Abstract
Background
A cancer diagnosis elicits greater distress than any other medical diagnosis, and yet very few studies have evaluated the efficacy of structured online self-help therapeutic programs to alleviate this distress. This study aims to assess the efficacy over time of an internet Cognitive Behaviour Therapy (iCBT) intervention (‘Finding My Way’) in improving distress, coping and quality of life for individuals with a recent diagnosis of early stage cancer of any type.
Methods/Design
The study is a multi-site Randomised Controlled Trial (RCT) seeking to enrol 188 participants who will be randomised to either the Finding My Way Intervention or an attention-control condition. Both conditions are delivered online; with 6 modules released once per week, and an additional booster module released one month after program-completion. Participants complete online questionnaires on 4 occasions: at baseline (immediately prior to accessing the modules); post-treatment (immediately after program-completion); then three and six months later. Primary outcomes are general distress and cancer-specific distress, with secondary outcomes including Health-Related Quality of Life (HRQoL), coping, health service utilisation, intervention adherence, and user satisfaction. A range of baseline measures will be assessed as potential moderators of outcomes. Eligible participants are individuals recently diagnosed with any type of cancer, being treated with curative intent, aged over 18 years with sufficient English language literacy, internet access and an active email account and phone number. Participants are blinded to treatment group allocation. Randomisation is computer generated and stratified by gender.
Discussion
Compared to the few prior published studies, Finding My Way will be the first adequately powered trial to offer an iCBT intervention to curatively treated patients of heterogeneous cancer types in the immediate post-diagnosis/treatment period. If found efficacious, Finding My Way will assist with overcoming common barriers to face-to-face therapy in a cost-effective and accessible way, thus helping to reduce distress after cancer diagnosis and consequently decrease the cancer burden for individuals and the health system.
Trial registration
Australian New Zealand Clinical Trials Registry ACTRN12613000001796 16.10.13
Similar content being viewed by others
Background
Despite improvements in treatment and survival rates, a cancer diagnosis continues to elicit greater distress than any other medical diagnosis [1]. Research has consistently found that 30 to 40 per cent of recently diagnosed patients experience clinically significant depressive or anxiety disorders [2,3]. Distress is most acute during the first 12 months after diagnosis, when a range of medical treatments take place, following which the prevalence reduces to levels comparable with the community [4]. Consequently, distress management within the first 12 months after diagnosis has been recognised as an integral component of a patient’s clinical treatment [5,6]. Despite this, distress and psychiatric disorders among cancer patients often go under-recognised and untreated [7]. This particularly applies to the 30% of Australian cancer patients who reside in rural or regional areas, where access to specialist cancer services is limited [6].
Psychological approaches that alleviate distress
Over the past two decades, a range of psychological interventions to alleviate distress have been empirically investigated, predominantly among women with breast cancer. Intervention research has focused on developing and evaluating interventions that target the known psychological predictors of maladjustment [8], namely, low social support, prior anxiety and depression (vulnerability to distress), and maladaptive coping, particularly repression of emotions, helplessness/hopelessness, and cognitive and behavioural avoidance. Interventions tested have included those based on Cognitive Behavioural Therapy (CBT) [9], Supportive Expressive Therapy (SET) [10], psycho-educational programs [11], mindfulness-based therapy [12], and peer-support groups [13]. There is clear meta-analytic evidence that all of these conventional psychosocial interventions are efficacious compared to control groups in facilitating adjustment [14]; with large effect sizes (ES) found for depression (ES = 1.2), anxiety (ES = 1.99), and functional adjustment / quality of life (QOL) (ES = 0.91) [14]. However, CBT has the largest evidence base for treating cancer-related distress to date [14], with most studies suggesting that treatment for distress at the time of cancer diagnosis is more effective than after cancer treatment has been completed [11].
Need for novel approaches to improve access
While demonstrably efficacious, there several barriers to attending face-to-face therapy in the Australian setting. First, there are limited psychosocial services freely available in the public health setting, with the current capacity not sufficient to meet the demand [6]. This is particularly evident in rural and remote areas where access to multidisciplinary cancer care is problematic, and resulting inequities in health outcomes are well recognised [6]. Second, even when psychosocial services are offered in urban settings, research suggests that less than 25% of Australians attend [15], with low attendance attributed to a variety of barriers including: personal barriers, such as ongoing stigma associated with seeking mental health assistance [16,17], and illness-related barriers such as patients’ reduced physical capacity for additional appointments [17]. As a result of these barriers, national government supportive care policies have recognised that innovative methods of increasing access to supportive care throughout the treatment trajectory are required for all cancer patients [6].
