Abstract
Background
In Australia in June 2001, a unique pneumococcal vaccine schedule commenced for Indigenous infants; seven-valent pneumococcal conjugate vaccine (7PCV) given at 2, 4, and 6 months of age and 23-valent pneumococcal polysaccharide vaccine (23PPV) at 18 months of age. This study presents carriage serotypes following this schedule.
Methods
We conducted cross sectional surveys of pneumococcal carriage in Aboriginal children 0 to 6 years of age living in remote Aboriginal communities (RACs) in 2003 and 2005. Nasal secretions were collected and processed according to published methods.
Results
902 children (mean age 25 months) living in 29 communities in 2003 and 818 children (mean age 35 months) in 17 communities in 2005 were enrolled. 87% children in 2003 and 96% in 2005 had received two or more doses of 7PCV. From 2003 to 2005, pneumococcal carriage was reduced from 82% to 76% and reductions were apparent in all age groups; 7PCV-type carriage was reduced from 11% to 8%, and 23PPV-non-7PCV-type carriage from 31% to 25% respectively. Thus non-23PPV-type carriage increased from 57% to 67%. All these changes were statistically significant, as were changes for some specific serotypes. Shifts could not be attributed to vaccination alone. The top 10 of 40 serotypes identified were (in descending order) 16F, 19A, 11A, 6C, 23B, 19F, 6A, 35B, 6B, 10A and 35B. Carriage of penicillin non-susceptible (MIC > = 0.12 μg/mL) strains (15% overall) was detected in serotypes (descending order) 19A, 19F, 6B, 16F, 11A, 9V, 23B, and in 4 additional serotypes. Carriage of azithromycin resistant (MIC > = 2 μg/mL) strains (5% overall), was detected in serotypes (descending order) 23B, 17F, 9N, 6B, 6A, 11A, 23F, and in 10 additional serotypes including 6C.
Conclusion
Pneumococcal carriage remains high (~80%) in this vaccinated population. Uptake of both pneumococcal vaccines increased, and carriage was reduced between 2003 and 2005. Predominant serotypes in combined years were 16F, 19A, 11A, 6C and 23B. Antimicrobial non-susceptibility was detected in these and 17 additional serotypes. Shifts in serotype-specific carriage suggest a need more research to clarify the association between pneumococcal vaccination and carriage at the serotype level.
Similar content being viewed by others
Background
Australian Aboriginal children in remote communities experience high rates of many infectious diseases[1, 2], particularly pneumococcal disease.[3] Concern about antibiotic resistance is used as an argument against greater use of antibiotics. Recent reports describe escalating rates of disease caused by pneumococcal serotypes not included in currently licensed pneumococcal conjugate vaccine (7PCV),[3, 4]including an increasing proportion of isolates having antibiotic resistance. [5–7] Serotype 19A is of particular interest in Australia[3] and internationally.[8] More recent data suggests 6C as a new and emerging replacement serotype, and that 7PCV is cross-protective for 6A. Prior to 7PCV introduction in 2001,[9] pneumococcal carriage in Indigenous infants was around 80% and approximately 60% were 7PCV serotypes (unpublished data from 3 of the communities also in these surveys). In 2003 and 2005 we conducted wider geographic surveillance of pneumococcal carriage.
Methods
Vaccine schedule
From July 2001 7PCV was recommended and funded for Australian Aboriginal and other high-risk infants at 2, 4 and 6 months of age. In the Northern Territory and in South Australia, 23-valent pneumococcal polysaccharide vaccine (23PPV) was recommended as a booster dose for Aboriginal children at 18 months of age.[9] Children less than 2 years of age were offered catch-up 7PCV.
Study setting and participant eligibility criteria
Participating communities were in four regions of South Australia and the Northern Territory. Children were eligible if they were Aboriginal, 0 to 6 years of age, resident in a participating community, and if their parents or caregiver provided written consent.
Swab collection, antibiotic use and vaccination history
Nasal secretions were collected using swabs or nose blowing into a tissue as previously described.[10, 11] Pneumococcal vaccination dates and antibiotics prescribed in the 5 weeks prior to swab collection were obtained from the NT childhood immunization register and participant medical records.
