Abstract
Background
Adequate operation interspace is the premise of laparoscopy, and carbon dioxide (CO2) was an ideal gas for forming lacuna. A retroperitoneal space is used to form operation interspace in retroperitoneal laparoscopic radical nephrectomy by making ballooning, and the retroperitoneal space has no relative complete and airtight serous membrane, therefore CO2 absorption may be greater in retroperitoneal than transperitoneal laparoscopic radical nephrectomy. Excess CO2 absorption may induce hypercapnemia and further cause physiopathological change of respiratory and circulatory system. Therefore, exact evaluation of amount of CO2 which is eliminated from body via minute ventilation is important during retroperitoneal laparoscopic radical nephrectomy. The aim of the paper is to study the correlation between CO2 storage at the last minute of gas insufflation and area of retroperitoneal lacuna during retroperitoneal laparoscopic radical nephrectomy.
Methods
Forty ASA I/II patients undergoing retroperitoneal laparoscopic radical nephrectomy were enrolled. CO2 storage at the last minute of gas insufflation and area of a retroperitoneal lacuna were observed. Linear correlation and regression were performed to determine the correlation between them.
Results
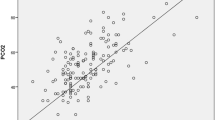
There was positive correlation between CO2 storage at the last minute of gas insufflation and area of retroperitoneal lacuna (r = 0.880, P = 0.000), and the equation of linear regression was y = −83.097 + 0.925x (R2 = 0.780, t = 11.610, P = 0.000).
Conclusions
Amount of CO2 which is eliminated from body via mechanical ventilation could be calculated by measuring the area of retroperitoneal lacuna during retroperitoneal laparoscopic radical nephrectomy, and an anesthetist should be aware of the size of lacuna to predict high CO2 storage at the last minute of gas insufflation.
Similar content being viewed by others
Background
Laparoscopic radical nephrectomy has gradually replaced conventional open nephrectomy with the improvement of operation technique and laparoscopic apparatus [1–3]. Adequate operation interspace is the premise of laparoscopy, and carbon dioxide (CO2) was an ideal gas for forming lacuna [4]. A retroperitoneal space is used to form operation interspace in retroperitoneal laparoscopic radical nephrectomy by making ballooning, and the retroperitoneal space has no relative complete and airtight serous membrane [5], therefore CO2 absorption may be greater in retroperitoneal than transperitoneal laparoscopic radical nephrectomy [6]. Excess CO2 absorption may induce hypercapnemia [7] and further cause physiopathological change of respiratory and circulatory system [8, 9]. This is harmful for patients with renal cancer because they are generally complicated with the dysfunction of critical organs. In the paper, the correlation between CO2 storage at the last minute of gas insufflation and the area of retroperitoneal lacuna in retroperitoneal laparoscopic radical nephrectomy was studied, and the aim was to evaluate exactly amount of CO2 which is eliminated from body via minute ventilation and further provide useful information for intraoperative management and mechanical ventilation strategy.
Methods
Participants
Forty ASA I/II patients between 22 and 70 years old undergoing retroperitoneal laparoscopic radical nephrectomy were enrolled in the study. All patients were treated by the same group of surgeons. Among them, 25 patients were male and 15 patients were female, and the body mass index (BMI) was 22.19 ± 0.47.
Anesthesia method
All the patients were not administered with medicine and their respiratory and circulatory functions were evaluated before operation. They received routine general anesthesia, and Electrocardiograph (ECG), blood oxygen saturation (SPO2) and blood pressure (BP) were monitored. Three arterial blood gas (ABG) samples were collected at the last minute of gas insulation, and partial pressure of carbon dioxide in artery (PaCO2) was then measured. Meanwhile, end-tidal partial pressure of carbon dioxide (PetCO2) was monitored at the corresponding time point. The mean arterial pressure and heart rate were measured before anesthesia induction, after anesthesia induction, at the time point when retroperitoneal lacuna was successfully formed, and at the end of operation.
Anesthesia was induced with propofol (2 mg/kg), fentanyl (4 ug/kg), and cisatracurium (0.2 mg/kg). After oral trachea cannula, patients underwent mechanical ventilation with a tidal volume of 8 ml/kg. PetCO2 was maintained at ≤50 mmHg by regulating respiratory frequency. Anesthesia was maintained by the method of intravenous-inhalation combined anesthesia with propofol (4–6 mg/kg∙h), sevoflurane (1.5–3 %), fentanyl (2 μg /kg∙h) and cisatracurium (0.1–0.15 mg/kg∙h).