One such innovative method of increasing patient access to supportive care is through internet-based provision of psychosocial services [16-18]. Since 2000 a plethora of randomised controlled trials and systematic reviews have examined internet-based interventions for both psychological [19,20] and physical [17,18] health complaints. Of these interventions, self-guided web-based interventions offer the particular advantage of overcoming the majority of the barriers discussed above for both rural and urban patients, along with anonymity, privacy and convenience of progressing through a program at the user’s own pace. Such interventions tend to be highly structured into modules, are derived from theory (predominantly cognitive behaviour therapy), and have been adapted from existing evidence-based print-resources or face-to-face therapy [21]. Consistent with research on face-to-face therapy, internet Cognitive Behaviour Therapy (iCBT) interventions have the largest evidence base for efficacy in improving both mental health conditions [22] and, increasingly, coping with chronic physical health conditions [17,18].
Status of iCBT for cancer distress
Given that cancer consumers prefer multi-media to print resources [23], and that 84% of Australians have access to the internet [24], web-based interventions, and in particular iCBT-based interventions, appear a logical format for the wide dissemination of psychological treatment for cancer patients. However, the evidence-base for self-guided iCBT-based psychological therapy in cancer is only now emerging [25-28].
Two groups [26,28] developed and evaluated structured self-guided online CBT-based coping programs for women with recently diagnosed early-stage breast cancer. Similar in design, their programs were both multi-component, and contained 6–10 self-guided CBT-based modules, biomedical information, links to other cancer resources and websites, and asynchronous discussion boards. Both studies showed evidence for the efficacy of their respective interventions: The smaller of the two studies [28] found one significant interaction where women with poorer baseline perceived health status experienced greater improvements in perceived health over time when assigned to the intervention, despite a small sample and consequent lack of power. The larger study [26] found the intervention was efficacious in improving self-efficacy for coping with cancer, regulating negative mood, and reducing cancer-related post-traumatic symptoms. However, as each of these studies involved only breast cancer patients, efficacy could not be demonstrated across cancer types.
In the third study, Duffecy et al. [27] ran a small RCT of 31 post-treatment survivors of various cancer types to examine the feasibility and acceptability of an 8-week Internet Support Group (ISG) combined with an Individual Internet Intervention (III), compared with the III alone. The study supported feasibility and acceptability of the combined program, and found that both conditions produced large reductions in depressive symptoms in participants with high baseline distress. However, the study was underpowered to detect improvement over time and time x treatment effects; further, it examined efficacy in post-treatment survivors, rather than patients currently undergoing treatment. Current CBT literature suggests that a more effective time to implement such interventions may be in the immediate post-diagnosis period, when patients are likely to be experiencing higher levels of distress generally [4].
Our research group was the first to pilot test a 6-week iCBT program for people with any type of early stage/curatively treated cancer, and designed to be delivered soon after diagnosis [25]. In contrast to the previous three programs which all depended on group-support as a key feature, our study tested an individual self-guided web-based intervention for newly diagnosed patients that was independent of moderators and peer-support components, and was therefore consistent with the large evidence base for CBT [14]. Program content was derived from our evidence-based print self-help breast cancer workbook [29], but heavily revised and expanded to ensure relevance to heterogeneous cancer populations. In a case-series design, participants (n = 12) were assessed at baseline and after completing the program. Analysis found the intervention led to reductions with moderate associated effect sizes in negative affect, helplessness/hopelessness, anxious preoccupation, and fatalism. Results therefore provided preliminary support for the potential efficacy of the web-based CBT program for improving cancer-related distress and anxious preoccupation after cancer diagnosis. However, the pilot nature of this study and small sample size meant that the efficacy of the intervention compared with a control condition could not be established.
In summary, the four studies published to date provide preliminary evidence of the feasibility of iCBT interventions for delivering psychosocial interventions for coping with cancer. However, studies examining the efficacy of iCBT programs aimed at heterogeneous cancer types have so far been limited by either (1) small sample sizes and consequent lack of power, (2) lack of a control condition, and/or (3) not providing analysis of the longer-term impact of the intervention. Further, only our group have investigated a self-guided intervention that is (a) independent of discussion board components and therefore truly self-guided and (b) applicable to delivery soon after diagnosis, as opposed to post cancer treatment, and therefore consistent with CBT literature suggesting that treatment for distress at the time of cancer diagnosis is more effective than treatment for distress after treatment for cancer.
This paper reports on the protocol for the proposed RCT to examine the effectiveness of the iCBT intervention in a multisite setting.
Aims and hypotheses
This study aims to evaluate the efficacy of the next iteration of our self-help internet cancer coping intervention (‘Finding My Way’) in improving wellbeing and quality of life of early-stage cancer patients over time, using a multi-site RCT.
