Abstract
Background
The trigeminal subnuclei interpolaris/caudalis transition zones (Vi/Vc) play an important role in orofacial deep pain, however, the role of primary afferent projections to the Vi/Vc remains to be determined. This study investigated the functional significance of hyperalgesia to the brain-derived neurotrophic factor (BDNF)-tyrosine kinase B (trkB) signaling system in trigeminal ganglion (TRG) neurons projecting to the Vi/Vc transition zone following masseter muscle (MM) inflammation.
Results
The escape threshold from mechanical stimulation applied to skin above the inflamed MM was significantly lower than in naïve rats. Fluorogold (FG) labeling was used to identify the TRG neurons innervating the MM, while microbeads (MB) were used to label neurons projecting to the Vi/Vc region. FG/MB-labeled TRG neurons were immunoreactive (IR) for BDNF and trkB. The mean number of BDNF/trkB-IR small/medium-diameter TRG neurons was significantly higher in inflamed rats than in naïve rats. In whole-cell current-clamp experiments, the majority of dissociated small-diameter TRG neurons showed a depolarization response to BDNF that was associated with spike discharge, and the concentration of BDNF that evoked a depolarizing response was significantly lower in the inflamed rats. In addition, the relative number of BDNF-induced spikes during current injection was significantly higher in inflamed rats. The BDNF-induced changes in TRG neuron excitability was abolished by tyrosine kinase inhibitor, K252a.
Conclusion
The present study provided evidence that BDNF enhances the excitability of the small-diameter TRG neurons projecting onto the Vi/Vc following MM inflammation. These findings suggest that ganglionic BDNF-trkB signaling is a therapeutic target for the treatment of trigeminal inflammatory hyperalgesia.
Similar content being viewed by others
Background
Although it is well known that the spinal trigeminal nucleus caudalis (SpVc) and the upper cervical spinal dorsal horn (C1-2) are important relay stations for trigeminal nociceptive inputs from inflammation and injury in superficial and deep tissues [1, 2], it has also been reported that the nociceptive inputs from receptors in deep craniofacial tissues are relayed to the ventral trigeminal subnucleus interpolaris/caudalis transition region (Vi/Vc) through the trigeminal subnucleus caudalis/cervical dorsal horn C2 (Vc/C2) junction region [3]. Recent studies demonstrate that orofacial injury and noxious stimulation of dental and craniofacial region activates a distinct region in the Vi/Vc transition zones [4–6]. Indeed, the injection of an N-methyl-D-aspartate (NMDA) receptor antagonist into the Vi/Vc transition zone attenuates hyperalgesia after masseter muscle (MM) inflammation [7]. Sugiyo et al. [5] demonstrated that reciprocal connections between the ventral Vi/Vc transition zone and rostral ventromedial medulla (RVM) pathways play a critical role in facilitating orofacial hyperalgesia. These findings suggest that the trigeminal Vi/Vc transition zone plays an important role in deep tissue pain processing, integrating nociceptive orofacial pain inputs and the development of persisting orofacial pain [6].
Since previous studies have demonstrated that non-synaptically-released diffusible chemical messengers, such as adenosine triphosphate (ATP), substance P (SP) and glial-derived neurotrophic factor (GDNF), act via local paracrine mechanisms in the sensory ganglia to contribute to the development of inflammation-induced sensory abnormalities [8–12], it can be assumed that transganglionic communication is one mechanism by which central sensitization can be triggered, and that suppression of ganglionic sensitization can effectively reduce the central sensitization of secondary neurons [13, 14]. Brain-derived neurotrophic factor (BDNF) facilitates pain transmission and contributes to the development of hyperalgesia [15–18] via the postsynaptic tyrosine kinase B (trkB) receptor to modulate nociceptive signaling in the spinal dorsal horn. BDNF is normally expressed in small- and medium-sized dorsal root ganglion (DRG) and trigeminal ganglion (TRG) neurons [19–21], and is localized to dense-core vesicles in axon terminals in the SpVc region [22]. Recent studies report upregulation of BDNF and trkB immunoreactivity (IR) in TRG neurons after tooth pulp inflammation or injury [23, 24]. These findings suggest that local release of BDNF from TRG neuronal somata and/or nerve terminals may regulate the excitability of TRG neurons projecting onto the Vi/Vc transition zone following deep tissue inflammation and may contribute to the development of hyperalgesia. Therefore, the present study investigated the functional significance of the BDNF-trkB signaling system in TRG neurons projecting to the Vi/Vc transition zone on trigeminal hyperalgesia following MM inflammation.
Methods
All experiments were approved by the Animal Use and Care Committee of Nippon Dental University and were consistent with the ethical guidelines of the International Association of the Study of Pain [25]. Each experiment was performed such that the experimenter was blind to experimental conditions. Every effort was made to minimize the number of animals used and their suffering.
Induction of masseter muscle inflammation
The experiments were performed on 18 adult male Wistar rats (110-150 g; naïve, n = 8; inflamed, n = 10). Each animal was anesthetized with sodium pentobarbital (45 mg/kg, i.p.), and complete Freund’s adjuvant (CFA) (0.05 ml 1:1 oil/saline suspension; inflamed rats) or vehicle (0.05 ml, 0.9% NaCl, pH 7.2; naïve rats) was injected into the left side of the MM, as described previously [26]. In some experiments (n = 2), the CFA-induced inflammation was verified with Evan’s blue dye (50 mg/ml, 1 ml/kg, i.v.) extravasation. Postmortem examination of the injected MM showed the accumulation of blue dye in the MM, indicating that the plasma protein extravasation was due to localized inflammation [10].
Double labeling of TRG neurons innervating MM and/or projecting to the Vi/Vc region
For electrophysiological and immunohistochemical studies, fluorogold (FG, Fluorochrome, Englewood, USA) and fluorescent latex microbead (MB, Lumafluor, Naples, FL) labeling methods [27] were used. Male Wistar rats were anaesthetized with pentobarbital sodium (45 mg/kg, i.p.) before FG solution (0.5% in distilled water, 10 μl) was injected into the left MM using a Hamilton syringe with a 31-gauge needle. The dorsal surface of the medulla oblongata at the obex level was then surgically exposed and MB (0.05 μl) was injected ipsilaterally into the Vi/Vc region (obex +0.5 mm, lateral 0.5 mm, depth 0.5 mm) by pressure injection through a glass micropipette (tip diameter of 30–50 μm) as described previously [5, 27–29]. After MB injection, the muscle and skin incisions were sutured and the rats were allowed to recover. The injection sites and spread of MB were verified by histology.
Mechanical threshold for escape behavior
The mechanical threshold for escape behavior was determined as described in previous studies [12]. Briefly, two days after the injection of CFA or vehicle into the MM, hyperalgesia was assessed with calibrated von Frey filaments (Semmes-Weinstein Monofilaments, North Coast Medical, CA). To evaluate the escape threshold, a set of the von Frey mechanical stimuli were applied to the skin overlying the MM in an ascending series of trials. Each von Frey stimulation was applied three times in each series of trials. The escape threshold intensity was determined when the rat moved its head away from at least one of three stimuli.
