Abstract
Background
Factors associated with low birth weight at term (TLBW), a proxy for intrauterine growth restriction (IUGR), are not well-elucidated in socioeconomically vulnerable populations. This study aimed to identify the factors associated with TLBW in impoverished Brazilian women.
Methods
Records in the 100 Million Brazilian Cohort database were linked to those in the National System of Information on Live Births (SINASC) to obtain obstetric, maternal, birth and socioeconomic data between 2001 and 2015. Multivariate logistic regression was performed to investigate associations between variables of exposure and TLBW.
Results
Of 8,768,930 term live births analyzed, 3.7% presented TLBW. The highest odds of TLBW were associated with female newborns (OR: 1.49; 95% CI: 1.47–1.50), whose mothers were black (OR: 1.20; 95% CI: 1.18–1.22), had a low educational level (OR: 1.57; 95% CI: 1.53–1.62), were aged ≥35 years (OR: 1.44; 95% CI: 1.43–1.46), had a low number of prenatal care visits (OR: 2.48; 95% CI: 2.42–2.54) and were primiparous (OR: 1.62; 95% CI: 1.60–1.64). Lower odds of TLBW were found among infants whose mothers lived in the North, Northeast and Center-West regions of Brazil compared to those in the South.
Conclusion
Multiple aspects were associated with TLBW, highlighting the need to comprehensively examine the mechanisms underlying these factors, especially in more vulnerable Brazilian populations, in order to contribute to the elaboration of health policies and promote better conditions of life for poor and extremely poor mothers and children.
Similar content being viewed by others
Background
Birth weight is strongly associated with infant morbidity and mortality, and is considered a predictor of immediate and future health status in newborns [1,2,3,4]. In 2015, 14.6% of all children (~ 20.5 million) were born with low birth weight (LBW); 91% of these births occurred in low- and middle-income countries [5]. In Brazil, the prevalence of LBW was estimated at 8.5% in 2017 [6], a rate very similar to that found in Latin America and the Caribbean (8.7%), which has not reduced significantly in the last 15 years [5].
Low birth weight, defined as less than 2500 g, may be a consequence of prematurity or associated with intrauterine growth restriction (IUGR), or a combination thereof [7]; The proportion of LBW related to restricted fetal growth and/or prematurity varies in accordance with the degree of economic development among countries [8]. In South Asia, among neonates with LBW, approximately 65% born at term were small for gestational age (a proxy for fetal growth restriction), while just over 50% presented LBW in Latin America and the Caribbean [8].
Evidence suggests that low birth weight at term (TLBW) (a proxy for IUGR) is associated with: i. maternal characteristics, such as age, and obstetrics history [9,10,11,12,13,14,15]; ii. newborn characteristics [10, 12]; iii. prenatal care [10, 11, 14]; iv. socioeconomic aspects [10, 12,13,14, 16,17,18]. Studies in low- and middle-income countries indicate that socioeconomic factors, including education, income, an urban/rural living environment, region of residence and domiciliary conditions, as well as access to prenatal care, are also important determinants of pregnancy and birth weight outcomes [4, 10,11,12,13,14, 16,17,18,19,20,21,22,23].
Although several studies have examined the determinants of TLBW, factors associated with TLBW remain unelucidated among socioeconomically vulnerable populations living in low- and middle- income countries, such as Brazil. To further investigate factors associated with TLBW, this study considered data between 2001 and 2015 from the 100 Million Brazilian Cohort linked to the National Live Birth System (SINASC). The 100 M Brazilian cohort contains information on low-income families with monthly per-capita income less than BRL200 (US$50), representing approximately 55% of the total Brazilian population [24]. Thus, the linkage of these two datasets enabled us to investigate the factors associated with TLBW in the Brazilian population living in poverty and extreme poverty, with the hope of contributing to the development of intervention strategies aimed at minimizing LBW.
Methods
Study design and population
This study employed data from the 100 Million Brazilian Cohort, a database constructed by the Center for Data and Knowledge Integration for Health (Centro de Integração de Dados e Conhecimentos para Saúde-CIDACS), affiliated with the Oswaldo Cruz Foundation (FIOCRUZ) [24]. This is a retrospective and dynamic cohort. The cohort database contains records of 114,001,661 low-income individuals (40,542,929 families) eligible for social assistance programs via the Unified Registry for Social Programs (CadÚnico), who were registered between between 2001 and 2015. Socioeconomic data from the 100 Million Brazilian Cohort were linked to data contained in the National System of Information on Live Births (SINASC), considering the period of Jan 1, 2001 to Dec 31, 2015.