A secondary aim is to investigate moderators of therapeutic change, consistent with recommendations that RCTs should identify who benefits most, and under what conditions, from psychosocial interventions [30]. For the present study, factors that have been previously shown to predict distress will be examined for their potential to moderate the effects of the intervention; namely, availability of social support, cognitive vulnerability to distress, and motivation to seek information [8,31].
Therefore it is hypothesised that:
-
1.
Intervention participants will report greater improvements compared to attention-control participants in the primary outcome, distress, from baseline to post-treatment and 3- and 6-month follow-up;
-
2.
Intervention participants will report greater improvements compared to attention-control participants in the secondary outcomes coping and HRQOL over time;
-
3.
Primary and secondary outcomes will be moderated such that
-
a.
The significant changes over time in distress between groups will be moderated by social support, cognitive vulnerability to distress, and motivation to seek information, and
-
b.
The significant changes over time in coping and HRQOL between groups will be moderated by social support, cognitive vulnerability to distress, and motivation to seek information.
-
a.
Methods/Design
Study design
Finding My Way (FMW) is a national level multi-site randomised controlled trial registered with the Australian and New Zealand Clinical Trials Registry with the registration number ACTRN12613000001796. Ethical approval to conduct the study has been sought and obtained from the Southern Adelaide Clinical, Royal Brisbane and Women’s and ACT Health Human Research Ethics Committees. Randomisation occurs at the patient level: patients are randomised to receive either the FMW intervention or an online attention-control. Procedural elements of this study follow CONSORT guidelines [32]. Attrition is monitored and reasons for non-participation and withdrawal are recorded in each arm. Data extraction and entry will be performed by research team members blinded to group allocation.
Setting
Participation in the study occurs entirely online. The web-program is hosted by Flinders University (www.findingmyway.org.au), with Flinders University as the administering institution.
Participants
Inclusion criteria
Patients are eligible to participate if they have been diagnosed with any cancer (e.g., breast, prostate, colorectal, testicular, lymphomas, haematologic or gynaecologic malignancies); their cancer is being treated with curative intent; they are currently receiving active cancer treatment (surgery, chemotherapy, radiotherapy), or, if they received surgery alone, have been diagnosed within the last six months; they are aged 18 years or over; and they have sufficient English language literacy to understand the information sheet and consent form and navigate the website, access to the internet (home or work), and an active email address and phone number.
Exclusion criteria
Patients are ineligible to participate if they have a diagnosis of advanced cancer.
Withdrawal criteria
Patients who opt to withdraw from the study are asked if they would consent to continue completing follow-up measures, and for any existing data to be included in analyses. If consent is not given, their data will be erased from the database along with any documentation related to their involvement.
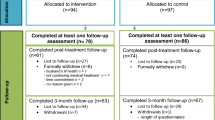
Recruitment
An overview of recruitment and enrolment processes is provided in Figure 1. Participants are recruited from Australian hospitals and cancer centres according to any of the following methods:
-
1.
Self-referral: Participants self-refer to the website in response to advertisements placed in local and national newspapers, on websites or in newsletters of cancer agencies or support networks, or in waiting areas of cancer agencies and clinics of participating hospitals.
-
2.
Direct approach: Potential participants are approached directly by cancer clinicians or research assistants at participating hospitals, and are given a flyer containing a brief overview of the program and the website address. Verbal consent is obtained at this time for the research coordinator to provide either (i) a single reminder phone call, during which the research coordinator provides further information about the study and obtains the participants’ email address in order to send a direct link to the website, or (ii) when the patient cannot be contacted by phone, a single reminder letter providing further information about the study including the website address.
-
3.
Letters of invitation: Letters printed on the site’s letterhead and signed by the department head are sent to patients missed in clinic. These letters ask patients to consider participation and allow contact by the researchers (via an opt-out response slip). A single reminder phone call is then made to all patients invited to take part in the study if they do not respond to the invitation letter after two weeks. Protocol at some sites requires that a clinician/ research assistant from the recruiting hospital contacts the patient to obtain verbal consent for patient details to be provided, prior to contact by the research coordinator.
Enrolment
Participants follow the email link or type in the web address in order to access the website and register for the program. Registration generates an automatic email to the participant containing a link to activate their account. Following account activation, participants are directed to read an online information page and consent form. Eligibility criteria are clearly highlighted on the information page, and consent requires participants to check a box stating they do not have advanced cancer. Consent is obtained by the participant clicking on an “I agree” button on the online consent form.
