Abstract
Background
Papillary squamotransitional cell carcinoma of the uterine cervix is a rare neoplasm, a subtype of transitional cervical carcinoma that appears to be a variation of squamous cervical carcinoma. It has a disposition toward metastasis at an advanced stage and local recurrence. Owing to the difficulty of illustrating the invasion histologically, misdiagnosis is likely to affect the patient’s prognosis.
Case presentation
We present a case report of an 81-year-old Caucasian patient with squamotransitional cell carcinoma with unusual clinical behavior that was primarily thought to be ovarian cancer. According to the clinical examination and radiologic imaging, the patient had no vaginal bleeding and a normal cervix. Nevertheless, the tumor was already metastasized at the retroperitoneal tissue and at the right ovary. Computed tomography-guided biopsy of the right adnexa gave no further clarification. Although the tumor resembled urothelial cancer, this diagnosis was dismissed because of the results of immunohistochemistry analysis with CK7+, CK5+, and CK20−. Because of the differential diagnosis of ovarian cancer, we decided in favor of an exploratory surgical approach. Hysterectomy with bilateral adnexectomy, extensive retroperitoneal tumor debulking, and infragastric omentectomy was performed by laparotomy. Histopathology revealed a squamotransitional cervical cancer as the primary tumor with a tumor stage of pT3b, pN1 (1/2), V0, RX, G2, corresponding to International Federation of Gynecology and Obstetrics stage IIIB.
Conclusions
As far as we are aware, this is the first report of papillary squamotransitional cell carcinoma of the uterine cervix metastatic to the ovary without vaginal bleeding and with a clinically and radiologically unsuspicious cervix. Physicians should always contemplate papillary squamotransitional cell carcinoma of the uterine cervix in unclear cases with ovarian metastasis, especially if the histology indicates a transitional cancer (CK7+ and CK20−), before proceeding with treatment. More cases are needed to illuminate the clinical characteristics and categorization of papillary squamotransitional cell carcinoma of the uterine cervix.
Similar content being viewed by others
Background
Papillary cell carcinomas of the uterine cervix are very rare but histologically clearly described with well-known histopathological features [1, 2]. To the best of our knowledge, there is no exact information about the incidence of papillary squamotransitional cell carcinoma (PSTCC). This type of cancer may show either a transitional, squamous, or mixed differentiation. PSTCC is named as such because it presents a mixed spectrum of morphologies with a more transitional or more squamous histological appearance [1,2,3]. PSTCC can be described as an in situ tumor with or without an invasive part but usually with both components existing. Furthermore, it is difficult to distinguish PSTCC from other papillary lesions of the cervix because of its papillary, exophytic nature. There is a disposition toward late metastasis at an advanced stage and local recurrence [2].
Transitional cell carcinomas were first described in the ovaries and fallopian tubes and many years later were observed in the uterine cervix and endometrium [4, 5]. These tumors were initially identified in 1952 by Marsh and characterized as papillary squamous cell carcinomas in 1986 by Randall et al. [6, 7]. Information on the clinical, histological, and immunohistochemical features of this tumor is based on a few case reports and a small case series in the literature [8]. Because of the rarity of this tumor and consequently the limited data, no information is available on tumors with clinical behavior similar to that of our patient’s case.
We present an unprecedented case of PTSCC with unusual clinical appearance. All cases of PSTCC should be reported to improve understanding of this rare tumor. Further observation of this and other cases is important to achieve a better comparison of the biological and clinical behavior of this tumor. Despite the rare incidence of PTSCC, the gynecologist should be aware of this tumor as an important differential diagnosis in women with genital cancer, especially when the histology indicates a transitional cancer, in order to provide the appropriate treatment.
Case presentation
We present a case of an 81-year-old Caucasian patient with a retroperitoneal tumor on the right side of the pelvis diagnosed by computed tomography (CT) during her stay in the hospital for deep vein thrombosis of the right leg. Abdominal CT revealed a tumor, which was first thought to be ovarian cancer, sized 7.5 cm × 6 cm × 6 cm with light inhomogeneous density at the right ovary (Fig. 1), lying on the external iliac artery (Fig. 2) and infiltrating the neighboring muscles at the pelvic wall. No distant metastasis or ascites was observed. The patient was then transferred to our gynecological division with the suspicion of primary ovarian cancer.
