Abstract
Background
Point-of-care ultrasound (POC-US) is gaining importance in almost all specialties. E-learning has been used to teach theoretical knowledge and pattern recognition. As social media are universally available, they can be utilized for educational purposes. We wanted to evaluate the utility of the sandwich e-learning approach defined as a pre-course e-learning and a post-course learning activity using Facebook after a one-day point-of-care ultrasound (POC-US) course and its effect on the retention of knowledge.
Methods
A total of 62 medial students were recruited for this study and randomly assigned to one of four groups. All groups received an identical hands-on training and performed several tests during the study period. The hands-on training was performed in groups of five students per instructor with the students scanning each other. Group 1 had access to pre-course e-learning, but not to post-course e-learning. Instead of a pre-course e-learning, group 2 listened to presentations at the day of the course (classroom teaching) and had access to the post-course learning activity using Facebook. Group 3 had access to both pre- and post-course e-learning (sandwich e-learning) activities, while group 4 listened classroom presentations only (classroom teaching only). Therefore only groups 2 and 3 had access to post-course learning via Facebook by joining a secured group. Posts containing ultrasound pictures and videos were published to this group. The students were asked to “like” the posts to monitor attendance. Knowledge retention was assessed 6 weeks after the course.
Results
After 6 weeks, group 3 achieved comparable results when compared to group 2 (82.2 % + −8.2 vs. 84.3 + −8.02) (p = 0.3). Students who participated in the post-course activity were more satisfied with the overall course than students without post-course learning (5.5 vs. 5.3 on a range from 1 to 6).
Conclusions
In this study, the sandwich e-learning approach led to equal rates of knowledge retention compared to classroom lectures and post-course learning. Students appreciate new media for learning experiences and are more satisfied with their learning activity. The sandwich e-learning can be used to maximize hands-on training during courses.
Similar content being viewed by others
Background
Social Media such as Facebook, Twitter, and YouTube are changing the way medical educators are teaching today. A significant percentage of students already use online resources and social media as means of self-directed learning [1–3]. The most popular and widely used network is Facebook with over 1.32 billion registered users, 945,000,000 of them using mobile devices [4]. Facebook allows users to communicate through chats or via private messages on an individual basis or in defined groups. Students already use Facebook for educational purposes on a daily basis [5, 6].
Ultrasound is an increasingly important diagnostic tool and is amenable to online learning. Facebook offers a broad variety of communication tools (messages, videos via walls, posts, etc.) that distinguish it from other media such as Twitter that are limited to 140 characters. A challenge in medical education has always been to teach not only for the moment but to achieve retention of knowledge over time. E-learning using social media and other forms such as password-secured platforms are increasingly being used by medical schools and in post-graduate education. The advantage of e-learning is that the learner can autonomously define time, pace, and location of the activity. As the use of social media is increasing, recommendations for the integration into educational programs have been published [7–9].
Hands-on training still is an integral part of every ultrasound course and is expected by the participants [10]. The time spent on this activity should be maximized.
In this study, we intended to assess the value of a pre-course e-learning combined with a post-course activity using Facebook, a concept we defined as sandwich e-learning. Our primary goal was to analyze the effect of this combined pre- and post-course e-learning (sandwich e-learning) activities on the retention of knowledge compared to standard lectures and post-course learning; the secondary aim was to evaluate the utility of post-course activity using social media.
Methods
We developed a one-day course based on emergency ultrasound courses offered by the DEGUM (German Society for Ultrasound in Medicine) and the German Society of Anesthesiology and Intensive care (Deutsche Gesellschaft für Anästhesie und Intensivmedizin; DGAI; curriculum of AFS module 5). The curriculae incorporate the E-FAST exam (extended focused assessment with sonography in trauma) and clinical applications of thoracic ultrasound such as pleural effusion, B-lines, and pulmonary edema, pneumothorax, and consolidations [11].