BDNF and trkB immunohistochemistry
Immunohistochemistry was used to determine whether inflammation induces BDNF and trkB expression in the trigeminal ganglia in both naïve (n = 3) and inflamed (n = 3) rats. Two days after CFA or vehicle injection rats were anesthetized (sodium pentobarbital; 50 mg/kg, intraperitoneal), and transcardially-perfused with 1% sodium nitrite in phosphate buffered saline (PBS; 50 ml) followed by Zamboni fixative (4% paraformaldehyde, 15% picric acid in 0.1 M phosphate buffer). Tissue was post-fixed for up to 2 hours. The left TRG was removed and incubated, in sequence, in 4% (5 min × 3), 10% (1 h), 20% (2 h) and 30% (overnight) sucrose solution. Sections were cut (10 μm) with a cryostat (Leica, Nussloch, Germany) and mounted on silane-coated glass slides.
Every third section was used for immunohistochemistry using a modification of the method previously described [10], with twenty sections analyzed per ganglion. Briefly, sections were incubated with sheep anti-BDNF(1:200, Millipore, CA, USA) and rabbit anti-trkB (1:1000, Millipore, CA, USA) for 24 h at 4°C, followed by Alexa Fluor® 568 donkey anti-sheep IgG (1:1000, Molecular Probes, Eugene, OR, USA) and Alexa Fluor® 647 goat anti-rabbit IgG (1:1000, Molecular Probes, Eugene, OR, USA), respectively. Labeled cryosections were rinsed in 0.01 M PBS, 5 min, and mounted with antifade medium (Molecular Probes). Control sections were incubated without the primary antibody.
The number of BDNF/trkB-IR TRG neurons was counted in each section. Immunopositive staining was compared with background staining by comparing least intense staining to that with primary antibody omitted [10]. In this study, we determine the fluorescence wave lengths of both BDNF and trkB to prevent interference. Digital images were collected and stored on a computer and analyzed with Adobe Photoshop and a Leica Imaging Analysis Tool. Confocal images were generated with a Leica TCS NT laser scanning microscope (Leica, Germany).
Acute cell dissociation and whole cell patch-clamp recording for TRG neurons
Patch-clamp recordings were conducted two days after CFA or vehicle injection, on naïve (n = 5) and inflamed rats (n = 7). Acute dissociation of TRG neurons was performed as described previously [10]. Briefly, adult rats were decapitated and the left TRG rapidly removed and incubated for 15–25 min at 37°C in modified Hank’s balanced salt solution (130 mM NaCl, 5 mM KCl, 0.3 mM KH2PO4, 4 mM NaHCO3, 0.3 mM Na2HPO4, 5.6 mM glucose, 10 mM N-2-hydroxyethylpiperazine-N’-2-ethanesulfonic acid (HEPES), pH 7.3) containing type XI collagenase (2 mg/ml; Sigma, St. Louis MO, USA) and type II collagenase (2 mg/ml; Sigma). Cells were dissociated by trituration with a fire-polished Pasteur pipette and plated onto poly-L-lysine-coated coverslips in 35 mm dishes. The plating medium contained Leibovitz’s L-15 solution (Invitrogen, Carlsbad, CA, USA) supplemented with 10% newborn calf serum, 26 mM NaHCO3 and 30 mM glucose. Cells were maintained in 5% CO2, 37°C and used for recording 2-8 h after plating. After incubation, the coverslips were transferred to the recording chamber in a standard external solution containing 155 mM NaCl, 3 mM KCl, 1 mM CaCl2, 1 mM MgCl2, 10 mM HEPES and 20 mM glucose, pH 7.3. The recording chamber (0.5 ml) was mounted onto an inverted microscope (Nikon, Tokyo, Japan) equipped with phase contrast, a video camera and two micromanipulators. The chamber was perfused under gravity with a standard external solution at approximately 0.5 ml/min.
Whole cell recordings were conducted with the rapid perforated-patch technique [10, 27]. Fire-polished patch-pipettes (2–5 MΩ) were filled with 120 mM potassium methanesulphonate, 20 mM KCl, 7.5 mM HEPES and 2 mM EGTA (ethylene glycol-bis-β-aminoethyl ether N,N,N’,N’-tetra-acetic acid), pH 7.3, containing amphotericin B (100 μg/ml). Current-clamp recordings were conducted with an Axopatch 200B amplifier (Molecular Devices, Foster City, CA, USA). Signals were low-pass filtered at 1 or 5 kHz and digitized at 10 kHz. To evaluate changes in cell membrane resistance associated with membrane potential during recordings in the current-clamp mode, negative current pulses (50–600 pA, 250 ms, 0.2 Hz) were injected through the patch pipette. Action potentials (overshoot of action potential > 0 mV) were elicited by depolarizing current pulses (10–500 pA, 10-70 pA steps, 200 ms). The threshold for action potentials was determined and defined as the minimum current required for eliciting a single spike. The tetrodotoxin (TTX) 1 μM sensitivity for TRG neurons was tested, with neurons defined as TTX-resistant (TTX-R) if no changes of spike amplitude elicited by threshold depolarizing current pulses were found in the presence of TTX [30]. The action potential firing rates were assessed by counting the number of action potentials elicited by depolarizing pulses (2-times threshold currents). Spike duration was determined as the duration of the first spike at the level of half amplitude. Access resistance was checked throughout the experiments, and no significant changes found during experiments. All recordings were performed at room temperature. Since spontaneous fluctuations in the membrane potential were less than 1 mV, a depolarizing response is defined as over 1 mV. The threshold for BDNF response (changes in the membrane potential) of each neurons tested was determined by minimum concentration of BDNF (1–100 ng/ml). After confirmation of a BDNF responsive cell, the tyrosine kinase inhibitor K252a was applied. In the current-clamp mode, the membrane potential in most cells recovered within 5–14 min.
Drug application
All drugs were stored at −20°C and stock solutions dissolved in distilled water. Drugs were subsequently dissolved in a standard external solution on the day of the experiment. BDNF (1-100 ng/ml; Sigma-Aldrich, St. Louis, MO, USA) and tyrosine kinase inhibitor K252a (10 ng/ml; Sigma-Aldrich) were added to the perfusion solution for a period of 30–60 sec.
Data analysis
Data were stored on a computer for off-line analysis (pClamp 8.0, Molecular Devices). Values are expressed as mean ± SEM. Statistical analyses were performed using Student’s te-test and one-way repeated measures analysis of variance (ANOVA) followed by the Tukey-Kramer/Dunnett’s post hoc tests for the data. P < 0.05 was considered statistically significant.
Results
Induction of MM inflammation and mechanical hyperalgesia
After CFA injection into the MM region, animals showed behavioral hyperalgesia, determined by probing the injected site (the left side) overlying orofacial skin with von Frey filaments. In inflamed rats, the threshold for escape from mechanical stimulation applied to the skin above the MM was significantly reduced one and two days after CFA injection (2 days; 46.9 ± 8.2 to 9.5 ± 3.5 g, P < 0.05; Figure 1).
Changes in the mechanical escape threshold after induction of MM inflammation and hyperalgesia. Two days after complete Freund’s adjuvant (CFA) or vehicle was injected into the skin overlying the ipsilateral MM, mechanical stimulation using von Frey filaments was applied to assess hyperalgesia in naïve and inflamed rats. Data are the mean ± SEM (naïve, n = 8; inflamed, n = 10). *P < 0.05.