The general health condition of the patient was good for her age. Her past medical history revealed a spontaneous vaginal delivery and no operations. In her family history, there was no evidence of cervical or any other type of cancer. Furthermore, the patient did not smoke or consume alcohol. She had hypertension, which was being treated with a β-blocker; Hashimoto’s thyroiditis, which was being treated with levothyroxine; and pernicious anemia, which was being treated with vitamin B12 substitution. The patient was raised in Germany, which has an established high standard of living and a well-developed social security system.
The patient did not present with any unusual pain or vaginal bleeding. Her clinical examination and laboratory findings, including complete blood count, urine analysis, and liver and renal function, were normal, except for a palpable mass on the right side of the pelvis. On admission, the patient’s vital parameters were normal (temperature 36.5 °C, pulse 60 per minute, blood pressure 85/140 mmHg). Furthermore, the results of her gynecological clinical examination, including transvaginal ultrasound and visual inspection of the cervix and the vagina, were completely normal. Upon palpation, the uterus was mobile, and the tumor at the right adnexa was almost fixed.
The patient’s ultrasound examination revealed no suspicious results for endometrial or cervical cancer, but at the right adnexa, an irregular restricted tumor, 10 × 6 × 8 cm in size, was found. The tumor marker CA 125 was pathological with 133 U/ml (normal value < 35 U/ml).
Because the spread of the tumor was unusual for ovarian cancer, we decided to proceed with a CT-guided biopsy of the right adnexa. This revealed a solid cancer infiltrating the right ovary and resembling a cancer of the urothelium. Immunohistochemistry (IHC) analysis revealed expression of cytokeratin 7 (CK7+) and cytokeratin 5 (CK5+) but a negative finding for cytokeratin 20 (CK20−). The estrogen receptors of the tumor were completely negative, and the reaction for p63 was recorded as positive. A neoplastic ureteral disease was excluded after the use of diagnostic cystoscopy and pyelography. Because of the differential diagnosis of ovarian cancer, we finally decided in favor of an exploratory surgical approach.
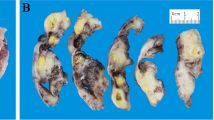
As expected, intraoperatively, a tumor (10 cm) was found in the right retroperitoneal space, emerging from the edge of the ovary and reaching the uterus. The remainder of the peritoneum, bowel, pelvic and paraaortic lymph nodes, and upper abdominal organs were macroscopically unsuspicious. Hysterectomy with bilateral adnexectomy, extensive retroperitoneal tumor debulking, and infragastric omentectomy were performed by laparotomy. The right external iliac vein was completely obstructed because of the tumor’s infiltration, and the right external iliac artery, which could be completely preserved, had stenosis. The entire venous blood flow of the right leg ran through the internal iliac vein. The results of a frozen section revealed transitional cancer with infiltration of part of the right ovary. During the operation, the primary origin of the tumor could not be recognized. The size of residual disease was less than 5 mm. A radical operation was not indicated, owing to the advanced age of the patient and its association with serious complications, such as compromised venous circulation of the right leg with the increased risk of mortality.
The histopathologic analysis results revealed, as the primary tumor, a squamotransitional cervical cancer with a histopathologic tumor stage of pT3b, pN1 (1/2), V0, R1, G2, corresponding to International Federation of Gynecology and Obstetrics (FIGO) stage IIIB. Retrospectively, we could observe a connection between retroperitoneal tumor and cervix on a CT scan (Fig. 3).
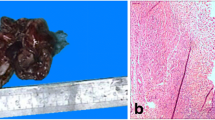
Macroscopic examination revealed that the cervix had a gray-white color and a smooth surface. Retention cysts were also located in the cervix. Microscopic examination showed that the surface of the ectocervix was covered with nonkeratinizing, stratified squamous epithelium. In the area of the transformation zone, atypical epithelial formations were found with moderate cellular and nuclear polymorphism. The tissue of the tumor of the right retroperitoneum had epithelial atypia with uncontrolled cell growth and infiltration of the trabecular formations. IHC revealed positive staining for CK14, p16, and p63 and negative staining for chromogranin and synaptophysin (Fig. 4).
We concluded that radiotherapy with 60 Gy at the former tumor region and 54 Gy at the pelvic lymphatic system was required; however, the patient refused further treatment, including the follow-up examinations.
Five months later, the patient was hospitalized with an unclear infection. A CT scan of the abdomen revealed a huge abscess in the right retroperitoneal space and recurrence of the tumor. After treatment with pigtail tube drainage and antibiotics, we were able to stabilize her condition. Subsequently, the patient refused any further medical treatment, so she was transported to the palliative unit, where she died a few days later of sepsis.
