Abstract
Background
Chronic fatigue is present in more than 60% of the patients with a neuromuscular disease and can be their most disabling symptom. In combination with other impairments, fatigue often results in low levels of physical activity and decreased social participation, leading to high societal costs. ‘Energetic’ is a self-management group program aimed at improving social participation, physical endurance and alleviating fatigue in these patients. The primary aim of this study is to evaluate the effectiveness and cost-effectiveness of the Energetic program.
Methods/Design
A multicentered, assessor-blinded, two-armed randomized controlled trial is conducted with evaluations at inclusion and four, seven and fifteen months later. The study includes patients with a neuromuscular disease and chronic fatigue and, when present, their caregivers. The participants are randomized (ratio 1:1) to either an intervention group, receiving the Energetic program, or a control group, receiving usual care (i.e., no specific intervention). The Energetic program covers four months and includes four modules: 1) individually tailored aerobic exercise training; 2) education about aerobic exercise; 3) self-management training in applying energy conservation strategies; and 4) implementation and relapse prevention in daily life. Two months after cessation of the program a booster session is provided. The primary outcome is the perceived performance score of the Canadian Occupational Performance Measure (COPM). Secondary outcomes include the COPM-satisfaction score, and measures of fatigue, physical endurance, activity engagement, mood, and self-efficacy. Caregiver burden is also evaluated as a secondary outcome. Health-related quality of life and medical and societal costs are assessed to estimate cost-effectiveness of the program.
Discussion
The Energetic study is the first randomized controlled trial to evaluate the effectiveness and cost-effectiveness of a combined physical and self-management group training program for improving social participation, physical endurance and alleviating fatigue in patients with neuromuscular diseases. It will generate new insights in (cost-)effective rehabilitation strategies for these incurable conditions.
Trial registration
Clinicaltrials.gov NCT02208687.
Similar content being viewed by others
Background
Chronic fatigue is present in more than 60% of patients with a neuromuscular disease (NMD), including facioscapulohumeral muscular dystrophy (FSHD), inclusion body myositis (IBM) and mitochondrial myopathies (MM), and can be their most prominent and disabling symptom [1,2]. In combination with muscle weakness, enhanced fall risk, and possible cardiopulmonary involvement, fatigue often results in low levels of physical activity and decreased social participation, which in turn leads to high societal costs. Compared to other neurological conditions, NMDs have the highest estimated costs of €30.000,- per person per year, with an estimated prevalence between 1:20.000 to 1:424 persons [3,4]. These include direct health costs related to treatment and rehabilitation, indirect costs related to low employment rates due to work absence or early retirement, and non-medical costs for social services, assistive devices and informal care [5].
In a recent randomized controlled trial, we have provided evidence that aerobic exercise training and cognitive behaviour therapy can both alleviate severe chronic fatigue in patients with FSHD [6]. Both interventions were based on a theoretical model of chronic fatigue in NMD, in which muscle strength, level of self-reported physical activity, sleep disturbances and pain were all associated with fatigue and, ultimately, with social participation [7]. Based on the first research results and experiences in patients with FSHD, we developed a multidisciplinary rehabilitation program to accommodate the clinical urge felt by many (other) patients with NMD and chronic fatigue. This rehabilitation program was called ‘Energetic’ and combines aerobic exercises and energy-conservation strategies in a self-management group program to improve social participation and physical endurance and alleviate fatigue. The program covers four months and includes four modules: (1) aerobic exercise training, (2) education about aerobic exercise, (3) self-management training in applying energy conservation strategies, and (4) implementation and relapse prevention in daily life. In the development of the program, we have acknowledged the research priorities identified by patients with NMD and healthcare professionals [8], and implemented the available clinical evidence regarding exercise training in NMD [6,9,10], fatigue management [11,12] and self-management training [13]. The following dimensions of self-management are addressed in the Energetic program; (1) medical management (e.g., regarding medication, diet or exercise (2) role management (regarding meaningful social roles), and (3) emotional management (dealing with emotions such as fear or depression) [13]. Self-management programs provide patients with the necessary knowledge, skills, and confidence (‘self-efficacy’) to manage life with a chronic illness and prepares patients to collaborate with their healthcare professionals and the healthcare system [13].