Cohort data were linked to the live birth registry from SINASC according to similarity using the CIDACS Record Linkage algorithm [25]. This novel record linkage tool considers the following attributes in its matching process: mother’s name or newborn’s name, mother’s municipality of residence at time of registry/delivery, newborn date of birth and/or mother’s age. In the current linkage process, the number of linked records was 24,695,618 (55.51%) and the estimated accuracy was over 90%/year.
The study population included live births of women aged 14–49 years who were registered in the 100 Million Brazilian Cohort between 2001 and 2015 (Fig. 1). We included only the most recent live birth reported for each woman, and excluded preterm (< 37 gestational weeks) and post-term births (42 gestational weeks or more). Multiple births and newborns with congenital anomalies were excluded in an effort to avoid bias, as these conditions are known to be strongly associated with low birth weight [13, 16, 26, 27].
Variables
Descriptions for the variables of interest are detailed in Table 1. The dependent variable was low birth weight, defined as less than 2500 g, in term births (37–41 completed weeks) [28]. The following covariates were considered: i. socioeconomic characteristics (marital status, self-reported race/ethnicity, maternal schooling, household conditions, urban/rural living environment and geographic region of residence); ii. prenatal assistance (number of visits); iii. maternal- and newborn-related variables (maternal age at birth, newborn sex and birth order).
Statistical analysis
Maternal and live birth characteristics were summarized using frequency distributions. We also calculated the percentage of TLBW among all those born with LBW (6.7%), prior to excluding preterm and post-term births. Multivariate logistic regression was conducted to investigate the factors associated with TLBW. A conceptual hierarchy-based approach (Fig. 2) was employed to introduce, in subsequent adjusted models, the variables contained in the datasets, considering covariates deemed relevant and plausible in the literature [7, 9,10,11,12,13,14,15,16,17,18]. The TLBW variables were grouped into three blocks representing distal, intermediate and proximal determinants, i.e. socioeconomic characteristics, use of the health services (prenatal care, defined by number of visits) and maternal and newborn characteristics, respectively [7, 29,30,31].
The initial model was adjusted for the distal factors. In the second model, all variables contained in the previous model were maintained, with the inclusion of the number of prenatal visits (intermediate factor). The final model included, in addition to the variables contained in the two previous models, the mother’s age at the time of delivery, birth order/parity and sex of the newborn. Odds ratio (OR) values and respective confidence intervals (95% CI) were calculated for each variable maintained in the final model. Data analysis was performed using Stata version 15.1 (Stata Corporation, 153 College Station, USA).
Advantages of large samples
Large sample sizes provide ample data to conduct analyses on subgroups of interest while maintaining sufficient power to gain insights into the direction and size of the effects. Due to changes in the SINASC registry with respect to gestational age, it was necessary to conduct additional analyses to verify the results of our multivariate regression analysis. From 2001 to 2010, gestational age was recorded as a categorical variable (gestational age in completed weeks: <22w; 22-27w; 28-31w; 32-36w; 37-41w; ≥42w). Beginning in 2011, gestational weeks at birth was recorded as a discrete variable (gestational age in number of completed weeks), estimated from the date of the mother’s last menstrual period, physical examination or image results obtained from SINASC records. Due to dynamic aspects of this cohort, such as the differences in the entry time of each woman in the study, as well as changes in 2011 in terms of how information on gestational age was collected/recorded by SINASC, additional analyses were carried out (shown in Suplemmentary material) for verification purposes. These additional multivariate logistic regression models were employed in accordance with the same variable selection method used in the main analysis, yet were stratified according to year of birth before and after 2011 and incorporated “time of exposure” quartiles prior to birth, considering the time difference (in years) between the mother’s inclusion in the cohort a newborn’s date of birth.
Results
Among the 8,768,930 term live births investigated, 3.7% were found to be TLBW. Table 2 lists the characteristics of newborns with TLBW. The percentage of TLBW ranged slightly among different regions of Brazil, with a higher prevalence noted in the Southeast (4.0%) and South (3.8%) and similar prevalence among the Center-West, North and Northeast regions (3.5%). Regarding distal socioeconomic maternal characteristics, 53.9% of the mothers were unmarried (single, widowed or divorced), 59.4% had more than 8 years of schooling, 59.2% self-reported mixed-race (“parda”), 39.6% were born in the Northeast and 73.8% lived in urban areas.
