Abstract
Background
Non-enzymatic glycation increases hemoglobin-oxygen affinity and reduces oxygen delivery to tissues by altering the structure and function of hemoglobin.
Objectives
We investigated whether an elevated blood concentration of glycosylated hemoglobin (HbA1c) could induce falsely high pulse oximeter oxygen saturation (SpO2) in type 2 diabetic patients during mechanical ventilation or oxygen therapy.
Methods
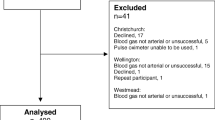
Arterial oxygen saturation (SaO2) and partial pressure of oxygen (PO2) were determined with simultaneous monitoring of SpO2 in 261 type 2 diabetic patients during ventilation or oxygen inhalation.
Results
Blood concentration of HbA1c was >7% in 114 patients and ≤ 7% in 147 patients. Both SaO2 (96.2 ± 2.9%, 95% confidence interval [CI] 95.7-96.7% vs. 95.1 ± 2.8%, 95% CI 94.7-95.6%) and SpO2 (98.0 ± 2.6%, 95% CI 97.6-98.5% vs. 95.3 ± 2.8%, 95% CI 94.9-95.8%) were significantly higher in patients with HbA1c >7% than in those with HbA1c ≤ 7% (Data are mean ± SD, all p < 0.01), but PO2 did not significantly differ between the two groups. Bland-Altman analysis demonstrated a significant bias between SpO2 and SaO2 (1.83 ±0.55%, 95% CI 1.73% -1.94%) and limits of agreement (0.76% and 2.92%) in patients with HbA1c >7%. The differences between SpO2 and SaO2 correlated closely with blood HbA1c levels (Pearson’s r = 0.307, p < 0.01).
Conclusions
Elevated blood HbA1c levels lead to an overestimation of SaO2 by SpO2, suggesting that arterial blood gas analysis may be needed for type 2 diabetic patients with poor glycemic control during the treatment of hypoxemia.
Similar content being viewed by others
Background
Glycohemoglobin is produced via a non-enzymatic reaction between the free aldehyde group of glucose or other sugars and the unprotonated form of free amino groups of hemoglobin[1]. Glycosylated hemoglobin A1c (HbAlc) is a stable minor hemoglobin variant separated by charge that is composed primarily but variably of glycohemoglobin. A clinical relationship between blood concentration of HbAlc and status of glycemic control has been elucidated[2], and elevated HbAlc levels represent increased risk of coronary artery disease and poor outcome in diabetic patients[3–5]. Previous studies have shown that glycosylation alters the structure and function of hemoglobin[6, 7] and tends to shift the oxygen dissociation curve to the left, leading to an increase in hemoglobin-oxygen affinity and a reduction in oxygen delivery to tissues[6, 8, 9]. Pulse oximetry is widely used as a noninvasive tool for continuous monitoring of artery oxygen saturation (SaO2)[10, 11], but pulse oximeter oxygen saturation (SpO2) may overestimate arterial blood gases-determined SaO2 in acute sickle chest syndrome and severe sepsis[12, 13]. So far, its accuracy for titrating fractional inspired oxygen in type 2 diabetic patients with mechanical ventilation or oxygen therapy remains unclear. Given that chronic hyperglycemia accelerates the accumulation of advanced glycation end products (AGE) in the skin collagen[14], which poses specific autofluorescence feature, may emit light by absorbing specific wavelengths light[15], and interfere with the accuracy of pulse oximetry, it is pertinent to examine if elevated blood HbAlc concentrations could result in an overestimation of SaO2 by SpO2 with finger probes particularly for type 2 diabetic patients with poor glycemic control.
