Abstract
Germ-line mutations in several genes, such as BRCA1 and BRCA2, are known to increase the risk of breast cancer. These heritable mutations are unequally represented among populations with different ethnic background due to founder effects and thereby contribute to differences in breast cancer rates in different populations. The BRCA1 mutation c.5266dupC (also known as 5382insC or 5385insC) was detected in a sample of 193 breast cancer patients in Ukraine by multiplex mutagenically separated PCR using published specific primers. Nine BRCA1 mutations 5382insC were detected (4.7 %). The difference in age of diagnosis (35 years in 5382insC carriers versus 45 years in non-carriers) we observed is consistent with other reports indicating that the 5382insC mutation is a factor of genetic predisposition to breast cancer, which is consistent with reports from other countries.
Similar content being viewed by others

Findings
The BRCA1 gene is critical for a number of important cellular processes, such as maintenance of genome integrity, repair of DNA double-strand breaks, and cell cycle control [1]. Mutations in BRCA1 and BRCA2 are associated with an increased risk of breast cancer, and is reported to be as high as 80 % [2], and also associated with ovarian, prostate, pancreatic and male breast cancer [3–5]. Breast cancer is the most frequent type of cancer in Ukrainian women and is the primary cause of cancer-related deaths. A total of 17,537 patients were diagnosed with breast cancer in 2011 (including 130 men) corresponding to a standardized incidence rate of 23.9 per 100,000 individuals [6], similar to that of other Eastern European countries (22.07 in Moldova, 45.86 in Belarus, 50.04 in Romania, 50.54 in Hungary, 51.89 in Poland) but far less than that of the United States (92.93) [7].
Knowledge of the presence of a BRCA1 mutation is important for both prevention of cancer and personalized treatment. Intensive screening of mutation carriers with magnetic resonance imaging is now recommended in developed countries [8–11]. Genetic testing at the time of diagnosis facilitates choice of treatment and BRCA1 carriers with breast cancer may benefit from bilateral mastectomy, from oophorectomy and from cisplatinum treatments [12, 13]. Unfortunately, in Ukraine, genetic screening is not currently offered at the time of breast cancer diagnosis [14–18].
The frequency of BRCA1 mutations has been shown to differ among ethnic backgrounds [13, 19–22], reaching as high as 2.5 % in Ashkenazi Jews [19, 21, 22]. A small number of studies of Ukrainian women breast cancer patients [14–18] have revealed the presence of a founder mutation in BRCA1, 5382insC. This is the most common mutation among Slavic patients with breast or ovarian cancer and has been studied extensively in Poland, Russia, Belarus and the Baltic countries. Here we present the results of a screening for the frequency of the BRCA1 mutations 5382insC among 193 Ukrainian breast cancer patients.
Patient samples
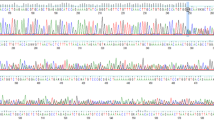
We screened 193 breast cancer patients diagnosed at different ages. Data on each patient were collected from their clinical records, accessed with the patients’ permission. We documented family history (FH) of disease in 135 patients out of 193 persons. Clinical material was collected at the Shupik National Postgraduate Education Medical Academy, the Kyiv Municipal Clinical Oncological Center, the Ukrainian National Cancer Institute, the Chernihiv Regional Oncology Center, and the Zhytomyr Regional Oncology Center with informed consent and approval from the local ethics committee (committee on Bioethics: order number №16 Educational and Scientific Centre “Institute of Biology”, Taras Shevchenko National University of Kyiv of February 25, 2014, 64 Volodymyrska St., 01601, Kyiv). DNA from blood samples was extracted using the phenol-chloroform method and by the DNA-SORB-B (AmpliSense, Russia). The BRCA1 mutation 5382insC was detected by multiplex mutagenically separated PCR using published specific primers [23]. Three primers were used to detect the mutation: one general, one specific to the mutation in question, and one specific to wild the type allele as described in Chan et al., 1999 [23]. PCR amplicons were analyzed by 8 % PAGE and 2 % agarose.