Although the Energetic program was well appreciated by participants already from the beginning, it has not yet been formally evaluated. So far, we only conducted an uncontrolled pilot study with pre-post measurements in 13 patients with a neurological condition (77% NMD) showing significant improvement in social participation based on the Canadian Occupational Performance Measure (COPM) and a significant decrease in fatigue as assessed with the Checklist Individual Strength - subscale Fatigue (CIS-Fatigue) [14]. These promising results formed the basis to conduct the present larger randomized controlled trial of the (cost-) effectiveness of the Energetic program in various forms of NMD, specifically FSHD, IBM and MM. In this study, the hypothesis is tested that the Energetic program results in improved social participation, better physical endurance and less fatigue in patients with NMD and severe chronic fatigue compared to no specific intervention (‘usual care’). Furthermore, we expect that these improvements will ultimately lead to a reduction in medical and societal costs.
Methods/Design
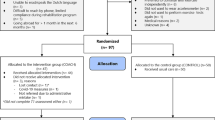
A multicentered, assessor-blinded, two-armed randomized controlled trial is conducted, in which eligible patients are randomized in a 1:1 ratio to either an intervention group, receiving the Energetic program, or a control group, receiving no specific intervention (‘usual care’). Randomization is based on a computerized minimization algorithm with the following minimization factors: gender, work (work ≥ no work), diagnosis (FSHD, IBM, MM, ≥ other NMD). Data will be collected at inclusion (before randomization, T0), at the end of the program (4 months after inclusion, T1), at three months follow-up (7 months after inclusion, T2), and at eleven months follow-up (15 months after inclusion, T3) (see Figure 1). Fifteen months after inclusion, the control group is offered participation in the Energetic program, but this post-study intervention period is not monitored.
All outcomes are assessed by blinded and independent occupational therapy research assistants. At the beginning of each assessment, participants are instructed not to reveal their group allocation to the assessor. After each assessment, blinding of the assessors is evaluated by asking them to indicate their idea of group assignment for each patient. Data entry is executed by the (blinded) research assistant. Adverse events or irregularities affecting protocol adherence are registered by the primary researcher (YV). Full ethical approval has been granted by the medical ethical committee of Arnhem-Nijmegen (NL47624.091.14) and all participating centers granted (ethical) approval to participate.
The Energetic study has been registered at clinicaltrial.gov (NCT02208687).
Setting
Patients are recruited at either the departments of Rehabilitation, Neurology or General Internal Medicine of the Radboud University Medical Centre or at a major regional rehabilitation center (RMC Groot Klimmendaal). In addition, the Dutch NMD patient association ‘Spierziekten Nederland’ facilitates patient recruitment by posting information about the study on their website, in their magazine, and by sending mails to the specific patient groups (FSHD, IBM, MM). Based on patient preference, the Energetic program is offered and evaluated in one of the following three settings: Radboud University Medical Centre (Nijmegen), RMC Groot Klimmendaal (Arnhem), and community health center Buitenlust (Venray). Three intervention groups are planned in Nijmegen, three groups in Arnhem, and one group in Venray. Intervention groups consist of four to seven patients.
Participants
Referred or otherwise interested patients are contacted by telephone by the primary investigator (YV) to provide detailed information about the content of the study, the informed consent procedure, and to answer any residual questions related to study participation. The primary informal caregiver of the patient is also asked to participate in the study when willing and available. When patients and caregivers express their willingness to participate and global screening of the inclusion and exclusion criteria indicates potential eligibility, appointments for visits with a rehabilitation physician and occupational therapist at the outpatient rehabilitation clinic of the Radboud University Medical Centre are made. During these visits the inclusion and exclusion criteria are thoroughly checked and the informed consent is signed.