Retrograde labeling of TRG neurons innervating MM and/or projecting to the Vi/Vc region
Based on our previous immunohistochemical examinations [44], TRG cell bodies were classified according to size as small (<30 μm), medium (30–39 μm) or large (>40 μm) in this study. Figure 2A shows schematic drawing of double labeling of TRG neurons and an example of FG/MB-labeled TRG neurons. In naïve rats, two days after the FG injection into the MM, 19.5% of TRG neurons (751/3850) innervating MM were retrogradely labeled by FG (Figures 2B-D), similarly to described in our previous studies [27]. Approximately half of these neurons were also labeled with the MB (44.1%, 331/751) and projected onto the Vi/Vc region (Figures 2C, 2D), similarly to as described previously [7]. These neurons ranged from small to medium in diameter (<39 μm). Similarly, in inflamed rats, 20.0% of TRG neurons innervating MM were retrogradely labeled by FG (733/3669; Figure 2E). Approximately half of these neurons ranged from small to medium in diameter, were labeled with the MB retrograde tracer (47.9%, 351/733), and projected onto the Vi/Vc region (Figure 2F, 2G).
Schematic drawing of double labeling of TRG neurons and an example of FG/MB-labeled TRG neurons. A: TRG neurons innervating the masetter muscle (MM) were labeled by fluorogold (FG) and the same neurons projecting to the trigeminal subnucleus interpolaris/caudalis transition region (Vi/Vc) were labeled by fluorescent latex microbeads (MB). Inset show the location of MB injection sites. AP, area postrema; NTS nucleus of tractus solitaries; Cu, cunate nucleus, LRN, Lateral reticular nucleus; Pyt, pyramidal tract. B-C : TRG neurons that innervated masseter muscle (MM) (B) projected onto the Vi/Vc region (C) in naïve rats. E-F: TRG neurons that innervated masseter muscle (MM) (E) projected onto the Vi/Vc region (F) in inflamed rats. B,E : Fluorescence micrograph showing FG-labeled TRG neurons. C,F : MB-labeled TRG neurons in the same section. D and G: Merge. Triangle shows an example of FG/MB-labeled TRG neurons. Bar = 20 μm.
Inflammation increases BDNF expression in FG/MB labeled TRG neurons
In both naïve and inflamed rats, the location of FG/MB-labeled BDNF-IR neuronal soma corresponded with those in the third branch of the trigeminal nerve [10, 31]. Figures 3A-G shows a typical example of FG/MB labeled BDNF-IR TRG neurons in naïve and inflamed rats. The FG/MB-labeled and BDNF-IR TRG neurons were small-medium in diameters in naïve rats (34.1%, 113/331) as described previously [21]. The size frequency of distribution of FG-/MB-labeled/BDNF-IR TRG neurons is shown in Figure 3I. The number of small-medium diameter BDNF-expressing neurons in the FG/MB-labeled TRG increased in the inflamed rat (72.9%: 256/351) compared to the naïve rat. The number of FG/MB-labeled BDNF-IR neurons was significantly higher in inflamed rats than naïve (naïve vs inflamed: 4.2 ± 0.9/section vs 8.5 ± 1.1/section, P < 0.01; Figure 3K). In the absence of primary antibody only background staining was evident (data not shown).
Difference between expression of BDNF and trkB in TRG neurons in naïve and inflamed rats. A-D : Naïve rats. FG/MB-labeled TRG neurons innervating MM ( A ) and projecting to Vi/Vc ( B ). Triangle shows an example of FG/MB-labeled and BDNF/trkB-IR TRG neurons. E-H : Inflamed rats. FG/MB-labeled TRG neurons innervating MM (C,D) ( E ) and projecting to Vi/Vc ( F ). Triangle shows an example of FG/MB-labeled and BDNF/trkB-IR TRG neurons. Bar = 20 μm. I : Size frequency distribution of FG/MB-labeled BDNF-IR TRG neurons in naïve and inflamed rats (G,H). K: Comparison of FG/MB-labeled BDNF-IR TRG neurons per section in both naïve and inflamed rats. *P < 0.05. J : Size frequency distribution of FG/MB-labeled trkB-IR TRG neurons in naïve and inflamed rats. L: Comparison of FG/MB-labeled trkB-IR TRG neurons per section in both naïve and inflamed rats.*P < 0.05.
Inflammation increases trkB expression in FG/MB-labeled TRG neurons
Similarly to the BDNF-IR TRG neurons, the location of FG/MB-labeled trkB-IR neuronal soma corresponded with those in the third branch of the trigeminal nerve. Examples of FG-/MB-labeled trkB-IR TRG neurons in naïve and inflamed rats are shown in Figures 3A, 3B, 3D and Figures 3E, 3F, 3H, respectively. The FG/MB-labeled and trkB-IR TRG neurons were small-medium in diameters in naïve rats (31%, 101/331). Importantly, the majority of FG/MB-labeled BDNF-IR neurons also expressed trkB (naïve 86%; inflamed 93%). The size frequency of distribution of FG-/MB-labeled/trkB-IR TRG neurons is shown in Figure 3J. The number of small-medium diameter trkB-expressing neurons in the FG-/MB-labeled TRG increased in the inflamed rat (66%: 226/351) compared to the naïve rat. The number of FG/MB-labeled trkB-IR neurons was significantly higher in inflamed rats than naïve rats (naïve vs inflamed: 4.6 ± 0.5/section vs 8.9 ± 1.3/section, P < 0.01; Figure 3L). In the absence of the primary antibody only background staining was evident (data not shown).
General electrophysiological properties of FG/MB-labeled TRG neurons
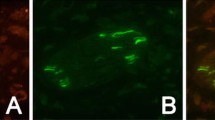
Based on the upregulation of BDNF and trkB expression in small-medium diameter TRG neurons after inflammation, and our interest in inflammatory hyperalgesia, we used small-diameter TRG neurons for the electrophysiological recordings. The isolated FG/MB-labeled TRG neurons were spherical in shape and bright in appearance with a 'halo’ around the cell body when viewed by phase contrast microscopy (Figures 4A-C). Figure 4D shows the size distribution of recorded FG/MB-labeled TRG neurons responding to 50 ng/ml BDNF (responding cell; naïve 19/36, 53%; inflamed 31/37, 84%). Since previous studies have suggested that BDNF may cause significant changes in neuronal excitability of DRG neurons [32] and Purkinje cells in the cerebellum [33], we used this concentration to test BDNF responsiveness of TRG neurons. The mean cell diameter of FG/MB-labeled TRG neurons used for electrophysiological recordings in naïve and inflamed rats was 26.5 ± 4.8 μm (n = 73). There was a tendency for the BDNF responsiveness to be greater in inflamed rats than in naïve rats. Following perforation of the cell membrane with amphotericin B in dissociated TRG neurons (naïve, n = 36; inflamed, n = 37), the series resistance dropped to below 20 MΩ (17.1 ± 5.3 MΩ, n = 73) within 3–9 min and remained stable for over 15 min. The mean cell capacitance was 15.2 ± 4.9 pF (n = 73).