Discussion and conclusions
We describe an unusual case of a patient with PTSCC who underwent surgery because of the suspicion of primary ovarian cancer based on a 7.5-cm tumor at the right ovary. The patient did not present with any unusual pain or vaginal bleeding. Moreover, the result of the patient’s clinical examination, including transvaginal ultrasound and visual inspection of the cervix and the vagina, was completely normal. CT-guided biopsy, intraoperative frozen section, and exploratory laparotomy were unable to clarify the origin of the tumor. The final histopathologic result revealed PTSCC with tumor stage pT3b, pN1 (1/2), V0, RX, G2, corresponding to FIGO stage IIIB.
It remains unclear whether papillary cell carcinomas of the cervix represent a different group of tumors or if they are morphologically similar within a single clinically homogeneous entity. Koenig et al. [2], who presented 32 cases of papillary cervical carcinomas, the largest case series in the literature, reported that the most common clinical presentation of PSTCC is abnormal bleeding and an abnormal Papanicolaou smear [2]. With regard to our patient’s case, a cervical biopsy was not performed, because the result of visual inspection of both the cervix and the vagina was completely normal. In addition, because the retroperitoneal tumor was at an advanced stage, cervical cancer as the primary tumor was not expected. Even in the case of clinical, sonographic, or radiologic suspicion of cervical cancer, it is not always easy to identify this neoplasm, owing to its papillary, exophytic nature, and sometimes a deep biopsy or a cone biopsy is necessary [1,2,3, 7].
PSTCC may exist in an in situ state with or without an invasive part, but usually it exhibits both components [2]. The invasive component is mostly without papillae, in contrast to the noninvasive component, which is more often papillary. It has been reported that PSTCC can be understaged because it may be difficult to illustrate histologically the invasion part, which can lead to incorrect staging, affecting the patient’s treatment and prognosis [3, 15]. As a result, it is very important to distinguish PSTCC from other papillary lesions of the cervix (Table 1). Furthermore, the papillary growth pattern makes it similar to a carcinoma of urothelial origin [10, 15, 16]. This diagnosis was suspected in our patient’s case, and our patient underwent cystoscopy to exclude urothelial carcinoma. As shown in Table 2, transitional cell carcinoma of urothelial origin often reveals a different immunoreactivity [12,13,14], which in our patient’s case helped us to dismiss this diagnosis. The uterine cervix must always be considered as the site of origin of transitional carcinoma.
Some reports advocate the hypothesis that the majority of transitional cell carcinomas of the cervix are variations of squamous cervix carcinoma (SCC) because they share almost the same etiologic and pathogenic features, such as human papillomavirus (HPV) infection, an immunoreactive profile, spread, and behavior, with the exception that late metastasis has been reported in referring to PSTCC [11]. Many reports describe that PSTCC has a positive correlation with HPV16 and a negative correlation with HPV6, 11, and 18. This finding supports the above-mentioned hypothesis that PSTCC and SCC are similar and suggests that HPV infection of the cervix may play an etiologic role in at least some of these tumors [2, 9, 14]. Currently, there are no specific treatment guidelines for PSTCC [18]; however, experts suggest the same treatment as for SCC [2, 7]. Koenig et al. [2] reported longer survival in one patient with advanced disease after treatment with chemotherapy. More cases are needed to clarify the appropriate treatment of this rare tumor.
In the literature, the clinical behavior of PSTCC is characterized as almost the same as that of SCC, except for the tendency of PSTCC toward late metastasis and local recurrence [2, 7]. However, in our patient’s case, the clinical behavior seems to have been fundamentally different, because the tumor extended into the retroperitoneal space and the right ovary without apparent local infiltration of the cervix or vaginal bleeding. The treatment of the patient would have been the same if we had known from the beginning that she had PSTCC. In the case of young patients, however, the treatment could affect the recurrence of the tumor and the postoperative survival of the patient if the correct diagnosis is not made during staging and as a result the appropriate oncologic procedure and adjusted therapy are not initiated.
In conclusion, to the best of our knowledge, this is the first report of a retroperitoneal PSTCC metastatic to the ovary without vaginal bleeding and with a normal cervix at clinical examination and imaging. Such a case can easily be misdiagnosed as primary ovarian cancer because of the absence of any visible cervical lesion or abnormal cervical screening history. A high index of suspicion is necessary to avoid misdiagnosis of such a case and to choose the appropriate treatment, which could strongly influence the patient’s prognosis. Thus, physicians should be aware of this case and should always consider PSTCC in patients with ovarian metastasis of unclear diagnosis despite an unsuspicious cervix, especially when the histology indicates a transitional cancer (CK7+ and CK20−). Further observation of this and other cases is important to achieve a better comparison of the biological and clinical behavior of this tumor.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
References
Albores-Saavedra J, Young R. Transitional cell neoplasms (carcinomas and inverted papillomas) of the uterine cervix. Am J Surg Pathol. 1995;19:1138–45.