Microbiological analysis
Nasal secretions were transported, stored and processed as previously described.[10] Pneumococci were identified and one or more colonies (if morphologically distinct) selected for serotyping with antisera from the Statens Serum Institute (Denmark). Antimicrobial susceptibility was determined by disc diffusion[12] and Etest (AB Biodisk, Sweden). We performed PCR for the wciN gene.[13]
Statistical analysis
Confidence intervals (CI, 95%) and risk differences (RD, with 95% CI) were calculated where appropriate. Stata version 10 was used for all data analysis[14]
Ethical Approval and Funding
The study was approved by the regional Human Research Ethics Committees and Aboriginal Sub-Committee with right of veto of the Northern Territory Department of Health and Community Services and Menzies School of Health Research. The study was funded by the National Health and Medical Research Council.
Results
Participant characteristics
Nasal secretions were collected from 902 children in 29 communities in 2003 and from 818 children in 17 communities in 2005 (Table 1). Nasal swabs comprised 94% specimens. Mean age was 30 months. 83 were less than 6 months of age.
Vaccine uptake
In 2003 87% children had received at least 2 doses of 7PCV (Table 2). In 2005, this figure was 96% (Risk Difference = 9% [95% Confidence Interval 7,12]). The proportion of children receiving a full primary 7PCV plus booster 23PPV course increased from 35% to 62% (RD = 27% [22,31]) (Tables 2 and 3). 169 children had no record of receiving either 7PCV or 23PPV. Ten children had 23PPV only. Of the 83 infants less than 6 months of age, 59 (71%) had received at least one dose of 7PCV.
Carriage
Pneumococcal carriage in 2003 and 2005 combined was 79%. There was no difference in pneumococcal recovery between nasal swab (79%) and nose blowing (80%) collection methods. Pneumococcal carriage declined overall from 82% in 2003 to 76% in 2005 (RD = -6% [-10, -2] p = 0.0037), and similar reductions were seen in all age groups (Table 2). However this was not seen in all regions (Table 3).
Carriage in children seen in both surveys
Of the 226 children seen in both surveys, 80% were positive each year, and 148 (65%) were carriage positive in both 2003 and 2005; only 11 carried the same serotype.
Carriage in communities seen only in 2003
In the 12 communities seen only in 2003, 106 (82%) of 130 children were carriage positive, 5% carried azithromycin resistant strains (MIC > = 2 μg/mL) and 23% carried penicillin non-susceptible strains (MIC > = 0.12 μg/mL). Carriage and resistance in the other 17 communities seen in 2003 was 82%, 5% and 17%, respectively.
Serotype-specific carriage
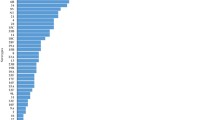
7PCV-type carriage was 11% in 2003 and 8% in 2005 (RD = -4% [-6, -0.1] p = 0.0105) (Table 2). 23PPV -non-7PCV-type carriage was 42% in 2003 and 33% in 2005 (RD = -6% [-10,-2] p = 0.0061]). Reductions reached statistical significance for serotypes 6B and 19A. Non-23PPV-type carriage increased overall (RD = 9% [CI 5,14] p = 0.0001) and reached statistically significance for non-vaccine types 23B, 23A, 34 and 10F, and for 23PPV types 20 and 9N. Of the isolates serotyped, the predominant carriage serotypes were 16F(14%), 19A(13%), and 11A (6.5%) and 6C (6%) (see Figure 1).
Non-vaccinated children
In 2003 and 2005, carriage in 169 non-vaccinated children (no 7PCV or 23PPV) was 74% and 70% respectively; carriage of 7PCV types was 9% and 7%, 23PPV-non-7PCV types was 19% and 24%. Predominant serotypes were 16F(10%) and 19A(9%) followed by 6% each of 11A, 6C, 23B and 22F.
Infants less than 6 months of age
Carriage in 83 infants less than 6 months of age was 83% in 2003 and 74% in 2005 (RD = -10% [-28, 8]). Carriage of 7PCV types was 20% and 4%, respectively (RD = -16% [-31, -1]). Predominant serotypes were 19A(17%), 16F(14%), 6A(8%) and 11A(8%) followed by 6B, 15C and 22F.
Non-vaccinated infants less than 6 months of age
For 24 non-vaccinated infants less than 6 months of age (mean age 1.9 months), carriage was 43% (3/7) and 65% (11/17) in 2003 and 2005, respectively (RD = 22% [-21, 65]). The 2003 serotypes were 6B, 11A and 20. The 2005 serotypes were 6A and 6C(2) and one each of 10F, 11A, 13, 18A, 19A, 19F, 33F, 34, and 22F.
