Abstract
Background
This study characterised the effects of persistent peripheral inflammation of the foot on pain and spinal cord expression of cyclooxygenase-1 and -2 (COX-1 and COX-2) and early growth response gene 1 (Egr-1), known markers of neuronal plasticity, in a clinical model of naturally-occurring inflammatory disease and hyperalgesia in sheep ('footrot'), before and after routine treatment (parenteral treatment with antibiotics and antiseptic footbathing). The temporal pattern of expression of COX-1, COX-2 and Egr-1 mRNA and protein were analysed using real-time PCR and Western blotting.
Results
Animals affected with persistent peripheral inflammation displayed significant hyperalgesia and lameness (a proxy indicator of spontaneous pain) restricted to the inflamed limb. Hyperalgesia and lameness were significantly attenuated 1 day after treatment, and resolved further by day 7 and day 3, respectively. COX-2 but not COX-1, protein expression was up-regulated in spinal cord from lame animals on day 0, before treatment. Following treatment and attenuation of pain behaviours, levels of COX-2 returned to control levels. Significant induction of Egr-1 mRNA and protein were observed in spinal cord from lame animals. Three days after treatment, levels of Egr-1 mRNA returned to control levels, however, Egr-1 protein remained elevated.
Conclusion
Elevated levels of spinal COX-2 and Egr-1 protein correlate with the presence of pain and hyperalgesia, and may underlie persistent pain, although a direct causal link has still to be established. Understanding the temporal pattern of expression of key mediators in clinical pain states may lead to better strategies to manage pain.
Similar content being viewed by others
Background
While experimental models of inflammatory pain have helped increase our understanding of pain mechanisms, they are sometimes limited in addressing the diverse nature of clinical pain, focussing more on short-term cellular and molecular changes. Furthermore, they do not represent the heterogeneity of clinical pain states. The present study utilized a model of naturally-occurring persistent inflammation, pain and hyperalgesia in sheep, induced by a bacterial infection of the digital tissues of the feet of ruminants, known as 'footrot' [1, 2]. 'Footrot' is a painful, chronic disease of sheep, where the anaerobic bacterium Dichelobacter nodosus is the primary pathogen [3]. 'Footrot' induces inflammation of the digital skin and underlying tissues, and typically extends abaxially to cause separation and under-run lesions of the keratin matrix of the hoof. Footrot is considered an economically significant disease, and to have an adverse effect on animal welfare. Both body weight and wool production are adversely affected during the clinical phase of the infection [4]. Hyperalgesia has been documented in sheep with footrot [2, 5] and studies have identified alterations in a number of pain-related genes in spinal cord recovered from these animals [2].
Prostaglandins (PGs), released by the action of cyclooxygenases (COX-1 and COX-2) on arachidonic acid, contribute to spinal nociception and hyperalgesia [6–9]. COX-2 is the major source of PGs in inflammatory pain, and the target for COX-2 selective non-steroidal anti-inflammatory drugs (commonly known as coxibs). COX-2 is induced in spinal cord in response to a variety of inflammatory stimuli [7, 10–15], and is associated with the central component of hyperalgesia [16], and as such, may prove to be a useful marker of spinal cord plasticity underlying persistent hyperalgesia.
The transcription factor, early growth response gene 1 (Egr-1) also known as zif268, Krox-24 and NGFI-A, is also regulated by neuronal activity, and is generally considered a model system to study synaptic plasticity [17, 18]. Egr-1 expression increases during long-term potentiation (LTP) [19, 20], and is required for encoding long-lasting memories (see review by Davis et al. [18]). Egr-1 is rapidly induced in spinal cord in response to sensory fibre stimulation [20–22] and following peripheral inflammation [23–27], suggesting a role for Egr-1 regulated target gene expression and persistent cell modifications in spinal cord neuronal plasticity and persistence of pain. Evidence that Egr-1 induction is dependent on NMDA receptor activation [27, 28], and increased intracellular Ca2+ concentration (see review by Thiel et al. [29]), both triggers of activity-dependent central sensitization [30] support this hypothesis.
This study was designed to characterise the effects of long-lasting clinical inflammation on pain behaviours and spinal cord nociceptive information processing while monitoring established markers of central neuronal plasticity, COX-2 and Egr-1, to determine the effectiveness of treatment on resolution of these behaviours. Results show that COX-2 and Egr-1 mRNA and protein expression in spinal cord correlate with the presence of pain and hyperalgesia, suggesting that these mediators, and their downstream targets, contribute to pain related plasticity in spinal cord pathways.
Results
Resolution of hyperalgesia after treatment
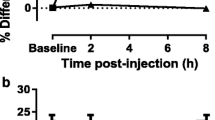
In healthy control animals, there was no significant difference in mechanical withdrawal threshold recorded from all four legs for the duration of the study (Figure 1b). Prior to treatment, sheep affected by unilateral lameness had reduced response thresholds to mechanical stimulation in the lame limb compared to non-affected limbs and control animal limb thresholds (Figure 1b). Sheep affected by unilateral lameness displayed significant hyperalgesia (p < 0.001 vs. control sheep) on day 0 prior to treatment, which was attenuated 1 day following treatment (p < 0.001 vs. day 0), and fully resolved by day 7 after treatment (p < 0.01 vs. day 0), when thresholds were similar to those observed in control animals. Data collected from each lame sheep are presented in Table 1.
