Abstract
BACKGROUND: Based on a series of clinical trials showing no difference in the effectiveness or tolerability of most major classes of antihypertensive medications, the Joint National Commission on High Blood Pressure Treatment recommends that physicians prescribe β-blockers or diuretics as initial hypertensive therapy unless there are compelling indications for another type of medication. Nevertheless, many physicians continue to favor more expensive medications like angiotensin-converting enzyme (ACE) inhibitors and calcium channel blockers as first line agents. The persistent use of these agents raises questions as to whether physicians perceive ACE inhibitors and calcium channel blockers to be better than β-blockers and diuretics.
METHODS: We surveyed 1,200 primary care physicians in 1997, and another 500 primary care physicians in 2000, and asked them to estimate the relative effectiveness and side effects of 4 classes of medication in treating a hypothetical patient with uncomplicated hypertension: ACE inhibitors, β-blockers, calcium channel blockers, and diuretics. In addition, we asked them to indicate whether they ever provided free samples of hypertension medications to their patients.
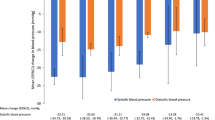
RESULTS: Perceptions of the relative effectiveness and side effects of the 4 classes of hypertension medications did not significantly change over the 3 years, nor did prescription recommendations. Physicians perceive that diuretics are less effective at lowering blood pressure than the other 3 classes (P<.001). They also perceive that β-blockers are less tolerated than the other 3 classes (P<.001). In a multivariate model, perceptions of effectiveness and tolerability displayed significant associations with prescription preference independent of background variables. The only other variable to contribute significantly to the model was provision of free medication samples to patients.
CONCLUSIONS: Despite numerous clinical trials showing no difference in the effectiveness or side-effect profiles of these 4 classes of drugs, most physicians believed that diuretics were less effective and β-blockers were less tolerated than other medications. Moreover, their prescription practices were associated with their provision of free samples provided by pharmaceutical representatives, even after adjusting for other demographic characteristics. Efforts to increase physicians’ prescribing of β-blockers and diuretics may need to be directed at overcoming misunderstandings about the effectiveness and tolerability of these medicines.
Similar content being viewed by others
References
Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. The Sixth Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Arch Intern Med. 1997;157:2413–46.
Hansson L, Hedner T, Lund-Johansen P, et al. Randomised trial of effects of calcium antagonists compared with diuretics and beta-blockers on cardiovascular morbidity and mortality in hypertension: the Nordic Diltiazem (NORDIL) study. Lancet. 2000;356:359–65.
Brown M, Palmer CR, Castaigne A, et al. Morbidity and mortality in patients randomised to double-blind treatment with a long-acting calcium-channel blocker or diuretic in the International Nifedipine GITS study: intervention as a goal in hypertension treatment (INSIGHT). Lancet. 2000;5:366–72.
Neaton J, Grimm R, Prineas R, et al. Treatment Mild Hypertension Study: final results. JAMA. 1993;270:713–24.
Materson B, Reda D, Cushman W. Department of Veterans Affairs Cooperative Study Group on Antihypertensive Agents. Department of Veterans Affairs single-drug therapy of hypertension study: revised figures and new data. Am J Hypertens. 1995;8:189–92.
Hannsson L, Lindholm LH, Niskanen L, et al. Effect of angiotensin-converting-enzyme inhibition compared with conventional therapy on cardiovascular morbidity and mortality in hypertension: the Captopril Prevention Project (CAPPP) randomized trial. Lancet. 1999;353:611–6.
Croog SH, Levine S, Testa MA, et al. The effects of antihypertensive therapy on the quality of life. N Engl J Med. 1986;314:1657–64.
Materson B, Reda D, Cushman W, et al. Single-drug therapy for hypertension in men: a comparison of six hypertensive agents with placebo. N Engl J Med. 1993;328:914–21.
Ogihara T, Kuramoto K. Effect of long-term treatment with antihypertensive drugs on quality of life of elderly patients with hypertension: a double-blind comparative study between a calcium antagonist and a diuretic. Hypertens Res. 2000;23:33–7.
Manolio T, Cutler J, Furberg C, Psaty B, Whelton P, Applegate W. Trends in pharmacologic management of hypertension in the United States. Arch Intern Med. 1995;155:829–37.
Siegel D, Lopez J. Trends in antihypertensive drug use in the United States: do the JNC V recommendations affect prescribing? JAMA. 1997;278:1745–8.
Avorn J, Chen M, Hartley R. Scientific versus commercial sources of influence on the prescribing behavior of physicians. Am J Med. 1982;73:4–8.
Chren M-M, Landefeld CS. Physicians’ behavior and their interactions with drug companies: a controlled study of physicians who requested additions to a hospital drug formulary. JAMA. 1994;271:684–9.
Moser M. Why are physicians not prescribing diuretics more frequently in the management of hypertension? JAMA. 1998;279:1813–6.
Wang TJ, Ausiello JC, Stafford RS. Trends in antihypertensive drug advertsing, 1985–96. Circulation. 1999;99:2055–7.
Lurie N, Rich EC, Simpson DE, et al. Pharmaceutical representatives in academic medical centers: interaction with faculty and housestaff. J Gen Intern Med. 1990;5:240–3.
Bowman MA. The impact of drug company funding on the content of continuing medical education. Mobius. 1986;6:66–9.
Bowman MA, Pearle DL. Changes in drug prescribing patterns related to commercial company funding of continuing medical education. J Contin Educ Health Prof. 1988;8:13–20.
Chew LD, O’Young TS, Hazlet TK, Bradley KA, Maynard C, Lessler DS. A physician survey of the effect of drug sample availability on physicians’ behavior. J Gen Intern Med. 2000;15:478–83.
Shaughnessy A, Bucci K. Drug samples and family practice residents. Ann Pharmacother. 1997;31:1296–1300.
Morelli D, Koenigsberg M. Sample medication dispensing in a residency practice. J Fam Pract. 1992;34:42–8.
Peay MY, Peay ER. The role of commercial sources in the adoption of a new drug. Soc Sci Med. 1988;26:1183–9.
Caudill ST, Johnson MS, Rich EC, McKinney PW. Physicians, pharmaceutical sales representatives, and the cost of prescribing. Arch Fam Med. 1996;5:201–6.
Peabody JW, Luck J, Glassman P, Dresselhaus TR, Lee M. Comparison of vignettes, standardized patients, and chart abstraction. A prospective validation study of 3 methods for measuring quality. JAMA. 2000;283:1715–22.
Author information
Authors and Affiliations
Corresponding author
Additional information
Support: Dr. Ubel is supported by a career development award from the Department of Veterans Affairs and by a Presidential Early Career Award for Scientists and Engineers. This work was also supported by the Matthew Slap Foundation and The National Cancer Institute (R01-CA78052-01).
Rights and permissions
About this article
Cite this article
Ubel, P.A., Jepson, C. & Asch, D.A. Misperceptions about β-blockers and diuretics. J GEN INTERN MED 18, 977–983 (2003). https://doi.org/10.1111/j.1525-1497.2003.20414.x
Issue Date:
DOI: https://doi.org/10.1111/j.1525-1497.2003.20414.x