Abstract
Aim
To compare the efficacy and safety of endoscopic resection (ER) and surgery for the treatment of early gastric cancer and precancerous lesions.
Methods
Databases, such as PubMed, EMBASE, Cochrane Library, and Science Citation Index, from 2000 to 2016, were searched for eligible articles. In this meta-analysis, the main outcome measurements were local recurrence, complications, metachronous lesions, hospital stay, and 5-year overall survival.
Results
Nine trials were identified and a total of 2748 patients were included. The rate of complication was higher in the surgery group compared with the ER group (OR 0.41; 95 % CI 0.30–0.55). The rates of local recurrence and metachronous lesions were lower in the surgery group (OR 0.03; 95 % CI 0.00–0.06; OR 8.76; 95 % CI 4.17–18.41). The hospital stay was shorter in the ER group (mean difference −6.96; 95 % CI −7.94 to −5.99). The 5-year overall survival rate did not significantly differ between the two groups (OR 1.23; 95 % CI 1.03–1.47).
Conclusions
We provided evidence that, ER was comparable to surgery in terms of the 5-year overall survival. In addition, ER had a lower rate of complications and shorter hospital stay, but a higher rate of local recurrence and metachronous lesions for the treatment of early gastric cancer and precancerous lesions.
Similar content being viewed by others
Background
Gastric cancer is the second most common cause of cancer-related death in the world, and it remains difficult to cure, primarily because most patients present with advanced disease. Early gastric cancer is defined as gastric carcinoma confined to the mucosa and submucosa of the stomach, with or without regional lymph node metastasis (Japanese Gastric Cancer Association 1998, 2011).
Gastrectomy with lymph node dissection remains the standard therapy for early gastric cancer. A variety of complications can develop after surgery, and the patient’s quality of life can be greatly impacted because of the modification of the stomach (Okamura et al. 1988).
Endoscopic resection (ER) methods, such as endoscopic mucosal resection (EMR) and endoscopic submucosal dissection (ESD), are widely accepted for the treatment of superficial gastric cancer without lymph node metastasis, because of the minimal invasion, low cost, good patient tolerance, and better quality of life after the operation, with low adverse event rates (El-Sedfy et al. 2014; Shen et al. 2013).
There is no current consensus on the optimal method for the treatment of early gastric cancer and precancerous lesions. We conducted a systematic literature review to compare the efficacy and safety of ER and surgical methods for the treatment of early gastric cancer and precancerous lesions.
Methods
Data sources and searches
We searched databases including PubMed, EMBASE, the Cochrane Library, and Science Citation Index from January 2000 to March 2016 to identify related articles, without language restriction, which compared ER and surgery. All bibliographies were indentified in the reference lists. The search terms were “gastric cancer or gastric neoplasia” and “endoscopic mucosal resection or endoscopic submucosal dissection”. Major proceedings of international meetings (such as Digestive Disease Week and Asian Pacific Digestive Week) were also hand-searched.
Study selection
The inclusion and exclusion criteria are shown in Table 1.
Data extraction and quality assessment
Data were extracted by one investigator and confirmed by the other according to a predefined data extraction form. Disagreements were resolved by consultation with a third investigator. The following data were collected: year of publication, first author, country, duration, age, sex, depth of invasion, differentiation and follow up period, the local recurrence rate, procedure-related complications, metachronous lesions, hospital stay, and 5-year overall survival. The Newcastle-Ottawa Scale was used to assess the quality of the included non-randomized studies (Wells et al. 2015).
Statistical analysis
All extracted data were entered in the freeware program Review Manager (Version 5.0 for Windows, Cochrane Collaboration). The weighted mean difference was recommended for continuous data, and the odds ratio (OR) with 95 % confidence intervals (CI) was recommended for dichotomous data. Statistical heterogeneity between trials was evaluated by the Chi square test and was considered to be present when P was less than 0.1. We also used I2 to assess the heterogeneity. An I2 of more than 50 % was considered to be statistically significant. In the presence of statistical heterogeneity, heterogeneity was explored by subgroup analysis or a random-effects model. Publication bias was detected by a funnel plot, and then the symmetry of the funnel plot was confirmed by the Egger’s test, with a P value of 0.05.
