Abstract
Background
The clinic-pathological features and outcomes of Chinese patients with antineutrophil cytoplasmic autoantibody (ANCA)-positive eosinophilic granulomatosis with polyangiitis (EGPA) and renal involvement have not been studied.
Methods
Fourteen EGPA patients with renal involvement were included. All patients underwent renal biopsy. Clinic-pathological features and outcomes were retrospectively analyzed.
Results
The most common initial symptom of EGPA was asthma (57.1 %), followed by hemoptysis (21.4 %), gross hematuria (14.3 %), and arthritis (7.1 %). All patients had positive serum ANCA (anti-MPO in 12, anti-PR3 in 2). Elevated eosinophils (median 15 %, range 10–45 %) were found in all patients. The median serum IgE level was 463 g/L (range 200–1000 g/L). All patients presented with renal dysfunction, with a median SCr of 5.4 mg/dL (range 1.47–11 mg/dL), seven patients (50 %) required initial renal replacement therapy. Thirteen patients showed hematuria and proteinuria (median 1.1 g/24 h, range 0.5–7.8 g/24 h). Renal biopsy showed pauci-immune segmental necrotizing glomerulonephritis with crescents in 13 patients and acute interstitial nephritis in one patient. Twelve patients (85.7 %) showed renal interstitial eosinophil infiltration, among whom three had eosinophilic granuloma. Among seven patients (71.4 %) who required initial dialysis, 5 discontinued dialysis, one died, one received maintenance dialysis after glucocorticoids plus immunosuppressive for induction treatment. Twelve patients were followed up for a median of 43.5 months (range 6–83 months), during follow-up, two patients progressed to end-stage renal disease, nine had chronic kidney disease with eGFR < 60 mL/min, and two patients had normal eGFR.
Conclusions
Renal involvement in ANCA-positive EGPA could be severe and showed varied renal histology. Although intensive immunosuppressive therapy effectively improved the renal function, the long-term renal survival was poor. Early diagnosis and treatment are essential to improve long-term renal survival.
Similar content being viewed by others
Background
Eosinophilic granulomatosis with polyangiitis (EGPA), previously termed Churg–Strauss syndrome [1], is a rare vasculitis disease, characterized by asthma, eosinophilia, and systemic vasculitis. EGPA is categorized as an antineutrophil cytoplasmic antibody (ANCA)-associated vasculitis (AAV), but only 35–40 % of EGPA patients are reported to be ANCA positive, mostly are MPO-ANCA positive [2, 3].
Renal disease has been reported in 25–45 % of EGPA [4, 5], with a higher incidence of renal involvement among ANCA-positive patients. Renal manifestations of the disease were diverse, most patients had mild urinary abnormalities [1, 6], whereas some presented with severe, rapidly progressive glomerulonephritis requiring dialysis [5]. Renal damage was reported to be more severe among ANCA-positive EGPA patients [5, 7]. The typical histopathological lesion was pauci-immune focal segmental necrotizing glomerulonephritis with crescent formation. However, other histological lesions have been reported, and eosinophilic interstitial infiltrates have been described [5]. The reported long-term renal survival of EGPA was variable. Most studies reported that renal function generally remained stable, whereas some studies reported that a proportion of patients progressed to ESRD, but all were reported European countries [8, 9]. In this study, we retrospectively analyzed the clinic-pathological features and outcomes of 14 Chinese patients with ANCA-positive EGPA.
Methods
Patients
Patients with EGPA were identified from AAV in the National Clinical Research Center of Kidney Diseases, Jinling Hospital, from January 1998 to December 2012. All patients met four or more of the following diagnostic criteria for EGPA, as proposed by the American Rheumatism Association in 1990 [10]: (1) asthma; (2) peripheral blood eosinophils > 10 %; (3) mononeuritis (including multiplex) or polyneuropathy; (4) nonfixed pulmonary infiltrates on roentgenography; (5) paranasal sinusitis; and (6) extravascular eosinophils proven histologically. All patients had renal involvement, and underwent renal biopsy.