23PPV vaccinated children
Although carriage of 23PPV-non-7PCV types declined from 2003 to 2005, this could not be explained by the rise in 23PPV uptake. For both years combined, among children more than 18 months of age, carriage of 23PPV-non-7PCV types was 30% in 23PPV-vaccinated children compared to 26% in non-vaccinated children (RD = 4% [-2,10]). This difference was statistically significant in 2003 (RD = 11% [3, 19]), but not in 2005 (RD = -1% [-12,9]). At the serotype level, these trends were present for serotype 19A but did not reach statistical significance.
Antibiotic use in the 5 weeks prior to swab collection
Beta-lactam antibiotics had been recently prescribed (within 5 weeks prior to swabbing) for 14% children in 2003 and for 16% in 2005 (Tables 2 and 3). In general, macrolides were rarely recently prescribed with the exception of 48 of 396 (13%) children the Darwin Rural region (Table 3). Of these 48 children, 45 were from one community and had been prescribed azithromycin for trachoma eradication.
Antibiotic resistance
Carriage of penicillin non-susceptible pneumococci (MIC ≥ 0.12 μg/mL) was 17% in 2003 and 14% in 2005 (Table 2). In Central Australia where prescribing was highest, carriage was 25% in 2003 and 42% in 2005 (Table 3). Penicillin resistance of 1.0 μg/mL or more was found in six children from 3 communities, all were serotype 9 V. Azithromycin resistant pneumococci (MIC ≥ 2 μg/mL) were carried by 5% children in 2003 and 6% in 2005. In the community where mass azithromycin had been recently used, 6 of 45 (13%) children with a record of recently prescribed azithromycin carried an azithromycin-resistant strain compared to 5 of 70 (7%) children with no record of recently prescribed azithromycin (RD = 6% [-5, 18]).
Antibiotic-resistant serotypes
Penicillin resistance (MIC> = 0.12 μg/mL) was found in both 7PCV and non-7PCV serotypes (Figure 2). In 2003, 34% of 137 resistant isolates were serotype 19A and in 2005, 26% (of 112 isolates) were 19A. Of 24 resistant isolates in Central Australia in 2005 9 (38%) were serotype 19A. Serotype 16F accounted for 7% in 2003 and 19% in 2005.
Proportion of children with nasopharyngeal carriage of pneumococcal serotypes and antimicrobial non-susceptible serotypes, 7PCV and 23PPV serotype group. A: 2003. B: 2005. Serogroups: Left – 7PCV serotypes. Middle – 23PPV serotypes. Right – non-23PPV serotypes. MacR (yellow): azithromycin MIC ≥ 2 μg/mL. PenR (mauve): penicillin MIC ≥ 0.12 μg/mL. Strains with resistance to both beta-lactam and macrolide antibiotics were included in each category. (in 2003 six of 38 6B isolates, two of 25 23Bs and one of 50 11As; in 2005 one of 39 23B isolates and one of 37 11As.)
Macrolide resistance (azithromycin MIC ≥ 2 μg/mL) was found mainly in the non-7PCV serotypes (Figure 2). Eight isolates with MIC > = 256 μg/mL were found in 6 communities in regions 1 and 2 in 2003. Serotypes were 16F(2) and 6B(6).
Discussion
Our survey of 1720 young children in remote communities two and four years after commencement of a government funded schedule for Indigenous children of 7PCV at 2, 4 and 6 months followed by a booster 23PPV at 18 months of age, provides a valuable source of pneumococcal serotype and susceptibility data for the region. Two major influences have had the potential to impact on pneumococcal carriage in this population; pneumococcal vaccination and antimicrobial prescribing. In three communities studied extensively in the 1990s, around 50% children carried 7PCV serotypes. Predominant pre-7PCV serotypes were 6B, 19F, 23F, 19A, 16F and 6A (unpublished data from 3 of the communities also in these surveys). Retrospective PCR analysis confirms one of 20 pre-7PCV 6A isolates was 6C.[15] A similar serotype distribution was found in cultures of discharge from acute perforations of the tympanic membrane.[16]
In general, this survey found small differences between 2003 and 2005. Vaccine uptake (at least 2 doses of 7PCV) was around 87% in 2003 and increased to 96% in 2005. By 2005, 84% age-eligible children had received 23PPV. Between 2003 and 2005 we detected small but statistically significant reductions in pneumococcal carriage (-6%). This trend was consistent across all age groups. Similarly for 7PCV types (-4%). There was a small reduction in 6A. Overall, carriage of 23PPV-non-7PCV types was significantly reduced (-5%), including serotype 19A (-4%), but other 23PPV-non-7PCV types (20 and 9N) increased. Non-vaccine serotypes (not in 23PPV) increased by 10%, mainly attributable to serotypes 23B, 34 and 10F. Serotypes 6C and 16F remained unchanged.