Table 1 provides an overview of the applied inclusion and exclusion criteria. All patients should be at least 18 years old and have an established neuromuscular disease, preferably FSHD, IBM, or MM. They should suffer from chronic fatigue with a clear influence on their social participation. They should also be motivated for participation in the Energetic program and show ‘readiness to change’. The latter aspects are tested by motivational interviewing [15], without the use of any formal cut-off criteria. In addition, each patient has to be able to formulate at least three personalized goals with regard to social participation. Possible depressive symptoms and other psychiatric or cognitive symptoms are judged by the psychologist for their severity to determine whether patients can participate in the Energetic program.
Upon inclusion, the following socio-demographic characteristics are registered in a questionnaire: age (years), gender (male/female), living together (yes/no), level of education (low, middle, high), employment status (yes/no), relationship with caregiver (partner/sibling/ child/friend). In addition, patients’ diagnoses and years of diagnoses are recorded. Patients’ self-reported knowledge, skills and confidence with regard to self-management of their disease are registered with the Patient Activation Measure (PAM) [16].
Intervention
The Energetic program is administered in small groups of minimally four and maximally seven patients. Although it is a group program, aerobic exercise training and self-management strategies are individualized as much as possible. At all settings, the program is delivered by a physical therapist and an occupational therapist, both experienced with behavioural modification techniques, and consists of the following modules:
Aerobic exercise training
During four months (16 weeks) patients receive individually tailored aerobic exercise training from the physical therapist, amounting to sessions of 90 minutes with regular breaks as needed; during the first 9 weeks twice a week and during the last 7 weeks once weekly. Patients are expected to perform physical exercises themselves once and twice a week during these periods, respectively, so that that the overall physical training load amounts to three sessions of at least 30 minutes per week during the entire intervention period. Training intensity is aimed at 50-70% of the maximum heart rate, guided by a cardiac rhythm monitor mounted on the chest that is read out by a wrist watch. Fine tuning takes place based on the recovery rate. The training includes different exercises, such as walking on a treadmill, cycling on a home trainer, rowing, and using a cross trainer, depending on the preference and motor abilities of the individual.
Education about aerobic exercise
In three 60-minute sessions (weeks 2-4), patients are taught about general training principles by the physical therapist. During these sessions the following training principles are addressed: (1) attaining an adequate training stimulus, (2) the need to rest and recuperate, (3) designing and adhering to a feasible training program, and (4) prevention of overtraining and relapse. Besides emphasizing relapse prevention, patients are taught that relapse cannot entirely be prevented (e.g., after a flu) especially not when living with a chronic illness.
Self-management training in applying energy conservation strategies
During eight 90-minute sessions (weeks 2-8 and 10), training in energy conservation strategies is given by the occupational therapist. These sessions are based on an evidence-based program for patients with multiple sclerosis, including education, discussion, goal setting, practicing activities, and performing homework activities with the aim to teach patients how to integrate energy conservation strategies into their daily lives. [11]. The following energy conservation strategies are addressed:
(1) benefits of rests, (2) effectively communicating with the social environment, (3) applying principles of proper body mechanics and ergonomics, (4) adequately modifying the personal environment, (5) analyzing and adjusting individual activities, (6) setting priorities, (7) finding an activity-rest balance over the entire day and week, (8) setting short-term and long-term goals, and (9) careful planning of activities to achieve one’s personal goals.
