Abstract
Background
Bilateral emphysematous pyelonephritis is a life threatening condition usually occurring in diabetics. Management of this condition has traditionally been aggressive and surgery is considered mandatory. However, this is itself a hazardous intervention in a septic, unstable patient with circulatory or liver failure. When bilateral disease is present, the need for long-term dialysis is obviously unavoidable.
Case presentation
We herein report one of the few cases of bilateral emphysematous pyelonephritis successfully managed by non-surgical treatment.
Similar content being viewed by others
Background
Emphysematous pyelonephritis (EPN) is a rare, life-threatening condition, usually occurring in diabetic patients [1]. Patients with emphysematous pyelonephritis are typically very ill with circulatory/liver failure caused by sepsis. In most cases, a normal native kidney is involved unilaterally, but in 10% of cases, the condition is bilateral [2]. Management of this condition has traditionally been aggressive and surgery has been considered mandatory. Many of the earlier series have stressed the very high mortality rate (75%) and the need for urgent nephrectomy [3–6]. However, this is itself a hazardous intervention in a septic patient with unstable circulatory or liver failure. In the case of bilateral renal disease, the patient requires long-term dialysis. With the advent of CT scanning, more powerful antibiotics, and better access to life support, an alternative medical approach to radical surgery has emerged [7].
Here we report one of the few cases of bilateral empysematous pyelonephritis successfully managed by non-surgical treatment.
Case report
A 41-year-old non-insulin dependent diabetic female with transverse myelitis was referred after a 7-day history of fever, generalized malaise, vomiting, increasing breathlessness and oliguria. She was a type 2 diabetic (onset 14 year before), requiring insulin for glucose control. She had been treated with high dose of steroids for transverse myelitis.
Upon admission, the patient appeared confused and obtunded, was febrile (39.0 C), tachycardic (110 beats/min) and hypotensive (90/60 mm Hg). She was conscious but not completely oriented in time and space. Cardiac and respiratory examinations were unremarkable.
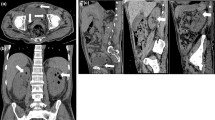
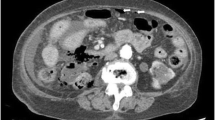
Relevant laboratory data were as follows: glucose 31.5 mmol/L, urea of 89 mmol/L, creatinine of 168 μmol/L, sodium of 133 mmol/L, and potassium of 5.2 mmol/L. Her hemoglobin was 7.7 g/dL, hematocrit 24 %, total peripheral white cell count of 17700 with a shift to the left, and a platelet count of 20 000 (Table 1). Arterial blood gases showed high anion gap metabolic acidosis. Initial ultrasound showed bilateral enlarged edematous kidneys. An abdominal computed tomography (CT) scan showed diffusely enlarged kidneys, with perinephric edema, extensive gas in the renal tissues and perinephric areas bilaterally (Figure 1). She was treated with intravenous fluids, ceftriaxone and amikacin.
Because of persistent high fever, hypotension, an increase in the total peripheral white cell count and worsening renal function (Table 1) the patient was transferred to the intensive care unit on day two and was treated with intravenous fluids, a tritrated insulin infusion, ceftriaxone, amikacin and inotropic support with dopamine. On review by the urologists, it was thought that conservative management should be attempted given the absence of obstruction of the urinary tract. Blood and urine cultures grew Escherichia Coli senstive to amikacin and ceftiraxone as well as ciprofloxacin.
The patient' s clinical condition improved remarkably over the fourth day of treatment, thus obviating the need for surgery.
A Follow-up CT scan obtained 7 days after the initial study showed global improvement with marked reduction of the gas within the kidneys and a decrease in perinephric edema.
Two weeks after admission to the hospital, during which time she made a steady clinical recovery, her antibiotic was switched to oral ciprofloxacin and fluconazole and was sent home 15 days after admission with a serum creatinine concentration of 124 μmol/L (Table 1). A CT scan on discharge showed complete resolution of the renal emphysema.
Upon further review she is clinically well and free of infection.
Conclusions
First described in 1898, emphysematous pyelonephritis (EPN) is an acute necrotizing parenchymal and perirenal infection caused by gas forming uropathogens [8–10]. Four factors appear to be involved in the pathogenesis of EPN: gas-forming bacteria, high tissue glucose, impaired tissue perfusion and a defective immune response [11]. Diabetics account for 70–90% of all cases [9, 12].