Double-labeling of dissociated TRG neurons recorded under current-clamp and BDNF responsiveness in naïve and inflamed rats. Acutely dissociated TRG neurons observed under phase contrast microscopy ( A ), identified by FG-injection in the MM ( B ) and by MB injection into the Vi/Vc region in the same field (C). Bar = 20 μm. Arrow heads denote the target cell following FG/MB injection. D : Size distribution of dissociated FG/MB-labeled small-diameter TRG neurons recorded in both naïve and inflamed rats. BDNF responsiveness was determined by changes in the membrane potentials (>1 mV). E : Percentage of BDNF responsiveness in FG/MB-labeled small-diameter TRG neurons.
Effect of BDNF on the resting membrane potential of small-diameter FG/MB-labeled TRG neurons in naïve and inflamed rats
To determine whether BDNF alters the excitability of TRG neurons, the effect of BDNF on the resting membrane potential of FG/MB-labeled small-diameter TRG neurons in naïve and inflamed rats was examined. Since BDNF depolarized the majority of neurons (naïve 14/19, 74%; inflamed 26/31, 84%) and the remaining neurons were hyperpolarized after BDNF application (naïve 5/19, 27%; inflamed 5/31, 13%), in this study we focused on the depolarization response.
Figure 5A shows a typical example of the depolarizing response of FG/MB-labeled TRG neurons to BDNF (50 ng/ml) with associated decreasing input resistance, in naïve rats. The duration of the depolarizing response ranged from 4 to 8 min. Figure 5B shows a typical example of a strong depolarization response to BDNF (10 ng/ml) which induced increments in spike discharge frequency and was associated with a decrease in input resistance in inflamed rat TRG neurons. The duration of the BDNF-induced depolarizing response in inflamed rats was significantly longer than in naïve rats (naïve vs inflamed; 4.8 ± 2.2 min vs 8.6 ± 3.1 min, P < 0.05). Although relatively few neurons (3/14, 21%) in naïve rats showed spontaneous discharges, there was a two-fold increase in the number of TRG neurons (11/36, 42%) having spontaneous discharges (Figure 5C) in the inflamed rats, and the discharge rate was greater than in naïve rats (naïve vs inflamed; 0.8 ± 0.4 Hz, n = 3, vs 2.6 ± 1.1 Hz, n = 11; P < 0.05), supporting previous findings [11]. The threshold concentration of BDNF that evoked a depolarizing response in the inflamed rats was significantly lower than in naïve (naïve vs inflamed; 52.3 ± 14 ng/ml vs 12.9 ± 6.3 ng/ml; P < 0.05; Figure 5D). This depolarizing response was associated with a decrease in cell input resistance and this decreasing input resistance was significantly higher in inflamed rats than in naïve rats (naïve vs inflamed; 11.4 ± 2.3% vs 25.2 ± 5.5%; P < 0.05). BDNF-induced depolarization was significantly increased in dose-dependent manner in both naïve and inflamed rats (1–100 ng/ml) and the mean depolarization of FG/MB-labeled TRG neurons induced by BDNF in inflamed rats was significantly higher than in naïve rats (Figure 5E). The mean firing frequency of inflamed rat FG/MB-labeled TRG neurons evoked by BDNF was significantly higher than in naïve rats (Figure 5F). The mean neuronal resting membrane potential in inflamed rats was not significantly different to naïve rats (naïve vs inflamed; -55.2 ± 2.9 mV, n = 16 vs −52.1 ± 2.3 mV, n =26; NS; Figure 5F), as described in a previous study [30].
Effect of BDNF on the neuronal excitability of small-diameter FG/MB-labeled TRG neurons in naïve and inflamed rats. A : BDNF (50 ng/ml) induced neuronal depolarization with spike discharges in FG/MB labeled TRG neurons in naïve rats. The break in the trace is 5 min. B : BDNF(10 ng/ml) induced strong neuronal depolarization with spike discharges in small-diameter FG/MB labeled TRG neurons in inflamed rats. The break in the trace is 13 min. C : Spontaneous discharge in small-diameter FG/MB labeled TRG neurons in inflamed rats. The percentage and mean firing frequency of TRG exhibiting spontaneous discharges increased following inflammation. The break in the trace is 7 min. D : The threshold concentration of BDNF required for spike generation depolarization in inflamed rats was significantly lower than in naïve rats. E : Dose–response relationship for BDNF-induced depolarization in naïve and inflamed rats. (n = 4, #, p < 0.05, 1 vs 10, 50 and 100 ng/ml, *, p < 0.05, naïve vs inflamed). F : Comparison of discharge frequency induced by BDNF (50 ng/ml) in naïve and inflamed rats. *P < 0.05.
Effect of BDNF on the firing rate of small-diameter FG/MB-labeled TRG neurons in naïve and inflamed rats
To determine whether MM inflammation alters spike generation evoked by BDNF in FG/MB-labeled small-diameter TRG neurons, the changes in action potential firing rate induced by a depolarizing step pulse was examined in the absence and presence of BDNF in naïve and inflamed rats. Small-diameter FG/MB-labeled TRG neurons had several characteristics typical of nociceptors: (1) small size (<30 μm); (2) presence of long-duration action potentials [34]; and (3) resistance of the action potential to TTX [35, 36]. A typical example of the wave form of an action potential is shown in Figure 6A. In current-clamp mode, FG/MB-labeled small-diameter TRG neurons exhibited a long duration (4.3-8.8 ms) with a prominent shoulder on the repolarization phase (naïve, n = 7; inflamed, n = 10). All neurons tested exhibited action potentials in the presence of TTX (1 M; Figure 6B).
Comparison of effect of BDNF on the firing frequency of small-diameter FG/MB-labeled TRG neurons from naïve and inflamed rats. A : Wave form of action potential in response to depolarizing current pulses. Note the prominent shoulder on the falling phase (triangle). B : Action potential induced at threshold level (300 ms, 100 pA) which was resistant to TTX (1 μM). C : Action potential firing rate during depolarization of step pulse before (upper trace) and after (middle trace) BDNF (50 ng/ml), and after BDNF (50 ng/ml) + K252a (10 ng/ml; lower trace) application to small-medium diameter TRG neurons in naïve and inflamed rats. D : Threshold current for spike generation during current injection before and after BDNF and after BDNF + K252a applications; P < 0.05. E : Number of spike discharges during current injection before and after BDNF and after BDNF + K252a applications; P < 0.05. F : The relative number of spikes during current injection (100 pA, 200 ms) was significantly higher in inflamed rats than in naïve rats. *P < 0.05.