With regard to newborn/maternal characteristics, 69.3% of newborns’ mothers were aged 20–35 years, 32.0% had primiparous mothers, 58.8% had multiparous mothers (2–4 previous live births) and 49.0% were female.
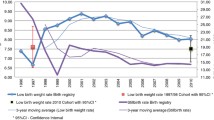
Figure 3 illustrates the results of our multivariate analysis. In the adjusted model, the odds of TLBW were higher among infants born to women who: self-declared skin color as black (OR: 1.20; 95% CI: 1.18–1.22), were unmarried (OR: 1.08; 95% CI: 1.07–1.09), had a low level of schooling (OR: 1.57; 95% CI: 1.53–1.62), had no prenatal visits (OR: 2.48; 95% CI: 2.42–2.54), were aged between 35 and 49 years (OR: 1.44; 95% CI: 1.43–1.46), gave birth for the first time (OR: 1.62; 95% CI: 1.60–1.64) and were female (OR: 1.49; 95% CI: 1.47–1.50). Dose-response associations were observed for the variables of schooling and number of prenatal visits. Lower odds of TLBW were observed among infants born to mothers living in the North (OR: 0.78; 95% CI: 0.76–0.79) and Northeast (OR: 0.78; 95% CI: 0.77–0.80) regions of Brazil. OR values approximating one were estimated for inadequate domiciliary conditions (OR: 1.02; 95% CI: 1.00–1.03) and a rural area of residence (OR: 0.93; 95% CI: 0.92–0.94). Our analysis of six models containing variables related to TLBW (supplementary material) confirmed the findings described above. The variables with stronger associations (self-reported race/ethnicity, level of schooling, age, number of prenatal visits, newborn sex and birth order) remained associated with TLBW in all supplementary models (Supplementary Tables 1 and 2).
Discussion
The present study evaluated factors associated with TLBW in Brazilian populations living in poverty or extreme poverty. The occurrence of TLBW found herein was similar to that estimated in the overall Brazilian population born in 2017 (3.7%) [6]. Of all newborns with LBW, our results indicated that 55.2% were born at term, which is higher than in the overall population (38%) [6], illustrating the importance of TLBW with respect to the total burden posed by low birth weight in poorer populations. The occurrence of TLBW in our study approximated that reported in China (2.0%) [13] and rural China (4.8%) [32], yet was different from rates reported in Northern Ethiopia (10%) [9], at an Ethiopian hospital (12.0%) [33], at a Pakistani hospital (10.6%) [34] and in rural Central India (33.1%) [35]. Herein, lower rates of TLBW were observed among newborns whose mothers lived in the North and Northeast regions of Brazil. Moreover, our findings indicate that TLBW was associated with infants born to mothers with lower educational levels, who were black, unmarried, received an insufficient number of prenatal visits, were aged between 35 and 49 years, and whose newborns who were their first child and/or were female.
Previous studies in Brazil [36,37,38,39] have demonstrated that the country’s more developed regions, the South and Southeast, presented the highest percentages of children born with LBW. In contrast, a lower occurrence of LBW was found in the North and Northeast, which are considered economically less-developed regions; women in these areas also have lower levels of education, with notably less frequent or no prenatal consultations [36]. With respect to TLBW, these differences remain, yet are more subtle, as our results corroborate the higher frequency seen in the Southeast, being less common in the Northeast and Central-West regions [36].
It is worth noting that a demographic transition is well underway in Brazil, as evidenced by increasing fertility trends in women over 35 years of age, mainly in highly urbanized areas. This combined with the late onset of reproductive activity has led to an increase in the proportion of primiparous women in this age group [40]. In addition to delayed pregnancy, these results may also be explained by a lack of rigor in accurately recording live births at regional centers, as well as the precarious availability of health services and lack of early medical intervention [38].
Many studies have compared the occurrence of LBW among regions in Brazil, which hinders the ability to make comparisons regarding TLBW. A plausible explanation for discrepancies regarding rates of TLBW may be that, as some authors have observed, in locations with poor childbirth care resources and access to perinatal technology, newborns who die shortly after birth are commonly misclassified as “stillborn” or are not even registered [38, 39], which contributes to lower rates of LBW recorded in these areas, and may be a factor influencing the lower occurrence of LBW in northern and northeastern Brazil. Although not evaluated herein, another possibility might be higher maternal rates of smoking, which is a known cause of LBW [41, 42].