Among the group of children not vaccinated, 19A, 16F and 6A and 6C were the predominant serotypes and 7PCV type carriage was less than 10%, indicating a herd effect. Similarly, in very young non-vaccinated infants (mean age 1.9 months) carriage was around 58% and only 8% carried 7PCV vaccine types. Serotypes were diverse and no dominant emerging serotype was evident in this young group.
There is no strong evidence from 23PPV studies to suggest that 23PPV has an impact on NP carriage[17] Our immunogenicity study[18] showed 23PPV to be an effective booster for 7PCV-primed serotypes, and that modest responses to some additional serotypes in 23PPV also occurred. Whether the antibody concentrations achieved would prevent pneumococcal acquisition in the nasopharynx was not assessed. In this survey we did detect a 5% reduction in 23PPV-non-7PCV serotype carriage between 2003 and 2005, at a time when uptake of 23PPV as a booster dose increased from 35% to 62%. In the age group eligible for 23PPV booster, carriage of serotypes unique to 23PPV was actually higher in 23PPV-vaccinated than non-vaccinated children, but only in 2003. We are unable to explain this observation which was not present in 2005. Whether this is related to lack of effect of 23PPV on carriage, or timing of the swabbing in relation to 23PPV vaccination, or other factors cannot be assessed from this study. Further studies of 23PPV seem warranted as is large-scale surveillance of 23PPV-non-7PCV serotypes in this population.
Beta-lactam prescribing did not change significantly between 2003 and 2005, however the region with highest prescribing also had higher carriage of penicillin non-susceptible strains. Serotypes 19A and 16F accounted for a considerable proportion of beta-lactam- non-susceptible strains, as did remaining 7PCV serotypes. The finding that penicillin non-susceptibility is linked to the major endemic replacement serotypes indicates a need for ongoing monitoring to assess trends over coming years. High level penicillin resistance was very uncommon in 2005 (1 isolate). The clinical impact of penicillin resistance will be much greater if high level resistance increases over time. In the 2008 report by Roche[3], serotype 19A caused the majority (36%) of penicillin non-susceptible IPD cases in Australia in 2006.
Macrolide prescribing was low, but increased significantly between 2003 and 2005, mainly due to recent mass azithromycin use in one community. At the time of our survey in that community there was no statistically significant difference in pneumococcal carriage or carriage of azithromycin resistant strains between children recently prescribed azithromycin and those not (RD = 6% [-5, 18]). Our previous longitudinal study[19] had shown that azithromycin reduces carriage of pneumococci, providing resistant strains with a selective advantage that allows spread within the community. Over time, and in the absence of further azithromycin use or selective pressure, susceptible stains re-populate and the proportion of the population carrying resistant strains declines.[19] The present cross-sectional study does not capture this dynamic process and therefore does not allow any conclusions regarding the relationship between mass azithromycin use and carriage. In Central Australia, recent macrolide prescribing was rare, but carriage of azithromycin resistant strains was clearly higher than other regions. We suggest that this higher background of resistance may be related to a longer period of exposure to azithromycin for trachoma[20] and STI (sexually transmitted infection)[21] eradication programs, in the central Australian region. Data to support this are lacking; the 2006 Trachoma surveillance report identified that azithromycin treatment was recommended but was poorly documented in the Northern Territory[20]
Whilst carriage prevalence does not fully predict IPD serotypes (particularly outbreak or epidemic serotypes such as serotypes 1 or 5), the majority of annual IPD cases are caused by the serotypes most prevalent in the carriage population. In Australia, rates of IPD caused by serotype 19A in Indigenous children have fluctuated over recent years and serotype 6A became the most common non-vaccine IPD serotype in Indigenous children and the second most common in non-Indigenous children.[3] Hanna[22] compared IPD serotypes in under 5 year old Indigenous children living in far North Queensland pre- and post-7PCV implementation. They concluded that there was no evidence of non-7PCV serotype replacement. However, the pre-vaccine non-7PCV cases were inflated by a serotype 1 outbreak. Excluding type 1 cases, there was a risk difference in non-7PCV IPD of 55% [95%CI 30,80]. Reporting of pneumococcal epidemiology needs to consider the epidemic and endemic nature of various serotypes and that serotype-specific data are needed to best describe and prepare for shifts over time and in response to vaccines and antibiotic selective pressures.
