Abstract
The Flint Water Crisis—due to changes of water source and treatment procedures—has revealed many unsolved social, environmental, and public health problems for US drinking water, including opportunistic premise plumbing pathogens (OPPP). The true health impact of OPPP, especially in vulnerable populations such as the elderly, is largely unknown. We explored 108 claims in the largest US national uniformly collected data repository to determine rates and costs of OPPP-related hospitalizations. In 1991–2006, 617,291 cases of three selected OPPP infections resulted in the elderly alone of $0.6 billion USD per year of payments. Antibiotic resistance significantly increased OPPP illness costs that are likely to be underreported. More precise estimates for OPPP burdens could be obtained if better clinical, microbiological, administrative, and environmental monitoring data were cross-linked. An urgent dialog across governmental and disciplinary divides, and studies on preventing OPPP through drinking water exposure, are warranted.
Similar content being viewed by others
Introduction
The 2010 Report of the national Waterborne Disease and Outbreak Surveillance System (WBDOSS)—established to document waterborne disease outbreaks reported by local, state, and territorial health departments—urged serious attention be paid to the growing proportion of outbreaks associated with premise plumbing deficiencies in public water systems, noting the increasing importance of Legionella since its 2001 inclusion in WBDOSS.1 According to the 2010 Report, between 2001 and 2006 Legionella was responsible for 29 per cent of the 84 drinking water outbreaks, and 80 per cent of the 15 drinking water-related deaths. Most of these legionellosis outbreaks occurred in hospitals, health care facilities, and nursing homes. The 2015 Report stated that in 2011–2012, Legionella in drinking water systems and deficiencies of untreated groundwater accounted for 72.4 per cent of all outbreak-associated cases.2
The ongoing Flint Water Crisis [Flint, Michigan] was triggered by changes of water source and a lack of corrosion control treatment. The corrosive water mobilized lead, leading to the lead poisoning of Flint residents.3 Less well known is that a simultaneous outbreak of 87 cases of Legionnaires’ disease occurred in Genesee County, which includes Flint, with 10 deaths.4 In addition to lead, the corrosive water may have mobilized iron from the pipes. Furthermore, there were several total coliform violations in Flint, which may also have been indicative of the lack of adequate chlorine residual. The residual chlorine disinfectant in Flint water may have been depleted by reactions with iron, allowing OPPP such as Legionella to flourish. Iron is believed to support the growth of Legionella bacteria.5
First recognized in Philadelphia in 1976,6,7 Legionella is the most frequently recognized OPP pathogen in both community and hospital settings. There is increasing awareness that the ‘normal microbial inhabitants’ of premise (household or building) plumbing may account for a greater proportion of waterborne disease outbreaks, and serious community and hospital-acquired infections, than previously envisioned. Modern water treatment facilities successfully eliminate almost all the common fecal-borne pathogens found in source waters. Yet in building water systems, microorganisms such as Legionella, Pseudomonas, and atypical mycobacteria can live on trace amounts of organic matter, attach to pipe inner surfaces, and grow as microbial biofilms encased in an extracellular polysaccharide (EPS) matrix.8–11 The negative charge and hydrophobic nature of the EPS enables the biofilm to concentrate ions and dissolved organic carbon from the oligotrophic bulk fluid, thus permitting organisms to grow in low nutrient conditions. Some free-living amoebae inhabiting water are highly resistant to chemical and physical disinfection, particularly in their dormant cyst stage, and can easily withstand the high temperature disinfection treatments currently used in healthcare facility (hospital) settings.8 Biofilms represent an important ecological niche, and biofilm infections are implicated in more than 80 per cent of hospital-associated and prosthetic device infections.9,10 Furthermore, water aerosolization becomes an important mode of transmission for legionellosis and other emerging infections. The ability of OPPP to grow as microbial biofilms in water provides them selective advantages, including (1) growth in low nutrient conditions, (2) resistance to antibiotics and disinfectants, (3) high metabolic and phenotypic diversity, enabling them to withstand environmental stresses (pH, UV, low oxygen), (4) horizontal gene transfer of antibiotic resistance and virulence genes, and (5) efficient transmission via ingestion, aerosols, and contact.8,10,12,13 A recent study of OPPP in chloraminated drinking water distribution systems using quantitative PCR methods revealed a high occurrence of Legionella spp. (≥69 per cent) and non-tuberculous mycobacteria (100 per cent), a lower prevalence of L. pneumophila (≤20 per cent) and M. avium (≤33.3 per cent), and uncommon detection of Pseudomonas aeruginosa (≤13.3 per cent).14
In this communication, we explored the burden and cost of OPPP hospitalizations associated with diagnosis of Legionella pneumophila, Mycobacterium avium, and Pseudomonas aeruginosa, as well as reported drug resistance, and reported charges to and reimbursements from Medicare.