The organisms most commonly associated with EPN are E. Coli, Klebsiella pneumoniae, Proteus mirabilis, Pseudomonas aeruginosa, Aerobacter aerogenes, Citrobacter and rarely yeast. Left untreated, EPN is uniformly fatal [13].
Estimates of mortality using current therapy range from 10% to 40% with patients treated medically having a higher mortality than those treated surgically, 70% versus 30%, respectively [8, 9, 12, 14]. Thus, traditionally, it is thought that antibiotic therapy alone is usually ineffective, and prompt nephrectomy is necessary [12].
In a previous report of 48 cases of EPN patients were classified in four classes according to CT findings, from class 1(the mildest) to class 4 (the most severe form) [15]. Ninety-six per cent (96%) had diabetes mellitus with 22% also having urinary obstruction. The mortality rate in those receiving antibiotics alone was 40% (2 of 5). The success rate of those treated with percutaneous catheter drainage (PCD) plus antibiotics (27 of 41) was 66% and those who had nephrectomy was 90% (9 of the 10 patients). In EPN class 1 and 2, all the patients who were treated with PCD plus antibiotics survived. In extensive EPN (classes 3 and 4), 85% (17 of 20) were successfully treated with PCD and antibiotics. Eight of the 14 who had an unsuccessful treatment using a PCD underwent nephrectomy, seven of whom survived.
Hui reported a case of EPN treated with nephrectomy and stated that based on available data, surgical intervention appears to be the preferred treatment [16]. Chen et al described 10-year experience with 25 EPN patients [17]. Eighty per cent (80%) required antibiotics plus PCD only; 12% underwent nephrectomy and 8% died. Shokeir reviewed their 15-year experience of 20 patients with EPN in Egypt [18]. He emphasized that immediate nephrectomy, as soon as the patient is medically stable, should not be delayed.
Goldsmith [19], Kondo [20], Labussiere [21, 22], Punnose [22], Jain [23], and Best [24] all have described individual cases of EPN treated successfully with antibiotics alone.
Angulo [25], Grozel [26], Shimizu [27] and Tahir [19] et.al. Each reported cases of bilateral EPN that were successfully treated with antibiotics alone, thus obviating the need for renal replacement therapy which would have been needed if they were treated with bilateral nephrectomies.
We believe that nephrectomy is not the preferred treatment anymore for all cases of emphysematous pyelonephritis. EPN shall be classified into grades of severity and treatment planned accordingly. Although difficult to perform because of the rarity of EPN, randomized controlled studies for management of EPN are greatly needed.
Authors contributions
Author 1 GF, participated in medical treatment throughout the entire hospitalization and wrote and drafted manuscript. Author 2HN, participated in medical treament in the ICU and drafted the manuscript also. Authors 3 and 4, JC and FM are third and fourth year residents of internal medicine and participated in medical treatment and diagnosis. All authors read and approved the final manuscript.
Abbreviations
- EPN:
-
Emphysematous pyelonephritis
References
Costas S: Renal and perirenal emphysema. BJU. 1972, 44: 311-9.
Zabbo A, Montie JL, Popowniak KL, et al: Bilateral emphysematous pyelonephritis. Urology. 1985, 25: 293-6.
Ahlering TE, Boyd SD, Hamilton CL, et al: Emphysematous pyelonephritis: a 5-year experience with 13 patients. J Urol. 1985, 134: 1086-8.
Ballanger P, Petit J, Thomas G, Tauzin-Fin P: La pyelonephrite emphysemateuse. Revue de la litterature a propos de quatre nouveaux cas. Ann Urol (Paris). 1986, 20: 195-200.
Dunn SR, Dewolf WC, Gonzalez R: Emphysematous pyelonephritis: report of 3 cases treated by nephrectomy. J Urol. 1975, 114: 348-50.
Picron B, Mauerhoff T, Farchakh E, et al: Pyelonephrite emphysemateuse (P.N.E.) chez une patiente diabetique. Revue de la litterature a propos d'un cas. Acta Clin Belg. 1991, 46: 94-9.