Otitis media (OM) serotypes closely align with carriage serotype profile,[23] and for Aboriginal children OM is a common and serious infection often resulting in chronic suppurative OM (CSOM). This study showed that the serotypes colonising infants at 2 months of age, and therefore the serotypes most likely causing early OM,[24] are no longer 7PCV-types. Vaccines that are effective in preventing early onset of ear disease (and pneumonia) are urgently needed.
Conclusion
Pneumococcal disease epidemiology is in a transition period in Australia. This surveillance shows that nasal carriage of 7PCV serotypes has been replaced by the serotypes that were the next most common carriage serotypes prior to 7PCV use – namely 19A and 16F. Antibiotic resistance is almost exclusively restricted to these serotypes (and remaining 7PCV serotypes) and requires monitoring at the regional level. The role of 23PPV in limiting carriage and preventing disease in children also needs further investigation. More work is needed to guide design of appropriate surveillance systems that measure serotype shifts and distinguish serotype replacement from secular trends.
References
Rothstein J, Heazlewood R, Fraser M: Health of Aboriginal and Torres Strait Islander children in remote Far North Queensland: findings of the Paediatric Outreach Service. Med J Aust. 2007, 186: 519-521.
Clucas DB, Carville KS, Connors C, Currie BJ, Carapetis JR, Andrews RM: Disease burden and health-care clinic attendances for young children in remote aboriginal communities of northern Australia. Bull World Health Organ. 2008, 86: 275-281. 10.2471/BLT.07.043034.
Roche P, Krause V, Cook H: Invasive pneumococcal disease in Australia, 2006. Communicable Diseases Intelligence. 2008, 32 (1): 18-30.
Singleton RJ, Hennessy TW, Bulkow LR, Hammitt LL, Zulz T, Hurlburt DA, et al: Invasive pneumococcal disease caused by nonvaccine serotypes among alaska native children with high levels of 7-valent pneumococcal conjugate vaccine coverage. JAMA. 2007, 297: 1784-1792. 10.1001/jama.297.16.1784.
Farrell DJP, Klugman KPM, Pichichero MM: Increased Antimicrobial Resistance Among Nonvaccine Serotypes of Streptococcus pneumoniae in the Pediatric Population After the Introduction of 7-Valent Pneumococcal Vaccine in the United States. [Article]. Pediatric Infectious Disease Journal. 2007, 26: 123-128. 10.1097/01.inf.0000253059.84602.c3.
Hanage WP, Huang SS, Lipsitch M, Bishop CJ, Godoy D, Pelton SI, et al: Diversity and Antibiotic Resistance among Nonvaccine Serotypes of Streptococcus pneumoniae Carriage Isolates in the Post-Heptavalent Conjugate Vaccine Era. J Infect Dis. 2007, 195: 347-352. 10.1086/510249.
Pai R, Moore MR, Pilishvili T, Gertz RE, Whitney CG, Beall B: Postvaccine genetic structure of Streptococcus pneumoniae serotype 19A from children in the United States. Infect Immun. 2005, 192: 1988-1995.
Moore MR, Gertz RE, Woodbury RL, Barkocy-Gallagher GA, Schaffner W, Lexau C, et al: Population snapshot of emergent Streptococcus pneumoniae serotype 19A in the United States. J Infect Dis. 2008, 197: 1016-1027. 10.1086/528996.
Australian Immunisation Handbook. 8th Edition 2003. 2007, 220-234.
Leach AJ, Stubbs E, Hare K, Beissbarth J, Morris PS: Comparison of nasal swabs with nose blowing for community-based pneumococcal surveillance in healthy children. J Clin Microbiol. 2008, 46: 2081-2082. 10.1128/JCM.00048-08.