Materials and Methods
We have used a data repository of 108 hospitalization records to describe emerging trends in hospitalization rates due to various infectious agents, and to determine the effects of environmental exposures at the national level.15 – 18 The national data repository of medical claims, maintained by the US Centers for Medicare and Medicaid Services (CMS), offers a universal, uniform, and near-exhaustive coverage of US Medicare beneficiaries aged 65 and older. It contains information on age, ZIP code of residence, date of admission, direct charges to and reimbursements from Medicare (Part B), and up to 10 diagnostic codes based on International Classification of Disease, 9th Revision, Clinical Modification (ICD-9-CM).
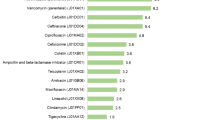
We abstracted hospitalization records for infections with three model OPPP: Legionella pneumophila, Mycobacterium avium, and Pseudomonas aeruginosa,12 using ICD-9CM codes: 482.1, 482.81, 482.84, and 031.x reported in primary or secondary diagnostic fields (see Table 1) during a 16-year period, from January 1st 1991 to December 31st 2006 among US residents aged 65 and older. We then tabulated all abstracted cases based on drug resistance (ICD:V09) reported in any diagnostic fields. ICD codes for infections with microorganisms resistant to cephalosporins and other B-lactam antibiotics (V09.1), macrolides (V09.2), tetracyclines (V09.3), and aminoglycosides (V09.4) were included in total drug resistance counts; ICD codes for infections with microorganisms resistant to quinolones and fluoroquinolones (V09.5), other specified antimycobacterial agents (V09.7), and other specified drugs without resistance to multiple drugs (V09.80) were aggregated and cross-tabulated. We calculated the proportions of cases with multiple drug resistance, denoted by additional subcoding (V09.x1), to the number of cases with reported resistance by V09.5, V09.7, V09.8, and V09.9.
Results
Of 18,202,047 hospitalizations due to pneumonia, 2,909,843 (16 per cent) were explicitly coded as bacterial pneumonia (ICD:482) that allowed detailed subcoding. A unique code (ICD:482.84) widely used by 1997 allowed the abstraction of 7,933 records for Legionnaires’ disease. (Prior to 1997, Legionnaires’ disease cases were likely coded under ICD:482.8 that included all anaerobic and facultative gram-negative organisms.) We also identified 544,643 records of hospitalization in the elderly due to Pseudomonas (ICD:482.1) and 15,861 records of hospitalization due to gram-negative anaerobes (ICD:482.81), which contributed 19 per cent to the “Other bacterial pneumonia” category. To minimize misclassification, 240 cases with ICD code 482 that lacked detailed subcoding, were not included in the analysis.
We found 48,854 hospitalization records associated with non-tuberculous mycobacteria (NTM) (ICD:031). This code was further divided into subcategories including pulmonary infection caused by NTMs including Mycobacterium avium-intracellulare [‘Battey bacillus’], that contributed 71 per cent of NTM-related cases (ICD:031.0). The rest (29 per cent) was associated with cutaneous infections caused by NTMs (ICD:031.1), disseminated, or blood stream infections caused predominately by Mycobacterium avium-intracellulare (MAI) and Mycobacterium avium-intracellulare complex (MAC) bacteremia (ICD:031.2), other specified mycobacterial diseases (ICD:031.8), and unspecified diseases due to mycobacteria or an atypical mycobacterium infection “not otherwise specified” (031.9).