Resolution of lameness and hyperalgesia after treatment. Photograph of a clinically lame animal and close-up of the hindfeet (a). The animal was given a lameness score of 10 (non-weight bearing). Inflammation can be seen in the right foot and tracking up the lower limb. The magnitude of hyperalgesia (Emax%) on the lame limb on day 0 prior to treatment, and up to 7 days post-treatment is represented as the percentage change from 3 non-affected limbs according to the formula: ((mean response threshold of non-affected limbs - response threshold of lame limb)/mean response threshold of non-affected limbs) × 100. In control animals, the mean percentage change in response threshold measured on one limb relative to the three other limbs was calculated (b). Mean lameness score for animals affected by unilateral lameness on day 0 prior to treatment for lameness, and up to 7 days post-treatment (c). Data are presented as mean values; s.e.d. represents the standard error of the difference. a, b, c Means with disparate letters are significantly different (p < 0.05).
Lameness Scores
On day 0 prior to treatment, mean lameness scores were 6.6 ± 0.3 in sheep affected by unilateral lameness (Table 1). There was a significant (p < 0.001 vs. day 0) decrease in lameness scores just 1 day following treatment, followed by a further significant (p < 0.001 vs. day 0) decrease in lameness 3 days post-treatment. No further resolution in lameness was observed, and some animals remained mildly lame at day 7 (1.8 ± 0.5; Figure 1c).
Foot Pathology
On day 0 prior to treatment, the median pathology score was 4 (range 2-4); by day 3 the median score had dropped significantly (p < 0.01) to 2.5 (range 0-4), although, in 5 out of the 18 sheep examined there was no noticeable improvement in foot condition. No further improvement in foot pathology was observed by 7 days (median score 2 (range 0 - 4)).
Lymph Node Pathology
In control animals, left and right lymph nodes were of approximately equal size (2.0 ± 0.2 g and 1.9 ± 0.2 g, respectively; Figure 2b). In contrast, the ipsilateral lymph nodes obtained from lame animals prior to treatment (7.2 ± 0.8 g) were significantly enlarged (p < 0.001) compared to the contralateral nodes (2.9 ± 0.4 g) and compared to control sheep lymph nodes. Lymph nodes collected from animals on day 3 after treatment were still significantly enlarged (13.5 ± 2.1 g) compared to contralateral nodes (2.4 ± 0.2 g) and compared to control sheep lymph nodes.
Lymph node hyperplasia in infected sheep. Photograph of popliteal lymph nodes ipsilateral and contralateral to inflamed limb collected from a clinically lame animal (a). Mean lymph node size (each lymph node represented as proportion (%) of combined weight) in control animals (left and right prescapular and popliteal lymph nodes) and animals affected by unilateral hindlimb (popliteal lymph nodes) and forelimb (prescapular lymph nodes) lameness on day 0 prior to treatment, and 3 days post-treatment (b). Data are presented as mean values; s.e.d. represents the standard error of the difference. a, b, c Means with disparate letters are significantly different (p < 0.001).
Expression of COX-1, COX-2 and Egr-1 in spinal cord
COX-1, COX-2 and Egr-1 mRNA were constitutively expressed in spinal cord collected from control sheep (Figure 3). No change was detected in expression of COX-1 or COX-2 mRNA in ipsilateral or contralateral spinal cord in lame animals on day 0 or day 3 post-treatment compared to control animals. Significant up-regulation of Egr-1 mRNA was detected in ipsilateral spinal cord in lame animals on day 0 before treatment compared to control animals (4.5 fold decrease; p < 0.05). Levels had returned to control levels by day 3 after treatment.
Expression of COX-1, COX-2 and Egr-1 mRNA in spinal cord. Real-time semi-quantitative measurement of COX-1 (a), COX-2 (b) and Egr-1 (c) mRNA in spinal cord from control sheep (n = 6) and sheep affected by unilateral lameness on day 0 (pre-treatment) (n = 6) and 3 days post-treatment (n = 6). Spinal cords were hemisected into ipsilateral and contralateral portions (data is pooled for control animals). Levels of mRNA are expressed relative to the endogenous reference gene β-actin. Significant increase from control: * p < 0.05.
Expression of COX-1, COX-2 and Egr-1 protein in spinal cord
Western blot analyses of protein extracts prepared from spinal cord homogenates revealed COX-1 and COX-2 antibody labelled bands at approximately 70 and 72 kDa, respectively, as expected (Figure 4). The antibody to Egr-1 detected bands at approximately 60 kDa, as expected (Figure 4). A significant up-regulation in COX-2 protein expression was found in ipsilateral and contralateral spinal cord from lame animals on day 0 relative to control animals (both p < 0.05 relative to control animals (100%)). COX-2 expression returned to control levels 3 days after treatment. No change was detected in levels of COX-1 protein in spinal cord between groups. Egr-1 protein levels were significantly increased in ipsilateral spinal cord from lame animals on day 0 (p < 0.05 relative to control animals (100%)), and this up-regulation persisted 3 days after treatment (p < 0.05 relative to control animals (100%)). Further analyses, however, revealed that levels Egr-1 proteins were decreased in ipsilateral spinal cord 3 days after treatment relative to levels in lame sheep on day 0 (p < 0.05; Figure 4).