Process of retroperitoneal lacuna formation
Jackknife position was adopted to protrude operation site after anesthesia. A retroperitoneal lacuna was formed by making ballooning with CO2 at an insufflation pressure of 12–13 mmHg for 30 min, and retroperitoneal tissues were separated gradually to get a regular triaxial ellipsoid. The surgeons were asked to try their best to make the surface of lacuna smooth.
Computing method
Computing the area of retroperitoneal lacuna
The area was generally stable after retroperitoneal lacuna was formed. The surface area of sphere was minimal at the condition of same volume, which could make the absorption of CO2 minimal. The surgeons were asked to try their best to make the surface of lacuna smooth. Therefore, the lacuna could be regarded as a triaxial ellipsoid. The surface area of lacuna could be calculated by the method of calculus after measuring the radius, which was equal to the area of CO2 absorption. The three radii of triaxial ellipsoid were simultaneously measured when designing operating field. The final formula was S = π (R2 + h2) for computing the area of retroperitoneal lacuna (Fig. 1).
Computing CO2 storage at the last minute of gas insufflation during retroperitoneal laparoscopic radical nephrectomy
CO2 storage (VCO2) at the last minute of gas insufflation was able to be calculated using the below equation.
Where PaCO2 is arterial partial pressure of carbon dioxide in kpa; VT is expired tidal volume in ml; VD is physiologic dead space in percent of tidal volume. K2 is the constant for arterial partial pressure of carbon dioxide transformed into concentration of carbon dioxide. The value of k2 is 8.16 when VA is expressed in ml and PaCO2 in kpa, on the condition of standard atmosphere pressure, 37 °C of body temperature and saturation of water vapor [10]. Physiologic dead space in percent of tidal volume (VD) is calculated in the following formula.
Where PaCO2 is arterial partial pressure of carbon dioxide in kpa and PetCO2 is end tidal partial pressure of carbon dioxide in kpa.
PaCO2 and PetCO2 were observed at the last minute of gas insufflation. Correspondently, VCO2 was computed at the time point in ml.
Statistical analysis
The statistical analyses were carried out with the SPSS version 17.0 for Windows (SPSS Inc., USA). All the variables were expressed as mean ± SD. Linear correlation and regression were performed to determine the correlation between amount of CO2 which is eliminated from body via mechanical ventilation and the area of retroperitoneal lacuna and obtain the equation of linear regression. Significance was set at P < 0.05.
Results
Retroperitoneal laparoscopic radical nephrectomy was successfully performed in all patients. The operation time ranged from 148 to 152 min with a mean of 150.12 ± 1.86, and was almost same for all patients. Subcutaneous emphysema did not occur. In addition, CO2 insufflation time and insufflation pressure were constant in the study. Therefore, the effects of operation time, subcutaneous emphysema, insufflation time and insufflation pressure on CO2 absorption were not studied in the paper. The mean arterial pressure and heart rate were not significantly different between different time points (all P > 0.05, Table 1). The results indicated that the conditions of patients were stable during the whole operation.
CO2 storage at the last minute of gas insufflation and the area of retroperitoneal lacuna were shown in Table 2. The mean of amount of CO2 which is eliminated from body via mechanical ventilation was 479.15 ± 46.71 ml for the 40 patients, the mean of the area of retroperitoneal lacuna was 686.52 ± 21.16 cm2, the mean of VT was 453.25 ± 97.91 ml, the mean of PaCO2 was 5.54 ± 0.22 kpa, and the mean of PetCO2 was 4.45 ± 0.35 kpa. The result of linear correlation showed that there was positive correlation between amount of CO2 which is eliminated from body via minute ventilation and area of retroperitoneal lacuna (r = 0.880, P = 0.000), and the equation of linear regression was y = −83.097 + 0.925x (R2 = 0.780, t = 11.610, P = 0.000).
Discussion
Retroperitoneal laparoscopic radical nephrectomy has special pathophysiologic change compared with transperitoneal laparoscopic radical nephrectomy. Firstly, retroperitoneum is a potential lacouna and has no relative complete and airtight serous membrane. Secondly, subcutaneous and connective tissue are separated during the course of establishing retroperitoneum, which makes subcutaneous capillaries torn and CO2 is then absorbed and solved easily in blood. Thirdly, retroperitoneal laparoscopic radical nephrectomy adopts Jackknife position, which can reduce the elimination of CO2. All these lead to greater CO2 absorption in retroperitoneal than transperitoneal laparoscopic radical nephrectomy. Therefore, an anesthetist should be aware of the size of lacuna to predict high amount of CO2 which is eliminated from body via mechanical ventilation.