We identified 11,861 cases of drug resistance for one pathogen, and 53 cases in which two pathogens were implicated in positive resistance tests. Drug resistance was reported for each diagnostic code and ranged from 1.68 per cent for Pseudomonas pulmonary infections, to 1.05 per cent for NTM pulmonary infections, and 0.6 per cent for Legionnaires’ disease (Table 1). One alarming finding was the magnitude of observed multidrug resistance, which reached 50 per cent for fluoroquinolones and antimycobacterial agents.
Overall, reported drug resistance led to a 32.8 per cent increase in per case charges to Medicare. The estimated payments for Pseudomonas aeruginosa totaled $8.8 billion USD over the 15 years, with a high mean per case differential payment of $14,510 ($62,440 resistant, versus $47,930 no resistance, Δ = $14,510 or 30.3 per cent). Of note, this significant difference in charges submitted to Medicare for resistant cases was not reflected in actual payments that were made (Table 1).
Discussion
We found the economic burden of three OPPP infections in persons aged ≥65 years averaged $0.6 billion per year over a 15-year period (1991–2006) in reimbursed payments to hospitals. Given these costs, recent outbreaks of Legionnaire’s disease, and the rising incidence of hospital-acquired OPPP illnesses, enhanced identification and reporting of these infections is warranted.
There has been a substantial increase in Pseudomonas infections in the last decade. The US Centers for Disease Control and Prevention (CDC) recently reported19 that this infection accounts for 51,000 cases (8 per cent) of healthcare-associated infections per year. More than 6000 (13 per cent) of these cases were multidrug-resistant infections with >70 per cent increased cost compared to non-resistant infections.20 Pseudomonas has been linked to waterborne biofilm infections, particularly in burn and cystic fibrosis patients, and infections involving solutions used for surface sterilization, indwelling catheters, bronchoscopes, hot tubs, and sink traps and aerosolizers.9,10 This increase in reported Pseudomonas infections has been demonstrable despite incomplete reporting for key OPPP organisms.
The increase in legionellosis is concerning. As reported by the CDC, during 2000–2011, passive surveillance for legionellosis in the United States demonstrated a 249 per cent increase in crude incidence, from 0.39 to 1.36 cases per 100,000 persons.21 The risk factors, causal links, preventive measures against drug resistance, and control options are far from being defined. Microbiology laboratories report only incident cases of Legionella pneumophila and M. tuberculosis complex to public health authorities. They do not report atypical mycobacteria (such as M. avium) or Pseudomonas. Most cases of Legionella are diagnosed by a rapid urinary assay for Legionella pneumophila serogroup 1 antigen (which accounts for 80 per cent of cases). In some US states, results are sent to the public health authorities via a secure electronic mechanism. Otherwise, cultures of respiratory secretions are plated on selective media, and may be sent to reference laboratories for identification and antibiotic sensitivity testing. If a reportable organism is cultured, the isolate is forwarded to the state reference laboratory. Furthermore, OPPP may also disproportionally affect immunocompromised elderly, and those with HIV.24 Yet OPPP are rarely tested for in community settings, even in severely ill patients. Thus the true incidence is likely to be substantially underestimated, given the limitation of available data and inpatient hospital care practices. Indeed, 40 per cent of Legionella cases reported to the CDC 2000–200925 occurred in persons aged ≥60, suggesting that the true clinical and economic burden may be 2–3 times larger than our estimate.