Methods
Study population
A total of 261 consecutive type 2 diabetic patients undergoing oxygen therapy and/or mechanical ventilation from October 2010 to May 2012 in Rui Jin Hospital, Shanghai Jiaotong University School of Medicine were included. None had any recorded history of carbon monoxide exposure. The diagnosis of type 2 diabetes was made according to the criteria of American Diabetes Association, including symptoms of diabetes plus casual plasma glucose concentration beyond 200 mg/dl (11.1 mmol/l), or an increased fasting (126 mg/dl [7.0 mmol/l]) or 2-hour postprandial glucose (2-h PG) level (200 mg/dl [11.1 mmol/l] during an oral glucose tolerance test)[16]. Patients with type 1 diabetes were excluded by measurement of C-peptide. For the purpose of this study, we also excluded patients who were current cigarette smokers within 3 months or alcohol-dependent, had renal insufficiency, anemia and fever, or were treated with vaso-constrictive agents. Poor glycemic control was defined as blood HbAlc level >7%[17]. The study was approved by the hospital Institutional Review Board (IRB), and written informed consent was obtained from all participants.
Biochemical assessments
Peripheral venous blood was collected after an overnight fasting in all patients, and serum levels of glucose, blood urea nitrogen, creatinine, total cholesterol, low-density lipoprotein-cholesterol (LDL-C), high-density lipoprotein cholesterol (HDL-C) and triglycerides were measured with standard laboratory techniques on a Hitachi 912 Analyzer (Roche Diagnostics, Germany). Hemoglobin concentrations were determined with a model T-890 Coulter (Beckman Coulter International, Nyon, Switzerland). In order to exclude individuals with abnormal hemoglobin, electrophoresis was carried out according to the method of Marengo-Rowe[18]. Blood HbA1c concentration was assayed using ion-exchange high performance liquid chromatography with a Bio-Rad Variant Hemoglobin Testing System (Bio-Rad Laboratories, Hercules, CA, USA). Levels of 2, 3-diphosphoglycerate (2,3-DPG) in the red blood cells were assayed within 15 min using enzymatic determination at 340 nm with an ultraviolet test kit from Roche Diagnostics (Roche Diagnostics GmbH, Mannheim, Germany) according to the manufacturer’s instructions.
Arterial blood gas analysis
Arterial blood gases were determined during simultaneous SpO2 monitoring with pulse oximetry. Blood was drawn anaerobically into a preheparinized 1-mL syringe, and mixed well before measurement. After removal of all air bubbles from the syringe, in vivo pH, partial pressure of carbon dioxide (PCO2), SaO2, partial pressure of oxygen (PO2) and carboxyhemoglobin were directly measured using a Cobas b 221 blood gas analyzer (Roche Diagnostics, Germany). All measurements were completed within 5 min of blood sampling. Arterial blood gas analysis and SpO2 values were one measurement per patient.
Monitoring of pulse oxygen saturation
SpO2 was monitored continuously with a pulse oximetry (Nellcor NPB 40 MAX, Hayward, California), which detects oxygen saturation by measuring transdermal light absorption in the blood flow through a fingertip (DS 100A finger probe). SpO2 values were recorded only after a consistent reading, with a strong arterial waveform signal and a pulse reading identical to the patient’s heart rate.
Statistical analysis
Baseline characteristics are expressed as mean and standard deviation (SD) for continuous variables, and percentages for categorical ones. Chi-square test was used to analyze dichotomous variables. Comparisons of continuous variables between groups were made by the appropriate Student’s t tests. Correlation between difference (SpO2 -SaO2) and HbA1c was analyzed using Pearson correlation coefficients. Accuracy (SpO2 - SaO2) of SpO2 was examined by the method of Bland and Altman analysis[19]. Bias was determined by the mean difference and 95% confidence intervals (CI) between SpO2 and SaO2, precision was determined by the standard deviation of the mean difference, and limits of agreement (mean difference ±1.96SD) was defined as a proportional function of distribution for differences between the 2 measurements. Data were analyzed using the Statistical Packages for Social Sciences (SPSS Version 13.0, Chicago, Ill). A 2-tailed p value < 0.05 was considered statistically significant. Only one measurement per patient for arterial blood gas and SpO2 was made.
Results
Clinical characteristics
Among overall 261 type 2 diabetic patients, 114 patients had a HbAlc >7%, and 147 had a HbA1c ≤ 7%. Patients with HbAlc >7% were older and had higher serum levels of fasting glucose, 2-h postprandial glucose, and triglycerides than those with HbA1c ≤ 7%. The two groups did not differ with respect to occurrence rates of hypertension, chronic obstructive pulmonary disease, and pulmonary edema (Table1).
