, A, et al. Malnutrition and associated factors among underfive in a Nigeria local government area. 2016.
Wolde M, Berhan Y, Chala A. Determinants of underweight, stunting and wasting among schoolchildren. BMC Public Health. 2015;15(1):8.
Khan S, Zaheer S, Safdar NF. Determinants of stunting, underweight and wasting among children< 5 years of age: evidence from 2012–2013 Pakistan demographic and health survey. BMC Public Health. 2019;19(1):358.
Yisak H, Gobena T, Mesfin F. Prevalence and risk factors for under nutrition among children under five at Haramaya district, Eastern Ethiopia. BMC Pediatr. 2015;15(1):212.
Kebede D, Merkeb Y, Worku E, Aragaw H. Prevalence of undernutrition and potential risk factors among children under 5 years of age in Amhara region, Ethiopia: evidence from 2016 Ethiopian demographic and health survey. J Nutr Sci. 2021;10:E22. https://doi.org/10.1017/jns.2021.1.
Mgongo M, Chotta N, Hashim T, Uriyo J, Damian D, Stray-Pedersen B, et al. Underweight, stunting and wasting among children in Kilimanjaro region, Tanzania; a population-based cross-sectional study. Int J Environ Res Public Health. 2017;14(5):509. https://doi.org/10.3390/ijerph14050509.
Gudu E, et al. Factors associated with malnutrition in children< 5 years in western Kenya: a hospital-based unmatched case control study. BMC Nutr. 2020;6(1):1–7.
Dasgupta A, et al. Assessment of under nutrition with composite index of anthropometric failure (CIAF) among under-five children in a rural area of West Bengal. Indian J Community Health. 2014;26(2):132–8.
Asfaw M, Wondaferash M, Taha M, Dube L. Prevalence of undernutrition and associated factors among children aged between six to fifty nine months in Bule Hora district, South Ethiopia. BMC Public Health. 2015;15(1):41. https://doi.org/10.1186/s12889-015-1370-9.
De Benoist, B, et al. Worldwide prevalence of anaemia 1993–2005; WHO global database of anaemia. 2008.
Khan REA, Raza MA. Determinants of malnutrition in Indian children: new evidence from IDHS through CIAF. Qual Quant. 2016;50(1):299–316. https://doi.org/10.1007/s11135-014-0149-x.
Christian P, Lee SE, Donahue Angel M, Adair LS, Arifeen SE, Ashorn P, et al. Risk of childhood undernutrition related to small-for-gestational age and preterm birth in low-and middle-income countries. Int J Epidemiol. 2013;42(5):1340–55. https://doi.org/10.1093/ije/dyt109.
Engidaye G, et al. Under nutrition, maternal anemia and household food insecurity are risk factors of anemia among preschool aged children in Menz Gera Midir district, eastern Amhara, Ethiopia: a community based cross-sectional study. BMC Public Health. 2019;19(1):1–11.
Isanaka S, Andersen CT, Cousens S, Myatt M, Briend A, Krasevec J, et al. Improving estimates of the burden of severe wasting: analysis of secondary prevalence and incidence data from 352 sites. BMJ Glob Health. 2021;6(3):e004342. https://doi.org/10.1136/bmjgh-2020-004342.
Keino S, Plasqui G, Ettyang G, van den Borne B. Determinants of stunting and overweight among young children and adolescents in sub-Saharan Africa. Food Nutr Bull. 2014;35(2):167–78. https://doi.org/10.1177/156482651403500203.
Kumar D, Goel NK, Mittal PC, Misra P. Influence of infant-feeding practices on nutritional status of under-five children. Indian J Pediatr. 2006;73(5):417–21. https://doi.org/10.1007/BF02758565.
Hien NN, Hoa NN. Under three years of age in nghean, Vietnam Pakistan. J Nutr. 2009;8(7):958–64. https://doi.org/10.3923/pjn.2009.958.964.
Siddiqi MNA, Haque MN, Goni MA. Malnutrition of under-five children: evidence from Bangladesh. Asian J Med Sci. 2011;2(2):113–9. https://doi.org/10.3126/ajms.v2i2.3662.
Genebo T, et al. The association of children’s nutritional status to maternal education in Zigbaboto, Guragie Zone. Ethiop J Health Dev. 1999;13(1):55–6111.
Acknowledgments
The authors would like to thank Ethiopia Central Statistical Agency for permitting us to use the data for our study.
Funding
Fund was not obtained for this study.
Author information
Authors and Affiliations
Contributions
D.K. and A.A. conceived the idea, draft the manuscript and interpreted the results. D.K. and A.A. also performed the statistical analysis, help in results interpretation and critically reviewed the manuscript. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethics approval and consent to participate The EDHS 2016 has taken into account the standard ethical guidelines of the measure DHS program. The authors have obtained the data from the measure DHS website (https://www.dhsprogram.com/data/dataset_admin/index.cfm) following their data obtaining procedure. The formal ethical clearance was obtained from the Demographic and Health Surveys (DHS) program. Based on DHS official letter, all methods were carried out in accordance with relevant guidelines and regulations. All experimental protocols were approved by Ethiopian Public Health Institute office. Informed consent was obtained from a parent and/or legal guardian.
Consent for publication
Not applicable as no personal data was used in this article.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Kebede, D., Aynalem, A. Prevalence of undernutrition and potential risk factors among children below five years of age in Somali region, Ethiopia: evidence from 2016 Ethiopian demographic and health survey. BMC Nutr 7, 56 (2021). https://doi.org/10.1186/s40795-021-00460-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40795-021-00460-0