Results
Study selection
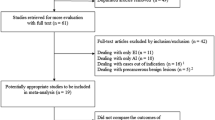
A total of 2251 potential studies were retrieved for the meta-analysis. 1675 were excluded for not including the surgical treatment and 565 were excluded because ER and surgery were not compared. Of the 11 remaining articles, 2 were excluded because they had not compared the main outcomes. The remaining 9 eligible studies (Cho et al. 2015; Song et al. 2015; Choi et al. 2011, 2015; Kim et al. 2014, 2015; Park et al. 2014; Chung et al. 2014; Chiu et al. 2012) were chosen for further analysis (Fig. 1). A total of 2748 patients were included in the meta-analysis, including 1339 patients in the ER group and 1409 patients in the surgery group. Of these studies, 6 included only patients with ESD (Cho et al. 2015; Song et al. 2015; Park et al. 2014; Kim et al. 2014; Chung et al. 2014; Chiu et al. 2012), 1 included only patients with EMR (Choi et al. 2011), and 2 included patients with both ESD and EMR (Choi et al. 2015; Kim et al. 2015). Open surgery or laparoscopic surgery were mentioned in 5 studies (Choi et al. 2015; Kim et al. 2014, 2015; Chung et al. 2014; Chiu et al. 2012), while the other 4 studies did not describe the specific operation method (Cho et al. 2015; Song et al. 2015; Park et al. 2014; Choi et al. 2011). All of the studies were retrospective case–control studies, not randomized controlled trials (RCTs). The key characteristics of the studies are listed in Table 2.
Local recurrence
The local recurrence rates were reported in 7 studies (Cho et al. 2015; Song et al. 2015; Choi et al. 2011, 2015; Park et al. 2014; Kim et al. 2014; Chung et al. 2014). A random effect model was applied because of the heterogeneity (P < 0.00001, I2 = 87 %). The analysis showed that the local recurrence rate was higher in the ER group (34/1064) than in the surgery group (8/1062) (OR 0.03; 95 % CI 0.00–0.06) (Fig. 2). When the study from China was excluded (Song et al. 2015), heterogeneity still existed (P < 0.00001, I2 = 90 %).
Complications
Complications were reported in 8 studies (Cho et al. 2015; Song et al. 2015; Choi et al. 2011, 2015; Kim et al. 2014, 2015; Park et al. 2014; Chiu et al. 2012). There was no heterogeneity among the studies (P = 0.12, I2 = 39 %). A fixed effect model was applied, and the subsequent analysis showed that the rate of complications was lower in the ER group (70/1263) than in the surgery group (149/1160) (OR 0.41; 95 % CI 0.30–0.55) (Fig. 3).
Metachronous lesions
Metachronous lesions were reported in 6 studies (Cho et al. 2015; Kim et al. 2014, 2015; Park et al. 2014; Chung et al. 2014; Choi et al. 2011). There was no heterogeneity in the studies (P = 0.85, I2 = 0 %), and a fixed effect model was applied. The rate of metachronous lesions was higher in the ER group (58/939) compared with the surgery group (8/1181) (OR 8.76; 95 % CI 4.17–18.41) (Fig. 4).
Hospital stay
The hospital stay was reported in 3 studies (Cho et al. 2015; Song et al. 2015; Kim et al. 2014). There was no heterogeneity in the studies (P = 0.95, I2 = 0 %), and a fixed effect model was applied. The mean hospital stay was significantly shorter in the ER group, compared with the surgery group (Mean difference −6.96; 95 % CI −7.94 to −5.99) (Fig. 5).
5-Year overall survival
The 5-year overall survival was reported in 5 studies (Cho et al. 2015; Song et al. 2015; Choi et al. 2011, 2015; Kim et al. 2015; Park et al. 2014). There was no heterogeneity in these studies (P = 0.33, I2 = 13 %), and a fixed effect model was applied. Analysis showed that there was no significant difference in the 5-year overall survival rate between the ER group and the surgery group (OR 1.23; 95 % CI 1.03–1.47) (Fig. 6).
Publication bias
We used the local recurrence rate as the outcome, and no publication bias was detected by funnel plot and the Egger’s test (P = 0.862).
Discussion
The comparison between ER and surgery in the treatment of early gastric cancer is still controversial. Even though ER is less invasive and less expensive, and could better preserve the physiological function of the stomach, additional surgery with lymph node dissection is recommended when ER is histologically non-curative or submucosal invasion is detected regardless of margin status because of possible residual tumors or lymph node metastasis (Oda et al. 2008; Song et al. 2008).
Therefore, we designed the meta-analysis to systematically evaluate the two techniques, providing evidence for the optimal treatment of early gastric cancer. In the present analysis, 9 retrospective studies were included, and the results confirmed that compared with surgery, ER had a higher rate of local recurrence and metachronous lesions for the treatment of early gastric cancer and precancerous lesions. Because the ER method preserves the whole stomach, the incidence of local recurrence and metachronous lesions after ER was higher than after surgery (Nakajima et al. 2006; Takeda et al. 1998; Hosokawa et al. 2002). In most cases, local recurrent and metachronous lesions were successfully cured with additional endoscopic treatments. That is why there was no significant difference in the 5-year overall survival rate between the two groups.