We screened a total of 193 breast cancer patients diagnosed ages 18 through 80 for the 5382insC mutation. A total of nine BRCA1 5382insC mutations were detected (4.7 %) (Table 1). Most carriers of the 5382insC mutation were younger that 40 years at the time of detection (ages 19, 27, 31, 34, 36, 38, 39), although two occurrences were found in older patients (52 and 44 years). This represents a frequency of occurrence of 7/79 (8.9 %) for individuals under age 40 and 2/114 (1.8 %) for patients older than 40. A mutation was found in 5 of 90 patients with a FH of cancer (5.5 %) and in 1 of 45 patients with no FH (2.2 %). 13 patients with a FH of cancer had precisely breast cancer in family (1 with mutation) and 77 patients with a FH had other cancer types: prostate, stomach, lung cancer and uterine fibroids (2 with mutation), also 14 patients had both, breast and other cancer types in FH, such as laryngeal, lung and prostate cancer (2 mutation carriers). The frequency of the 5382insC mutation is similar in patients with and without a FH of breast cancer (F = 0.01, p > 0.05).
In this study, we report that 4.7 % of unselected breast cancer patients from Ukraine carry a 5382insC mutation. This estimate is similar to those of previous studies that estimated the prevalence of the mutation between 2.5 % and 7.1 % (F = 0.45, p > 0.05) [14–18]. Combining the results of all studies, including ours, the pooled frequency for Ukrainian patients is estimated at 5.81 ± 0.9 % (38 cases out of the total 654 women patients screened).
Ukrainians are eastern Slavics by genetic background and are close relatives of Belarusians, Poles, and Russians. The estimate of the 5382insC mutation in the BRCA1 gene for Ukraine (5.8 %) is higher than reported for Belarusians (2.5 %) (F = 9.23, p < 0.05) [24], but lower than that of Poles (10.4 %) (F = 12.21, p > 0.05) [25] and is similar to an estimate from Saint Petersburg, Russian (4.7 %) (F = 0.42, p > 0.05) [26].
The average age amounted 35 years in 5382insC carriers versus 45 years in non-carriers which is consistent with other reports indicating that the 5382insC mutation is a factor of genetic predisposition to breast cancer, which is also consistent with reports from other countries [27].
The 5382insC mutation of BRCA1 is a frequent germline mutation in Ukrainian breast cancer patients. Interestingly, and in contrast to other reports, our results suggest no difference in 5382insC mutation frequencies between breast cancer patients with and without a FH of the disease. The presented data can confirm a noticeable contribution of BRCA1 5382insC mutation in breast cancer development in Ukraine and as there is no difference between the frequency of mutations in the groups with and without a FH it may justify to screen for 5382insC mutation all breast cancer patients totally, not primarily that who have a FH.
Abbreviations
- BRCA1 :
-
Breast cancer 1, early onset
- FH:
-
Family history
References
O’Donovan PJ, Livingston DM. BRCA1 and BRCA2: Breast/ovarian cancer susceptibility gene products and participants in DNA double-strand break repair. Carcinogenesis. 2010;31:961–7.
Petrucelli N, Daly MB, Feldman GL. Hereditary breast and ovarian cancer due to mutations in BRCA1 and BRCA2. Genet Med. 2010;12:245–59.
Finch A, Beiner M, Lubinski J, Lynch HT, Moller P, Rosen B, et al. Salpingo-oophorectomy and the risk of ovarian, fallopian tube, and peritoneal cancers in women with a BRCA1 or BRCA2 Mutation. JAMA. 2006;296(2):185–92.
Tai YC, Domchek S, Parmigiani G, Chen S. Breast cancer risk among male BRCA1 and BRCA2 mutation carriers. J Natl Cancer Inst. 2007;99(23):1811–4.
Levy-Lahad E, Friedman E. Cancer risks among BRCA1 and BRCA2 mutation carriers. Br J Cancer. 2007;96(1):11–5.
Cancer in Ukraine, 2013–2014 Ukrainian cancer registry statistics, 2014 Bulletin of National Cancer Registry of Ukraine. http://www.ncru.inf.ua/
Organisation for Economic Cooperation and Development. Health at a glance: Europe 2010. OECD, 2010. http://ec.europa.eu/health/reports/docs/health_glance_en.pdf
Saadatmand S, Vos JR, Hooning MJ, Oosterwijk JC, Koppert LB, de Bock GH, et al. Relevance and efficacy of breast cancer screening in BRCA1 and BRCA2 mutation carriers above 60 years: A national cohort study. 2014. doi:10.1002/ijc.28941.
Mostowska A, Pawlik P, Sajdak S, Markowska J, Pawałowska M, Lianeri M, et al. An analysis of polymorphisms within the Wnt signaling pathway in relation to ovarian cancer risk in a Polish population. Mol Diagn Ther. 2014;18:85–91.
McCarthy AM, Armstrong K. The role of testing for BRCA1 and BRCA2 mutations in cancer prevention. JAMA Intern Med. 2014;174:1023–4.