Clinical and laboratory data
Clinical measurement included age at disease onset, duration of EGPA, initial symptoms and organ involvement, red blood cell count of the urinary sediment, 24 h urinary protein excretion, and serum creatinine (SCr). Serum ANCA and anti-glomerular basement membrane antibody were detected by both indirect immunofluoresence and enzyme-linked immunosorbent assay. The estimated glomerular filtration rate (eGFR) was estimated by the Chronic Kidney Disease Epidemiology Collaboration equation [11].
Nephrotic syndrome was defined as proteinuria ≥ 3.5 g/24 h and serum albumin < 30 g/L. Rapidly progressive glomerulonephritis was defined as massive hematuria, ccompanied by a rapidly progressive decline in renal function. Chronic kidney disease (CKD) was defined as eGFR < 60 mL/min/1.73 m2 lasting for more than 3 months and stages of CKD were defined according to eGFR as Stage 3: eGFR 30–59 mL/min/1.73 m2, Stage 4: eGFR 15–29 mL/min/1.73 m2, or Stage 5 (ESRD): eGFR < 15 mL/min/1.73 m2 lasted for at least 3 months [12].
Renal histology
Renal biopsy samples obtained from all patients were examined with light microscopy, immunofluorescence, and electronic microscopy. Renal tissues were routinely stained with hematoxylin and eosin, PAS, and PASM-Masson for light microscopy. Frozen sections were used for immunofluorescence. For electron microscopy, tissue samples were stained with sodium acetate and lead citrate and examined with a transmission electron microscope. Glomerular histology was categorized into four classes: focal (≥50 % normal glomeruli), crescentic (≥50 % glomeruli with cellular crescents), mixed (<50 % normal, <50 % crescentic, and <50 % globally sclerotic glomeruli), and sclerotic (≥50 % globally sclerotic glomeruli) [13]. Extensive foot process effacement was defined as an area of podocyte foot process effacement larger than 50 % of the capillary loop by electron microscopy.
Treatment
Induction therapy included glucocorticoids, glucocorticoids plus mycophenolate mofetil (MMF,1–1.5 g/d), or intravenous cyclophosphamide pulse (IV-CTX) as previously reported [14]. For patients with severe renal damage or pulmonary hemorrhage received intravenous methylprednisolone (500 mg/d for 3–6d) pulse therapy and additional immunoadsorption, followed by oral prednisone (started at 0.6 mg/kg/d for 4 weeks, then reduced gradually to a maintenance dosage of 10 mg/d) [15].
Maintenance therapy included prednisone (10 mg/d) plus azathioprine (AZA,50–100 mg/d) or Tripterygium wilfordii polyglycoside (TW, a Chinese herbal medicine; 60 mg/d) [16].
Statistical analysis
Data are presented as mean ± SD or median (range). Statistical analysis was performed with SPSS 16.0 statistical package (SPSS Inc., Chicago, IL, USA).
Results
Patient data
The 14 EGPA patients accounted for 5.0 % of the 282 Chinese AAV patients in our department during the study period. Eight were female and six were male, with a median age of 53 years (range 20–70 years), duration of EGPA 120 months (range 1–600 months) and duration of renal involvement 1.0 month (range 0.5–36 months). The duration between EGPA and renal involvement was 119 months (range 0–598 months) (Table 1). Prior to the admission, 12 patients received no glucocorticoids or immunosuppressive agents, two patients (Cases 4 and 9) received low-dose glucocorticoids.
Laboratory measurements
All 14 patients were serum ANCA positive, twelve were P-/MPO-ANCA, with MPO-ANCA levels of 20–674.64 RU/ml, two were C-/PR3-ANCA.
All patients had elevated eosinophils in the peripheral blood (median 15 %, range 10–45 %) and elevated serum IgE level (median 463 g/L, range 200–1000 g/L). Eleven patients (78.6 %) presented with anemia (Table 1).