In conclusion, we analyzed the correlation between amount of CO2 which is eliminated from body via minute ventilation and area of retroperitoneal lacuna and obtain the equation of linear regression in the paper. The result was instructive for preoperative evaluation of CO2 storage at the last minute of gas insufflation and was then helpful in determining whether open nephrectomy should be adopted or not and evaluating safety of patients.
Conclusions
Amount of CO2 which is eliminated from body via mechanical ventilation could be calculated by measuring the area of retroperitoneal lacuna in retroperitoneal laparoscopic radical nephrectomy, and an anesthetist should be aware of the size of lacuna to predict high CO2 storage at the last minute of gas insufflation.
Abbreviations
CO2, carbon dioxide; BMI, body mass index; ECG, electrocardiograph; SPO2, blood oxygen saturation; PaCO2, partial pressure of carbon dioxide in artery; PetCO2, end-tidal partial pressure of carbon dioxide; VCO2, CO2 storage; BP, blood pressure; ABG, arterial blood gas.
References
Jeon SH, Kwon TG, Rha KH, et al. Comparison of laparoscopic versus open radical nephrectomy for large renal tumors: a retrospective analysis of multi-center results. BJU Int. 2011;107(5):817–21.
Porpiglia F, Volpe A, Billia M, Scarpa RM. Laparoscopic versus open partial nephrectomy: analysis of the current literature. Eur Urol. 2008;53:732–42.
Gill IS, Schweizer D, Hobart MG, et al. Retroperitoneal laparoscopic radical nephrectomy: the Cleveland clinic experience. J Urol. 2000;163:1665–70.
Chen ZY, Wu JH, Wang YZ, et al. Effects of mechanical ventilation with lower tidal volume and positive end-expiratory pressure on pulmonary function during laparoscopic surgery in patients with chronic obstructive pulmonary disease. Chinese Journal of Anesthesiology. 2013;33(10):1229–32.
Quan R, Jing L, Jing Y, et al. Effect of one-lung ventilation on occurrence of subcutaneous emphysema in patients undergoing retroperitoneal laparoscopic urologic surgery. Chinese Journal of Anesthesiology. 2012;32(8):920–2.
Balogh A, Varga L, Julesz J, et al. Minimally invasive adrenalectomy with posterior retroperitoneoscopy. Orv Hetil. 2000;14(1):845–7.
Karagulle E, Turk E, Dogan R, et al. Effects of the application of intra-abdominal cholecystectomy on acid–base equilibrium. Int Surg. 2009;94(3):205–11.
Sharma KC, Kabinoff G, Ducheine Y, et al. Laprascopic surgery and its potential for medical complications. Heat Lung. 1997;26:52–67.
Sun JL, Zhang QL, Wang ZG, et al. Treatment of hydrocephalus by ventriculoscope or ventriculoscope associated with laparoscope. Chin J Neurosurg. 2005;21(8):84–6.
Wolf Jr JS, Monk TG, Dougall M, et al. The extraperitoneal approach and subcutaneous emphysema are associated with greater absorption of carbon dioxide during laparoscopic renal surgery. J Urol. 1995;154(2):959–63.
Acknowledgements
Not applicable.
Funding
The manuscript was supported by Scientific Research Innovation Fund of Xinjiang Medical University (contract no. XJC201260).
Availability of data and materials
The datasets supporting the conclusion of this article is included within the article.
Authors’ contributions
HJJ and LYH were responsible for collecting the data and writing the manuscript, and the two authors equally contributed to the work. JN conceived of the study, and participated in its design and coordination and helped to draft the manuscript. YCJ was responsible for analyzing the data. All authors read and approved the final manuscript.
Authors’ information
HJJ and LYH are experienced anesthetists at anesthesia department of Xinjiang Medical University Affiliated Tumor Hospital. YCJ and JN are experienced researchers at anesthesia department of Xinjiang Medical University Affiliated Tumor Hospital.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
The study was approved by the ethic committee of Xinjiang Medical University Affiliated Tumor Hospital (2012096006), and informed consent was obtained from each participant.
Disclosures
The manuscript was supported by Scientific Research Innovation Fund of Xinjiang Medical University (contract no. XJC201260). The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Hu, Jj., Liu, YH., Yu, Cj. et al. Correlation between CO2 storage at the last minute of gas insufflation and area of retroperitoneal lacuna during retroperitoneal laparoscopic radical nephrectomy. BMC Anesthesiol 16, 42 (2015). https://doi.org/10.1186/s12871-016-0208-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12871-016-0208-z