Following the consent process, participants complete the baseline questionnaire. Participants are then randomised to either the intervention or attention-control condition and are directed to a welcome tutorial and their user home screen, from which they are able to access their first module immediately. Participants work through 6 modules: one new module is accessible each week, along with previously accessed modules. The order of module release is self-determined during a goal-setting exercise conducted when first logging into the program, which allows participants to identify which topics are most immediately relevant to them, and can be subsequently modified if certain topics become more relevant as participants progress through the program. Participants receive automated email reminders to use the program each week. A booster module, comprised of a summary of the key information points from the program and links back to topics and worksheets, is accessible one month later. The opportunity to provide qualitative and quantitative feedback is provided at the end of each module.
Randomisation
This study is a parallel RCT, with equal numbers of participants randomised to the intervention and control arms. Randomisation is automated within the website; the random allocation sequence is generated by a researcher blinded to the identity of participants using computer-generated random numbers, and allocation is then automated by the website in a 1:1 ratio. Randomisation is stratified by gender.
Blinding
Participants are blinded to their intervention assignment; while they are aware there are two different versions of the website (explained as ‘information’ and ‘activities’ versions), they are not informed that one is a ‘control’ condition, are not aware which is the primary intervention being evaluated, and are blinded as to their own treatment group allocation. A list of blinded participant details is accessible to the research assistant for the purposes of conducting reminders about follow-up surveys.
Intervention and control arms
Intervention
Finding My Way is a 6-week password-protected CBT internet application comprised of three main components: (1) psycho-education, (2) cognitive-behavioural worksheets/strategies including worksheets, quizzes, relaxation and meditation exercises, and (3) survivor testimonials. Each week a new module is released to participants, and participants can continue referring back to previous modules throughout the study.
The 6 modules address: (i) starting treatment – working with your medical team, covering assertive communication and decision making, (ii) coping with physical symptoms and side effects – including fatigue, pain, insomnia, and provides activity pacing worksheets, and relaxation audiotracks; (iii) coping with emotional distress – which covers depression, anxiety, anger and stress, and provides cognitive restructuring diaries, and mindfulness audio-tracks; (iv) body image, identity and sexuality – with psychosexual worksheets, and therapeutic writing activities; (v) your family and friends – comprising further assertive communication and needs assessment worksheets; and (vi) completing treatment, which includes self-management strategies to facilitate healthy lifestyles.
A private online note-taking feature, mood monitoring/management, and a resource section with links to reputable cancer-related organisations and other health websites are also available throughout the duration of the program. The program is outlined in Table 1.
Attention control
An information-only version of Finding My Way, developed to provide an appropriate attention control for the study, covers the same 6 module topics without any of the worksheets, activities, relaxation exercises, or note-taking feature. Our previous research indicates that an attention control condition does not significantly reduce distress [29], and provides a more rigorous test of the intervention.
Outcomes
Primary, secondary and moderator outcomes are assessed using online self-report questionnaires. Baseline questionnaires are completed upon enrolment/ prior to randomisation. Post treatment questionnaires are completed at the conclusion of the sixth module (seven weeks after completing the baseline survey), and follow-up questionnaires are completed approximately 3 months and 6 months after treatment completion.
Primary outcome: distress
The primary outcome for this study is distress, measured as general distress and as cancer-specific distress. General distress is measured using the total scale score of the 21-item Depression Anxiety Stress Scale – short form (DASS: [33]), which assesses levels of anxiety, depression and stress over the previous week on a four-point scale ranging from (0) Did not apply to me at all to (3) Applied to me very much, or most of the time. Cancer-specific distress is measured using the 17-item Posttraumatic Stress Scale-Self Report [34], which measures on a 4-point scale (0 = Not at all or only one time, 3 = 5 or more times per week / almost always), the severity of each DSM-IV post-traumatic stress disorder symptom criterion in terms of how often respondents experienced each symptom in the previous week. For this study, the measure was adapted in order to reflect cancer diagnosis as the stressor.
Secondary outcomes
Secondary outcomes for this study include Health-Related Quality of Life (HRQOL), coping, and the economic impact of the intervention in terms of Health Service Utilisation. HRQOL is measured using the European Organisation for Research and Treatment of Cancer Quality of Life Core Questionnaire [35], a 30-item comprehensive health related quality of life assessment for cancer patients which yields a global QOL score, and five functional subscales (physical, emotional, social, role, cognitive).
Coping is measured with the mini-Mental Adjustment to Cancer Scale (mini-MAC: [36]), a 29-item scale yielding 5 factors: Fighting Spirit, Helplessness/Hopelessness, Anxious Preoccupation, Fatalism, and Cognitive Avoidance. Items are responded to on a 4-point scale ranging from ‘definitely does not apply’ to ‘definitely does apply’.
