Abstract
Pulmonary contusion and acute respiratory distress syndrome (ARDS) is a common manifestation in polytraumatic patients. Although mechanical ventilation is still the first choice of treatment, a group of patients are still unable to maintain their oxygenation. The role of extracorporeal membrane oxygenation (ECMO) has been more clarified when the lung is extensively damaged and when conventional modality failed. ECMO provides the lung an opportunity to rest by permitting reduced ventilator settings and limiting further barotraumas. However, ECMO is still considered contraindicated in polytramatic patients combining pulmonary contusion and other organ hemorrhage because of systemic anticoagulation during the treatment. We herein report a patient who successfully survive a multitrauma combining pulmonary contusion and grade IV liver laceration using non-heparinized venovenous extracorporeal membrane oxygenation (vv-ECMO). The associated literature were reviewed.
Similar content being viewed by others
Introduction
Acute pulmonary failure is a common manifestation in polytraumatic patients. The mechanism included pulmonary contusion, acute respiratory distress syndrome (ARDS) resulting from any inflammation process such as aspiration pneumonia, or fat embolism because of long bone fracture [1]. The management could be very challenging despite advances in critical care management.
Extracorporeal membrane oxygenation (ECMO) serves as the final method when conventional mechanical ventilation fails to maintain the oxygenation. It helps maintain systemic tissue oxygenation via extracorporeal circuit when the lung function is compromised [2,3]. However, the situation became more complicated when the lung failure combines other vital organ damage and risk of bleeding because of systemic anticoagulation during the treatment.
The introduction of heparin-free ECMO seems to be the possible solution for such dilemma. We report our experience of using heparin-free vv-ECMO to help a patient survive a trauma combining acute pulmonary failure and severe liver subcapsular laceration. The literature regarding the application of ECMO in polytraumatic patients combining acute pulmonary failure and other vital organ damage were reviewed.
Case report
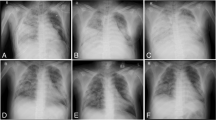
A 19-year-old man suffered from a multi-trauma after a traffic accident when he was riding a motorcycle and collided into a car. Upon arrival at our tertiary trauma center, he initially presented with a Glasgow Coma Score of 8 and severe hypoxia. He was intubated immediately. Large amount of food content was sucked from the endotracheal tube. Primary chest computed tomography (CT) reported right lung consolidation with patchy opacities, which was consistent with a combination of blunt chest contusion and aspiration pneumonia (Figure 1). Abdominal CT showed grade IV laceration over bilateral hemiliver without evident contrast extravasation (Figure 2). The gas exchange did not improve despite of mechanical ventilation, and the patient still presented with severe hypoxemia. The parameter about respiration showed PaO2/FiO2: 70.2 under invasive ventilation (pressure-mode inverse ratio ventilation, I:E 2:1). ECMO was thus recommended for lung contusion, aspiration pneumonia and acute pulmonary failure.
With regards of a polytraumatic patient combining liver laceration, ECMO is contraindicated because the need of systemic anticoagulation may induce further internal bleeding. A heparin-free, vv-ECMO was thus suggested. An extracorporeal circuit was constructed via a venous access through internal jugular vein and femoral vein, using Seldinger technique. The blood flow was set at the rate of 2.42 L/min, and the FiO2 was set at 45%. The oxygenation status improved dramatically after the introduction of ECMO (Table 1). The liver laceration was treated conservatively. The patient weaned from ECMO five days later, and was extubated nine days later. The total intensive care unit stay was 10 days, and he discharged after a sixteen-day hospitalization. There was no ECMO related complications during the course.
Literature review
We searched the PubMed (2000–2013) database for case reports about the launch of ECMO regardless of heparin-containing or heparin-free in multi-trauma patients. The abstracts of all articles published in English were screened. The full texts of articles published in other languages but with an abstract in English were analyzed. Articles were selected for review if they included the following patient data: age, sex, clinical presentation, combined injury besides acute pulmonary failure, the details of ECMO treatment, and the outcome.
There were six case reports containing 11 patients described in detail, and one clinical paper containing 10 cases found in the literature, which are listed in Table 2.
Discussion
Despite of the various mechanical ventilation technique and the improved knowledge of the adjustment of ventilation parameters, a group of patients with traumatic pulmonary contusion or ARDS are still unable to benefit from these technique. ECMO has been proved to be an rescue therapy when conventional methods are ineffective. ECMO was also reported to be effective in polytraumatic patients combining pulmonary contusion and other organ damage including bronchial rupture [2,4], endobronchial hemorrhage [5], blunt abdominal trauma (BAT) with internal bleeding necessitating exploratory laparotomy [6], or traumatic brain injury [7-10]. However, the use of ECMO on patients with a preexisting bleeding risk without need of immediate operation is still rarely reported.
The application of heparin-free ECMO has been proposed recently to overcome the dilemma. Muellenbach et al. reported three successful cases of heparin-free vv-ECMO on a patient with traumatic lung failure and severe traumatic brain injury [9]. Matthias et al. reported that six of ten polytraumatic patients with coexisting pulmonary failure or cardiopulmonary failure and bleeding shock survived using a heparin-free ECMO, which is by far the only largest series in the literature [6]. However, ECMO is still a controversy on a multitrauma combining pulmonary failure and blunt abdominal trauma needing only nonoperative management. Of the total 11 cases reported in detail in the literature (Table 2), six patients had concurrent BAT with liver or spleen laceration [2,4,8,9]. Only one received successful nonoperative treatment for grade III liver laceration [4].