The complications of ER included bleeding and perforation, which can be managed using endoscopic treatment. The complications that occurred after gastrectomy included bleeding, duodenal leakage, ileus and hepatic dysfunction, and pancreatic leakage. 5 studies provided the data of the complication rate for EGC. The pooled analysis showed that it was higher in the surgery group than the ER group.
Five studies compared the hospital stay between the two groups, three studies provided the data of mean ± SD, and the mean hospital stay was significantly shorter in the ER group, compared with the surgery group.
Two studies (Choi et al. 2011; Kim et al. 2014) compared the medical cost between the two groups. The results showed that ER patients had lower medical costs than patients who had conventional surgeries for early gastric cancer. Choi et al. (2015) reported that endoscopic treatment for EGC provides a better quality of life, but stomach preservation might provoke cancer recurrence worries.
There is an alternative therapeutic approach for the treatment of early gastric cancer which combines the advantages of both surgical and endoscopic treatment also known as laparoscopic endoscopic cooperative surgery (LECS) which was introduced in 2009. It was reported that LECS held great promise for the future of minimally invasive oncologic procedures for the treatment of early gastric cancer (Ntourakis and Mavrogenis 2015). It can be used as an alternative to endoscopic therapy and surgical treatment.
There were certain limitations in our analysis. First, the major limitation of this meta-analysis was that none of the included studies were randomized. This certainly attenuated the evidence level and value of this meta-analysis. Second, included studies were from only 2 countries, Korea and China, so the results need further confirmation in other countries.
In conclusion, based on the findings of our meta-analysis, ER showed advantages over surgery for early gastric cancer and precancerous lesions regarding the procedure-related complication rate and hospital stay. The disadvantages of ER were the higher rate of local recurrence and metachronous lesions. Fortunately, we can treat these with additional endoscopic treatments without affecting overall survival. In the view of the present meta-analysis and all available trials, we suggest that ER is appropriate to most early gastric cancer and precancerous lesions.
References
Chiu PW, Teoh AY, To KF, Wong SK, Liu SY, Lam CC, Yung MY, Chan FK, Lau JY, Ng EK (2012) Endoscopic submucosal dissection (ESD) compared with gastrectomy for treatment of early gastric neoplasia: a retrospective cohort study. Surg Endosc 26(12):3584–3591
Cho JH, Cha SW, Kim HG, Lee TH, Cho JY, Ko WJ, Jin SY, Park S (2015) Long-term outcomes of endoscopic submucosal dissection for early gastric cancer: a comparison study to surgery using propensity score-matched analysis. Surg Endosc. doi:10.1007/s00464-015-4672-1
Choi KS, Jung HY, Choi KD, Lee GH, Song HJ, do Kim H, Lee JH, Kim MY, Kim BS, Oh ST, Yook JH, Jang SJ, Yun SC, Kim SO, Kim JH (2011) EMR versus gastrectomy for intramucosal gastric cancer: comparison of long-term outcomes. Gastrointest Endosc 73(5):942–948
Choi IJ, Lee JH, Kim YI, Kim CG, Cho SJ, Lee JY, Ryu KW, Nam BH, Kook MC, Kim YW (2015a) Long-term outcome comparison of endoscopic resection and surgery in early gastric cancer meeting the absolute indication for endoscopic resection. Gastrointest Endosc 81(2):333–341
Choi JH, Kim ES, Lee YJ, Cho KB, Park KS, Jang BK, Chung WJ, Hwang JS, Ryu SW (2015b) Comparison of quality of life and worry of cancer recurrence between endoscopic and surgical treatment for early gastric cancer. Gastrointest Endosc 82(2):299–307
Chung MW, Jeong O, Park YK, Lee KH, Lee JH, Lee WS, Joo YE, Choi SK, Cho SB (2014) Comparison onthe long term outcome between endoscopic submucosal dissection and surgical treatment forundifferentiated early gastric cancer. Korean J Gastroenterol 63(2):90–98
El-Sedfy A, Brar SS, Coburn NG (2014) Current role of minimally invasive approaches in the treatment of early gastric cancer. World J Gastroenterol 20(14):3880–3888
Hosokawa O, Kaizaki Y, Watanabe K, Hattori M, Douden K, Hayashi H, Maeda S (2002) Endoscopic surveillance for gastric remnant cancer after early cancer surgery. Endoscopy 34:469–473