Stubbs E, Hare K, Wilson C, Morris P, Leach AJ: Streptococcus pneumoniae and noncapsular Haemophilus influenzae nasal carriage and hand contamination in children: a comparison of two populations at risk of otitis media. Pediatr Infect Dis J. 2005, 24: 423-428. 10.1097/01.inf.0000160945.87356.ca.
Bell SM: The CDS disc method of antibiotic sensitivity testing (calibrated dichotomous sensitivity test). Pathology. 1975, 7 (Suppl-48):
Park IH, Pritchard DG, Cartee R, Brandao A, Brandileone MC, Nahm MH: Discovery of a new capsular serotype (6C) within serogroup 6 of Streptococcus pneumoniae. J Clin Microbiol. 2007, 45: 1225-1233. 10.1128/JCM.02199-06.
StataCorp: 2008, Stata Statistical Software: Release 10.0. College Station, Texas. Stata Corporation
Hare KM, Smith-Vaughan HC, Binks M, Park IH, Nahm MH, Leach AJ, 'Dodgy 6As': Differentiating pneumococcal serotype 6C from 6A using the Quellung reaction. J Clin Microbiol. 2009, 47 (6): 1981-1982. 10.1128/JCM.00046-09.
Leach AJ: Microbiology of acute otitis media with perforation in Indigenous children. Streptococci – New insights into an Old Enemy Proceedings of the XVIth Lancefield International Symposium on Streptococci and Streptococcal Diseases Ed Kadaba S Sriprakash. 2006, 89-92.
Moberley S, Mulholland EK, Leach AJ, Morris PS, Carapetis JR, Balloch A, et al: Maternal and infant antibody following pneumococcal vaccination during pregnancy.
Leach AJ, Morris PS, Mackenzie G, McDonnell J, Balloch A, Carapetis J, et al: Immunogenicity for 16 serotypes of a unique schedule of pneumococcal vaccines in a high-risk population. Vaccine. 2008, 26: 3885-3891. 10.1016/j.vaccine.2008.05.012.
Leach AJ, Shelby-James TM, Mayo M, Gratten M, Laming AC, Currie BJ, et al: A prospective study of the impact of community-based azithromycin treatment of trachoma on carriage and resistance of Streptococcus pneumoniae. Clin Infect Dis. 1997, 24: 356-362.
Tellis B, Keeffe JE, Taylor HR: Surveillance report for active trachoma, 2006: National Trachoma Surveillance and Reporting Unit. Commun Dis Intell. 2007, 31: 366-374.
Bowden FJ, Fethers K: "Let's not talk about sex": reconsidering the public health approach to sexually transmissible infections in remote Indigenous populations in Australia. Med J Aust. 2008, 188: 182-184.
Hanna J, Humphreys JL, Murphy DM: Invasive pneumococcal disease in Indigenous people in north Queensland: an update, 2005–2007. MJA. 2008, 189: 43-46.
Leach AJ, Morris PS: The burden and outcome of respiratory tract infection in Australian and Aboriginal children. Pediatr Infect Dis J. 2007, 26: S4-S7. 10.1097/INF.0b013e318154b238.
Leach AJ, Boswell JB, Asche V, Nienhuys TG, Mathews JD: Bacterial colonization of the nasopharynx predicts very early onset and persistence of otitis media in Australian aboriginal infants. Pediatr Infect Dis J. 1994, 13: 983-989.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2334/9/121/prepub
Acknowledgements
The authors thank the many Indigenous children and their families who consented to be in this study. Financial Support was from the National Health and Medical Research Council of Australia which had no role in the study design, analysis, interpretation or decision to submit for publication.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
AL, PM & HSV conceived of the study, participated in its design, securing funding and coordination and helped to draft the manuscript. GM and CW managed participant recruitment and specimen collection. LS coordinated laboratory studies. KH conducted bacteriology and pneumococcal serotyping. JB assisted with the bacteriology and database management. SJ assisted with the statistical analysis. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Leach, A.J., Morris, P.S., McCallum, G.B. et al. Emerging pneumococcal carriage serotypes in a high-risk population receiving universal 7-valent pneumococcal conjugate vaccine and 23-valent polysaccharide vaccine since 2001. BMC Infect Dis 9, 121 (2009). https://doi.org/10.1186/1471-2334-9-121
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2334-9-121