Expression of COX-1, COX-2 and Egr-1 proteins in spinal cord. Western blot analyses of COX-1 (a), COX-2 (b) and Egr-1 (c) protein in spinal cord. Photomicrographs show expression of COX-1, COX-2 and Egr-1 at 70, 72 and 60 kDa, respectively, as expected in a representative control sample (con) and ipsilateral (i) and contralateral (c) spinal cord from an animal affected by unilateral lameness on day 0. Graphs show densitometric quantification of levels of COX-1 (a), COX-2 (b) and Egr-1 (c) protein in ipsilateral and contralateral spinal cord tissues from animals affected by unilateral lameness on day 0 before treatment (n = 6) and 3 days after treatment (n = 6). Bars represent mean ± SEM protein expression (as %) relative to control levels (100%). Significant increase from control: * p < 0.05; significant decrease from day 0: * p < 0.05.
Discussion
This study describes a unique approach to the neurobiology of the resolution of clinical inflammatory pain. The model of inflammatory pain used in this study, has been described previously and is an excellent model of naturally-occurring pain [1, 2]. Strict inclusion criteria were adhered to and from clinical examination animals recruited to the study were estimated to have had the infection for more than two weeks. Therefore, this model is representative of persistent pain. The condition 'footrot' is initiated by invasion of bacteria into the interdigital tissues inducing dermatitis, and as infection spreads the bacteria penetrate further into deep tissues causing extensive tissue damage and separation of the hoof horn, accompanied by inflammation and pain [31]. To contain the clinical heterogeneity of diseased animals, only sheep with lameness scores ≥ 5 and pathology scores ≥ 2, were recruited. As expected, animals affected with unilateral inflammation displayed significant lameness (taken as a proxy indicator of spontaneous pain) and hyperalgesia, restricted to the inflamed limb. Previous studies in this laboratory revealed a significant relationship between lameness score and mechanical hyperalgesia, supporting a positive association between the magnitude of hyperalgesia and the intensity of inflammatory pain [2]. The presence of mechanical hyperalgesia localised to the inflamed limb indicates an alteration in sensory nerve function and nociceptive processing occurring centrally, as a consequence of release of pro-inflammatory mediators at the site of inflammation and at spinal cord level. Previous studies have shown that parenteral and topical antibacterial treatment produces rapid recovery (within 5 days of treatment) from foot lesions and lameness in sheep with footrot [32]. In the present study, antiseptic footbathing, trimming the hoof horn and parental antibiotics rapidly reversed both lameness and hyperalgesia, with more than 85% of animals showing significant improvements 3 days after treatment, despite the persistence of foot pathology and lymph node hyperplasia. These findings indicate that treating the primary source of infection and therefore reducing inflammation is effective and sufficient to reverse persistent pain hypersensitivity in this clinical model.
The bilateral induction of COX-2 protein in spinal cord from sheep with inflammation and subsequent decrease in expression 3 days after treatment as lameness and hyperalgesia were resolving, supports the theory derived from experimental models that that spinal COX-2 derived PGs play a key role in central mechanisms of hyperalgesia in clinical pain [33–36]. A bilateral and inter-segmental induction of spinal COX-2 in response to unilateral inflammation induced by injection of complete Freund's adjuvant (CFA) into the footpad in rat has been described previously [12, 15], suggested to be due to a humoral response induced by circulating pro-inflammatory mediators such as IL-1β. A humoral immune response could account for the bilateral increase in COX-2 protein in spinal cord observed in the present study, however, no corresponding increase in levels of COX-2 were detected in spinal cord segments distal to the inflamed limb afferent termination site (data not presented). It is likely that increased noxious input from activated primary afferents from the inflamed limb, driving activity of spinal dorsal horn neurons, contribute to induction of COX-2, perhaps through activation of substance P, which is known to lead to increased expression of COX-2 and release of PGE2 in spinal cord [37]. Induction of COX-2 in spinal cord appears to be transient in most rodent models of inflammation, for instance, peaking 6 hours after hindpaw incision or intraplantar injection of carrageenan [38], and between 6-12 hours in response to injection of CFA into the footpad; returning to baseline levels a few days later [11, 12, 15], even though hyperalgesia and paw inflammation persists for several days beyond this period in this model [12, 39, 40]. These studies indicate that COX-2 in spinal cord plays key role in initiating central sensitization with acute inflammation. The elevated levels of COX-2 protein observed in spinal cord from sheep with persistent inflammatory disease, however, suggests that COX-2 derived PGs also contribute to maintaining the central component of hyperalgesia in this model. This is supported by a recent study by Prochazkova et al. [41] showing long-lasting up-regulation of COX-2 mRNA and protein in spinal cord in a model of osteoarthritis and persistent hyperalgesia.