Implementation and relapse prevention in daily life
During ten 60-minute sessions (weeks 5-13 and 16), the physical and occupational therapists support and empower the patients in implementation of the aerobic exercise training and energy conservation strategies into their daily lives until they are sufficiently able to maintain these skills. One session is specifically devoted to the preparation of healthy food and is provided by a dietician, while another session, provided by an occupational therapist, is specifically focused on self-management at work. Caregivers are involved in two sessions in which patients are encouraged to think about how to maintain their level of physical endurance after cessation of the intervention. During this module different types of exercise are explored and guided by sports trainers and physical therapists, such as swimming, Nordic walking, yoga, and body work-out. Patients are also stimulated to explore possibilities for exercising in their own environment and share these experiences with group members. The ultimate goal for each patient is to have a feasible home-exercise program encompassing at least three days a week. In order to check whether patients are indeed able to maintain their achieved level of physical activity and exercise, a booster session of two hours with the physical and occupational therapists is organized two months after the end of the intervention program to reinforce previously learned skills.
A typical day program lasts at least three hours and encompasses aerobic exercise training and one of the other modules, including a 45-minute break (see Table 2). Individual therapy compliance is recorded by the therapists with regard to both the attendance of training sessions, education sessions, and participation in homework assignments. Whenever applicable, patients are asked for their reasons for noncompliance or drop-out.
Before the start of the study, the participating physical and occupational therapists in each clinical setting follow a specific training how to deliver the Energetic program and adopt a self-management approach. This training consists of theoretical education as well as teaching practical skills at Energetic group sessions. During the study period, two sessions are organized for all therapists to reinforce their learned skills, to reflect on the program, and to share information among one another. At any point during the study, therapists are stimulated to contact each other to share experiences and consult the primary investigator whenever necessary (YV).
Usual care consists of continuation of every-day life, which often means regular physical therapy or sometimes no intervention at all [17]. In both the experimental and control groups, all (additional) interventions are monitored during the study period. The consultation of healthcare and social support professionals is recorded with a healthcare-utilization questionnaire at every assessment focusing on the preceding months. Patients are not restricted in any activities.
Outcome measures
All primary and secondary outcome measures for determining the effectiveness of the Energetic program are listed in Table 3. The primary outcome is the patient’s self-rated performance in three to five self-identified problematic daily occupations assessed with the Canadian Occupational Performance Measure (COPM-performance) [18]. The COPM is a semi-structured interview designed to help patients to identify problems in their occupational performance using a structured scoring method. The patient has to put forward a minimum of three and maximum of five problematic daily occupations. These occupations are subsequently rated on a 10-point scale for perceived performance capacity (1 = not able at all, 10 = perfectly able). Previous studies have shown that the COPM is a valid and responsive instrument to assess self-care, productivity and leisure and patients’ perspectives related to these activities [19,20].
Secondary measures of effectiveness include the COPM-satisfaction score (1 = not satisfied at all, 10 = extremely satisfied) [18-20], Checklist Individual Strength - subscale fatigue (CIS-Fatigue) [21], physical endurance (6-Minute Walking Test) [22], activity engagement (Activity Card Sort) [23,24], mood (Hospital Anxiety and Depression Scale) [25], and self-efficacy (General Self-Efficacy Scale) [26]. At the level of the caregiver, secondary outcomes are perceived caregiver burden (Zarit Burden Interview) [27] and objective caregiver burden (Objective Care Burden Questionnaire; a self developed scale for amount of care (hours)).
Outcome measures in the economic evaluation are costs (direct health costs and indirect societal costs) and quality adjusted life years (QALY). The quality of the health status of the patients is based on the Short Form-36 Health Survey (SF-36) [28] and costs are based on a self-developed resource utilization questionnaire.
Sample size calculation
The primary outcome is the change in COPM-performance score at the end of the program (T1) since baseline (T0). A conservative estimate of the improvement of the Energetic group compared to usual care is set at 2.0 and the standard deviation of the change in each group at 1.7. These numbers are based on the results of our pilot study with 13 participants [14]. Based on these assumptions, 13 participants are needed in each group to obtain a power of 80% (two sided t-test set 5%). Taking into account a drop-out rate of 10%, a total of 30 participants would be required. However, to meet the required estimates for determining the cost-effectiveness, our aim is to include 50 patients.