Health Service Utilisation is examined using the 17-item Health Service Utilisation Questionnaire [37], which assesses health service use in the previous 12 months in terms of whether patients have been hospitalised and the number of visits to doctors and other health professionals. Hospitalisation is indicated as no/yes day only/yes spent at least one night (with number of days then recorded). Visits to GPs/hospital doctors/specialist doctors are indicated on a 7-point scale ranging from none to 25 or more times, and utilisation of other health professionals (e.g. physiotherapist) is indicated as yes or no.
Moderators of outcomes
Participant and medical characteristics, availability of social support, information-seeking preferences, emotion regulation, vulnerability to cancer-distress, adherence to the program, and participant satisfaction are assessed as postulated moderators of program efficacy.
Participant and medical characteristics are assessed at baseline only, and consist of age, marital status, occupational status, annual gross income, level of educational attainment, area of residence (rural/urban, state), ethnicity, cancer type, time since diagnosis, treatment received (surgery, chemotherapy, radiotherapy, hormonal therapy, other), any other chronic health conditions, and other support-services accessed.
Availability of social support is assessed using the 20-item Medical Outcome Study Social Support Survey [38], which consists of four subscales: emotional/informational, tangible, affectionate, and positive social interactions, with availability of the support type listed in each item rated on a 5-point scale (1 = none of the time, 5 = all of the time).
Information seeking preferences in terms of the type and amount of cancer information sought by patients is measured by the Miller Behavioral Style Scale scale [39]. This scale identifies information seekers who look for and amplify threat-related cues (monitors) and distracters who avoid and minimize such cues (blunters), and has been used extensively in cancer populations. The scale asks the respondent to imagine two stress-evoking scenarios, each of which is followed by eight statements that describe different ways of coping with the stressor, with four statements being of a monitoring or information-seeking variety and four of a blunting or information-avoiding variety. Respondents are asked to check all statements that apply to them.
Vulnerability to distress is assessed using the Difficulties in Emotion Regulation Scale [40], a 36-item measure of difficulties in emotion regulation across six dimensions, namely a) lack of awareness of emotional responses, b) lack of clarity of emotional responses, c) non-acceptance of emotional responses, d) limited access to emotion regulation strategies perceived as effective, e) difficulties controlling impulses when experiencing negative emotions, and f) difficulties engaging in goal-directed behaviours when experiencing negative emotions. Participants respond to each item on a 5-point scale (1 = almost never, 5 = almost always).
Adherence to the study is measured in two ways. First, the self-help compliance scale [41] measures participant self-reported engagement with program’s (i) information, (ii) worksheets, and (iii) weekly time usage. Second, website use indicators are tracked on the website itself, including: number of visits, length of time logged in, and number of modules and worksheets completed.
Finally, levels of satisfaction with the website will be assessed as a measure of whether this intervention improved psychosocial support for patients. Qualitative feedback will be gathered within the website, and at follow-up assessments.
Analysis
Sample size
Longitudinal sample size calculation for repeated measures was conducted using a program developed by Hedeker [42]. Previous online interventions targeting distress in community samples have effect sizes ranging from .42 to .65 for depression, and from .29 to 1.74 for anxiety [19]. Therefore, a conservative small-to-moderate effect size was selected for the current study. Based on the pilot RCT findings, an attrition rate of 21% at each of the assessment points can be expected [29]. Thus for a study with 2 groups and 4 assessment points, power set at 0.80, statistical significance set at α = .05 (two tailed), total attrition set at 21%, an effect size set at 0.35 SD, and an expected primary endpoint standard deviation of 4.0 at each time point [43], 94 participants per group are required, summing to a total sample of 188 participants.
Statistical analysis
Quantitative data will be analysed using the Statistical Package for the Social Sciences (SPSS) Version 17.0. Baseline differences between groups will be investigated using t-tests for continuous measures and χ2 tests of independence for categorical measures. Linear Mixed Effects Models (LMEM) will be employed to examine the efficacy of the intervention. The LMEM calculates a regression line for each individual while controlling for baseline observation (fixed main effects). Baseline observations will be entered as covariates to eliminate the influence of baseline variability, resulting in a 2 (group: intervention; control) X 3 (time: post-program; 3-month follow-up; 6 month follow-up) fixed effects model for each outcome variable, with random effects accounting for individual variation. This approach effectively equalises conditions at baseline and consequently allows for direct comparison between conditions at each follow-up point. In this context, (a) interactions between condition and time, (b) main effects of group and (c) post-hoc pairwise comparisons at each follow-up point are all indicators of intervention effects. This analysis offers the benefit of estimation maximisation; it provides joint modelling for each participant of observed and missing data based on maximising likelihood for population parameters as a function of the observed data. LMEM analyses are therefore robust with respect to handling missing data and unbalanced designs in longitudinal research as all participants with at least one observed post-treatment data point are included. That is, as baseline data is entered as a covariate, participants who do not complete any of the post-program assessments are not retained. To overcome this limitation and ensure this trial adopts a fully intention-to-treat design, multiple imputation will be performed for participants with only baseline-data. Therefore all participants, regardless of missing data at one or more assessment points, will be included in analyses and accurate parameter estimates obtained. Within-group effect sizes and reliable change indices will be calculated to provide a measure of the magnitude and clinical significance of changes respectively. To test for moderation, separate LMEM analyses will be conducted for each combination of moderator and outcome variable, where the moderator and group are entered in model 1 to control for main effects. The product term is then entered in model 2, to represent the interaction between group and moderating variable, and will indicate the moderating effect.