Biosynthesis of Egr-1 mRNA and protein was increased in ipsilateral spinal cord from sheep with unilateral inflammation, also likely due to increased input from activated nociceptors in the inflamed limb. Egr-1 is primarily expressed in superficial dorsal horn neurons that receive input from small-diameter myelinated and unmyelinated afferent fibres [22, 25], and expression is rapidly induced in these laminae in response to a variety of acute experimental inflammatory stimuli including intraplantar injection of formalin [24, 26, 27] and carrageenan [25], and nerve-injury [42]. Furthermore, the temporal pattern of Egr-1 expression is reported to parallel development of hyperalgesia and inflammation [23, 25], suggesting a link between Egr-1 expression and behavioural responses to inflammatory pain. This hypothesis was further strengthened by a study in Egr-1 knockout mice by Ko et al. [43], that reported that although acute nociception is unaltered, hypersensitivity induced by formalin or CFA was diminished in these mice. A role for spinal Egr-1 in the maintenance of inflammatory pain is supported by evidence that Egr-1 antisense treatment in rat resulted in deficits in the maintenance of mechanical allodynia [21]. In the present study, the return of Egr-1 mRNA levels to baseline levels and decrease in protein expression 3 days after treatment, as lameness and hyperalgesia were resolving, further strengthens a role for Egr-1 in central neuronal plasticity underlying inflammatory or persistent pain.
Egr-1 activates a variety of downstream target genes by binding to the DNA sequence GCG(G/T)GGCG in the genes promoter region, including microsomal prostaglandin E synthase-1 (mPGES-1), the enzyme that couples with COX-2 to produce PGE2 [44], and COX-2 [45], suggesting an interaction between Egr-1 regulated transcription and inflammatory prostanoid production. This hypothesis is supported by evidence that inhibition of Egr-1 results in decreased COX-2 and mPGES-1 expression in LPS-stimulated murine macrophages [45], and induction of mPGES-1 mRNA following injurious ventilation in lung tissues is diminished in Egr-1 knockout mice [46]. Inflammatory prostaglandins also seem to play an important regulatory upstream role, acting as initiators of Egr-1 activity. For instance, treatment of stimulated endothelial cells with a COX-2 selective inhibitor was reported to inhibit production of Egr-1 mRNA and protein [47], while PGE2 induces Egr-1 mRNA expression cementoblastic OCCM periodontal cells [48]. The co-induction of COX-2 and Egr-1 in spinal cord from sheep with unilateral inflammation and hyperalgesia supports a link between the COX-2 signalling pathway and enhanced Egr-1 gene transcription, and may underlie persistent cell modifications at the spinal level and persistence of pain.
Conclusion
These data provide valuable information on the temporal pattern of expression of plasticity-related genes in spinal cord with resolution of naturally-occurring persistent inflammatory disease and associated pain. It is hypothesised that the biosynthesis of COX-2 and Egr-1 contribute to pain related synaptic potentiation in spinal cord pathways by mediating long lasting changes in expression of downstream targets and persistent alterations in neuronal functioning. The rapid decrease in COX-2 and Egr-1 expression with diminished pain and hyperalgesia following treatment of peripheral inflammation, suggest that these mediators and their downstream targets may be targeted to prevent the evolution of persistent pain into chronic pain.
Methods
The study was approved by the Institute's Ethics and Welfare committee and all procedures were performed according to the UK Animal Scientific Procedures Act (1986). Animals were treated in accordance with the Ethical Guidelines for Investigations of Experimental Pain in Conscious Animals as issued by the International Association for the Sudy of Pain.
Clinical model of persistent inflammation and hyperalgesia
A total of 45 adult 'Scottish Mule' ewes were used in this study, consisting of 24 sheep affected by unilateral inflammation-induced lameness ("footrot"- Figure 1), and 21 age-matched healthy control sheep selected from the same flock for euthanasia due to poor dentition or poor fertility. All lame sheep were examined clinically by an experienced observer on day 0 (prior to treatment) and a diagnosis made as appropriate. Only animals affected by unilateral 'footrot' fitting the selection criteria (described below) were recruited into the study. Control animals were also examined to exclude the presence of any other clinical signs of disease.
All unilaterally lame sheep were scored for lameness severity using an 11-point numerical rating scale (0-10; where 0 = normal and 10 = could not be more lame, i.e. not weight bearing), as previously described [49]. In addition, the affected digit was scored for pathology using a simple 5-point descriptive scale (0-4; Table 2) as described by Ley et al. [1]. Only sheep with lameness and pathology scores of ≥ 5 and ≥ 2, respectively, were recruited onto the study. All 'footrot'-affected sheep recruited had pathological lesions indicative of duration in excess of 2 weeks.
Following initial behavioural testing on day 0, selected animals were treated according to standard farm practice; foot paring (trimming off diseased horn), foot-bathing for 10 min in 10% zinc sulphate (Golden Hoof Plus; Sheep Fair Products Ltd., UK), and antibiotic (oxytetracycline) therapy administered parenterally (Duphacycline™ LA (Fort Dodge Animal Health Ltd., UK); 20 mg kg-1 bodyweight, i.m.).
Lymph node pathology
Left and right pre-scapular and popliteal lymph nodes were obtained following euthanasia from sheep with hindlimb lameness on day 0 (n = 6) before treatment, and on day 3 after treatment (n = 6), and weighed for size analysis to further confirm unilateral inflammation. In control sheep (n = 6), left and right pre-scapular and popliteal lymph nodes were collected for size comparison with those obtained from lame animals.