Our analysis indicated that TLBW is inversely associated with the level of maternal schooling, i.e. fewer years of formal study leads to a greater chance giving birth to a neonate with TLBW (Fig. 3). These findings corroborate those of many other studies investigating the factors associated with TLBW, highlighting the importance of socioeconomic conditions, especially with regard to mothers or their family’s educational level [10, 13, 14, 17, 18]. A mother’s level of schooling affects her use of health care services, as women with higher socioeconomic status often attend more prenatal visits, have better knowledge regarding nutrition [43] and generally understand and observe health professionals’ recommendations during pregnancy [44].
The findings of the present study also indicate that black women have a higher chance of giving birth to newborns with TLBW. How race translates into the social and economic environment and affects birth outcomes remains poorly understood [45]. While a previous study reported a higher occurrence of LBW in black women, this was only seen in individuals with low levels of education [3]. Another study found greater risk of LBW in Brazilian women of African descent (i.e. a grandparent, great grandparent, or great-great-grandparent born in Africa) [46]. We were unable to identify any studies reporting on racial disparities and TLBW in Brazil.
Marital status was found to be weakly associated with TLBW. It is possible that bias occurred in the recording of this variable, resulting in the overreporting of single women, since previous versions of the SINASC form used for registering live births did not include “stable union” as an option, rather specifying consensual union, which denotes a legal recognition of status [47]. However, this weak association did remain in our verification analysis (shown in Suplemmentary material) that compared study periods before and after 2011, the year in which changes were made to the live birth registry form, which further supports the observed association.
The estimated OR for TLBW was found to increase with reduced numbers of prenatal visits, indicating the importance of prenatal care. The provision of fewer prenatal health services, characterized by lower numbers of visits, has been associated with negative perinatal outcomes, such as TLBW [10, 11, 14]. The prevention of LBW is also conditional on compliance with nutritional guidance and lifestyle recommendations during pregnancy [43, 44], including the use of multivitamin supplements containing calcium, iron and folic acid, all micronutrients essential to proper fetal growth [29], in addition to the prevention of risk behaviors, e.g. use of tobacco, alcohol and other drugs [1, 45, 48,49,50,51,52].
Older women (between 35 and 49 years) are more likely to give birth to newborns with TLBW. Advanced maternal age, commonly defined as ≥35 years, is considered a risk factor for adverse health outcomes in children, including LBW and TLBW [9, 12,13,14, 18, 22, 23, 53,54,55], increased risk of comorbidities (hypothyroidism, type 2 diabetes, hypertension), obstetric complications (preeclampsia/eclampsia and emergency cesarean section) and the prior occurrence of obstetric complications in past pregnancies (history of spontaneous abortion and caesarean delivery) [56, 57]. Advanced maternal age has been particularly linked to LBW among primiparous women [57]. While extremes in maternal parity (primiparity and grand multiparity) are considered to present high risk of LBW and TLBW [14, 55], our results showed that only the first maternal pregnancy was associated with TLBW, which corroborates other findings in the literature [13, 18, 34]. As noted herein, some studies have reported increased risk for TLBW in female newborns [12, 18, 35], since male infants tend to have higher birth weights and face a lower risk of IUGR [7].
Study strengths and limitations
The study has some important strengths. First, the large-scale dataset allowed us to comprehensively investigate known factors associated with TLBW. Second, the SINASC registry has high national coverage (over 90%), which provided a truly representative study population [58]. Moreover, the high reliability of the information contained in the SINASC database reinforces the suitability of using this system for epidemiological investigations [58]. With regard to limitations, the use of secondary data subjects the collected information to bias. This further implies that since data collection procedures were not performed as a function of the present study’s objectives, some important variables relevant to the determination of TLBW were not collected, such as maternal smoking habits, weight gain during pregnancy, the mother’s nutritional status and other maternal comorbidities. It is important to highlight that larger samples provide great opportunities for empirical research, but also may lead to equivocal interpretations due to the detection of statistical significance [59, 60].
This population-based study was focused on investigating live births to poor and extremely poor women. With due caution, some of the findings reported herein may be generalized to other populations with similar characteristics. Importantly, these limitations do not greatly detract from the promising potential enabled through research conducted on the “100 Million Brazilian Cohort”.