Figure 6C shows a typical example of the effect of BDNF and co-application of K252a on the spike generation during depolarizing pulses in small-diameter FG/MB-labeled TRG neurons in naïve and inflamed rats. Similarly to a previous study [30], in the present study we observed; (1) the threshold current of FG/MB-labeled TRG neurons in inflamed rats was significantly decreased compared to naïve rats (121.2 ± 12.4 pA vs 61.1 ± 8.9 pA; P < 0.05; Figure 6C, upper trace and Figure 6D); (2) the number of spike discharges during current injections by FG/MB-labeled TRG neurons in inflamed rats was significantly increased compared to naïve rats (1.2 ± 0.3 spikes vs 2.1 ± 0.2 spikes; P < 0.05; Figure 6C, upper trace and Figure 6E). In both naïve and inflamed rats, the number of spike discharges during the current injection significantly increased after BDNF (50 ng/ml) application (n = 5, P < 0.05; Figure 6C middle trace and Figure 6E). The threshold current of spike generation significantly decreased after BDNF application in both naïve and inflamed rats (n = 5, P < 0.05; Figure 6D). The relative number of spikes during current injection (100 pA, 200 ms) was significantly higher in inflamed rats than in naïve rats (355.2 ± 41.4% vs 205.3 ± 38.9%, respectively, n = 5, P < 0.05; Figure 6F). The decreased threshold current evoked by BDNF was blocked by co-administration of the tyrosine kinase inhibitor, K252a (10 ng/ml) in both naïve and inflamed rats (Figure 6C, lower trace and Figure 6D). Increased spike discharges evoked by BDNF were also blocked by co-administration of K252a (10 ng/ml) in both naïve and inflamed rats (Figure 6C, lower trace and Figure 6E).
Discussion
Inflammation upregulates BDNF/trkB expression in TRG neurons innervating MM and projecting to the Vi/Vc
By means of double-labeling tracing techniques with FG and MB, we observed that approximately half of TRG neurons identified masseteric input to ventral Vi/Vc transition zone in this study. This was consistent with the report that both masseter and cutaneous inputs to project the Vc, masseter afferents provide an addtional input to the Vi/Vc [37]. Since the location of deposits of MB was localized in the Vi/Vc region (Figure 2), it is unlikely that MB was taken up by damaged fibers that course laterally through the region and that the tracer spreads to the spinal trigeminal tract. Also, there was no significant difference in the percentage of FG/MB-labeled neurons between naïve and inflamed rats (P > 0.05). Taken together, therefore, our double-retrograde labeling methods are a valid technique for examining the primary afferent TRG neurons innervating MM and projecting to the Vi/Vc region.
BDNF is expressed in small-medium diameter DRG neurons that also express tyrosine kinase A (trkA) and calcitonin gene related peptide (CGRP). BDNF synthesized in the DRG [19, 38, 39] was transported to the central terminals of primary afferents [19, 38, 39] and released into the spinal dorsal horn, where it bound to the trkB receptors on the second order neurons to modulate painful stimuli [40–42]. Similarly, small-medium diameter TRG neurons also expressed both BDNF and trkB in naïve rats [21, 43, 44]. Furthermore, we found that most of FG/MB-labeled small-medium diameter TRG neurons co-expressed BDNF and trkB and that this expression was predominantly co-localised (naïve 86%; inflamed 93%).
BDNF and trkB mRNA levels are reported to be significantly increased in DRG neurons in a CFA inflammation model [41, 45, 46]. BDNF and trkB in small-medium diameter TRG neurons is known to be upregulated after inflammation and tooth-injury, and BDNF is released from TRG neurons in response to neuronal hyperactivity [22–24]. The inflammation-induced upregulation of BDNF is hypothesized to be mediated by NGF and hyperalgesia [41]. Peripheral inflammation and injury are also associated with the release of pro-inflammatory cytokines such as tumor necrosis factorα (TNFα) and interleukin 1β (IL-1β) [47]. Recently, Balkowiec-Iskra et al. [48] reported that TNFα upregulated BDNF expression in TRG neurons via p38-mitogen-activated protein kinase (MAP) in an 'NGF-independent manner’, leading to trigeminal hyperalgesia. This study shows that two days after CFA-induced MM inflammation, the mean number of BDNF- and trkB-IR small-medium diameter TRG neurons in inflamed rats was significantly higher than in naïve rats. Therefore, taken together, these observations suggest that both NGF and cytokine signaling may upregulate BDNF and trkB in small-medium diameter TRG neurons to induce hyperalgesia. This is also supported by a recent report that, under inflammatory conditions, enhanced production of BDNF in DRG neurons might activate presynaptic trkB receptors via an autocrine/paracrine signal to synergistically act with cytokines such as TNFα, and upregulate synaptic excitability in pain transmission [49].
Changes in the excitability of TRG neurons via upregulation of BDNF and trkB
Although we have no evidence that release of BDNF from TRG neurons into the TRGs is increased following peripheral inflammation in this study, there are reports that primary sensory neurons can release endogenous BDNF in activity-dependent manner, and that the magnitude of release dependents on the pattern and frequency of stimulation [50, 51]. Thus, it can be assumed that TRG neurons contain BDNF secrete BDNF into the extracellular space in the TRGs following neuronal excitation, resulting in an increase in BDNF concentration in the extracellular space.
Previous studies have indicated that BDNF is not only a potent neuromodulator, but also has a fast excitatory action on neurons which acutely controls resting membrane potential, neuronal excitability and synaptic transmission, and also participates in the induction of synaptic plasticity [52]. With regards to the effect of BDNF on nociceptive transmission, Matayoshi et al. [16] reported that in spinal cord slice preparations, BDNF acted on presynaptic terminals and increased the frequency of miniature excitatory post-synaptic currents (mEPSCs) of substantia gelatinosa neurons in CFA-induced inflammation via activation of receptor tyrosine kinase and TTX-sensitive (TTX-s) Na+ channels. In addition, a previous study demonstrated that acutely applied BDNF enhances the excitability of dissociated small-diameter DRG neurons via activation of the p75 neurotrophin receptor and its downstream sphingomyelin signalling cascade and increases in TTX-R Na+ currents [32].
In the present study, we observed that in inflamed rats, the threshold for escape from mechanical stimulation applied to the skin above the MM was significantly reduced two days after CFA injection, suggesting inflammatory hyperalgesia. The present study demonstrated that in dissociated FG/MB-labeled small-diameter TRG neurons; (1) there was a tendency for the BDNF responsive FG/MB-labeled small-diameter TRG neurons to be larger in inflamed rats than naïve rats; (2) the threshold concentration of BDNF that evoked a depolarizing response of neurons in the inflamed rats was significantly lower than in naïve rats; (3) BDNF induced higher frequency and longer lasting spontaneous neuronal discharges in inflamed rats; (4) The relative number of BDNF-induced TTX-R neuronal spikes during current injection was significantly higher in inflamed rats; (5) The BDNF-induced changes in the TTX-R neuron excitability was abolished by K252a. Thus, these findings suggest that BDNF released from small-diameter TRG neurons upregulates trkB through an paracrine/autocrine mechanism, increasing spontaneous activity and triggering the release of chemical neuromodulators (CGRP, SP and ATP) which act on the neighboring neurons or satellite glial cells via a similar mechanism [8–11, 53].