Onset of symptoms
Eight patients (57.1 %) presented with asthma as the initial symptom, asthma were mostly paroxysmal, only one patient presented with persistent asthma. The median interval between the onset of asthma and systemic vasculitis was 239 months (range119–598 months). The remaining six patients initially presented with symptoms of systemic vasculitis, including hemoptysis (n = 3), gross hematuria (n = 2), and arthritis (n = 1) (Tables 1 and 3).
Extra-renal manifestations
The lungs were the most common extra-renal organ involved, with pulmonary hemorrhage in six patients (42.9 %), interstitial lung disease in four (28.6 %), and pulmonary nodules in one (7.1 %). The upper respiratory tract was the second common involved. Other organ involvement included the skin, peripheral nerves, joints, ears, and eyes (Table 2).
Renal manifestations
Twelve patients (85.7 %) presented with rapidly progressive glomerulonephritis and two with CKD. All patients but one had both hematuria and proteinuria (Table 1). Urine protein ranged from 0.5–7.8 g/24 h (median 1.1 g/24 h). Five patients (35 %) presented with nephrotic syndrome, and two patients had gross hematuria. All patients had renal dysfunction, with a median SCr level of 5.4 mg/dl (range1.47–11.0 mg/dl) and a median eGFR of 9.8 mL/min/1.73 m2 (range 3.5–52.2 mL/min/1.73 m2), seven patients (50 %) initially required dialysis.
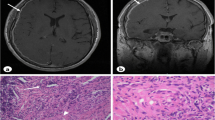
Thirteen renal biopsies showed pauci-immune segmental necrotizing glomerulonephritis, and one biopsy (Case 2) showed acute interstitial nephritis with normal glomeruli. Thirteen biopsies (92.8 %) showed glomerular crescents with the median crescents 39 % (range 9–90 %). Ten patients (71.4 %) showed glomerular segmental necrosis. The median glomerular sclerotic ratio was 26 % (range 0–80 %). Twelve patients (85.7 %) had renal interstitial eosinophilic infiltration, three of whom showed renal interstitial eosinophilic granuloma. Renal histologic classification included crescentic type in four, mixed in six, focal in two, and sclerotic in one. Six biopsies were evaluated with electron microscopy, and three of the patients with nephrotic syndrome showed extensive foot process effacement (Table 3).
Treatment and outcomes
Induction treatment included glucocorticoids plus MMF regimen (n = 6) or IV-CTX regimen (n = 4), or glucocorticoids alone (n = 4; Cases 11 and 12 were complicated with pneumonia on admission, Case 13 was sclerotic type and case 14 died at 2 weeks of treatment). Twelve patients were given methylprednisolone pulse therapy; five patients received additional immunoadsorption therapy.
During induction period, five of seven patients (71.4 %) who needed initial dialysis were able to discontinue dialysis, three of them received the MMF regimen, one received the IV-CTX regimen and one received glucocorticoids alone. One patient (Case 13) required maintenance dialysis, and the other one (Case 14) died of cardiac arrhythmia at 2 weeks.
Maintenance therapy included glucocorticoids combined with AZA (n = 6), TW (n = 5) or glucocorticoids alone (n = 1) (Table 3). The other 12 patients were follow-up for a median of 43.5 months (range 6–83 months). At last visit, two patients (14.2 %) had normal renal function, nine (64.3 %) were CKD stage 3–4 with a mean SCr of 2.13 ± 0.03 mg/dl (range 1.58–2.45) and eGFR (20.3–39.8 mL/min/1.73 m2), and one patient (Case 10) progressed to ESRD.
None of the five patients who needed initial dialysis and were able to discontinue it progressed to ESRD during 46–63 months (mean 52.4 ± 7.0 months) follow-up. At last visit, the median SCr was 1.21–2.30 mg/dL with an eGFR of 24.7–64.4 mL/min/1.73 m2.
During the follow-up, serum ANCA turned negative in four patients, declined in eight patients. One patient (Case 2) relapsed with hemoptysis, skin rash, and eosinophilia, which were concurrent with increased serum ANCA level in the 25th month of follow-up. No patient died during maintenance treatment.