Arterial blood gas profiles, pulse oximetry, and 2, 3-DPG
Both SaO2 (96.2 ± 2.9%, 95% confidence interval [CI] 95.7-96.7% vs. 95.1 ± 2.8%, 95% CI 94.7-95.6%) and SpO2 (98.0 ± 2.6%, 95% CI 97.6-98.5% vs. 95.3 ± 2.8%, 95% CI 94.9-95.8%) were significantly higher in patients with HbA1c >7% than in those with HbA1c ≤ 7% (Data are mean ± SD, all p < 0.01), but PO2 did not significantly differ between the two groups.
Levels of 2, 3-DPG in the red blood cells and PCO2 were slightly elevated in patients with HbA1c >7%, but did not reach statistical significance levels (p >0.05). Body temperature, pH, and carboxyhemoglobin were similar in the two groups (Table2).
The difference between SpO2 and SaO2 correlated closely with blood HbA1c levels (Pearson’s r = 0.307, p < 0.01) (Figure1).
Arterial oxyhemoglobin sigmoid curves
The sigmoid fitted curve for patients with HbA1c >7% shifted to the left compared with that with HbA1c ≤ 7%. The mean difference of SaO2 between diabetic patients with HbA1c >7% and those with HbA1c ≤ 7% was 1.1% (Figure2).
Bland-Altman analysis
The simultaneous readings of SaO2 and SpO2 were analyzed to determine the bias and limits of agreement. Bland-Altman analysis indicated that the bias (mean difference of SpO2 minus SaO2) between the two methods was 1.83 ±0.55% (95% CI1.73% -1.94%) and limits of agreement were 0.76% and 2.92% in patients with HbA1c >7% (Figure3). Overall, there was a significant bias between pulse oximetry and arterial blood gases in patients with HbA1c >7%.
Discussion
The present study is the first to demonstrate that despite similar levels of red blood cell 2, 3-DPG, PO2, PCO2, pH and body temperature, type 2 diabetic patients with HbA1c > 7% had higher SaO2 (the mean difference was 1.1%) and bias (1.83 ±0.55%) compared with those with HbA1c ≤ 7%, suggesting that elevated blood HbAlc levels led to an overestimation of SaO2 by pulse oximetry.
Hypoxemia denotes a condition that is characterized by low oxygen content or percent saturation of hemoglobin with oxygen[13]. Arterial blood gases have been traditionally used to assess the status of oxygenation and to adjust fractional inspired oxygen in patients receiving mechanical ventilation or oxygen therapy[20]. Currently, noninvasive continuous monitoring of SaO2 with SpO2 has become the standard care for patients with critical conditions[13, 21], to decrease the likelihood of hypoxemia[22–25] and to wean mechanical ventilation[10, 11, 26]. In the present study, when comparisons were performed at identical PO2, SaO2 was higher in type 2 diabetic patients with HbA1c > 7%, which is likely due to an increased hemoglobin-oxygen affinity. Our results are in line with previous findings that higher blood concentrations of HbA1c significantly reduce oxygen dissociation velocity[27]. Although the exact mechanism remains not fully understood, it may be, at least partly, explained by glycation of multiple ß-chain sites of hemoglobin A molecule, accompanied by increasing -chain glycation at high glycohemoglobin concentrations[28, 29].
The major finding of this study is that in type 2 diabetic patients with poor glycemic control, pulse oximetry overestimated arterial blood gases-determined SaO2 by a mean of 2.7% when compared with those with HbA1c ≤ 7%. Previous studies showed that older women have higher HbA1c than men, even after controlling for body mass index[30], and accumulation of AGE in human skin collagen is age-dependent[31]. However, both gender distribution and age did not significantly differ between the two groups in the present study, suggesting that the difference between SpO2 and SaO2 may be mainly related to HbA1c levels as higher HbA1c levels were associated with great differences (Pearson’s r = 0.307, p < 0.01).