Couch FJ, Nathanson KL, Offit K. Two decades after BRCA: setting paradigms in personalized cancer care and prevention. Science. 2014;343:1466–70.
Kurian AW, Sigal BM, Plevritis SK. Survival analysis of cancer risk reduction strategies forBRCA1/2mutation carriers. J Clin Oncol. 2010;28:222–31.
Tong A, Kelly S, Nusbaum R, Graves K, Peshkin BN, Valdimarsdottir HB, et al. Intentions for risk-reducing surgery among high-risk women referred for BRCA1/BRCA2 genetic counseling. Psychooncology. 2014. doi:10.1002/pon.3560.
Zakhartseva LM, Gorovenko NG, Podolskaya SV, Anikusko NF, Lobanova OE, Pekur KA, et al. Breast cancer immunohistochemical features in young women with BRCA1/2 mutations. Exp Oncol. 2009;31:174–8.
Kitsera NI, Shparyk IV, Bilynskyi BT, Tril OV, Mashalyga MS, Oleksyak OO, et al. Analysis of mutations in the genes BCRA1/2 in patients withfamily/hereditary breast cancer which live in the Lviv region (Ukraine). Onkologiia. 2012;11:44–9 (in Ukrainian).
Kruk TV, Peresunko OV, Volkov RA. A molecular genetics study of the types of BRCA1 gene mutations in breast cancer patients and their relatives in the Chernivtsi region of Ukraine. Novoutvorennia. 2012;12:310–4 (in Ukrainian).
Hossein R. Molecular genetic markers of breast cancer in patients of different age groups. PhD thesis. 2012.
Rybchenko LA. Optimization of mutations determination in the BRCA1/2 genes for medical genetic counseling of women about breast cancer. PhD thesis. 2014.
Karami F, Mehdipour P. A comprehensive focus on global spectrum of BRCA1 and BRCA2 mutations in breast cancer. Biomed Res Int. 2013. doi:10.1155/2013/928562.
Navarro de Souza A, Groleau D, Loiselle CG, Foulkes WD, Wong N. Cultural aspects of healthy BRCA carriers from two ethnocultural groups. Qual Health Res. 2014;24:665–81.
Sharma P, Klemp JR, Kimler BF, Mahnken JD, Geier LJ, Khan QJ, et al. Germline BRCA mutation evaluation in a prospective triple-negative breast cancer registry: implications for hereditary breast and/or ovarian cancer syndrome testing. Breast Cancer Res Treat. 2014;145:707–14.
Rubinstein WS. Hereditary breast cancer in Jews. Fam Cancer. 2004;3:249–57.
Chan PC, Wong BY, Ozcelik H, Cole DE. Simple and rapid detection of BRCA1 and BRCA2 mutations by Multiplex Mutagenically Separated PCR. Clinical Chemistry. 1999;45:1285–7.
Bogdanova NV, Antonenkova NN, Rogov YI, Karstens JH, Hillemanns P, Dörk T. High frequency and allele-specific differences of BRCA1 founder mutations in breast cancer and ovarian cancer patients from Belarus. Clin Genet. 2010;78(4):364–72.
Gaj P, Kluska A, Nowakowska D. High frequency of BRCA1 founder mutations in Polish women with nonfamilial breast cancer. Familial Cancer. 2012;11:623–8.
Sokolenko AP, Mitiushkina NV, Buslov KG, Bit-Sava EM, Iyevleva AG, Chekmariova EV, et al. High frequency of BRCA1 5382insC mutation in Russian breast cancer patients. Eur J Cancer. 2006;42:1380–4.
Edlich RF, Winters KL, Lin KY. Breast cancer and ovarian cancer genetics. J Long Term Eff Med Implants. 2005;15(5):533–45.
Acknowledgements
The authors thank Prof., Dr. Steven Narod, University of Toronto, for his help in writing this manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
IG and SS detected the BRCA1 mutations 5382insC by multiplex mutagenically separated PCR, TL extracted DNA, NL, NA, VC, IS, SS, SP and OB sampled peripheral blood from breast cancer patients and collected the patient's history, LO, SD and IK conceived of the study, and participated in its design and coordination and helped to draft the manuscript. All authors read and approved the final manuscript.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Gorodetska, I., Serga, S., Levkovich, N. et al. The frequency of BRCA1 founder mutation c.5266dupC (5382insC) in breast cancer patients from Ukraine. Hered Cancer Clin Pract 13, 19 (2015). https://doi.org/10.1186/s13053-015-0040-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13053-015-0040-3