Statistical analysis
The primary variable for effectiveness will be analyzed in a covariance model with the COPM-performance scores at the end of the program (T1) as dependent variable. The baseline COPM-performance (T0) and the minimization factors will be covariates. Two-sided 95% confidence intervals will be presented. Data will be analyzed following the principle of intention-to-treat. Similarly, the secondary variables will be evaluated.
The economic evaluation is based on the principles of a cost-effectiveness (utility) analysis from a societal perspective. The primary incremental cost-effectiveness ratio is the cost per QALY gained (ICER) based on SF-6D utilities [29]. Uncertainty surrounding this ICER will be determined using the bootstrap method. A cost-effectiveness acceptability curve will be derived that is able to evaluate the probability that ‘Energetic’ is efficient against different thresholds (Willingness To Pay) for a QALY.
Discussion
To the best of our knowledge, the Energetic study is the first randomized controlled trial to evaluate the effectiveness and cost-effectiveness of a combined physical and self-management group training program for improving social participation, physical endurance and alleviating fatigue in patients with neuromuscular diseases (NMDs). We expect that this study will generate new insights in (cost-) effective rehabilitation strategies for these incurable conditions.
The current study includes patients with various forms of NMD, but specifically focuses on patients with FSHD, IBM and MM. These are all chronic degenerative muscle diseases with a slowly progressive character. The commonality among these disorders is the struggle that patients experience to manage their lives with chronic fatigue and reduced physical capacity. Although the study is powered to establish (cost-)effectiveness across the different diagnoses, an attempt will be made to perform subgroup analyses, using diagnosis as a between-subjects factor, to detect trends in differences in effect sizes and therapy compliance between groups. In addition, diversity will be addressed by examining the influence of socio-demographic characteristics on effect size and therapy compliance.
As a primary outcome, we chose the COPM because this measure potentially fits best with the self-management and participation goals of the Energetic program. The COPM assesses the perceived performance of daily activities as well as the individual satisfaction with these activities, and has shown to be a sensitive and clinically relevant outcome in many other rehabilitation studies [30-33]. In addition, a wide range of secondary outcome measures is used to fully examine and understand the impact of the Energetic program on the lives of patients with NMD and their caregivers. The economic evaluation serves to underscore the financial and societal impact of the program and to secure future reimbursement by health insurances.
We purposively included three clinical settings for a first implementation of the Energetic program: besides a university medical center, we selected a regional rehabilitation center and a community health center. This choice allows us to evaluate barriers and facilitators of implementation in each of these settings, which will help future dissemination of the Energetic program across other health institutions. To this end, we will monitor protocol adherence by therapists using a logbook, organize booster sessions for therapists during the study, and organize a group meeting with all therapists for process evaluation after the study period.
Abbreviations
- FSHD:
-
Facioscapulohumeral muscular dystrophy
- IBM:
-
Inclusion body myositis
- MM:
-
Mitochondrial myopathies
- NMD:
-
Neuromuscular diseases
- CIS:
-
Checklist Individual Strength
- COPM:
-
Canadian Occupational Performance Measure
- HRQoL:
-
Health-related quality of life
- QALY:
-
Quality adjusted life years
References
Lou JS, Weiss MD, Carter GT. Assessment and management of fatigue in neuromuscular disease. Am J Hosp Palliat Care. 2010;27(2):145–57.
Kalkman JS, Schillings ML, van der Werf SP, Padberg GW, Zwarts MJ, van Engelen BG, et al. Experienced fatigue in facioscapulohumeral dystrophy, myotonic dystrophy, and HMSN-I. J Neurol Neurosurg Psychiatry. 2005;76(10):1406–9.
Needham M, Mastaglia FL. Inclusion body myositis: current pathogenetic concepts and diagnostic and therapeutic approaches. Lancet Neurol. 2007;6(7):620–31.