Participants
We recruited medical students without prior ultrasound experience (3rd year and higher) from two medical schools in Germany (University of Frankfurt and University of Bonn). Participation in the course was not required for completing the curriculum at university and had no influence on the progress or grading of their medical studies. For participating in the study, all students received an expense allowance of 50 Euros and a compensation for their traveling expenses. All were given ultrasound pocket-sized cards (www.SonoABCD.org) and a textbook summarizing the content of AFS Module 5 after the end of the study. The cards are pocket-sized cards summarizing scanning techniques, physiologic, and pathologic findings. We developed five different cards covering POC-US as an introduction, the FAST exam, thoracic ultrasound, the FEEL exam (focused echocardiographic evaluation in life support [12]), and deep vein thrombosis. Every student received the FAST and the thoracic ultrasound pocket cards. The textbook handed out to the students was published by two of the authors (RB and AS) as complementary material to the certified ultrasound courses. To motivate the students, the three top scorers were invited to participate in another ultrasound course free of cost. All participants gave written consent for their data being used for research purposes and publication; an approval by the ethics committee was waived.
Study design
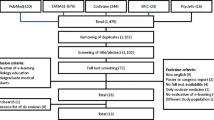
The study was designed as a randomized, controlled, parallel group study. Students were randomized into four groups (G 1–4) (Fig. 1).
All students were required to take a multiple choice test (Test A) consisting of 20 questions including multiple choice questions (MC) and drag-and-drop tasks during the 4 weeks prior to the course.
The pre-course e-learning consisted of 14 case-based screencasts with a maximum duration of 5 min. The content of the screencasts is listed in Table 1. The screencasts, defined as digital recordings of a computer screen output enhanced with audio narration [13], were produced by seven experienced physicians using a standard template. All physicians were certified POCUS instructors and were taught how to use the free online program screencast-o-matic (www.screencast-o-matic.com) for production of the screencasts. Every presentation included a standard structure of the following slides: title, presentation of the case/problem, ultrasound images or clips, interpretation/progress of the case, key messages, conclusion, questions, and title again [14]. Screencasts were uploaded as an e-learning curriculum onto a password-secured platform.
G 1 and G 3 were given access to a case-based e-learning curriculum 4 weeks prior to the course and participated in a discussion (60 min) on the day of the course. The discussion was moderated by two tutors and intended to clarify all issues that arose during the e-learning.
G 2 and 4 (classroom groups) had no access to the pre-course e-learning and listened to standardized classroom-based presentations on the day of the course. The classroom teaching consisted of nine lectures lasting 15 min each, covering identical content as that for the pre-course e-learning (Table 1).
All groups participated in a hands-on training (HT) identical in structure and content (180 min in total). HT was performed in small groups of five students rotating through six stations with the students scanning each other under supervision of an experienced instructor who was not compensated for the activity (stations 1–3: thoracic ultrasound; stations 4–6: FAST).
After the HT, every participant performed a standardized objective clinical skills examination (OSCE) with the maximum score of 50. The test required the students to perform a defined exam, i.e., FAST, and name structures displayed. The instructors evaluated the tasks as right (1 point) or wrong (0 points). With a total of 50 tasks, the maximum score that could be achieved was 50.
After the course, G 2 and G 3 were invited to join a password-protected group in the social network Facebook. Every weekday, a Facebook post was posted to the group for a total of 6 weeks (30 tweets). Each post had a maximum word count of 140 characters; 17 out of 30 included an ultrasound video or image (Fig. 2). To monitor attendance, students were instructed to like each of the posts. The original posts can be found in the Additional file 1: Table S1.
All students performed a MC test (test B) on the day of the course; an online MC test within 3 days after the course (test C); and an online MC test 6 weeks after (test D). Another test (test E) consisted of 20 questions including pictures and videos showing physiologic or pathologic findings. These questions had to be answered in free text and were intended to assess the pattern/image-recognition ability of the students.