Our findings may be of important clinical relevance. First, falsely high SpO2 could cause under-diagnosis of hypoxemia in type 2 diabetic patients. Second, because a greater SpO2 was required to achieve the same arterial blood gases-determined PO2 for diabetic patients with HbA1c >7% compared with those with HbA1c ≤ 7%, care should be taken in adjusting oxygen supply during mechanical ventilation or oxygen therapy. The reason for a higher SpO2 than SaO2 may be partly explained by an extensive accumulation of AGE in the skin collagen in patients with poor glycemic control[14], interfering with transdermal absorption of the specific wavelength light by hemoglobin with finger probes[12, 32]. These observations support a notion that the causes of high bias does include skin effect[33, 34], and when SaO2 needs to be determined with a high degree of accuracy, arterial blood gases are recommended in type 2 diabetic patients with poor glycemic control.
Limitations
Due to relatively small sample size, potential for selection bias may raise some concerns on the statistical precision of the estimates. A large-scale study is warranted to confirm our findings. The other major limitation is that most of the data are at high SaO2 because of a specially selected study population as all patients were receiving mechanical ventilation and/or oxygen therapy. The oxyhemoglobin dissociation curves could actually be fitted with non-linear regression, and a partial pressure of oxygen in blood associated to a hemoglobin oxygen saturation of 50% (P50) could also be calculated[35]. Most oximetry testing intentionally gathers data below 90% by performing desaturation experiments in volunteers. Gather multiple data points on volunteers increase the data set substantially, and allow one to test over a wide range of SaO2, and control for other effects. By creating a gas pocket with CO2 and O2/N2 mixtures, one can create a much more detailed oxyhemoglobin dissociation curve. The US FDA requires testing balanced by gender and ethnicity. Repeated measures statistics would then be necessary, and P50 is not determined quite as precisely unless the sample is near a SaO2 of 50%. Certainly, it remains unclear whether the issue with diabetic patients would be safe given the possibility of cardiovascular disease, although younger subjects could be reasonable.
Conclusions
Elevated blood HbA1c concentrations lead to an overestimation of SaO2 by SpO2, suggesting that arterial blood gas analysis may be needed for type 2 diabetic patients with poor glycemic control during the treatment of hypoxemia.
Abbreviations
- AGE:
-
Advanced glycation end products
- 2, 3-DPG:
-
2, 3-diphosphoglycerate
- CI:
-
Confidence interval
- HbAlc:
-
Glycosylated hemoglobin A1c
- HDL:
-
High-density lipoprotein
- LDL:
-
Lower-density lipoprotein
- PCO2:
-
Partial pressure of carbon dioxide
- PO2:
-
Partial pressure of oxygen
- SaO2:
-
Arterial oxygen saturation
- SD:
-
Standard deviation
- SpO2:
-
Pulse oximeter oxygen saturation.
References
Miedema K: Electrospray mass spectrometry for measurement of glycohemoglobin. Clin Chem. 1997, 43: 705-707.
American Diabetes Association: Clinical practice recommendations. Diabetes Care. 2000, 23: S32-42.
Daida H, Takayama T, Hiro T, Yamagishi M, Hirayama A, Saito S, Yamaguchi T, Matsuzaki M: High HbA1c levels correlate with reduced plaque regression during statin treatment in patients with stable coronary artery disease: Results of the coronary atherosclerosis study measuring effects of rosuvastatin using intravascular ultrasound in Japanese subjects (COSMOS). Cardiovasc Diabetol. 2012, 11: 87-10.1186/1475-2840-11-87.
Nishimura R, Nakagami T, Sone H, Ohashi Y, Tajima N: Relationship between hemoglobin A1c and cardiovascular disease in mild-to-moderate hypercholesterolemic Japanese individuals: subanalysis of a large-scale randomized controlled trial. Cardiovasc Diabetol. 2011, 10: 58-10.1186/1475-2840-10-58.