Koenig C, Turnicky RP, Kankam CF, Tavassoli FA. Papillary squamotransitional cell carcinoma of the cervix: a report of 32 cases. Am J Surg Pathol. 1997;21:915–21.
Walker AN, Mills SE. Unusual variants of uterine cervical carcinoma. Pathol Annu. 1987;22:277–310.
Austin RM, Norris HJ. Malignant Brenner tumor and transitional cell carcinoma of the ovary: a comparison. Int J Gynecol Pathol. 1987;6:29–39.
Bass PS, Birch B, Smart C, Theaker JM, Wells M. Low-grade transitional cell carcinoma of the vagina – an unusual cause of vaginal bleeding. Histopathology. 1994;24:581–3.
Marsh MR. Papilloma of the cervix. Am J Obstet Gynecol. 1952;64:281–91.
Randall M, Andersen WA, Mills SE, Kim JC. Papillary squamous cell carcinoma of the uterine cervix: a clinicopathologic study of nine cases. Int J Gynecol Pathol. 1986;5:1–10.
Al-Nafussi AI, Al-Yusis R. Papillary squamotransitional cell carcinoma of the uterine cervix: an advance stage disease despite superficial location: report of two cases and review of the literature. Eur J Gynaecol Oncol. 1998;5:455–7.
Brinck U, Jakob C, Bau O, Fuzesi L. Papillary squamous cell carcinoma of the uterine cervix; report of three cases and a review of its classification. Int J Gynecol Pathol. 2000;19:231–5.
Fukunaga M. Inverted papilloma-like transitional cell carcinoma of the uterine cervix. Histopathology. 1998;33:189–91.
Kokka F, Verma M, Singh N, Faruqi A, Yoon J, Reynolds K. Papillary squamotransitional cell carcinoma of the uterine cervix: report of three cases and review of the literature. Pathology. 2006;38:584–6.
Kurman RJ, editor. Blaustein’s pathology of the female genital tract. 5th ed. New York: Springer-Verlag; 2002.
Southgate J, Harnden P, Trejdosiewicz LK. Cytokeratin expression patterns in normal and malignant urothelium: a review of the biological and diagnostic implications. Histol Histopathol. 1999;14:657–64.
Lininger RA, Wistuba I, Gazdar A, Koenig C, Tavassoli FA, Albores-Saavedra J. Human papillomavirus type 16 is detected in transitional cell carcinomas and squamotransitional cell carcinoma of the cervix and endometrium. Cancer. 1998;83:521–7.
Anand M, Deshmukh SD, Gulati HK. Papillary squamotransitional cell carcinoma of the uterine cervix: a histomorphological and immunohistochemical study of nine cases. Indian J Med Paediatr Oncol. 2013;34(2):66–71.
Nakamura E, Shimizu M, Fujiwara K, Yamauchi H, Monobe Y, Hirokawa M, et al. Papillary squamous cell carcinoma of the uterine cervix: diagnostic pitfalls. APMIS. 1998;106:975–8.
Ortega-Gonzalez P, Chanona-Vilchis J, Dominguez-Malagon H. Transitional cell carcinoma of the uterine cervix. Acta Cytol. 2002;46:585–90.
Koh WJ, Greer BE, Abu-Rustum NR, Apte SM, Campos SM, Cho KR. Cervical cancer, version 2.2015. J Natl Compr Canc Netw. 2015;13(4):395–404.
Funding
There were no sources of funding.
Author information
Authors and Affiliations
Contributions
GG and EK analyzed and interpreted the patient data. GG, TD, and IA performed the histological examination and were major contributors to the writing of the manuscript. AR and SB performed the literature research. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Approval was obtained from the Ethics Committee of the Medical Faculty of the University of Kiel. Patient consent was also obtained.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Gitas, G., Ertan, K., Rody, A. et al. Papillary squamotransitional cell carcinoma of the uterine cervix: a case report and review of the literature. J Med Case Reports 13, 319 (2019). https://doi.org/10.1186/s13256-019-2217-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13256-019-2217-2