Discussion
EGPA, the incidence was reported to be 0.5–6.8 patients per million per year [8, 9], accounted for 12.2–21.4 % of AAV in European countries [17, 18]. EGPA accounted for 5.0 % of patients with AAV in this study, which was consistent with a report from Japan, but was lower than that reported in European studies [19].
Typical EGPA presented with three stages [20]: the allergic stage (characterized by prodromal symptoms of asthma and anaphylactic rhinitis), the eosinophilic stage (marked by hypereosinophilia and eosinophilic infiltration in tissues), and the vasculitic stage (with systematic vasculitis). The patients in European studies were reported to have typical allergic disease; the incidence of asthma in those studies was as high as 96–100 % [9, 21]. Among our patients, only 57.1 % had a history of asthma or other allergic symptoms prior to the onset of vasculitis. The reported incidence of asthma among EGPA patients in Japan is 72.7–89 % [19, 22]. Hence, the reported incidence of asthma among patients with EGPA is lower in Asian populations than in European countries, a difference that might result from racial and geographic differences. In our study, vasculitis arose without prodromal allergic symptoms in 42.8 % of the patients, suggesting rapid disease progression. In fact, no significant association has been found between allergic disease and EGPA severity [21, 23, 24].
Previous studies [1, 6, 8] found that the renal involvement in EGPA is usually mild with a benign course, which is an important difference between EGPA and other types of AAV. Chumbley and colleagues [7] reported that six of 30 EGPA patients had isolated microscopic hematuria, and three had slightly increased SCr. Lanham et al. [8] reported that among 16 EGPA patients, only four had renal involvement. However, in recent years, several studies [2, 5, 25] found that EGPA patients with positive serum ANCA had severe renal damage. Sinico et al. [5] reported that among 30 EGPA patients who presented with rapidly progressive glomerulonephritis, 75 % were ANCA positive, and 50 % had renal dysfunction. Clutterbuck et al. [25] found that 87 % of EGPA patients had renal dysfunction and 18.6 % had nephrotic syndrome; four patients had SCr levels exceeding 500 μmol/L. Compared with previous reports, the renal damage of patients in our study was more severe; all patients had renal dysfunction and half required dialysis. Moreover, 35.7 % of patients had nephrotic syndrome, and the percentage of glomeruli with crescent lesions was high, with a mean of 38 %. It was unclear whether the difference in severity of renal involvement in our study versus others was associated with positive serum ANCA or with racial differences.
Lanham et al. [8] described the histological features of EGPA as eosinophilic tissue infiltration, extravascular granulomatosis, and necrotizing vasculitis [1, 6]. The former two histological findings were thought to differentiate EGPA from other types of AAV. However, it was reported that these specific lesions rarely existed simultaneously. In the present study, only three patients had all three of these lesions, but the proportion of eosinophilic infiltration and eosinophilic granuloma in the renal interstitium were higher in our study than in other reports [5, 25], consistent with increased eosinophils and IgE levels in the peripheral blood. This finding indicates that these pathological changes are not uncommon in the active stage of the disease, which is the key clue to the diagnosis of EGPA. We also found one patient who had only interstitial nephritis without glomerular involvement. Similar cases have been reported in the literature [5, 17, 26]. In addition, other renal diseases, such as IgA nephropathy [15] and focal segmental glomerulosclerosis [27], have also been reported, suggesting that the renal damage of EGPA can vary. Moreover, five patients had massive proteinuria, which was a higher percentage than that in previous reports [5, 25]. Electron microscopy showed extensive podocyte foot process fusion, which is characteristic of podocyte disease. Park et al. [27] reported the case of an EGPA patient with massive proteinuria, whose renal histology showed focal segmental glomerulosclerosis. This finding indicates that EGPA can also cause podocyte disease by undefined pathogenesis.