The improvement of ECMO technique including centrifugal pumps and heparin-coated circuits reduced the amount of heparin needed. However, with regards to a patient who had spontaneous hemostasis on liver laceration, we still chose the heparin-free method to reduce the risk of rebleeding. Based on the hemodynamic stability and the daily improvement of lung condition, we did not used additional method to prevent clotting of the circuit except the close monitor of ACT. The duration of ECMO was five days, which is comparable to other report.
Conclusion
ECMO can serve as a rescue method to provide the traumatic lung to rest. Although it was previously regarded to be contraindicated in polytraumatic patient with coexisting organ hemorrhage, there are growing successful experiences reported recently. We report a heparin-free, vv-ECMO method for patients combining acute pulmonary failure and nonoperative liver laceration, which may extend the feasibility of ECMO in polytraumatic patients.
Consent
Written informed consent was obtained from the patient for the publication of this report and any accompanying images.
Abbreviations
- ECMO:
-
Extracorporeal membrane oxygenation
- ARDS:
-
Acute respiratory distress syndrome
- v-v ECMO:
-
Venovenous ECMO
- CT:
-
Computed tomography
- FiO2 :
-
Fraction of inspired oxygen
- BAT:
-
Blunt abdominal trauma
- SDH:
-
Subdural hemorrhage
- EDH:
-
Epidural hemorrhage
- ICH:
-
Intracerebral hemorrhage
- ICP:
-
Intracerebral pressure
- V-a ECMO:
-
Venoarterial ECMO
- V-va ECMO:
-
Veno-venoarterial ECMO
References
Cordell-Smith JA, Roberts N, Peek GJ, Firmin RK. Traumatic lung injury treated by extracorporeal membrane oxygenation (ECMO). Int J Care Injured. 2006;37:29–32.
Madershahian N, Wittwer T, Strauch J, Franke UF, Wippermann J, Kaluza M, et al. Application of ECMO in multitrauma patients with ARDS as rescue therapy. J Card Surg. 2007;22:180–4.
Michaels AJ, Schriener RJ, Kolla S, Awad SS, Rich PB, Reickert C, et al. Extracorporeal life support in pulmonary failure after trauma. J Trauma Inj Infect Crit Care. 1999;46:638–45.
Campione A, Agostini M, Portolan M, Alloisio A, Fino C, Vassallo G. Extracorporeal membrane oxygenation in respiratory failure for pulmonary contusion and bronchial disruption after trauma. J Thorac Cardiovasc Surg. 2007;133:1673–4.
Yuan K-C, Fang J-F, Chen M-F. Treatment of endobronchial hemorrhage after blunt chest trauma with extracorporeal membrane oxygenation (ECMO). J Trauma. 2008;65:1151–4.
Arlt M, Philipp A, Voelkel S, Rupprecht L, Mueller T, Hilker M, et al. Extracorporeal membrane oxygenation in severe trauma patients with bleeding shock. Resuscitation. 2010;81:804–9.
Yen T-S, Liau C-C, Chenc Y-S, Chaoa A. Extracorporeal membrane oxygenation resuscitation for traumatic brain injury after decompressive craniotomy. Clin Neurol Neurosurg. 2008;110:295–7.
Friesenecker BE, Peer R, Rieder J, Lirk P, Knotzer H, Hasibeder WR, et al. Craniotomy during ECMO in a severely traumatized patient. Acta Neurochir. 2005;147:993–6.
Muellenbach RM, Kredel M, Kunze E, Kranke P, Kuestermann J, Brack A, et al. Prolonged heparin-free extracorporeal membrane oxygenation in multiple injured acute respiratory distress syndrome patients with traumatic brain injury. J Trauma Acute Care Surg. 2012;72:1444–7.
Muellenbach RM, Redel A, Kuestermann J, Brack A, Gorski A, Rosner T, et al. Extracorporeal membrane oxygenation and severe traumatic brain injury. Is the ECMO-therapy in traumatic lung failure and severe traumatic brain injury really contraindicated? Anaesthesist. 2011;60:647–52.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
PHW is the first author who reviewed the medical records and wrote the main article. WHC is the visiting staff who was in charge of the patient during the hospitalization, and serves as the corresponding author. YCC is the vascular surgeon responsible for the ECMO use. YLC is the chief of the surgery department and the vice superintendent of Changhua Christian Hospital who coordinated between the department. CPC is the chief of the trauma department who coordinated the trauma team. PYL is the doctor in research department responsible for article review. All authors read and approved the final manuscript.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Wen, PH., Chan, W.H., Chen, YC. et al. Non-heparinized ECMO serves a rescue method in a multitrauma patient combining pulmonary contusion and nonoperative internal bleeding: a case report and literature review. World J Emerg Surg 10, 15 (2015). https://doi.org/10.1186/s13017-015-0006-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13017-015-0006-9