Ikeda N, Iijima R, Hara H, Moroi M, Nakamura M, Sugi K: Glycated hemoglobin is associated with the complexity of coronary artery disease, even in non-diabetic adults. J Atheroscler Thromb. 2012, 19: [Epub ahead of print]
De Rosa MC, Sanna MT, Messana I, Castagnola M, Galtieri A, Tellone E, Scatena R, Botta B, Botta M, Giardina B: Glycated human hemoglobin (HbA1c): functional characteristics and molecular modeling studies. Biophys Chem. 1998, 72: 323-335. 10.1016/S0301-4622(98)00117-3.
Samaja M, Melotti D, Carenini A, Pozza G: Glycosylated haemoglobins and the oxygen affinity of whole blood. Diabetologia. 1982, 23: 399-402.6.
Bunn HF: The glycosylation of hemoglobin: relevance to diabetes mellitus. Science. 1978, 200: 21-27. 10.1126/science.635569.
Ditzel J: Affinity hypoxia as a pathogenic factor of microangiopathy with particular reference to diabetic retinopathy. Acta Endocrinologica Supplementum. 1980, 238: 39-55.
Jubran A, Tobin MJ: Reliability of pulse oximetry in titrating supplemental oxygen therapy in ventilator-dependent patients. Chest. 1990, 97: 1420-1425. 10.1378/chest.97.6.1420.
Moloney ED, Kiely JL, McNicholas WT: Controlled oxygen therapy and carbon dioxide retention during exacerbations of chronic obstructive pulmonary disease. Lancet. 2001, 357: 526-528. 10.1016/S0140-6736(00)04049-6.
Kress JP, Pohlman AS, Hall JB: Determination of hemoglobin saturation in patients with acute sickle chest syndrome: a comparison of arterial blood gases and pulse oximetry. Chest. 1999, 115: 1316-1320. 10.1378/chest.115.5.1316.
Wilson BJ, Cowan HJ, Lord JA, Zuege DJ, Zygun DA: The accuracy of pulse oximetry in emergency department patients with severe sepsis and septic shock: a retrospective cohort study. BMC Emerg Med. 2010, 10: 9-10.1186/1471-227X-10-9.
Dyer DG, Dunn JA, Thorpe SR, Bailie KE, Lyons TJ, McCance DR, Baynes JW: Accumulation of Maillard reaction products in skin collagen in diabetes and aging. J Clin Invest. 1993, 91: 2463-2469. 10.1172/JCI116481.
Bos DC, de Ranitz-Greven WL, de Valk HW: Advanced glycation end products, measured as skin autofluorescence and diabetes complications: a systematic review. Diabetes Technol Ther. 2011, 13: 773-779. 10.1089/dia.2011.0034.
Expert Committee on the Diagnosis and Classification of Diabetes Mellitus: Report of the expert committee on the diagnosis and classification of diabetes mellitus. Diabetes Care. 2003, 26 (Suppl 1): S5-20.
Kassaian SE, Goodarzynejad H, Boroumand MA, Salarifar M, Masoudkabir F, Mohajeri-Tehrani MR, Pourhoseini H, Sadeghian S, Ramezanpour N, Alidoosti M, Hakki E, Saadat S, Nematipour E: Glycosylated hemoglobin (HbA1c) levels and clinical outcomes in diabetic patients following coronary artery stenting. Cardiovasc Diabetol. 2012, 11: 82-10.1186/1475-2840-11-82.
Marengo-Rowe AJ: Rapid electrophoresis and quantitation of hemoglobin on cellulose acetate. J Clin Pathol. 1965, 18: 790-792. 10.1136/jcp.18.6.790.
Bland JM, Altman DG: Measuring agreement in method comparison studies. Stat Methods Med Res. 1999, 8: 161-179. 10.1191/096228099668524590.
de Jonge E, Peelen L, Keijzers PJ, Joore H, de Lange D, van der Voort PH, Bosman RJ, de Waal RA, Wesselink R, de Keizer NF: Association between administered oxygen, arterial partial oxygen pressure and mortality in mechanically ventilated intensive care unit patients. Crit Care. 2008, 12: R156-10.1186/cc7150.
Birnbaum S: Pulse oximetry: identifying its applications, coding, and reimbursement. Chest. 2009, 135: 838-841. 10.1378/chest.07-3127.