Students were also asked to answer a questionaire after the day of the course and after completion of the study protocol grading items from one (poor) to six (very good). The survey covered every phase of the study (pre-course, classroom lectures, HT, post-course, tests, etc.) and asked about their satisfaction with organization, layout, content, and applicability.
Statistical analysis
Statistical analysis was performed using GraphPad Prism version 6.0 (GraphPad software, Inc. La Jolla, CA 92037, USA). Test results were analyzed and presented in % score with 25 and 75 % percentiles.
The Mann–Whitney-U test was used for group comparison. We chose a significance level of α = 5 %. The primary outcome was the performance in the MC tests and the OSCE; therefore, a Bonferroni–Holm correction for multiple testing was applied, and power calculation was performed for α = 2.5 %.
Results and discussion
A total of 62 students were recruited from the universities of Bonn and Frankfurt. Two students did not attend the course, while three students did not complete test C, leaving 57 students for this statistical analysis. When comparing group 3 (sandwich e-learning) with the other groups (post-course learning alone, pre-course learning only, and classroom-based), no significant differences were found both in test D and test E (p = 0.3; p = 0.5) (Fig. 3). Groups 1 and 3 performed significantly better in test A compared to groups 2 and 4 (p < 0.05). Results of tests B and C did not show any significant difference. The results and a detailed discussion of tests A, B, and C have previously been published elsewhere [14].
The evaluation by the participants showed that the post-course learning raised the satisfaction as G 2 and 3 evaluated the course with a mean score of 5.5 (95 % CI 5.7–5.3) compared to a mean score of 5.3 (95 % CI 5.5–5.1) given by G 1 and 4 (p < 0.05).
81.8 % of the participants evaluated the post-course activity as good or very good with an adequate amount of time spent on this activity. 60.6 % of students felt their increase in knowledge was good; this was only their subjective judgement.
In this study, we designed and applied the sandwich e-learning technique, a novel approach defined as a learning pathway including a pre-course e-learning curriculum, a hands-on training (HT) session, and a post-course activity using social media after the course.
Teaching POC-US ultrasound has to incorporate different aspects of learning. They are the sensor–motor component of moving the ultrasound probe, the skill of pattern recognition, and the skill of incorporation of the findings into the clinical setting. Pattern-recognition training can be imparted utilizing e-learning. The integration into the clinical context can be partially trained unsing e-learning by adding short case vignettes. Description, for example, of the history of present illness, vital signs, etc., in combination with an ultrasound picture or video, can instead be used in the training for the integration of the ultrasound findings into the clinical context. The motor skills of probe placement on the patient can most effectively be learned via hands-on training [15]. Many studies have evaluated educational methods for teaching procedural skills [16, 17]. Hands-on training is very staff-intensive as the number of students trained by one teacher should be as small as possible to allow the individual student enough time. Many physicians and students learn the basics of POC-US in focused courses lasting only one to 2 days [18, 19]. Therefore, hands-on time during these courses should be maximized.
E-learning both traditional methods such as online curricula and new methods utilizing social media such as Facebook can be used to teach theoretical knowledge and pattern recognition [5, 6]. The advantages of e-learning are flexibility regarding space, time, and duration [20], and in contrast to generic courses, the form of a self-organized learning pathway over time which can enhance retention of knowledge. It is important to point out that every educational activity using social media needs to be rigorous regarding the appropriate use and privacy policies that apply [7].
Conclusions
In our study, students trained with the sandwich e-learning approach achieved similar test results after 6 weeks compared to the groups with traditional teaching methods such as classroom lectures. Therefore, we argue that e-learning might be an alternative to classroom lectures as it offers the possibility to maximize the time spent on hands-on training and seems to be a feasible method of learning in addition to hands-on training for POC-US.