Discussion
Internet-based self-help modalities represent one means of overcoming existing barriers to cancer patients accessing supportive care and psychosocial services, including the lack of such services within the public health system, particularly for rural patients, and barriers to attendance even where such services are provided. However, previous studies examining the efficacy of web-based self-help modalities for cancer populations have suffered from a range of limitations including (1) lack of an established psychological model (such as CBT) as the basis for the program, (2) lack of a control condition (3) small sample size and consequent lack of power for analyses, (4) lack of follow-up analysis over time, (5) examining efficacy of programs for one cancer type (i.e. breast cancer) only, as opposed to heterogeneous cancer types, and/or (6) examining programs implemented after completion of cancer treatment, as opposed to soon after diagnosis when distress tends to be highest and psychological treatment most warranted.
To our knowledge, Finding My Way is unique in offering an iCBT intervention applicable to individuals with heterogeneous cancer types soon after diagnosis. The large scale of this national multi-site RCT will therefore enable examination of the efficacy of such a program in reducing patient distress, improving coping and health related quality of life, and reducing health service utilisation in individuals with a range of cancer diagnoses. Furthermore, this study offers the important contribution of evaluating potential moderators of change. This information can be of benefit clinically when determining who to refer for online-interventions (versus who may be more suitably treated via other modalities) as well as benefitting future research via the refinement of inclusion and exclusion criteria, improving trial stratification and increasing power [30]. Indeed, it has been suggested that results of treatment trials are often weak because moderators of treatment are not examined, thus they should be part and parcel of any treatment study [30]; however, few studies have specifically examined moderators of psycho-oncology interventions.
If found efficacious, Finding My Way will represent an important means of overcoming common barriers to face-to-face therapy in a cost-effective and accessible way, which may particularly assist those residing in rural/remote areas. Integration of such a program into the supportive care offered to cancer patients within the health system will therefore be a promising avenue for reducing patient distress after cancer diagnosis, and consequently for decreasing the cancer burden both on individuals and within the health system.
Abbreviations
- CBT:
-
Cognitive behaviour therapy
- DASS:
-
Depression anxiety stress scales
- ES:
-
Effect size
- FMW:
-
Finding My Way
- HRQoL:
-
Health related quality of life
- iCBT:
-
Internet cognitive behaviour therapy
- ISG:
-
Internet support group
- LMEM:
-
Linear mixed effects models
- mini-MAC:
-
Mini Mental Adjustment to Cancer Scale
- QOL:
-
Quality of life
- RCT:
-
Randomised controlled trial
- SET:
-
Supportive expressive therapy
- SPSS:
-
Statistical package for the social sciences
References
Turner J, Zapart S, Pedersen K, Rankin N, Luxford K, Fletcher J. Clinical practice guidelines for the psychosocial care of adults with cancer. Psycho-Oncology. 2005;14:159–73. doi: 10.1002/pon.897.
Carlson LE, Angen M, Cullum J, Goodey E, Koopmans J, Lamont L, et al. High levels of untreated distress and fatigue in cancer patients. Br J Cancer. 2004;90:2297–304.
Zabora J, Brintzenhofeszoc K, Curbow B, Hooker C, Piantadosi S. The prevalence of psychological distress by cancer site. Psycho-Oncology. 2001;10:19–28.
Boyes AW, Girgis A, Zucca AC, Lecathelinais C. Anxiety and depression among long-term survivors of cancer in Australia: results of a population-based survey. Med J Aust. 2009;190:s94–8.
Bultz BD, Carlson LE. Emotional distress: the sixth vital sign in cancer care. J Clin Oncol. 2005;23:6440–1.
Cancer Australia, Cancer Council Australia. Review of national cancer control activity in Australia. Canberra: Cancer Australia; 2010.