Immunosuppressive treatment could improve the renal function of EGPA [28, 29]. In this study, five of seven patients were able to discontinue dialysis. After immunosuppressive therapy with glucocorticoids combined with either MMF or IV-CTX, SCr levels returned to normal in one patient who needed initial renal replacement therapy. The currently recommended regimen is glucocorticoids combined with IV-CTX as induction therapy. However, the IV-CTX regimen had substantial adverse effects and relapses are frequent [30]. Although MYCYC [31], a randomized controlled study compared the efficacy of MMF and IV-CTX regimens, was unable to demonstrate that MMF was non-inferior to IV-CTX in induction therapy for AAV. Our previous study found that MMF was effective in inducing remission and improving renal function in Chinese patients with microscopic polyangiitis (MPA) [14], suggesting that MMF may have therapeutic potential in Chinese MPA patients. Other small sample, non-controlled studies also showed that MMF was effective in inducing remission in patients with AAV [32–35], indicating that glucocorticoids plus MMF might be an alternative regimen for the treatment of AAV. Because EGPA is a rare disease and no large-scale, randomized controlled trials for treatment. Despite the distinct differences in clinical character and pathogenesis among MPA, granulomatosis with polyangiitis and EGPA, the treatment regimens for these AAV are not different and the patients have been uniformly treated according to disease stage and severity. Both IV-CTX and MMF were effective in the treatment of EGPA in this study; however, given the small sample size of this study, the difference in treatment response between the two regimens was only observational.
During the follow-up period, only two patients had renal function return to normal; nine patients developed Stage 3–4CKD and two progressed to Stage 5 CKD. The long-term renal survival in this study was lower than that reported in other studies [5, 25, 36]. The study of the French Vasculitis Study Group demonstrated that SCr ≥140 μmol/L and proteinuria ≥1 g/d were risk factors for poor renal prognosis in EGPA. In the present study, 64.3 % of patients had both of the above risk factors. Moreover, the high proportion of glomerular crescents and sclerosis, severe renal interstitial fibrosis, and old age seen in our patients were all considered to be poor renal prognosis [28, 29]. In addition, IMPROVE study [37] found that MMF was less effective than AZA for maintaining remission and glucocorticoids combined with AZA has been recommended as the maintenance therapy for AAV. But in this study, only half of the patients were given AZA as maintenance therapy, the dosage of AZA was also lower than that recommended by EULAR [38], which may be associated with the increased risk of renal relapse and low renal survival rate.
This study has several limitations. First, all patients were Chinese, so the results of this study might not apply to other populations. Second, all patients were ANCA positive, we did not compare the difference between ANCA-positive and ANCA-negative EGPA. Third, sample size was small and the conclusions need further investigation. Forth, for a retrospective study, the treatment regimens and the dosage of the immunosuppressive agents were not uniform. These factors may affect our assessments of the clinical features, renal outcomes and treatment efficacy for patients with EGPA.
Conclusions
Renal involvement in ANCA-positive Chinese EGPA patients could be severe, and long-term renal survival was poor in this study. Intensive immunosuppressive therapy effectively improves renal function, therefore, early diagnosis and treatment are essential to improve long-term renal survival.
Abbreviations
AAV, ANCA associated vasculitis; ANCA, antineutrophil cytoplasmic autoantibody; AZA, azathioprine; CKD, chronic kidney disease; eGFR, estimated glomerular filtration rate; EGPA, eosinophilic granulomatosis with polyangiitis; IV-CTX, intravenous cyclophosphamide pulse; MMF, mycophenolate mofetil; SCr, serum creatinine; TW, tripterygium wilfordii polyglycoside
References
Churg J, Strauss L. Allergic granulomatosis, allergic angiitis, and periarteritisnodosa. Am J Pathol. 1951;27:277–301.
Sinico RA, Di Toma L, Maggiore U, Bottero P, Radice A, Tosoni C, Grasselli C, Pavone L, Gregorini G, Monti S, Frassi M, Vecchio F, Corace C, Venegoni E, Buzio C. Prevalence and clinical significance of antineutrophil cytoplasmic antibodies in churg-strauss syndrome. Arthritis Rheum. 2005;52:2926–35.