Behavioural testing
Withdrawal thresholds to noxious mechanical stimulation were measured according to a method used previously by our group [50]. In lame sheep, thresholds were measured on day 0 (n = 24), and 1 (n = 18), 2 (n = 18), 3 (n = 18) and 7 (n = 12) days post-treatment. In control animals, thresholds were also measured on day 0 (n = 21), and 1, 2, 3 and 7 (n = 10) days post-treatment. In brief, a pneumatic device connected to a calibrated pressure meter (C9595 IS, Comark, UK) was used to push a blunt pin, positioned on the skin of the leg, with increasing force until a withdrawal response was evoked. The minimum force required to evoke a clear lifting of the limb from the ground was defined as the withdrawal response threshold. This procedure was repeated 2-4 times at each time point. Readings from the pressure meter (mBar) were subsequently converted into force (Newtons; N). A cut-off threshold of 30 N was employed.
Real-time PCR
Real-time PCR was performed on spinal cord tissue (L6-S2) from control animals (n = 6) and animals affected by unilateral hindlimb lameness. Tissue was utilised from lame animals euthanased (Somulose™ (Arnolds, UK); 1 ml 10 kg-1 bodyweight, i.v.) on day 0 (n = 6) and on day 3 (n = 6) post-treatment. Spinal cord samples were hemisected into ipsilateral (side of pathological lesion) and contralateral sections. Total RNA was then extracted from spinal cord using TRIZOL® Reagent (Invitrogen, UK), and reverse transcribed using random hexamers (Promega, UK) and M-MLV reverse transcriptase (Invitrogen, UK). Semi-quantitative real-time PCR was performed on cDNA for ovine COX-1, COX-2 and Egr-1 and the endogenous reference gene β-actin (MWG-Biotech AG, Germany), using a MX3000P® Q-PCR system (Stratagene, UK). The PCR reaction was performed using Thermo-Start® DNA polymerase (ABgene, UK) as described in Dolan et al. [2]. Samples were run in duplicate for each quantification assay. For relative quantification of target gene mRNA the comparative Ct (cycle threshold) method was used as described in Dolan et al. [2], which involves normalisation of the number of target gene copies to the reference genes.
Western blotting
Western blots were performed on spinal cord (L6-S2) tissue protein extracts from control animals (n = 6) and animals affected by unilateral hindlimb lameness. Tissue was utilised from lame animals euthanased on day 0 (n = 6) prior to treatment and on day 3 (n = 6) post-treatment. Spinal cord samples were hemisected into ipsilateral and contralateral sections. Protein was isolated using RIPA buffer, which enables extraction of cytoplasmic, membrane and nuclear proteins, as previously described by our group [2]. Prior to loading, protein supernatants were diluted in loading buffer (NuPage® LDS sample buffer, 1 × final concentration (Invitrogen, UK); 0.05 M DTT) to a final concentration of 2 mg ml-1 and incubated for 10 min at 90°C. Diluted protein lysates (30 μg spinal cord) and protein molecular weight markers (SeaBlue Plus 2® Pre-Stained Standard and Magic Mark™ XP (Invitrogen, UK)) were loaded onto NuPage® Novex 4-12% Bis-Tris gels (Invitrogen, UK), and run for 50 min at 200 V. Proteins were transferred onto PVDF membranes (Invitrogen, UK) at 30 V for 1 h using a semi-dry blotting system. Membranes were blocked in 0.1 M PBS; 5% skimmed milk proteins; 5% BSA; 0.1% Tween® 20 for 1 h at room temperature. Following blocking, membranes were incubated overnight at 4°C with COX-1 (ovine polyclonal; 1:1000; Cayman Chemical, USA) or COX-2 (murine polyclonal; 1:1000; Cayman Chemical, USA) or Egr-1 primary antisera (rabbit polyclonal; 1:1000; Santa Cruz Biotechnology, Inc. USA) diluted in blocking buffer. Immunoblots were then washed for 3 × 5 min in 0.1 M PBS; 0.1% Tween® 20 prior to incubation for 1 h at room temperature in secondary antibody (donkey anti-rabbit IgG, HRP-linked whole antibody; 1:1,000; Amersham Biosciences, UK) solution diluted in blocking buffer. Immunoblots were then washed for 3 × 5 min in 0.1 M PBS; 0.1% Tween®20. Following washing, immunoblots were developed and visualised by enhanced chemiluminescence ECL™ detection reagents and Hyperfilm™ (Amersham Biosciences, UK). Immunoreactivity was quantified using a calibrated imaging densitometer (GS-710™, Bio-Rad UK) linked to PC-based analysis software (Quantity One®, Bio-Rad UK).
Statistical analyses
The magnitude of hyperalgesia (Emax) on the lame limb is represented as the percentage change from each animal's three other non-affected limbs according to the formula: ((mean response threshold of non-affected limbs - response threshold of lame limb)/mean response threshold of non-affected limbs) × 100. In control animals, the mean percentage change in response threshold measured on one limb relative to the three other limbs was calculated. The effect of time after treatment on the magnitude of hyperalgesia or lameness was analysed as a repeated measurements design using a residual maximum likelihood (REML) program. REML analysis was carried out due to non-orthogonality as a result of the imbalance in animal numbers between groups and time. Significant differences in the magnitude of hyperalgesia or lameness were tested using least significant differences, determined using the standard error of the difference (s.e.d.) obtained from the REML analyses.