Fann JR, Thomas-Rich AM, Katon WJ, Cowley D, Pepping M, McGregor BA, et al. Major depression after breast cancer: a review of epidemiology and treatment. Gen Hosp Psychiatry. 2008;30:112–26.
Hack TF, Degner LF. Coping responses following breast cancer diagnosis predict psychological adjustment three years later. Psycho-Oncology. 2004;13:235–47.
Beatty L, Koczwara B. An effectiveness study of a CBT group program for women with breast cancer. Clin Psychol. 2010;14:45–53.
Classen C, Kraemer HC, Blasey C, Giese-Davis J, Koopman C, Palesh OG, et al. Supportive-expressive group therapy for primary breast cancer patients: a randomized prospective multicenter trial. Psycho-Oncology. 2008;17:438–47.
Zimmermann T, Heinrichs N, Baucom DH. “Does One Size Fit All?” Moderators in psychosocial interventions for breast cancer patients: A meta-analysis. Ann Behav Med. 2007;34:225–39.
Foley E, Baillie A, Huxter M, Price M, Sinclair E. Mindfulness-based cognitive therapy for individuals whose lives have been affected by cancer: a randomised controlled trial. J Consult Clin Psychol. 2010;78:72–9.
Helgeson VS, Cohen S, Schulz R, Yasko J. Education and peer discussion group interventions and adjustment to breast cancer. Arch Gen Psychiatry. 1999;56:340–7.
Osborn RL, Demoncada AC, Feuerstein M. Psychosocial interventions for depression, anxiety, and quality of life in cancer survivors: Meta-analyses. Int J Psychiatry Med. 2006;36:13–34.
Wade TD, Nehmy T, Koczwara B. Predicting worries about health after breast cancer surgery. Psycho-Oncology. 2005;14:503–9.
Christensen H. Increasing access and effectiveness: using the internet to deliver low intensity CBT. In: Bennett-Levy J, Richards DA, Farrand P, Christensen H, Griffiths KM, Kavanagh DJ, Klein B, Lau MA, Proudfood J, Ritterband LM, editors. Oxford guide to low intensity CBT interventions. New York: Oxford University Press; 2010. p. 53–68.
Beatty L, Lambert S. A systematic review of internet-based self-help therapeutic interventions to improve distress and disease-control among adults with chronic health conditions. Clin Psychol Rev. 2013;33:609–22.
Cuijpers P, van Straten A, Andersson G. Internet-administered cognitive behavior therapy for health problems: a systematic review. J Behav Med. 2008;31:169–77.
Griffiths KM, Farrer L, Christensen H. The efficacy of internet interventions for depression and anxiety disorders: a review of randomised controlled trials. Med J Aust. 2010;192:S4–11.
Newman MG, Szkodny LE, Llera SJ, Przeworski A. A review of technology-assisted self-help and minimal contact therapies for anxiety and depression: Is human contact necessary for therapeutic efficacy? Clin Psychol Rev. 2011;31:89–103.
Barak A, Klein B, Proudfoot J. Defining internet-supported therapeutic interventions. Ann Behav Med. 2009;38:4–17.
Nathan PE, Gorman JM. A guide to treatments that work. 3rd ed. New York: Oxford University Press; 2007.
Bader J, Strickman-Stein N. Evaluation of new multimedia formats for cancer communication. J Med Internet Res. 2003;5:e16.
Australian Bureau of Statistics. Household use of information technology, (Cat No. 8146.0). Canberra: ABS; 2006.
Beatty L, Koczwara B, Wade T. ‘Cancer Coping Online’: a pilot trial of a self-guided CBT internet intervention for cancer-related distress. Electronic J Applied Psychol. 2011;7:17–25.
Carpenter KM, Stoner SA, Schmitz K, McGregor BA, Doorenbos AZ. An online stress management workbook for breast cancer. J Behav Med. 2014;37:458–68.
Duffecy J, Sanford S, Wagner L, Begale M, Nawacki E, Mohr DC. Project onward: an innovative e-health intervention for cancer survivors. Psycho Oncolo. 2013;22:947–51.
Owen JE, Klapow JC, Roth DL, Shuster Jr JL, Bellis J, Meredith R, et al. Randomized pilot of a self-guided internet coping group for women with early-stage breast cancer. Ann Behav Med. 2005;30:54–64.
Beatty L, Koczwara B, Rice J, Wade T. A randomised controlled trial to evaluate the effects of a self-help workbook intervention on distress, coping and QOL after breast cancer diagnosis. Med J Aust. 2010;193:S68–73.