We estimated annual charges to Medicare for Legionnaires’ disease and NTM infections as $339,970,596 and $88,008,503, respectively. Our estimates for the per case costs for these two infections ($42,855 and $27,022, respectively) were similar to the estimates provided by others for hospitalization costs per episode of $33,336 and $25,985.22 As expected, the reimbursed payments per case were smaller than the charges. Both payments and charges were ~10–40 per cent higher for resistant than for non-resistant infections. In 1991–2006, the total payment to hospitals for the three model OPPP-related infections in this dataset was about $9 billion for more than 41,000 cases per annum. The annual costs may now exceed $2 billion for 80,000 cases per year.8,22 Our data and conclusions are consistent with analyses of infections by resistant versus antimicrobial-susceptible organisms. These analyses have found greater hospital charges, longer lengths of stay, and increased risk of death.23
While the proportion of hospitalizations with reported resistance was fewer than 2 per cent, we found that the incidence of multiple drug resistance was high. This may be the result of selection for resistance in hospital-acquired infections due in part to the ability of these organisms to grow in a biofilm community where transfer of genetic elements (antibiotic resistance genes, phages, plasmids) occurs.9,10 Water stress conditions such as low, non-killing levels of disinfectants and low nutrients induce upregulation of transferable elements.9,10,12 We differentiate multidrug resistance from the ‘intrinsic’ resistance these OPPP have to penicillin (V09.0) and vancomycin (V09.8), that ranged between 69 per cent and 91 per cent, as expected. We note that vancomycin antibiotic resistance was reported in 91 per cent of our identified cases, suggesting that in 9 per cent sensitivity to vancomycin was present. This would occur if the reported resistance were for a non-OPPP second organism such as Staphylococcus aureus, a common “second infection” bacterium. We thus attribute ~9 per cent to multiple organism infections for which different-organism resistance coding might occur. This highlights the limitations of data collection as it currently stands.
A restricted coding for antimicrobial resistance that captures exclusively the primary pathogen rather than all tested is a serious limitation of administrative databases. Another limitation of this study is that historic administrative hospitalization records are substantially inferior to direct clinical or microbiological testing results, and antibiotic resistance reporting is likely to be incomplete in administrative records. The reporting improved in the last decade, yet the incentives for hospitals to test are likely to be insufficient. For example, in 2013, the CDC estimated that 6700 hospital-acquired infections with MDR Pseudomonas occur per year in all age groups, based upon sentinel laboratory site reporting data. In contrast, we found 8998 Pseudomonas pneumonia in CMS records that reported resistance during 1991–2006, equivalent to ~600 cases per year. We suspect this is a substantial undercount. Similar discrepancies are noted for Legionella. In 2000–2009, adults over 60 y.o. had contributed half of 22,418 cases of legionellosis, which is equivalent to ~1120 annual reports to the CDC25 and twice of ~530 annual records we had identified in the CMS database. We also found a pattern of higher charges for resistant infections, but not a consistent pattern of increased payments (See Table 1). If in fact true costs were higher for antimicrobial-resistant infections than for susceptible ones, but payments are not significantly different, it is very likely that there have been little or no incentive for hospitals to test for resistant organisms.
Only over the past decade has there been a stronger mandate to report healthcare-associated infections (HAI) to the CDC’s National Healthcare Safety Network (NHSN).19,26 These reports include infections of surgical sites, bloodstream intravenous catheter lines, urinary catheters, and ventilator-associated pneumonias obtained through CMS hospital inpatient quality reporting programs. With new ICD coding rules implemented in 2015, reporting of HAI will be substantially improved. The ICD-10 rules require reporting specific infection locations, the organism, and resistance for certain bacteria, including methicillin-resistant Staphylococcus aureus (MRSA), and vancomycin-resistant enterococci (VRE). Hospitals also have additional financial incentives to report, as they receive higher reimbursements for treating drug-resistant than drug-sensitive infections.
A strength of this study is that it used a nationwide database of >108 hospitalization records that comprehensively collates data from >96 per cent of the US elderly. Benefits accrue to linking administrative data with more accurate clinical or microbiological data. The ICD-10 changes are a first step to creating better cross-link across various reporting strategies. Recent hospitalization administrative records are likely to reflect increased vigilance to both community- and hospital-acquired infections.