Lymph node size is represented as the percentage of the total weight that each ipsilateral and contralateral lymph node contributes according to the formula: (ipsilateral lymph node weight/(ipsilateral + contralateral lymph node weight)) × 100. Data from forelimb and hindlimb lame animals were pooled and analysed together as initial analysis indicated no difference in response between pre-scapular and popliteal lymph nodes. Lymph node data were analysed using analysis of variance, and post-hoc least significant difference tests provided tests for differences between treatment groups, and ipsilateral and contralateral lymph node.
Real-time PCR data were analysed using an out using analysis of variance adopting a general linear model routine with post-hoc Tukey's test (Mintab, v. 14). Western blot data were converted to percentages of control values and statistical significance assessed using analysis of variance (Minitab, v13.1). The 95% confidence intervals were used for comparisons between treatment groups and controls (100%).
Abbreviations
- COX-1:
-
cyclooxyenase-1
- COX-2:
-
cyclooxyenase-2
- Egr-1 :
-
early growth response gene 1
- LTP:
-
long-term potentiation
References
Ley SJ, Livingston A, Waterman AE: The effect of chronic clinical pain on thermal and mechanical thresholds in sheep. Pain 1989, 39: 353–357. 10.1016/0304-3959(89)90049-3
Dolan S, Kelly JG, Monteiro AM, Nolan AM: Up-regulation of metabotropic glutamate receptor subtypes 3 and 5 in spinal cord in a clinical model of persistent inflammation and hyperalgesia. Pain 2003, 106: 501–12. 10.1016/j.pain.2003.09.017
Beveridge WIB: Foot rot in sheep: a transmissible disease due to infection with Fusiformis nodosus (n. sp.): studies on its cause, epidemiology and control. Commonwealth Scientific and Industrial Research Organisation (CSIRO). Australian Bulletin 1941, 140: 1–56.
Marshall DJ, Walker RI, Cullis BR, Luff MF: The effect of footrot on body weight and wool growth of sheep. Aust Vet J 1991, 68: 45–9. 10.1111/j.1751-0813.1991.tb03126.x
Ley SJ, Waterman AE, Livingston A: A field study of the effect of lameness on mechanical nociceptive thresholdsin sheep. Vet Rec 1995, 137: 85–7. 10.1136/vr.137.4.85
Malmberg AB, Yaksh TL: Hyperalgesia mediated by spinal glutamate or substance-P receptor blocked by spinal cyclooxygenase inhibition. Science 1992, 257: 1276–9. 10.1126/science.1381521
Hay CH, Trevethick MA, Wheeldon A, Bowers JS, DeBelleroche JS: The potential role of spinal cord cyclooxygenase-2 in the development of Freund's complete adjuvant-induced changes in hyperalgesia and allodynia. Neuroscience 1997, 78: 843–50. 10.1016/S0306-4522(96)00598-2
Handy RLC, Moore PK: Effects of selective inhibitors of neuronal nitric oxide synthase on carrageenan-induced mechanical and thermal hyperalgesia. Neuropharmacology 1998, 37: 37–43. 10.1016/S0028-3908(97)00201-3
Dolan S, Nolan AM: N-methyl D-aspartate induced mechanical allodynia is blocked by nitric oxide synthase and cyclooxygenase-2 inhibitors. NeuroReport 1999, 10: 449–52. 10.1097/00001756-199902250-00002
Dolan S, Kelly JG, Huan M, Nolan AM: Transient up-regulation of spinal cyclooxygenase-2 and neuronal nitric oxide synthase following surgical inflammation. Anesthesiol 2003, 98: 170–180. 10.1097/00000542-200301000-00027
Beiche F, Scheuerer S, Brune K, Geisslinger G, Goppelt-Struebe M: Upregulation of cyclooxygenase-2 mRNA in the rat spinal cord following peripheral inflammation. Febs Lett 1996, 390: 165–9. 10.1016/0014-5793(96)00604-7
Beiche F, Brune K, Geisslinger G, Goppelt-Struebe M: Expression of cyclooxygenase isoforms in the rat spinal cord and their regulation during adjuvant induced arthritis. Inflammation Res 1998, 47: 482–7. 10.1007/s000110050362
Ebersberger A, Grubb BD, Willingale HL, Gardiner NJ, Nebe J, Schaible HG: The intraspinal release of prostaglandin E 2 in a model of acute arthritis is accompanied by an up-regulation of cyclo-oxygenase-2 in the spinal cord. Neuroscience 1999, 93: 775–81. 10.1016/S0306-4522(99)00164-5
Donaldson LF, Humphrey PS, Oldfield S, Giblett S, Grubb BD: Expression and regulation of prostaglandin E receptor subtype mRNAs in rat sensory ganglia and spinal cord in response to peripheral inflammation. Prostaglandins & Other Lipid Mediators 2001, 63: 109–22. 10.1016/S0090-6980(00)00101-5
Samad TA, Moore KA, Sapirstein A, Billet S, Allchorne A, Poole S, Bonventre JV, Woolf CJ: Interleukin-1beta-mediated induction of Cox-2 in the CNS contributes to inflammatory pain hypersensitivity. Nature 2001, 410: 471–5. 10.1038/35068566