Sablé-Fourtassou R, Cohen P, Mahr A, Pagnoux C, Mouthon L, Jayne D, Blockmans D, Cordier JF, Delaval P, Puechal X, Lauque D, Viallard JF, Zoulim A, Guillevin L. French vasculitis study group. Antineutrophil cytoplasmic antibodies and the churg-strauss syndrome. Ann Intern Med. 2005;143:632–8.
Keogh KA, Specks U. Churg-strauss syndrome: clinical presentation, antineutrophil cytoplasmic antibodies, and leukotriene receptor antagonists. Am J Med. 2003;115:284–90.
Sinico RA, Di Toma L, Maggiore U, Tosoni C, Bottero P, Sabadini E, Giammarresi G, Tumiati B, Gregorini G, Pesci A, Monti S, Balestrieri G, Garini G, Vecchio F, Buzio C. Renal involvement in churg-strauss syndrome. Am J Kidney Dis. 2006;47:770–9.
Chumbley LC, Harrison Jr EG, DeRemee RA. Allergic granulomatosis and angiitis (churg-strauss syndrome). report and analysis of 30 cases. Mayo Clin Proc. 1977;52:477–84.
Sokolowska BM, Szczeklik WK, Wludarczyk AA, Kuczia PP, Jakiela BA, Gasior JA, Bartyzel SR, Rewerski PA, Musial J. ANCA-positive and ANCA-negative phenotypes of eosinophilic granulomatosis with polyangiitis (EGPA): outcome and long-term follow-up of 50 patients from a single polish center. Clin Exp Rheumatol. 2014;32(3 Suppl 82):S41–47.
Lanham JG, Elkon KB, Pusey CD, Hughes GR. Systemic vasculitis with asthma and eosinophilia: a clinical approach to the churg-strauss syndrome. Medicine (Baltimore). 1984;63:65–81.
Della Rossa A, Baldini C, Tavoni A, Tognetti A, Neglia D, Sambuceti G, Puccini R, Colangelo C, Bombardieri S. Churg-strauss syndrome: clinical and serological features of 19 patients from a single Italian centre. Rheumatology (Oxford). 2002;41:1286–94.
Masi AT, Hunder GG, Lie JT, Michel BA, Bloch DA, Arend WP, Calabrese LH, Edworthy SM, Fauci AS, Leavitt RY. The American College of rheumatology 1990 criteria for the classification of churg-strauss syndrome (allergic granulomatosis and angiitis). Arthritis Rheum. 1990;33:1094–100.
Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro 3rd AF, Feldman HI, Kusek JW, Eggers P, Van Lente F, Greene T, Coresh J. CKD-EPI (chronic kidney disease epidemiology collaboration). a new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150:604–12.
Levey AS, de Jong PE, Coresh J, El Nahas M, Astor BC, Matsushita K, Gansevoort RT, Kasiske BL, Eckardt KU. The definition, classification, and prognosis of chronic kidney disease: a KDIGO controversies conference report. Kidney Int. 2011;80:17–28.
Berden AE, Ferrario F, Hagen EC, Jayne DR, Jennette JC, Joh K, Neumann I, Noël LH, Pusey CD, Waldherr R, Bruijn JA, Bajema IM. Histopathologic classification of ANCA-associated glomerulonephritis. J Am SocNephrol. 2010;21:1628–36.
Hu W, Liu C, Xie H, Chen H, Liu Z, Li L. Mycophenolatemofetil versus cyclophosphamide for inducing remission of ANCA vasculitis with moderate renal involvement. Nephrol Dial Transplant. 2008;23:1307–12.
Hu W, Liu Z, Ji D, Xie H, Gong D, Li L. Staphylococcal protein a immunoadsorption for Goodpasture’s syndrome in four Chinese patients. J Nephrol. 2006;19:312–7.
Chen Y, Gong Z, Chen X, Tang L, Zhao X, Yuan Q, Cai G. Tripterygium wilfordii hook F (a traditional Chinese medicine) for primary nephrotic syndrome. Cochrane Database Syst Rev. 2013;11:8. doi:10.1002/14651858.