Wilbers J, Frants RR, van Engelen BG, Padberg GW, Van der Maarel SM. [Facioscapulohumeral muscular dystrophy]. Ned Tijdschr Tandheelkd. 2010;117(1):11–4.
Gustavsson A, Svensson M, Jacobi F, Allgulander C, Alonso J, Beghi E, et al. Cost of disorders of the brain in Europe 2010. Eur Neuropsychopharmacol. 2011;21(10):718–79.
Voet N, Bleijenberg G, Hendriks J, de Groot I, Padberg G, van Engelen B, et al. Both aerobic exercise and cognitive-behavioral therapy reduce chronic fatigue in FSHD: an RCT. Neurology. 2014;83(21):1914–22.
Kalkman JS, Schillings ML, Zwarts MJ, van Engelen BG, Bleijenberg G. The development of a model of fatigue in neuromuscular disorders: a longitudinal study. J Psychosom Res. 2007;62(5):571–9.
Nierse CJ, Abma TA, Horemans AM, van Engelen BG. Research priorities of patients with neuromuscular disease. Disabil Rehabil. 2013;35(5):405–12.
Voet NB, van der Kooi EL, Riphagen II, Lindeman E, Van Engelen BG, Geurts AC. Strength training and aerobic exercise training for muscle disease. Cochrane Database Syst Rev. 2013;7:CD003907.
Cup EH, Pieterse AJ, Ten Broek-Pastoor JM, Munneke M, van Engelen BG, Hendricks HT, et al. Exercise therapy and other types of physical therapy for patients with neuromuscular diseases: a systematic review. Arch Phys Med Rehabil. 2007;88(11):1452–64.
Mathiowetz VG, Finlayson ML, Matuska KM, Chen HY, Luo P. Randomized controlled trial of an energy conservation course for persons with multiple sclerosis. Mult Scler. 2005;11(5):592–601.
Mathiowetz VG, Matuska KM, Finlayson ML, Luo P, Chen HY. One-year follow-up to a randomized controlled trial of an energy conservation course for persons with multiple sclerosis. Int J Rehabil Res. 2007;30(4):305–13.
Lorig KR, Sobel DS, Ritter PL, Laurent D, Hobbs M. Effect of a self-management program on patients with chronic disease. Eff Clin Pract. 2001;4(6):256–62.
Cup E, Nab N, Maas D, De Roode M, De Groot IJM, Smeenge M, et al. ENERGETIC, a multidisciplinary self-management group program for reconditioning and managing fatigue. Neuromuscul Disord. 2012;22(9-10):896–7.
Copeland L, McNamara R, Kelson M, Simpson S. Mechanisms of change within motivational interviewing in relation to health behaviors outcomes: a systematic review. Patient Educ Couns. 2015;98(4):401–11.
Rademakers J, Nijman J, van der Hoek L, Heijmans M, Rijken M. Measuring patient activation in The Netherlands: translation and validation of the American short form Patient Activation Measure (PAM13). BMC Public Health. 2012;12:577.
Cup EH, Pieterse AJ, Knuijt S, Hendricks HT, van Engelen BG, Oostendorp RA, et al. Referral of patients with neuromuscular disease to occupational therapy, physical therapy and speech therapy: usual practice versus multidisciplinary advice. Disabil Rehabil. 2007;29(9):717–26.
McColl MA, Law M, Baptiste S, Pollock N, Carswell A, Polatajko HJ. Targeted applications of the Canadian Occupational Performance Measure. Can J Occup Ther. 2005;72(5):298–300.
Dedding C, Cardol M, Eyssen IC, Dekker J, Beelen A. Validity of the Canadian Occupational Performance Measure: a client-centred outcome measurement. Clin Rehabil. 2004;18(6):660–7.
Eyssen IC, Beelen A, Dedding C, Cardol M, Dekker J. The reproducibility of the Canadian Occupational Performance Measure. Clin Rehabil. 2005;19(8):888–94.