Jain NK, Ishikawa TO, Spigelman I, Herschman HR: COX-2 expression and function in the hyperalgesic response to paw inflammation in mice. Prostaglandins Leukot Essent Fatty Acids 2008, 79: 183–90. 10.1016/j.plefa.2008.08.001
Bozon B, Davis S, Laroche S: A requirement for the immediate early gene zif268 in reconsolidation of recognition memory after retrieval. Neuron 2003, 40: 695–701. 10.1016/S0896-6273(03)00674-3
Davis S, Bozon B, Laroche S: How necessary is the activation of the immediate early gene zif268 in synaptic plasticity and learning? Behav Brain Res 2003, 142: 17–30. 10.1016/S0166-4328(02)00421-7
Cole AJ, Saffen DW, Araban JM, Worley PF: Rapid increase of an immediate early gene messenger RNA in hippocampal neurons by synaptic NMDA receptor activation. Nature 1989, 340: 474–6. 10.1038/340474a0
Wisden W, Errington ML, Williams S, Dunne SB, Waters C, Hitchcock D, Evans G, Bliss TVP, Hunt SP: Differential expression of immediate early genes in the hippocampus and spinal cord. Neuron 1990, 4: 603–14. 10.1016/0896-6273(90)90118-Y
Rygh LJ, Suzuki R, Rahman W, Wong Y, Vonsy JL, Sandhu H, Webber M, Hunt S, Dickenson AH: Local and descending circuits regulate long-term potentiation and zif268 expression in spinal neurons. Eur J Neurosci 2006, 24: 761–72. 10.1111/j.1460-9568.2006.04968.x
Herdegen T, Kovary K, Leah J, Bravo R: Specific temporal and spatial distribution of JUN, FOS, and KROX-24 proteins in spinal neurons following noxious transsynaptic stimulation. J Comp Neurol 1991, 313: 178–91. 10.1002/cne.903130113
Lantéri-Minet M, de Pommery J, Herdegen T, Weil-Fugazza J, Bravo R, Menétrey D: Differential time course and spatial expression of Fos, Jun, and Krox-24 proteins in spinal cord of rats undergoing subacute or chronic somatic inflammation. J Comp Neurol 1993, 333: 223–35. 10.1002/cne.903330208
Pertovaara A, Bravo R, Herdegen T: Induction and suppression of immediate-early genes in the rat brain by a selective alpha-2-adrenoreceptor agonist and antagonist following noxious peripheral stimulation. Neuroscience 1993, 54: 117–26. 10.1016/0306-4522(93)90387-U
Buritova J, Honoré P, Besson JM: Indomethacin reduces both Krox-24 expression in the rat lumbar spinal cord and inflammatory signs following intraplantar carrageenan. Brain Res 1995, 674: 211–20. 10.1016/0006-8993(95)00009-F
Herdegen T, Riidiger S, Mayer B, Bravo R, Zimmermann M: Expression of nitric oxide synthase and colocalisation with Jun, Fos and Krox transcription factors in spinal cord neurons following noxious stimulation of the rat hindpaw. Mol Brain Res 1994, 22: 245–58. 10.1016/0169-328X(94)90053-1
Rahman OI, Terayama R, Ikeda T, Koganemaru M, Nakamura T, Shiba R, Nishimori T: Differential effects of NMDA and AMPA/KA receptor antagonists on c-Fos or Zif/268 expression in the rat spinal dorsal horn induced by noxious thermal or mechanical stimulation, or formalin injection. Neurosci Res 2002, 43: 389–99. 10.1016/S0168-0102(02)00067-6
Beckmann AM, Davidson MS, Goodenough S, Wilce PA: Differential expression of Egr-1-like DNA-binding activities in the naive rat brain and after excitatory stimulation. J Neurochem 1997, 69: 2227–37.
Thiel G, Mayer SI, Müller I, Stefano L, Rössler OG: Egr-1-A Ca(2+)-regulated transcription factor. Cell Calcium 2010, 47: 397–403. 10.1016/j.ceca.2010.02.005
Latremoliere A, Woolf CJ: Central Sensitization: A Generator of Pain Hypersensitivity by Central Neural Plasticity. J Pain 2009, 10: 895–926. 10.1016/j.jpain.2009.06.012
Abbott KA, Lewis CJ: Current approaches to the management of ovine footrot. Vet J 2005, 169: 28–41. 10.1016/j.tvjl.2004.05.008
Kaler J, Daniels SLS, Wright JL, Green LE: Randomised clinical trial of long acting oxytetracycline, foot trimming and flunixine meglumine on time to recovery in sheep with footrot. J Vet Intern Med 2010, 24: 420–25. 10.1111/j.1939-1676.2009.0450.x
Yamamoto T, Nozaki-Taguchi N: Analysis of the effects of cyclooxygenase (COX)-1 and COX-2 in spinal nociceptive transmission using indomethacin, a non-selective COX inhibitor, and NS-398, a COX-2 selective inhibitor. Brain Res 1996, 739: 104–10. 10.1016/S0006-8993(96)00817-7
Dirig DM, Isakson PC, Yaksh TL: Effect of COX-1 and COX-2 inhibition on induction and maintenance of carrageenan-evoked thermal hyperalgesia in rats. J Pharmacol Exp Ther 1998, 285: 1031–38.