Limitations
In this study, we only analyzed the effect of the sandwich e-learning approach on a limited number of medical students; further research is needed applying this approach to postgraduate training where the use of social media is not as common, especially regarding ultrasound education. We assume that all participating students had a high motivation, but we did not perform a motivational analysis. The results of the online tests are limited by the fact that students could have used other resources while completing the tests. As all groups would have this possibility, this does not contradict the results and conclusion of our study. Our study is further limited by the fact that we only assessed the retention of knowledge after 6 weeks. Further study comparing different models of sandwich e-learning, i.e., social media-based pre-course and post-course versus a structured curriculum-based pre-course and post-course, is needed to explore the efficacy of this technique. More detailed investigation is also needed to ascertain if knowledge is retained over longer periods of time and when it is applied in clinical practice.
References
Hollinderbäumer A, Hartz T, Rückert F (2013) Education 2.0—How has social media and Web 2.0 been integrated into medical education? A systematical literature review. GMS Z Med Ausbild 30(1):1–12
Barry DS, Marzouk F, Chulak-Oglu K, Bennett D, Tierney P, O’Keeffe GW (2015) Anatomy education for the YouTube generation. Anat Sci Educ 9(1):90–96
Choi-Lundberg DL, Low TF, Patman P, Turner P, Sinha SN (2015) Medical student preferences for self-directed study resources in gross anatomy. Anat Sci Educ. doi:10.1002/ase.1549
Wikipedia. https://de.wikipedia.org/wiki/Facebook. Accessed 17 Oct 2014
Pander T, Pinilla S, Dimitriadis K, Fischer MR (2014) The use of Facebook in medical education—a literature review. GMS Z Med Ausbild 31(3):Doc33. doi:10.3205/zma000925
Gray K, Anabell L, Kennedy G (2010) Medical students’ use of Facebook to support learning: Insights from four case studies. Med Teach 32(12):971–976
Pearson D, Cooney R, Bond MC (2015) Recommendations from the Council of Residency Directors (CORD) Social Media Committee on the Role of Social Media in Residency Education and Strategies on Implementation. West J Emerg Med 16(4):510–515
Chang TP, Pham PK, Sobolewski B, Doughty CB, Jamal N, Kwan KY, Little K, Brenkert TE, Mathison DJ (2014) Pediatric emergency medicine asynchronous e-learning: a multicenter randomized controlled Solomon four-group study. Acad Emerg Med 21(8):912–919
Chu LF, Ngai LK, Young CA, Pearl RG, Macario A, Harrison TK (2013) Preparing interns for anesthesiology residency training: development and assessment of the successful transition to anesthesia residency training (START) e-learning curriculum. J Grad Med Educ 5(1):125–159
Röhrig S, Hempel D, Stenger T, Armbruster W, Seibel A, Wlcher F, Breitkreutz R (2014) Which learning methods are expected for ultrasound training? Blended learning on trail. Anaesth 63(10):745–752
Röhrig S, Seibel A, Zechner PM, Steigerwald M, Kummer T, Groesdonk HV, Armbruster W, Breitkreutz R (2011) Thoracoabdominal sonography (E-FAST plus)- AI training module 5 in anaesthesiologist-performed focussed sonography. Anasthesiol Intensivmed Notfallmed Schmerzther. 46(11–12):772–781
Breitkreutz R, Price S, Steiger HV, Seeger FH, Ilper H, Ackermann H, Rudolph M, Uddin S, Weigand MA, Müller E, Walcher F (2010) Emergency Ultrasound Working Group of the Johann Wolfgang Goethe-University Hospital, Frankfurt am Main (2010) Focused echocardiographic evaluation in life support and peri-resuscitation of emergency patients: a prospective trial. Resuscitation. 81(11):1527–1533
http://en.wikipedia.org/wiki/Screencast. Accessed 22 Aug 2015
Hempel D, Sinnathurai S, Haunhorst S, Seibel A, Michels G, Heringer F, Recker F, Breitkreutz R (2015) Influence of case based E-learning on students’ performance in point-of-care ultrasound courses: a randomized trail. Eur J Emerg Med. doi:10.1097/MEJ.0000000000000270