Conclusion
This population-based study reveals important information regarding the frequencies and associated factors relative to TLBW in poor and extremely poor Brazilian women. Inequity in TLBW has persisted in economically vulnerable populations, especially in live births to mothers with lower educational levels who are black and receive insufficient prenatal care. The identification of factors associated with TLBW is essential to contribute to more inclusive health policies and promote improved welfare for poor and extremely poor mothers and children. Our study highlights the need to assess the underlying mechanisms behind these factors and expand on the analysis through the further exploration of the variables considered herein. We observed that a very high percentage of women receive an insufficient number of prenatal consultations, despite living in a country with a nationalized public health system. In sum, it will be important not only to implement social policies designed to protect pregnant women is economically vulnerable situations, such as through conditional cash transfer programs, but also to provide greater coverage of prenatal care as well as educational support regarding health and nutrition, in addition to paying special attention to the occurrence of comorbidities, especially among older women.
Availability of data and materials
All data supporting the findings presented herein were obtained from Centro de Integração de Dados e Conhecimentos para Saúde (CIDACS). Importantly, restrictions apply to the availability of these data, which were licensed for exclusive use in the current study, and are thus not publicly available. Upon reasonable request and with the express permission of CIDACS, the authors are willing to make every effort to grant data availability.
Abbreviations
- TLBW:
-
Low birth weight at term
- LBW:
-
Low birth weight
- IUGR:
-
Intrauterine growth restriction
- SINASC:
-
National Live Birth System
- OR:
-
Odds ratio
- 95%CI:
-
95% confidence interval
References
Dubois L, Girard M. Determinants of birthweight inequalities: population-based study. Pediatr Int. 2006;48(5):470–8.
Goldenberg RL, Culhane JF. Low birth weight in the United States. Am J Clin Nutr. 2007;85(2):584s–90s.
Leal MC, Gama SGN, Cunha CB. Desigualdades sociodemográficas e suas conseqüências sobre o peso do recém-nascido. Rev Saude Publica. 2006;40:466–73.
Mahumud RA, Sultana M, Sarker AR. Distribution and determinants of low birth weight in developing countries. J Prev Med Public Health. 2017;50(1):18–28.
Blencowe H, Krasevec J, de Onis M, Black RE, An X, Stevens GA, Borghi E, Hayashi C, Estevez D, Cegolon L, et al. National, regional, and worldwide estimates of low birthweight in 2015, with trends from 2000: a systematic analysis. Lancet Glob Health. 2019;7(7):e849–60.
Ministério da Saúde do Brasil. Nascimentos por residência da mãe e por região. 2017. Retrieved from http://tabnet.datasus.gov.br/cgi/deftohtm.exe?sinasc/cnv/nvuf.def.
Kramer MS. Determinants of low birth weight: methodological assessment and meta-analysis. Bull World Health Organ. 1987;65(5):663–737.
Lee ACC, Katz J, Blencowe H, Cousens S, Kozuki N, Vogel JP, Adair L, Baqui AH, Bhutta ZA, Caulfield LE, et al. National and regional estimates of term and preterm babies born small for gestational age in 138 low-income and middle-income countries in 2010. Lancet Glob Health. 2013;1(1):e26–36.
Gebregzabiherher Y, Haftu A, Weldemariam S, Gebrehiwet H. The prevalence and risk factors for low birth weight among term newborns in Adwa General Hospital, Northern Ethiopia. Obstet Gynecol Int. 2017;2017:2149156. https://doi.org/10.1155/2017/2149156.
Kader M, Perera NK. Socio-economic and nutritional determinants of low birth weight in India. N Am J Med Sci. 2014;6(7):302–8.
Mumbare SS, Maindarkar G, Darade R, Yenge S, Tolani MK, Patole K. Maternal risk factors associated with term low birth weight neonates: a matched-pair case control study. Indian Pediatr. 2012;49(1):25–8.
Agorinya IA, Kanmiki EW, Nonterah EA, Tediosi F, Akazili J, Welaga P, Azongo D, Oduro AR. Socio-demographic determinants of low birth weight: evidence from the Kassena-Nankana districts of the upper east region of Ghana. PLoS One. 2018;13(11):1–10.
Chen Y, Li G, Ruan Y, Zou L, Wang X, Zhang W. An epidemiological survey on low birth weight infants in China and analysis of outcomes of full-term low birth weight infants. BMC Pregnancy Childbirth. 2013;13:242.
Minuci EG, Almeida MF. Birth weight intra-urban differentials in the city of São Paulo. Rev Saude Publica. 2009;43(2):256–66.
Abubakari A, Kynast-Wolf G, Jahn A. Maternal determinants of birth weight in northern Ghana. PLoS One. 2015;10(8):e0135641.
Li CY, Sung FC. Socio-economic inequalities in low-birth weight, full-term babies from singleton pregnancies in Taiwan. Public Health. 2008;122(3):243–50.