Van de Louw A, Cracco C, Cerf C, Harf A, Duvaldestin P, Lemaire F, Brochard L: Accuracy of pulse oximetry in the intensive care unit. Intensive Care Med. 2001, 27: 1606-1613. 10.1007/s001340101064.
Lee WW, Mayberry K, Crapo R, Jensen RL: The accuracy of pulse oximetry in the emergency department. Am J Emerg Med. 2000, 18: 427-431.
Seguin P, Le Rouzo A, Tanguy M, Guillou YM, Feuillu A, Malledant Y: Evidence for the need of bedside accuracy of pulse oximetry in an intensive care unit. Crit Care Med. 2000, 28: 703-706. 10.1097/00003246-200003000-00017.
Jubran A: Pulse oximetry. Intensive Care Med. 2004, 30: 2017-2020.
Mihm FG, Halperin BD: Noninvasive detection of profound arterial desaturations using a pulse oximetry device. Anesthesiology. 1985, 62: 85-87. 10.1097/00000542-198501000-00020.
Marschner JP, Seidlitz T, Rietbrock N: Effect of 2,3-diphosphoglycerate on O2-dissociation kinetics of hemoglobin and glycosylated hemoglobin using the stopped flow technique and an improved in vitro method for hemoglobin glycosylation. Int J Clin Pharmacol Ther. 1994, 32: 116-121.
Peterson KP, Pavlovich JG, Goldstein D, Little R, England J, Peterson CM: What is hemoglobin A1c? An analysis of glycated hemoglobins by electrospray ionization mass spectrometry. Clin Chem. 1998, 44: 1951-1958.
Roberts NB, Amara AB, Morris M, Green BN: Long-term evaluation of electrospray ionization mass spectrometric analysis of glycated hemoglobin. Clin Chem. 2001, 47: 316-321.
Martins RA, Jones JG, Cumming SP, Coelho e Silva MJ, Teixeira AM, Veríssimo MT: Glycated hemoglobin and associated risk factors in older adults. Cardiovasc Diabetol. 2012, 11: 13-10.1186/1475-2840-11-13.
Dunn JA, McCance DR, Thorpe SR, Lyons TJ, Baynes JW: Age-dependent accumulation of Nε-(carboxymethyl)lysine and Nε-(carboxymethyl)hydroxylysine in human skin collagen. Biochemistry. 1991, 30: 1205-1210. 10.1021/bi00219a007.
Gerrits EG, Lutgers HL, Kleefstra N, Graaff R, Groenier KH, Smit AJ, Gans RO, Bilo HJ: Skin autofluorescence: a tool to identify type 2 diabetic patients at risk for developing microvascular complications. Diabetes Care. 2008, 31: 517-521.
Bickler PE, Feiner JR, Severinghaus JW: Effects of skin pigmentation on pulse oximeter accuracy at low saturation. Anesthesiology. 2005, 102: 715-719. 10.1097/00000542-200504000-00004.
Feiner JR, Severinghaus JW, Bickler PE: Dark skin decreases the accuracy of pulse oximeters at low oxygen saturation: the effects of oximeter probe type and gender. Anesth Analg. 2007, 105: S18-23. 10.1213/01.ane.0000285988.35174.d9.
Severinghaus JW: Simple, accurate equations for human blood O2 dissociation computations. J Appl Physiol. 1979, 46: 599-602.
Acknowledgements and funding
This study was supported by a grant from Shanghai Municipal Science and Technology Committee (10JC1410500).
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
LJP designed the study and drafted the manuscript; YS collected the samples and performed the experiments; LL participated in the whole process of experiments; RYZ and QZ contributed to data analysis; WFS was responsible for the whole research project and prepared the manuscript. All authors have read and approved the final manuscript.
Li Jin Pu, Ying Shen contributed equally to this work.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Pu, L.J., Shen, Y., Lu, L. et al. Increased blood glycohemoglobin A1c levels lead to overestimation of arterial oxygen saturation by pulse oximetry in patients with type 2 diabetes. Cardiovasc Diabetol 11, 110 (2012). https://doi.org/10.1186/1475-2840-11-110
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1475-2840-11-110