BDNF binds to two structurally unrelated plasma membrane receptor types, the p75 neurotrophin receptor and the tyrosine kinase receptor trkB [54]. Activation of trkB by BDNF triggers intracellular signaling cascades that effectively modulate voltage-gated, ligand-gated and second-messenger gated ion channels [52, 55]. Cao et al. [8] report that paracrine released BDNF and trkB receptor activation enhanced the excitability of DRG neurons in diabetic neuropathy through voltage-gated A-type potassium channels. In this study we observed that a BDNF-induced depolarizing response was associated with a decrease in cell input resistance. This decreased input resistance in inflamed rats was significantly higher than in naïve rats. The present study shows that BDNF-induced depolarization and increased firing frequency in the TRG neuron excitability was abolished by the tyrosine kinase inhibitor K252a. Since voltage-gated potassium channels determine the resting membrane potential of neurons and regulate their excitability [56], it can be speculated that BDNF-induced increases in the excitability of FG/MB-labeled small-diameter TRG neurons may be due to the depression of voltage-gated potassium currents. This is supported by the following studies; (1) inhibition of voltage-gated potassium currents by somatostatin, interleukin 1β and GDNF in a small-diameter TRG neurons potentiates neuronal excitability, thereby contributing to trigeminal inflammatory hyperalgesia [27, 53, 57]; (2) BDNF enhances the excitability of small-diameter DRG neurons via activation of p75 neurotrophin receptor and suppression of delayed rectifier-like potassium currents [38]. (3) BDNF significantly affects auditory brainstem neuronal excitability via a decrease in the potassium channels [58]. Although the precise ionic mechanism for BDNF-induced enhanced TRG neuronal excitability is unclear, we hypothesise that BDNF/trkB signaling induces hyperexcitability of the small-diameter TRG neurons via a depression of voltage-gated potassium currents within trigeminal ganglia. Further studies are required to fully elucidate the underlying ion mechanisms between BDNF/trkB signaling and TRG neuronal excitability, including other ion channels.
Functional significance of BDNF/trkB signaling in the trigeminal ganglia and inflammatory hyperalgesia
BDNF-trkB signaling within the RVM descending pathways has been reported to contribute to the net descending facilitation of synaptic transmission in the Vi/Vc and pain hypersensitivity [18, 59]. In addition, inflamed MM primary afferent inputs onto the Vi/Vc region are necessary and sufficient to induce astroglial hyperactivity, concomitant IL-1β induction, and coupling of neuronal NMDA receptor phosphorylation through IL-1β signaling [37]. Thus it can be postulated that modulations of both synaptic transmission in the Vi/Vc and the descending facilitation pathway from the RVM are potential therapeutic targets for the treatment of persisting orofacial pain.
Several reports have demonstrated the functional significance of transganglionic signal communication [8–11, 60–62], and we have previously suggested that sensory signals are effectively amplified or attenuated downstream of the ascending sensory pathway and then sent to higher centers. Thus, transganglionic communication, including neuron-satellite glial cell interaction, is one mechanism by which central sensitization can be triggered [53]. We recently provided evidence that in the early stages of CFA inflammation, suppression of the SP/neurokinin-1 receptor mechanism in trigeminal ganglia may prevent central sensitization of hyperexcitability of SpVc wide-dynamic range nociceptive neurons [14]. Taken together, our reports suggest that blocking ganglionic sensitization can effectively reduce the central sensitization of nociceptive neurons and/or neuron-glial interactions in the Vi/Vc transition zone. Therefore, in addition to BDNF/trkB signaling in the central nervous system, the local paracrine mechanism of BDNF/trkB on TRG neurons provides a novel therapeutic target for the treatment of debilitating orofacial deep inflammatory pain.
Conclusion
The present study provided evidence that BDNF enhances the excitability of the small-diameter TRG neurons projecting onto the Vi/Vc following MM inflammation. These findings suggest that ganglionic BDNF-trkB signaling is a therapeutic target for the treatment of trigeminal inflammatory hyperalgesia.
Abbreviations
- SpVc:
-
Spinal trigeminal nucleus caudalis
- C1-2:
-
Upper cervical spinal dorsal horn
- Vi/Vc:
-
Trigeminal subnuclei interpolaris/caudalis transition zones
- BDNF:
-
Brain-derived neurotrophic factor
- trkB:
-
Tyrosine kinase B
- TRG:
-
Trigeminal ganglion
- MM:
-
Masseter muscle
- FG:
-
Fluorogold
- MB:
-
Microbeads
- IR:
-
Immunoreactive
- NMDA:
-
N-methyl-D-aspartate
- RVM:
-
Rostral ventromedial medulla
- ATP:
-
Adenosine triphosphate
- SP:
-
Substance P
- GDNF:
-
Glial-derived neurotrophic factor
- DRG:
-
Dorsal root ganglion
- CFA:
-
Freund’s adjuvant
- PBS:
-
Phosphate buffered saline
- EDTA:
-
Ethylene diaminetetra acetic acid
- HEPES:
-
N-2-hydroxyethylpiperazine-N’-2-ethanesulfonic acid
- EGTA:
-
Ethylene glycol-bis-β-aminoethyl ether N,N,N’,N’-tetra acetic acid
- TTX:
-
Tetrodotoxin
- TTX-s:
-
TTX-sensitive
- TTX-r:
-
TTX-resistant
- ANOVA:
-
Analysis of variance
- trkA:
-
Tyrosine kinase A
- CGRP:
-
Calcitonin gene related peptide
- TNFα:
-
Tumor necrosis factor α
- IL-1β:
-
Interleukin 1β
- MAP:
-
Mitogen-activated protein kinase
- mEPSCs:
-
Miniature excitatory post-synaptic currents.
References
Bereiter DA, Bereiter DF: Morphine and NMDA receptor antagonism reduce c-fos expression in spinal trigeminal nucleus produced by acute injury to TMJ region. Pain 2000, 85: 65–77. 10.1016/S0304-3959(99)00246-8
Sessle BJ: Acute and chronic craniofacial pain: brainstem mechanisms of nociceptive transmission and neuroplasticity and their clinical correlates. Crit Rev Oral Biol Med 2000, 11: 57–91. 10.1177/10454411000110010401
Bereiter DA, Shen S, Benetti AP: Sex differences in amino acid release from rostral trigeminal subnucleus caudalis after acute injury to the TMJ region. Pain 2002, 98: 89–99. 10.1016/S0304-3959(01)00476-6
Imbe H, Dubner R, Ren K: Masseteric inflammation-induced Fos protein expression in the trigeminal interpolaris/caudalis transition zone: contribution of somatosensory-vagal-adrenal integration. Brain Res 1999, 845: 165–175. 10.1016/S0006-8993(99)01913-7
Sugiyo S, Takemura M, Dubner R, Ren K: Trigeminal transition zone/rostral ventral medial medulla connections and facilitation of orofacial hyperalgesia after masseter muscle inflammation in rats. J Comp Neurol 2005, 493: 510–523. 10.1002/cne.20797
Ren K, Dubner R: The role of trigeminal interpolaris-caudalis transition zone in persistent orofacial pain. Int Rev Neurobiol 2011, 97: 207–225.
Wang H, Wei F, Dubner R, Ren K: Selective distribution and function of primary afferent nociceptive inputs from deep muscle tissue to the brain stem trigeminal transition zone. J Comp Neurol 2006, 498: 390–402. 10.1002/cne.21062
Amir R, Devor M: Chemically mediated cross-excitation in rat dorsal root ganglia. J Neurosci 1996, 16: 4733–4741.