Taywade ML, Pisudde PM. Study of sociodemographic determinants of low birth weight in Wardha district, India. Clin Epidemiol Glob Health. 2017;5(1):14–20.
Mohammad K, Kassab M, Gamble J, Creedy DK, Foster J. Factors associated with birth weight inequalities in Jordan. Int Nurs Rev. 2014;61(3):435–40.
Manyeh AK, Kukula V, Odonkor G, Ekey RA, Adjei A, Narh-Bana S, Akpakli DE, Gyapong M. Socioeconomic and demographic determinants of birth weight in southern rural Ghana: evidence from Dodowa Health and Demographic Surveillance System. BMC Pregnancy Childbirth. 2016;16(1):160.
Dahlui M, Azahar N, Oche OM, Aziz NA. Risk factors for low birth weight in Nigeria: evidence from the 2013 Nigeria Demographic and Health Survey. Glob Health Action. 2016;9:28822.
Bharati P, Pal M, Bandyopadhyay M, Bhakta A, Chakraborty S, Bharati P. Prevalence and causes of low birth weight in India. Malays J Nutr. 2011;17(3):301–13.
Momeni M, Danaei M, Kermani AJN, Bakhshandeh M, Foroodnia S, Mahmoudabadi Z, Amirzadeh R, Safizadeh H. Prevalence and risk factors of low birth weight in the southeast of Iran. Int J Prev Med. 2017;8:12.
Khatun S, Rahman M. Socio-economic determinants of low birth weight in Bangladesh: a multivariate approach. Bangladesh Med Res Counc Bull. 2008;34(3):81–6.
Centro de Integração de Dados e Conhecimentos para a Saúde. Cohort of 100 million Brazilians. 2018. Retrieved from https://cidacs.bahia.fiocruz.br/en/platform/cohort-of-100-million-brazilians/.
Ali MS, Ichihara MY, Lopes LC, Barbosa GCG, Pita R, Carreiro RP, Dos Santos DB, Ramos D, Bispo N, Raynal F, et al. Administrative data linkage in Brazil: potentials for health technology assessment. Front Pharmacol. 2019;10:984.
Wehby GL, Murray JC, Castilla EE, Lopez-Camelo JS, Ohsfeldt RL. Prenatal care effectiveness and utilization in Brazil. Health Policy Plan. 2009;24(3):175–88.
Woodhouse C, Lopez Camelo J, Wehby GL. A comparative analysis of prenatal care and fetal growth in eight south American countries. PLoS One. 2014;9(3):e91292.
World Health Organization. Certain conditions originating in the perinatal period. In: International statistical classification of diseases and related health problems for mortality and morbidity statistics. 11th ed: World Health Organization; 2019.
Black RE, Victora CG, Walker SP, Bhutta ZA, Christian P, de Onis M, Ezzati M, Grantham-McGregor S, Katz J, Martorell R, et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet. 2013;382(9890):427–51.
Belfort GP, Santos MMAS, Pessoa LS, Dias JR, Heidelmann SP, Saunders C. Determinantes do baixo peso ao nascer em filhos de adolescentes: uma análise hierarquizada. Cien Saude Colet. 2018;23:2609–20.
Ribeiro AM, Guimarães MJ, Lima Mde C, Sarinho SW, Coutinho SB. Risk factors for neonatal mortality among children with low birth weight. Rev Saude Publica. 2009;43(2):246–55.
Chen S, Yang Y, Qu Y, Zou Y, Zhu H, Yang H, Gong F, Wang L, Jiang Y, Lian BQ, et al. Both maternal and paternal risk factors for term singleton low birthweight infants in rural Chinese population: a population-based, retrospective cohort study. Sci Rep. 2018;8(1):12539.
Mekie M, Taklual W. Magnitude of low birth weight and maternal risk factors among women who delivered in Debre Tabor Hospital, Amhara Region, Ethiopia: a facility based cross-sectional study. Ital J Pediatr. 2019;45(1):86.
Khan A, Nasrullah FD, Jaleel R. Frequency and risk factors of low birth weight in term pregnancy. Pak J Med Sci. 2016;32(1):138–42. https://doi.org/10.12669/pjms.321.8120.
Kumar V, Deshmukh PR, Taywade M, Gupta SS. Magnitude and correlates of low birth weight at term in rural Wardha, Central India. Online J Health Allied Sci. 2016;15(1):1–5.