Vercoulen JH, Swanink CM, Fennis JF, Galama JM, van der Meer JW, Bleijenberg G. Dimensional assessment of chronic fatigue syndrome. J Psychosom Res. 1994;38(5):383–92.
Enright PL. The six-minute walk test. Respir Care. 2003;48(8):783–5.
Jong AM, van Nes FA, Lindeboom R. The Dutch Activity Card Sort institutional version was reproducible, but biased against women. Disabil Rehabil. 2012;34(18):1550–5.
Foster ER, Golden L, Duncan RP, Earhart GM. Community-based Argentine tango dance program is associated with increased activity participation among individuals with Parkinson’s disease. Arch Phys Med Rehabil. 2013;94(2):240–9.
Spinhoven P, Ormel J, Sloekers PP, Kempen GI, Speckens AE, Van Hemert AM. A validation study of the Hospital Anxiety and Depression Scale (HADS) in different groups of Dutch subjects. Psychol Med. 1997;27(2):363–70.
Romppel M, Herrmann-Lingen C, Wachter R, Edelmann F, Dungen HD, Pieske B, et al. A short form of the General Self-Efficacy Scale (GSE-6): Development, psychometric properties and validity in an intercultural non-clinical sample and a sample of patients at risk for heart failure. Psychosoc Med. 2013;10:Doc01.
Van Durme T, Macq J, Jeanmart C, Gobert M. Tools for measuring the impact of informal caregiving of the elderly: a literature review. Int J Nurs Stud. 2012;49(4):490–504.
Aaronson NK, Muller M, Cohen PD, Essink-Bot ML, Fekkes M, Sanderman R, et al. Translation, validation, and norming of the Dutch language version of the SF-36 Health Survey in community and chronic disease populations. J Clin Epidemiol. 1998;51(11):1055–68.
Health Economics and Decision Science, SF-6D [https://www.shef.ac.uk/scharr/sections/heds/mvh/sf-6d]
Sturkenboom IH, Graff MJ, Hendriks JC, Veenhuizen Y, Munneke M, Bloem BR, et al. Efficacy of occupational therapy for patients with Parkinson’s disease: a randomised controlled trial. Lancet Neurol. 2014;13(6):557–66.
Carswell A, McColl MA, Baptiste S, Law M, Polatajko H, Pollock N. The Canadian Occupational Performance Measure: a research and clinical literature review. Can J Occup Ther. 2004;71(4):210–22.
Geerdink Y, Aarts P, Geurts AC. Motor learning curve and long-term effectiveness of modified constraint-induced movement therapy in children with unilateral cerebral palsy: a randomized controlled trial. Res Dev Disabil. 2013;34(3):923–31.
Cup EH, Scholte OP, Reimer WJ, Thijssen MC, Van Kuyk-Minis MA. Reliability and validity of the Canadian Occupational Performance Measure in stroke patients. Clin Rehabil. 2003;17(4):402–9.
Acknowledgements
Following a thorough review procedure of the study proposal by the funding organisation on relevance and quality, this study is funded by the Netherlands Organisation for Health Research and Development (ID; ZonMw; 837001402), the National Rehabilitation Fund (Nationaal Revalidatie Fonds) and Centre of Expertise “Sneller herstel”.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
YV is primary investigator and responsible for data collection, supervising the therapists, and drafting the manuscript. JH will perform the statistical analysis and EA will perform the cost-effectiveness analysis. EC, JG, AG, BvE, JH and EA designed and supervised the study and obtained funding. All authors helped in finalizing the manuscript. All authors read and approved the final manuscript.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Veenhuizen, Y., Cup, E.H., Groothuis, J.T. et al. Effectiveness and cost-effectiveness of a self-management group program to improve social participation in patients with neuromuscular disease and chronic fatigue: protocol of the Energetic study. BMC Neurol 15, 58 (2015). https://doi.org/10.1186/s12883-015-0314-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12883-015-0314-4