Matsuka Y, Neubert JK, Maidment NT, Spigelman I: Concurrent release of ATP and substance P within guinea pig trigeminal ganglia in vivo. Brain Res 2001, 915: 248–255. 10.1016/S0006-8993(01)02888-8
Takeda M, Tanimoto T, Ikeda M, Nasu M, Kadoi J, Shima Y, Ohta H, Matsumoto S: Temporomandibular joint inflammation potentiates the excitability of trigeminal root ganglion neurons innervating the facial skin in rats. J Neurophysiol 2005, 93: 2723–2738. 10.1152/jn.00631.2004
Takeda M, Tanimoto T, Nasu M, Ikeda M, Kadoi J, Matsumoto S: Activation of NK1 receptor of trigeminal root ganglion via substance P paracrine mechanism contributes to the mechanical allodynia in the temporomandibular joint inflammation in rats. Pain 2005., 116:
Takeda M, Takahashi M, Hara N, Matsumoto S: Glial cell line-derived Neurotrophic factor modulates the excitability of nociceptive trigeminal ganglion neurons via a paracrine mechanism following inflammation. Brain Behav Immun 2013, 28: 100–107. 375–385
Takeda M, Takahashi M, Matsumoto S: Contribution of activation of satellite glia in sensory ganglia to pathological pain. Neurosci Biobehav Rev 2009, 33: 784–792. 10.1016/j.neubiorev.2008.12.005
Takeda M, Takahashi M, Matsumoto S: Suppression of neurokinin-1 receptor in trigeminal ganglia attenuates central sensitization following inflammation. J Peripher Nev Syst 2012, 17: 169–181. 10.1111/j.1529-8027.2012.00404.x
Pezet S, Malcangio M, McMahorn SB: BDNF: a neuromodulator in nociceptive pathways ? Brain Res Rev 2002, 40: 240–249. 10.1016/S0165-0173(02)00206-0
Matayoshi S, Jiang N, Katafuchi T, Koga K, Furue H, Yasaka T, Nakatsuka T, Zhou XF, Kawasaki Y, Tanaka N, Yoshimura M: Actions of brain-derived Neurotrophic factor on spinal nociceptive transmission during inflammation in the rat. J Physiol 2005, 569: 685–695. 10.1113/jphysiol.2005.095331
Obata K, Noguchi K: BDNF in sensory neurons and chronic pain. Neurosci Res 2006, 55: 1–10. 10.1016/j.neures.2006.01.005
Ren K, Dubner R: Pain facilitation and activity-dependent plasticity in pain modulatory circuitry: role of BDNF-trkB signaling and NMDA receptors. Mol Neurobiol 2007, 35: 224–235. 10.1007/s12035-007-0028-8
Zhou XF, Rush RA: Endogenous brain-derived Neurotrophic factor is anterogradely transported primary sensory neurons. Neuroscience 1996, 74: 945–953.
Thompson SW, Bennett DL, Ker BJ, Bradbury EJ, McMahon SB: Brain-derived Neurotrophic factor is an endogenous modulator of nociceptive responses in the spinal cord. Proc Natl Acad Sci USA 1999, 96: 7714–7718. 10.1073/pnas.96.14.7714
Wetmore C, Olson L: Neuronal and nonneuronal expression of neurotrophins and their receptor in sensory and sympathetic ganglia suggest new intracellular trophic interactions. J Comp Neurol 1995, 353: 143–159. 10.1002/cne.903530113
Buldyrev T, Tanner NM, Hsieh HY, Dodd EG, Nguyen LT, Balkowiec A: Calcitonin gene-related peptide enhances release of native brain derived neurotorophic factor from trigeminal ganglion neurons. J Neurochem 2006, 99: 1338–1350. 10.1111/j.1471-4159.2006.04161.x
Behnia A, Zhang L, Charles M, Gold MS: Changes in trkB-like immunoreactivity in rat trigeminal ganglion after tooth injury. J Endo 2003, 29: 135–140. 10.1097/00004770-200302000-00012
Tarsa L, Balkowiec-Iskra E, Kratochvil FJ 3rd, Jenkins VK, McLean A, Brown A, Smith JA, Baumgartner JC, Balkowiec A: Tooth pulp inflammation increases brain-derived Neurotrophic factor expression in rodent trigeminal ganglion neurons. Neuroscience 2010, 167: 1205–1215. 10.1016/j.neuroscience.2010.03.002
Zimmermann M: Ethical guidelines for investigations of experimental pain in conscious animals. Pain 1983, 16: 109–110. 10.1016/0304-3959(83)90201-4
Takeda M, Tanimoto T, Ito M, Nasu M, Matsumoto S: Role of capsaicin-sensitive primary afferent inputs from the masseter muscle in the C 1 spinal neurons responding to tooth-pulp stimulation in rats. Exp Brain Res 2005, 160: 107–117. 10.1007/s00221-004-1990-2
Takeda M, Kadoi J, Takahashi M, Nasy M, Matsumoto S: Somatostatin inhibits the excitability of rat small-diameter trigeminal ganglion neurons that innervate nasal mucosa and project to upper cervical dorsal horn via activation of Somatostatin 2a receptor. Neuroscience 2007, 148: 744–756. 10.1016/j.neuroscience.2007.06.048
Phillips JK, Goodchild AK, Dubey R, Sesiashvili E, Takeda M, Chalmers PM, Pilowsky PM, Lipski J: Differential expression of catecholamine biosynthetic enzymes in the rat ventrolateral medulla. J Comp Neurol 2001, 431: 20–34.
Paxinos G, Watson C: The Rat brain in stereotaxic coordinates, compact. 6th edition. Sydney: Academic; 2009.
Takeda M, Tanimoto T, Ikeda M, Nasu M, Kadoi J, Yoshida S, Matsumoto S: Enhanced excitability of rat trigeminal root ganglion neurons via decrease in a-type potassium currents following temporomandibular joint inflammation. Neuroscience 2006, 138: 621–630. 10.1016/j.neuroscience.2005.11.024
Greg JM, Dixon AD: Somatotopic organization of the trigeminal ganglion in the rat. Arch Oral Biol 1993, 18: 487–498.
Zhang YH, Chi XX, Nicol GD: Brain derived Neurotrophic factor enhances the excitability of rat sensory neurons through activation of the p75 neurotrophin receptor and the sphingomyelin pathway. J Physiol 2008, 586: 3113–3127. 10.1113/jphysiol.2008.152439
Drake-Baumann R: Rapid modulation of inhibitory synaptic currents in cerebellar purkinje cells by BDNF. Synapse 2005, 57: 183–190. 10.1002/syn.20170
Waddell PJ, Lawson SN: Electrophysiological properties of subpopulations of rat dorsal root ganglion neurons in vitro. Neuroscience 1990, 1036: 811–822.
Ritter AM, Mendell LM: Somal membrane properties of physiologically identified sensory neurons in the rat: effects of nerve growth factor. J Neurophysiol 1992, 68: 2033–2041.
Moore BA, Stewart TMR, Hill C, Vanner SJ: TNBS ileitis evokes hyperexcitability and changes in ionic membrane properties of nociceptive DRG neurons. Am J Physiol Gastrointest Liver Physiol 2002, 282: G1045-G1051.
Wang H, Guo W, Yang K, Wei F, Dubner R, Ren K: Contribution of primary afferent input to trigeminal astroglial hyperactivity, cytokine induction and NMDA receptor phosphorylation. Open Pain J 2010, 3: 144–152.