Andrade CLT, Szwarcwald CL, Castilho EA. Baixo peso ao nascer no Brasil de acordo com as informações sobre nascidos vivos do Ministério da Saúde, 2005. Cad Saúde Pública. 2008;24:2564–72.
Lima MCBM, Oliveira GS, Lyra CO, Roncalli AG, Ferreira MAF. A desigualdade espacial do Baixo Peso ao Nascer no Brasil. Cien Saude Colet. 2013;18:2443–52.
Silva AAM, Silva LM, Barbieri MA, Bettiol H, Carvalho LM, Ribeiro VS, Goldani MZ. The epidemiologic paradox of low birth weight in Brazil. Rev Saude Publica. 2010;44(5):767–75.
Silva AA, Bettiol H, Barbieri MA, Pereira MM, Brito LG, Ribeiro VS, Aragão VM. Why are the low birthweight rates in Brazil higher in richer than in poorer municipalities? Exploring the epidemiological paradox of low birthweight. Paediatr Perinat Epidemiol. 2005;19(1):43–9.
Alencar GP, da Silva ZP, Santos PC, Raspantini PR, Moura BLA, de Almeida MF, do Nascimento FP, Rodrigues LC. What is the impact of interventions that prevent fetal mortality on the increase of preterm live births in the State of Sao Paulo, Brazil? BMC Pregnancy Childbirth. 2015;15(1):152.
Johnson CD, Jones S, Paranjothy S. Reducing low birth weight: prioritizing action to address modifiable risk factors. J Public Health (Oxf). 2017;39(1):122–31.
Wilcox AJ. On the importance--and the unimportance--of birthweight. Int J Epidemiol. 2001;30(6):1233–41.
Dolatian M, Mahmoodi Z, Alavi-Majd H, Moafi F, Ghorbani M, Mirabzadeh A. Psychosocial factors in pregnancy and birthweight: path analysis. J Obstet Gynaecol Res. 2016;42(7):822–30.
Astone NM, Misra D, Lynch C. The effect of maternal socio-economic status throughout the lifespan on infant birthweight. Paediatr Perinat Epidemiol. 2007;21(4):310–8.
Grady SC. Racial disparities in low birthweight and the contribution of residential segregation: a multilevel analysis. Soc Sci Med (1982). 2006;63(12):3013–29.
Wehby GL, Gili JA, Pawluk M, Castilla EE, López-Camelo JS. Disparities in birth weight and gestational age by ethnic ancestry in south American countries. Int J Public Health. 2015;60(3):343–51.
Gabriel GP, Chiquetto L, Morcillo AM, Carmo Ferreira M, Bazan IGM, Daolio LD, Rocha Lemos JJ, Faria Carniel E. Avaliação das informações das Declarações de Nascidos Vivos do Sistema de Informação sobre Nascidos Vivos (Sinasc) em Campinas, São Paulo, 2009. Rev Paul Pediatr. 2014;32(3):183–8.
Brown SJ, Yelland JS, Sutherland GA, Baghurst PA, Robinson JS. Stressful life events, social health issues and low birthweight in an Australian population-based birth cohort: challenges and opportunities in antenatal care. BMC Public Health. 2011;11(1):196.
Farley TA, Mason K, Rice J, Habel JD, Scribner R, Cohen DA. The relationship between the neighbourhood environment and adverse birth outcomes. Paediatr Perinat Epidemiol. 2006;20(3):188–200.
Jansen PW, Tiemeier H, Looman CWN, Jaddoe VWV, Hofman A, Moll HA, Steegers EAP, Verhulst FC, Mackenbach JP, Raat H. Explaining educational inequalities in birthweight: the generation R study. Paediatr Perinat Epidemiol. 2009;23(3):216–28.
Kuo C-P, Lee S-H, Wu W-Y, Liao W-C, Lin S-J, Lee M-C. Birth outcomes and risk factors in adolescent pregnancies: results of a Taiwanese national survey. Pediatr Int. 2010;52(3):447–52.
Balazs P, Rakoczi I, Grenczer A, Foley KL. Risk factors of preterm birth and low birth weight babies among Roma and non-Roma mothers: a population-based study. Eur J Pub Health. 2013;23(3):480–5.
Saloojee H, Coovadia H. Maternal age matters: for a lifetime, or longer. Lancet Glob Health. 2015;3(7):e342–3.
Jacobsson B, Ladfors L, Milsom I. Advanced maternal age and adverse perinatal outcome. Obstet Gynecol. 2004;104(4):727–33.