Yaksh TL, Dirig DM, Conway CM, Svensson C, Luo D, Isakson PC: The acute antihyperalgesic action of non-steroidal, anti-inflammatory drugs and release of spinal PGE 2 is mediated by the inhibition of constitutive spinal cyclo-oxygenase-2 (COX-2) but not COX-1. J Neurosci 2001, 21: 5847–53.
Seybold VS, Jia YP, Abrahams LG: Cyclo-oxygenase-2 contributes to central sensitization in rats with peripheral inflammation. Pain 2003, 105: 47–55. 10.1016/S0304-3959(03)00254-9
Rasley A, Marriott I, Halberstadt CR, Bost KL, Anguita J: Substance P augments Borrelia burgdorferi-induced prostaglandin E2 production by murine microglia. J Immunol 2004, 172: 5707–13.
Prochazkova M, Dolezal T, Sliva J, Krsiak M: Different patterns of spinal cyclooxygenase-1 and cyclooxygenase-2 mRNA expression in inflammatory and postoperative pain. Basic Clin Pharmacol Toxicol 2006, 99: 173–7. 10.1111/j.1742-7843.2006.pto_457.x
Jia YP, Linden DR, Serieb JR, Seybold VS: Nociceptin/orphanin FQ binding increases in superficial laminae of the rat spinal cord during persistent peripheral inflammation. Neurosci Lett 1998, 250: 21–24. 10.1016/S0304-3940(98)00430-3
Zhang YH, Chen Y, Zhao ZQ: Resiniferatoxin reversibly blocks adjuvant-induced thermal hyperalgesia in the rat. Eur J Pharm 2003, 481: 301–4. 10.1016/j.ejphar.2003.09.053
Prochazkova M, Zanvit P, Dolezal T, Prokesova L, Krsiak M: Increased gene expression and production of spinal cyclooxygenase 1 and 2 during experimental oste oarthriti s pain. Physiol Res 2009, 58: 419–25.
Delander GE, Schott E, Brodin E, Fredholm BB: Spinal expression of mRNA for immediate early genes in a model of chronic pain. Acta Physiol Scand 1997, 161: 517–25. 10.1046/j.1365-201X.1997.00260.x
Ko SW, Vadakkan KI, Ao H, Gallitano-Mendel A, Wei F, Milbrandt J, Zhuo M: Selective contribution of Egr1 (zif/268) to persistent inflammatory pain. J Pain 2005, 6: 12–20. 10.1016/j.jpain.2004.10.001
Murakami M, Kudo I: Prostaglandin E Synthase: A Novel Drug Target for Inflammation and Cancer. Curr Pharmaceut Des 2006, 12: 943–54. 10.2174/138161206776055912
Díaz-Muñoz MD, Osma-García IC, Cacheiro-Llaguno C, Fresno M, Íñiguez MA: Coordinated up-regulation of cyclooxygenase-2 and microsomal prostaglandin E synthase 1 transcription by nuclear factor kappa B and early growth response-1 in macrophages. Cell Signal 2010, 22: 1427–36. 10.1016/j.cellsig.2010.05.011
Ngiam N, Peltekova V, Engelberts D, Otulakowski G, Post M, Kavanagh BP: Early growth response-1 worsens ventilator-induced lung injury by up-regulating prostanoid synthesis. Am J Respir Crit Care Med 2010, 181: 947–56. 10.1164/rccm.200908-1297OC
Szabó IL, Pai R, Soreghan B, Jones MK, Baatar D, Kawanaka H, Tarnawski AS: NSAIDs inhibit the activation of egr-1 gene in microvascular endothelial cells. A key to inhibition of angiogenesis? J Physiol Paris 2001, 95: 379–83. 10.1016/S0928-4257(01)00051-1
Pham L, Bezouglaia O, Camargo PM, Nervina JM, Tetradis S: Prostanoids induce egr1 gene expression in cementoblastic OCCM cells. J Periodontal Res 2007, 42: 486–93. 10.1111/j.1600-0765.2007.00972.x
Welsh EM, Gettinby G, Nolan AM: Comparison of a visual analogue scale and a numerical rating scale for assessment of lameness, using sheep as a model. Am J Vet Res 1993, 54: 976–83.
Nolan A, Livingston A, Morris R, Waterman A: Techniques for comparison of thermal and mechanical nociceptive stimuli in the sheep. J Pharmacol Meth 1987, 17: 39–49. 10.1016/0160-5402(87)90035-0
Acknowledgements
This work was supported by funding from the Biotechnology and Biological Sciences Research Council, UK.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
SD and AMN conceived and designed the study. AMN carried out the clinical assessments, while SD, PH and CC carried out nociceptive threshold tests, treatments and molecular expression studies. SD and PH carried out the statistical analysis and SD, PH and AMN were responsible for drafting the manuscript. All authors have read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Dolan, S., Hastie, P., Crossan, C. et al. Co-induction of cyclooxyenase-2 and early growth response gene (Egr-1) in spinal cord in a clinical model of persistent inflammation and hyperalgesia. Mol Pain 7, 91 (2011). https://doi.org/10.1186/1744-8069-7-91
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1744-8069-7-91