Japanese Gastric Cancer Association (1998) Japanese classification of gastric carcinoma: 2nd English edition. Gastric Cancer 1:10–24
Japanese Gastric Cancer Association (2011) Japanese classification of gastric carcinoma: 3rd English edition. 14(2):101–112
Kim DY, Hong SJ, Cho GS, Jeong GA, Kim HK, Han JP, Lee YN, Ko BM, Lee MS (2014a) Long-term efficacy of endoscopic submucosal dissection compared with surgery for early gastric cancer: a retrospective cohort study. Gut Liver 8(5):519–525
Kim Y, Kim YW, Choi IJ, Cho JY, Kim JH, Kwon JW, Lee JY, Lee NR, Seol SY (2014b) Cost comparison between surgical treatments and endoscopic submucosal dissection in patients with early gastric cancer in Korea. Gut Liver 63(2):90–98
Kim YI, Kim YW, Choi IJ, Kim CG, Lee JY, Cho SJ, Eom BW, Yoon HM, Ryu KW, Kook MC (2015) Long-term survival after endoscopic resection versus surgery in early gastric cancers. Endoscopy 47(4):293–301
Nakajima T, Oda I, Gotoda T, Hamanaka H, Eguchi T, Yokoi C, Saito D (2006) Metachronous gastric cancers after endoscopic resection: how effective is annual endoscopic surveillance? Gastric Cancer 9:93–98
Ntourakis D, Mavrogenis G (2015) Cooperative laparoscopic endoscopic and hybrid laparoscopic surgery for upper gastrointestinal tumors: current status. World J Gastroenterol 21(43):12482–12497
Oda I, Gotoda T, Sasako M, Sano T, Katai H, Fukagawa T, Shimoda T, Emura F, Saito D (2008) Treatment strategy after noncurative endoscopic resection of early gastric cancer. Br J Surg 95:1495–1500
Okamura T, Tsujitani S, Korenaga D, Haraguchi M, Baba H, Hiramoto Y, Sugimachi K (1988) Lymphadenectomy for cure in patients with early gastric cancer and lymph node metastasis. Am J Surg 155:476–480
Park CH, Lee H, Kim DW, Chung H, Park JC, Shin SK, Hyung WJ, Lee SK, Lee YC, Noh SH (2014) Clinical safety of endoscopic submucosal dissection compared with surgery in elderly patients with early gastric cancer: a propensity-matched analysis. Gastrointest Endosc 80(4):599–609
Shen L, Shan YS, Hu HM, Price TJ, Sirohi B, Yeh KH, Yang YH, Sano T, Yang HK, Zhang X, Park SR, Fujii M, Kang YK, Chen LT (2013) Management of gastric cancer in Asia: resource-stratified guidelines. Lancet Oncol 14(12):e535–e547
Song KY, Hyung WJ, Kim HH, Han SU, Cho GS, Ryu SW, Lee HJ, Kim MC, Korean Laparoscopic Gastrointestinal Surgery Study (KLASS) Group (2008) Is gastrectomy mandatory for all residual or recurrent gastric cancer following endoscopic resection? A large-scale Korean multi-center study. J Surg Oncol 98:6–10
Song WC, Qiao XL, Gao XZ (2015) A comparison of endoscopic submucosal dissection (ESD) and radical surgery for early gastric cancer: a retrospective study. World J Surg Oncol 13:309
Takeda J, Toyonaga A, Koufuji K, Kodama I, Aoyagi K, Yano S, Ohta J, Shirozu K (1998) Early gastric cancer in the remnant stomach. Hepatogastroenterology 45:1907–1911
Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, Tugwell P (2015) The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in the meta-analysis. www.ohri.ca/programs/clinical_epidemiology/oxford.asp
Authors’ contributions
ZSL and ZXH are co-first authors. WJ proposed and designed the study. ZSL, ZXH, LJ performed the research and wrote the first draft. ZXH and GJ collected and analyzed the data. All authors contributed to the design and interpretation of the study. WJ is the guarantor. All authors read and approved the final manuscript.
Acknowledgements
Thanks to Dr. Edward C. Mignot, Shandong University, for linguistic advice.
Competing interests
The authors declare that they have no competing interests.
Statement
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1964 and later versions. Informed consent or a substitute for it was obtained from all patients included in the study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Shulei Zhao and Xiaohua Zhang are co-first authors and also contributed equally to this work
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Zhao, S., Zhang, X., Wang, J. et al. Endoscopic resection versus surgery for early gastric cancer and precancerous lesions: a meta-analysis. SpringerPlus 5, 678 (2016). https://doi.org/10.1186/s40064-016-2273-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40064-016-2273-7