Mahr A, Guillevin L, Poissonnet M, Aymé S. Prevalences of polyarteritisnodosa, microscopic polyangiitis, Wegener’s granulomatosis, and churg-strauss syndrome in a french urban multiethnic population in 2000: a capture-recapture estimate. Arthritis Rheum. 2004;51:92–9.
Watts RA, Lane SE, Scott DG, Koldingsnes W, Nossent H, Gonzalez-Gay MA, Garcia-Porrua C, Bentham GA. Epidemiology of vasculitis in Europe. Ann Rheum Dis. 2001;60:1156–7.
Horai Y, Miyamura T, Hirata A, Nakamura M, Takahama S, Ando H, Minami R, Yamamoto M, Suematsu E. Churg-strauss syndrome: a retrospective study of 11 cases from a single center in Japan. Int J Rheum Dis. 2010;13:e6–e10.
Fauci AS, Haynes B, Katz P. The spectrum of vasculitis: clinical, pathologic, immunologic and therapeutic considerations. Ann Intern Med. 1978;89(5 Pt 1):660–76.
Baldini C, Talarico R, Della Rossa A, Bombardieri S. Clinical manifestations and treatment of churg-strauss syndrome. Rheum Dis Clin North Am. 2010;36:527–43.
Shimoi T, Shojima K, Murota A, Takizawa Y, Maruyama J, Setoguchi K. Clinical and pathological features of churg Strauss syndrome among a Japanese population: a case series of 18 patients. Asian Pac J Allergy Immunol. 2012;30:61–70.
Sharma BK, Daga MK, Sharma M. A limited form of churg-strauss syndrome presenting without asthma and eosinophilia. Med J Aust. 2004;181:498–9.
Solans R, Bosch JA, Pérez-Bocanegra C, Selva A, Huguet P, Alijotas J, Orriols R, Armadans L, Vilardell M. Churg-strauss syndrome: outcome and long-term follow-up of 32 patients. Rheumatology (Oxford). 2001;40:763–71.
Clutterbuck EJ, Evans DJ, Pusey CD. Renal involvement in churg-strauss syndrome. Nephrol Dial Transplant. 1990;5:161–7.
Kikuchi Y, Ikehata N, Tajima O, Yoshizawa N, Miura S. Glomerular lesions in patients with churg-strauss syndrome and the anti-myeloperoxidase antibody. Clin Nephrol. 2001;55:429–35.
Park SY, Chang JH, Kim HW, Kim DK, Kim EY, Park JT, Chang TI, Park JW, Jeong HJ, Han DS, Kang SW. A case of nephrotic syndrome in a patient with churg-strauss syndrome. Rheumatol Int. 2010;30:1385–8.
Guillevin L, Lhote F, Cohen P, Jarrousse B, Lortholary O, Généreau T, Léon A, Bussel A. Corticosteroids plus pulse cyclophosphamide and plasma exchanges versus corticosteroids plus pulse cyclophosphamide alone in the treatment of polyarteritisnodosa and churg-strauss syndrome patients with factors predicting poor prognosis. A prospective, randomized trial in sixty-two patients. Arthritis Rheum. 1995;38:1638–45.
Ribi C, Cohen P, Pagnoux C, Mahr A, Arène JP, Lauque D, Puéchal X, Letellier P, Delaval P, Cordier JF, Guillevin L. French VasculitisStudy group. Treatment of churg-strauss syndrome without poor-prognosis factors: a multicenter, prospective, randomized, open-label study of seventy-two patients. Arthritis Rheum. 2008;58:586–94.
Mukhtyar C, Flossmann O, Hellmich B, Bacon P, Cid M, Cohen-Tervaert JW, Gross WL, Guillevin L, Jayne D, Mahr A, Merkel PA, Raspe H, Scott D, Witter J, Yazici H, Luqmani RA. European vasculitis study group (EUVAS). outcomes from studies of antineutrophil cytoplasm antibody associated vasculitis: a systematic review by the European league against rheumatism systemic vasculitis task force. Ann Rheum Dis. 2008;67:1004–10.