Campbell's Urology Walsh, Patrick C 7th ed Cloth Text. 1997
Ouellet LM, Brook MP: Emphysematous pyelonephritis: an emergency indication for the plain abdominal radiograph. Ann Emerg Med. 1988, 17: 722-4.
Evanoff GV, Thompson CS, Foley R, et al: Spectrum of gas within the kidney. Emphysematous pyelonephritis and emphysematous pyelitis. Am J Med. 1987, 83: 149-54.
Michaeli J, Mogle P, Perlberg S, et al: Emphysematous pyelonephritis. J Urol. 1984, 131: 203-8.
Chen KW, Huang JJ, Wu MH, et al: Gas in hepatic veins: a rare and critical presentation of emphysematous pyelonephritis. J Urol. 1994, 151: 125-6.
Cook DJ, Achong MR, Dobranowski J: Emphysematous pyelonephritis. Complicated urinary tract infection in diabetes. Diabetes Care. 1989, 12: 229-32.
Andersen JB: Pyelonephritis emphysematosa. En alvorlig komplikation til diabetes mellitus. Ugeskr Laeger. 1992, 154: 1419-21.
Joris L, van Daele G, Timmermans U, et al: Emphysematous pyelonephritis. Intensive Care Med. 1989, 15: 206-8.
Huang JJ, Tseng CC: Emphysematous pyelonephritis: clinicoradiological classification, management, prognosis, and pathogenesis. Arch Intern Med. 2000, 160: 797-805. 10.1001/archinte.160.6.797.
Hui L, Tokeshi J: Emphysematous pyelonephritis. Hawaii Med J. 2000, 59: 336-7.
Chen MT, Huang CN, Chou YH, et al: Percutaneous drainage in the treatment of emphysematous pyelonephritis: 10-year experience. J Urol. 1997, 157: 1569-73. 10.1097/00005392-199705000-00008.
Shokeir AA, El-Azab M, Mohsen T, et al: Emphysematous pyelonephritis: a 15-year experience with 20 cases. Urology. 1997, 49: 343-6. 10.1016/S0090-4295(96)00501-8.
Tahir H, Thomas G, Sheerin N, et al: Successful medical treatment of acute bilateral emphysematous pyelonephritis. Am J Kidney Dis. 2000, 36: 1267-70.
Kondo T, Okuda H, Suzuki M, et al: [A case of emphysematous pyelonephritis improved with conservative therapy–indication for conservative therapy]. Hinyokika Kiyo. 2000, 46: 335-8.
Labussiere AS, Gazaigne J, Walker P, Laplace M: Pyelonephrite emphysemateuse. Un cas traite medicalement. J Urol (Paris). 1996, 102: 127-9.
Punnose J, Yahya TM, Premchandran JS, et al: Emphysematous pyelonephritis responding to medical therapy. Int J Clin Pract. 1997, 51: 468-70.
Jain SK, Agarwal N, Chaturvedi SK: Emphysematous pyelonephritis: a rare presentation. J Postgrad Med. 2000, 46: 31-2.
Best CD, Terris MK, Tacker JR, et al: Clinical and radiological findings in patients with gas forming renal abscess treated conservatively. J Urol. 1999, 162: 1273-6. 10.1097/00005392-199910000-00007.
Angulo JC, Dehaini A, Escribano J, et al: Successful conservative management of emphysematous pyelonephritis, bilateral or in a solitary kidney. Scand J Urol Nephrol. 1997, 31: 193-7.
Grozel F, Berthezene Y, Guerin C, et al: Bilateral emphysematous pyelonephritis resolving to medical therapy: demonstration by US and CT. Eur Radiol. 1997, 7: 844-6. 10.1007/s003300050216.
Shimizu H, Hariu K, Kamiyama Y, et al: Bilateral emphysematous pyelonephritis with autosomal-dominant polycystic kidney disease successfully treated by conservative method. Urol Int. 1999, 63: 252-4. 10.1159/000030462.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2369/3/4/prepub
Acknowledgements
Written consent was obtained from the patient's relatives for publication of the study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
None declared.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Flores, G., Nellen, H., Magaña, F. et al. Acute bilateral emphysematous pyelonephritis successfully managed by medical therapy alone: A case report and review of the literature. BMC Nephrol 3, 4 (2002). https://doi.org/10.1186/1471-2369-3-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2369-3-4