Bae J, Park JH, Park YK, Kim JY, Lee SW, Park SW. Changes in the distribution of maternal age and parity and increasing trends in the low birth weight rate in Korea between 1995 and 2005. J Prev Med Public Health. 2011;44(3):111–7.
AlShami HAA, Kadasne AR, Khalfan M, Iqbal SZ, Mirghani HM. Pregnancy outcome in late maternal age in a high-income developing country. Arch Gynecol Obstet. 2011;284(5):1113–6.
Schimmel MS, Bromiker R, Hammerman C, Chertman L, Ioscovich A, Granovsky-Grisaru S, Samueloff A, Elstein D. The effects of maternal age and parity on maternal and neonatal outcome. Arch Gynecol Obstet. 2015;291(4):793–8.
Szwarcwald CL, Leal MC, Esteves-Pereira AP, Almeida WS, Frias PG, Damacena GN, Souza Júnior PRB, Rocha NM, Mullachery PMH. Avaliação das informações do Sistema de Informações sobre Nascidos Vivos (SINASC), Brasil. Cad Saude Publica. 2019;35(10):e00214918.
Gelman A. P values and statistical practice. Epidemiology (Cambridge, Mass). 2013;24(1):69–72.
Siontis GCM, Ioannidis JPA. Risk factors and interventions with statistically significant tiny effects. Int J Epidemiol. 2011;40(5):1292–307.
Acknowledgements
The authors would like to thank Andris K. Walter for his critical analysis of the manuscript, English revision and copyediting services.
Funding
This study was funded by MCTI / CNPq / MS / SCTIE / Decit / Bill & Melinda Gates Foundation’s Grandes Desafios Brasil – Desenvolvimento Saudável para Todas as Crianças (Call number 47/2014). CIDACS and the 100 million cohort received core support from the Wellcome Trust (Grant number 202912 / Z / 16 / Z), the Health Surveillance Secretariat, Ministry of Health, Brazil, Bahia State, Fundação de Amparo à Pesquisa do Estado da Bahia (FAPESB), Financiadora de Estudos e Projetos-FINEP and the Secretariat of Science and Technology of the State of Bahia-SECTI. IRF received a doctoral scholarship from the Fundação de Amparo à Pesquisa do Estado da Bahia (FAPESB) (grant number BOL2330 / 2016). ESP is a fellow supported by the Wellcome Trust (grant number 213589 / Z / 18 / Z).
Author information
Authors and Affiliations
Contributions
IRF and RCRS conceptualized and designed the study, drafted the initial manuscript, carried out the analyses, and reviewed and revised the manuscript. MFA and RLF conceptualized and designed the study and critically reviewed the intellectual content of the manuscript. MLB, LCR and MYI conceptualized and designed the study, acquired data, contributed to data interpretation and critically reviewed the intellectual content of the manuscript. ASR, NO, NJS and ESP drafted the initial manuscript and contributed to data analysis, interpretation and the critical review of the manuscript. All authors approved the final submitted version of this manuscript and accept accountability for all aspects of the work.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Institutional Review Board of the Collective Health Institute, Federal University of Bahia (ICS-UFBA) (CAAE: 41695415.0.0000.5030).
The present study exclusively employed secondary data. The respective owners of the administrative databases utilized have given Cidacs custody and permission to carry out research upon formal request, with the guarantee that all data processing occurs in a safe and private environment. All procedures for pre-processing and linking administrative data were performed in a secure room at CIDACS: an environment with strict security and data protection procedures that follows the regulatory framework and ethical standards established in Brazil. In order to access the data, each researcher needs to present a research project, ethical approval and a data plan in order to extract an unidentified/anonymized dataset for analysis. None of the researchers in this study had access to any personally identifiable information. For all analyzes, a de-identified database was used, which can only be accessed by previously authorized researchers. All steps subsequent to data obtaining were performed following CIDACS information security protocols.
Consent for publication
Not applicable.
Competing interests
The authors deny the existence of any competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1: Table S1.
Adjusted models† used to assess factors associated with term low birth weight by year of birth. Table S2. Adjusted models† used to assess factors associated with term low birth weight by exposure time at birth categorized into quartiles intervals.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Falcão, I.R., Ribeiro-Silva, R., de Almeida, M.F. et al. Factors associated with low birth weight at term: a population-based linkage study of the 100 million Brazilian cohort. BMC Pregnancy Childbirth 20, 536 (2020). https://doi.org/10.1186/s12884-020-03226-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12884-020-03226-x