JonesR HL, BallarinJ BD, Brogan P, Bruchfeld A, Cid M, Dahlsveen K, Dezoysa J, Lanyon P, Peh CA, Tesar V, Vaglio A, Walsh M, Walsh D, Walters G, Jayne D. A randomized trial of mycophenolate mofetil versus cyclophosphamide for remission induction of ANCA-associated vasculitis: “MYCYC”.on behalf of the European vasculitis study group [abstract]. Presse Med. 2013;42:678–9.
Silva F, Specks U, Kalra S, Hogan MC, Leung N, Sethi S, Fervenza FC. Mycophenolate mofetil for induction and maintenance of remission in microscopic polyangiitis with mild to moderate renal involvement–a prospective, open-label pilot trial. Clin J Am SocNephrol. 2010;5:445–53.
Joy MS, Hogan SL, Jennette JC, Falk RJ, Nachman PH. A pilot study using mycophenolate mofetil in relapsing or resistant ANCA small vessel vasculitis. Nephrol Dial Transplant. 2005;20:2725–32.
Koukoulaki M, Jayne DR. Mycophenolate mofetil in anti-neutrophil cytoplasm antibodies-associated systemic vasculitis. Nephron Clin Pract. 2006;102:c100–107.
Stassen PM, Tervaert JW, Stegeman CA. Induction of remission in active anti-neutrophil cytoplasmic antibody-associated vasculitis with mycophenolate mofetil in patients who cannot be treated with cyclophosphamide. Ann Rheum Dis. 2007;66:798–802.
Comarmond C, Pagnoux C, Khellaf M, Cordier JF, Hamidou M, Viallard JF, Maurier F, Jouneau S, Bienvenu B, Puéchal X, Aumaître O, Le Guenno G, Le Quellec A, Cevallos R, Fain O, Godeau B, Seror R, Dunogué B, Mahr A, Guilpain P, Cohen P, Aouba A, Mouthon L, Guillevin L. French vasculitis study group. Eosinophilic granulomatosis with polyangiitis (churg-strauss): clinical characteristics and long-term follow up of the 383 patients enrolled in the French vasculitis study group cohort. Arthritis Rheum. 2013;65:270–81.
Hiemstra TF, Walsh M, Mahr A, Savage CO, de Groot K, Harper L, Hauser T, Neumann I, Tesar V, Wissing KM, Pagnoux C, Schmitt W, Jayne DR. European vasculitis study group (EUVAS). mycophenolate mofetil vs azathioprine for remissionmaintenance in antineutrophil cytoplasmic antibody-associated vasculitis: a randomized controlled trial. JAMA. 2010;304:2381–8.
Mukhtyar C, Guillevin L, Cid MC, Dasgupta B, de Groot K, Gross W, Hauser T, Hellmich B, Jayne D, Kallenberg CG, Merkel PA, Raspe H, Salvarani C, Scott DG, Stegeman C, Watts R, Westman K, Witter J, Yazici H, Luqmani R. European vasculitis study group. EULAR recommendations for the management of primary small and medium vessel vasculitis. Ann Rheum Dis. 2009;68:310–7.
Acknowledgments
This study was supported by the National Key Technology Research and Development (R&D) Program of the Ministry of Science and Technology of China (No. 2011BAI10B04).
Funding
Not applicable.
Availability of supporting data
The data supporting the conclusions of this article are included within the article.
Authors’ contributions
YHC participated in the design of the study, performed the statistical analysis and wrote the manuscript. YMD helped to collect the data. ZZL helped to check the analysis. HTZ helped to check the first draft. WXH conceived of the study, participated in its design and coordination, and helped to modify the manuscript. ZHL approved the final version. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
This study was approved by the institutional review board of Jinling Hospital, Nanjing University School of Medicine, China. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional review board at our institution and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Chen, Y., Ding, Y., Liu, Z. et al. Long-term outcomes in antineutrophil cytoplasmic autoantibody–positive eosinophilic granulomatosis with polyangiitis patients with renal involvement: a retrospective study of 14 Chinese patients. BMC Nephrol 17, 101 (2016). https://doi.org/10.1186/s12882-016-0319-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12882-016-0319-2