Cartier RA, Skinner C, Laselle BJ (2014) Perceived effectiveness of teaching methods for point of care ultrasound. Emerg Med. 47(1):86–91
Jayaraman V, Feeney JM, Brautigam RT, Burns KJ, Jacobs LM (2014) The use of simulation procedural training to improve self-efficacy, knowledge, and skill to perform cricothyroidotomy. Am Surg 80(4):377–381
Andreatta P, Chen Y, Marsh M, Cho K (2011) Simulation-based training improves applied clinical placement of ultrasound-guided PICCs. Support Care Cancer 19(4):539–543
Mozzini C, Garbin U, Fratta Pasini AM, Cominacini L (2015) Short training in focused cardiac ultrasound in an Internal Medicine department: what realistic skill targets could be achieved? Intern Emerg Med 10(1):73–80
Gaspar HA, Morhy SS, Lianza AC, de Carvalho WB, Andrade JL, do Prado RR, Schvartsman C, Delgado AF (2014) Focused cardiac ultrasound: a training course for pediatric intensivists and emergency physicians. BMC Med Educ 14:25
Platz E, Goldflam K, Mennicke M, Parisini E, Christ M, Hohenstein C (2010) Comparison of Web-versus classroom-based basic ultrasonographic and EFAST training in 2 European hospitals. Ann Emerg Med 56(6):660–667
Walcher F, Weinlich M, Conrad G et al (2006) Prehospital ultrasound imaging improves management of abdominal trauma. Br J Surg 93(2):238–242
Authors’ contributions
DH was involved in drafting the study, contributed to the screencasts used in this study and wrote the manuscript. SH and SS were involved in drafting and designing the study; both carried out the study and data collection. SH was involved in data analysis and approved the final manuscript after critical revision. AS contributed to the study conception and critically revised the manuscript. He has given approval of the final version. FR contributed significantly to recruitment of participants and data collection. He has given approval of the final version. FH contributed significantly to recruitment of participants and data collection. He was involved in designing the study. He has given approval of the final version. GM has been involved in data analysis and drafting of the manuscript. He has also given approval of the final version. RB has contributed to the study design and conception, supervised data analysis, and has critically revised data and manuscript. He has given approval of the final version. All authors read and approved the final manuscript.
Acknowledgements
The authors thank tutors (S. Schellhaas, T. ElAnsari, K. Kunz, Y. Trusau, C. Schrader, and T. Schröder) for their help during this study. The authors also want to thank Sono4students and FINEST Frankfurt for the cooperation. Regional network of ultrasound in acute and critical care www.SonoABCD.org designed and supported this study. The authors are also indebted to J. Geib for her organizational help. Studying the effects of Tweets to enhance student’s performance was inspired by David P. Bahner, Ohio State University, USA and is gratefully acknowledged.
Parts of the data was presented at the World Congress of Ultrasound in Medical Education meeting, Portland, USA October 2014.
Competing interests
R. Breitkreutz is co-founder of the working group emergency ultrasound—UEC Partners GmbH, Fischbachtal, and MedUserv GbR, Wilnsdorf—which develops and conducts ultrasound courses and learning sources. He has cooperated with the following companies: European space association, Nordwijk, Netherlands; Space Applications Services, Brussels; SonoSite GmbH, Frankfurt; and GE Health- care GmbH, Solingen, Esaote Germany. A. Seibel is also co-founder of UEC and MedUserv GbR. D. Hempel received compensation for travel expenses from UEC Partners. The remaining authors have declared no competing interests.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Hempel, D., Haunhorst, S., Sinnathurai, S. et al. Social media to supplement point-of-care ultrasound courses: the “sandwich e-learning” approach. A randomized trial. Crit Ultrasound J 8, 3 (2016). https://doi.org/10.1186/s13089-016-0037-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13089-016-0037-9