Kraemer HC, Wilson GT, Fairburn CG, Agras WS. Mediators and moderators of treatment effects in randomized clinical trials. Arch Gen Psychiatry. 2002;59:877–83.
Stanton AL, Danoff-Burg S, Cameron CL, Bishop M, Collins CA, Kirk SB, et al. Emotionally expressive coping predicts psychological and physical adjustment to breast cancer. J Consult Clin Psychol. 2000;68:875–82.
Schulz K, Altman D, Moher D, for the CONSORT Group: CONSORT. Statement: updated guidelines for reporting parallel group randomised trials. BMJ. 2010;2010(340):698–702.
Lovibond SH, Lovibond PH. Manual for the Depression Anxiety Stress Scales (DASS). Sydney: University of New South Wales; 1995.
Foa EB, Riggs DS, Dancu CV, Rothbaum BO. Reliability and validity of a brief instrument for assessing posttraumatic stress disorder. J Trauma Stress. 1993;6:459–73.
Klee M, Groenvold M, Machin D. Quality of life of Danish women: population-based norms for the EORTC QLQ-C30. Qual Life Res. 1997;6:27–34.
Watson M, Law M, dos Santos M, Greer S, Baruch J, Bliss J. The Mini-MAC: further development of the mental adjustment to cancer scale. J Psychosoc Oncol. 1994;12:33–46.
Australian Bureau of Statistics. 1989–1990 National health survey users’ guide, (Cat No. 4363.0). Canberra: ABS; 1991.
Sherbourne CD, Stewart AL. The MOS social support survey. Soc Sci Med. 1991;32:705–14.
Miller SM. Monitoring and blunting: validation of a questionnaire to assess styles of information seeking under threat. J Pers Soc Psychol. 1987;52:345–53.
Gratz K, Roemer L. Multidimensional assessment of emotion regulation and dysregulation: development, factor structure, and inital validation of the difficulties in emotion regulation scale. J Psychopathol Behav Assess. 2004;26:41–54.
Thiels C, Schmidt U, Troop N, Treasure J, Garthe R. Compliance with a self-care manual in guided self-change for bulimia nervosa. Eur Eat Disord Rev. 2001;9:115–22.
Hedeker D, Gibbons RD, Waternaux C. Sample size estimation for longitudinal studies with attrition:comparing time related contrasts between two groups. J Educ Behav Stat. 1999;24:70–93.
Kaldo V, Levin S, Widarsson J, Buhrman M, Larsen H-C, Andersson G. Internet versus group cognitive-behavioral treatment of distress associated with tinnitus: a randomized controlled trial. Behav Ther. 2008;39:348–59.
Acknowledgements
This study was funded by a National Health and Medical Research Council project grant (NHMRC grant #1042942).
The authors would like to acknowledge the valuable contributions of the following Finding My Way Investigators; Associate Professor Jane Turner (University of Queensland), Professor Patsy Yates (Queensland University of Technology), Professor Phyllis Butow (University of Sydney), Dr Sylvie Lambert (McGill University), Dr Addie Wootten (Royal Melbourne Hospital), Dr Donna Milne (Peter MacCallum Cancer Centre), Dr Vikki Knott (Menzies University), Mr Paul Katris (Western Australian Clinical Oncology Group), Ms Sue De Bono (Alfred Health), Associate Professor Desmond Yip (Australian National University/The Canberra Hospital), Dr Sarah McKinnon (Ballarat Health Services), Ms Simone Noelker (Ballarat Health Services), Ms Bernadette Zappa (Eastern Health), Ms Judy Allen (Eastern Health).
Many thanks to all of the medical staff who are assisting with recruitment.
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
LB design of study protocol, review of manuscript. EK drafting of manuscript. BK design of study protocol, review of manuscript. TW design of study protocol, review of manuscript. All authors read and approved the final manuscript.
Authors’ information
Dr Lisa Beatty is a research fellow at Flinders University, South Australia, and a clinical psychologist at the Flinders Centre for Innovation in Cancer, Flinders Medical Centre, South Australia
Dr Emma Kemp is a research associate at Flinders University, currently based at the Flinders Centre for Innovation in Cancer, Flinders Medical Centre, South Australia
Professor Tracey Wade is the Dean, School of Psychology at Flinders University, South Australia
Professor Bogda Koczwara is a medical oncologist at the Flinders Centre for Innovation in Cancer, Flinders Medical Centre, South Australia
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Beatty, L., Kemp, E., Wade, T. et al. Finding My Way: protocol of a randomised controlled trial evaluating an internet self-help program for cancer-related distress. BMC Cancer 15, 328 (2015). https://doi.org/10.1186/s12885-015-1322-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-015-1322-x