Michael GJ, Averill S, Nitkunan A, Rattray M, Bennett DL, Yan Q, Priestley JV: Nerve growth factor treatment increases brain-derived Neurotrophic factor selectively in trkA-expressing dorsal root ganglion cells and in their central termination within the spinal cord. J Neurosci 1997, 17: 8476–8490.
Li WP, Xian C, Rush RA, Zhou XF: Upregulation of brain-derived Neurotrophic factor and Neuropeptide Y in the dorsal ascending sensory pathway following sciatic nerve injury in rat. Neurosci Lett 1999, 260: 49–52. 10.1016/S0304-3940(98)00958-6
Kafitz KW, Rose CR, Thoenen H, Konnerth A: Neurotrophin-evoked rapid excitation through trkB receptor. Nature 1999, 401: 918–921. 10.1038/44847
Mannion RJ, Costigan M, Decosterd I, Amaya F, Ma QP, Holstege JC, Ji RR, Acheson A, Lindsay RM, Wilkinson GA, Woolf CJ: Neurotrophins: peripherally and centrally acting modulators of tactile stimulus induced inflammatory pain hypersensitivity. Proc Natl Acad Sci USA 1999, 96: 9385–9390. 10.1073/pnas.96.16.9385
Lever IJ, Bradbury EJ, Cunningham JR, Adelson DW, Jones MG, Mc Mahon SB, Marvizon JC, Malcangio M: Brain-derived Neurotrophic factor is released in the dorsal horn by distinctive patterns of afferent fiber stimulation. J Neurosci 2001, 21: 4469–4477.
Gunjigake KK, Got T, Nakano K, Konoo T, Kobayashi S, Yamaguchi K: Correlation between the appearance of neuropeptides in the rat trigeminal ganglion and reinnervation of healing root socket tooth extraction. Acta Histochem 2006, 39: 69–77.
Ichikawa H, Yabuuchi T, Jin HW, Terayama R, Yamaai T, Deguchi T, Kamioka H, Takani-Yamamoto T, Sugimoto T: Brain-derived Neurotrophic factor-immunoreactive primary sensory neurons in the trigeminal ganglion and trigeminal sensory nucleus. Brain Res 2006, 1081: 113–118. 10.1016/j.brainres.2006.01.027
Lee SL, Kim JK, Kim DS, Cho HJ: Expression of mRNAs encoding full-length and truncated TrkB receptors in rat dorsal root ganglia and spinal cord following peripheral inflammation. Neuroreport 1999, 9: 2847–2851.
Cho HJ, Kim SY, Park MJ, Kin DS, Kim JK, Chu MY: Expression of mRNA for brain-derived Neurotrophic factor in the dorsal root ganglion following peripheral inflammation. Brain Res 1997, 749: 358–362. 10.1016/S0006-8993(97)00048-6
Watkins LR, Maier SF: Beyond neurons: evidence that immune and glial cells contribute to pathological pain states. Physiol Rev 2001, 82: 981–1011.
Balkowiec-Iskra E, Vermehren-Schmadeick A, Balkowiec A: Tumor necrosis factor -α increases brain-deribed Neurotrophic factor expression in trigeminal ganglion neurons in an activity-dependent manner. Neuroscience 2011, 180: 322–333.
Lin YT, Ro LS, Wang HL, Chen JC: Upregulation of dorsal root ganglia BDNF and trkB receptor in inflammatory pain: an in vivo and in vitro study. J Neuroinflammation 2011, 8: 126. 10.1186/1742-2094-8-126
Balkowiec A, Katz DM: Activity-dependent release of endogenous brain-deribed Neurotrophic factor from primary sensory neurons detected by Elisa in situ . J Neurosci 2000, 20: 7417–7423.
Trueta C, De-Miguel FF: Extrasynaptic exocytosis and its mechanism: a source of molecules mediating volume transmission in the nervous system. Front Physiol 2012, 3: 319.
Rose CR, Blum R, Kafitz KW, Kovalchuk Y: Konnerth: from modulator to mediator: rapid effects of BDNF on ion channels. Bioassays 2004, 26: 1185–1194. 10.1002/bies.20118
Takeda M, Kitagawa J, Takahashi M, Iwata K, Mastsumoto S: Glial cell line-derived Neurotrophic factor acutely modulates the excitability of rat small-diameter trigeminal ganglion neurons innervating facial skin. Brain Behav Immun 2010, 24: 72–82. 10.1016/j.bbi.2009.08.002
Chao MV: Neurotrophins and their receptors: a convergence point for many signaling pathways. Nat Neurosci 2003, 4: 299–309.
Cao XH, Byum HS, Chen SR, Cai YQ, Pan HL: Reduction in voltage-gated K+ channel activity in primary sensory neurons in painful diabetic neuropathy: role of brain derived Neurotrophic factor. J Neurochemistry 2010, 114: 1460–1475.
Hille B: Potassium channels and chloride channels. In Ion channels of excitable membranes. 3rd edition. Edited by: Hille B. Sunderland, Massachusetts: Sinauer Associates; 2001:134–167.
Takeda M, Kitagawa J, Takahashi M, Mastsumoto S: Activation of interleukin-1β receptor suppresses the voltage-gated potassium currents in the small-diameter trigeminal ganglion neurons following peripheral inflammation. Pain 2008, 139: 594–602. 10.1016/j.pain.2008.06.015
Yossoufian M, Walmsley B: Brain-derived Neurotrophic factor modulates cell excitability in the mouse medial nucleus of trapezoid body. Eur J Neurosci 2007, 25: 1647–1652. 10.1111/j.1460-9568.2007.05428.x
Guo W, Robbins MT, We F, Zou S, Dubner R, Ren K: Supraspinal brain-derived Neurotrophic factor signaling: a novel mechanism for descending pain facilitation. J Neurosci 2006, 26: 126–137. 10.1523/JNEUROSCI.3686-05.2006
Devor M, Wall PD: Cross-excitation in dorsal root ganglia of nerve-injured and intact rats. J Neurophysiol 1990, 64: 1733–1746.
Utzschneider D, Kocsis J, Devor M: Mutual excitation among dorsal root ganglion neurons in the rat. Neurosci Lett 1992, 146: 53–56. 10.1016/0304-3940(92)90170-C
Oh EJ, Weinreich D: Chemical communication between vagal afferent somata in nodose ganglia of the rat and guinea pig in vitro. J Neurophysiol 2001, 2001(87):2801–2807.
Acknowledgements
This study was supported by a Grant in-Aid for Scientific research from the Japanese Society for Promotion of Science No.24592819.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
MT (CA) participated in the design of study, carried out the experiment and wrote the manuscript. MT and JK carried out retrograde-labeling and the electrophysiological experiment. TK and MN carried out the immunohistochemical experiment. SM provided data interpretation and helped to finalize the manuscript. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Takeda, M., Takahashi, M., Kitagawa, J. et al. Brain-derived neurotrophic factor enhances the excitability of small-diameter trigeminal ganglion neurons projecting to the trigeminal nucleus interpolaris/caudalis transition zone following masseter muscle inflammation. Mol Pain 9, 49 (2013). https://doi.org/10.1186/1744-8069-9-49
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1744-8069-9-49