While reporting of OPPP was imperfect during 1991–2006, we nonetheless found highly significant differences in costs when treating antibiotic resistant infections. Our central finding, that resistant OPPP organisms are associated with higher economic burden is, if anything, an underestimate based on the number of recorded cases. If antibiotic resistance was not consistently recorded, then the ‘true’ economic burden of resistance per episode would be underestimated, because the category of non-resistant infections may contain some episodes with resistant organisms.
What to do next? Studies examining the epidemiology and microbial ecology of OPPP could inform thoughtful strategies to reliably reduce OPPP human disease. Targeted investigations should examine common ecological factors shared by OPPP, such as biofilm formation. Implementing plumbing rules that eliminate or reduce OPPP organisms in water systems of healthcare facility buildings or in the homes of at-risk persons (such as those with cystic fibrosis or immunocompromised) may prove most effective.13 The long-term effectiveness, safety, and cost associated with coatings that prevent biofilm formation either by chemical modification or micropatterned surfaces within the plumbing pipes could be further examined. Should they be used in high-risk surgical or hospital settings?9,10,27
Water distribution systems across the US are aging, which will increase their susceptibility to OPPP contamination. Budgets for state and federal water regulators have decreased in real dollar terms. The annual budget of the EPA’s Office of Ground Water and Drinking Water declined 15 per cent from 2006 to 2015. It lost over 10 per cent of its employees. In 2013, the Association of State Drinking Water Administrators reported that “federal officials had slashed drinking-water grants, 17 states had cut drinking-water budgets by more than a fifth, and 27 had cut spending on full-time employees,’’ with “serious implications for states’ ability to protect public health”.28
Premise plumbing systems are generally unregulated and fall outside the purview of most federal (e.g., Safe Drinking Water Act) and state regulatory agencies. In combination, these factors will inevitably lead to inconsistent monitoring and reporting despite warnings to the contrary.1 The rise of OPPP infections is a clear call for an urgent dialog across disciplinary boundaries and government agencies, stakeholders, and policy makers.
References
Craun, G.F., Brunkard, J.M., Yoder, J.S., Roberts, V.A., Carpenter, J., Wade, T. et al (2010) Causes of outbreaks associated with drinking water in the United States from 1971 to 2006. Clinical Microbiology Reviews 23(3): 507–528.
Beer, K.D., Gargano, J.W., Roberts, V.A., Hill, V.R., Garrison, L.E., Kutty, P.K. et al (2015) Surveillance for Waterborne Disease Outbreaks Associated with Drinking Water - United States, 2011–2012. MMWR Morbidity and Mortality Weekly Report 14;64(31):842–8.
Hanna-Attisha, M., LaChance, J., Sadler, R.C. and Champney, Schnepp A. (2016) Elevated blood lead levels in children associated with the flint drinking water crisis: A spatial analysis of risk and public health response. American Journal of Public Health 106(2): 283–290.
Al-Hajal, K. (2016) 87 cases, 10 fatal, of Legionella bacteria found in Flint area; connection to water crisis unclear. The Flint Journal via MLive. http://www.mlive.com/news/detroit/index.ssf/2016/01/legionaires_disease_spike_disc.html.
Rose, J.B. and Wiant, C. (2016) Legionella in Flint’s Drinking Water. Water Quality and Health. http://www.waterandhealth.org/legionella-flints-drinking-water/.
Fraser, D.W., Tsai, T.R., Orenstein, W., Parkin, W.E., Beecham, H.J., Sharrar, R.G. et al (1977) Legionnaires’ disease. New England Journal of Medicine 297(22): 1189–1197.
McDade, J.E., Shepard, C.C., Fraser, D.W., Tsai, T.R., Redus, M.A., Dowdle, W.R. et al (1977) Legionnaires’ disease. New England Journal of Medicine 297(22): 1197–1203.
Falkinham, J.O., Pruden, A. and Edwards, M. (2015) Opportunistic premise plumbing pathogens: Increasingly important pathogens in drinking water. Pathogens 4(2): 373–386.
Kleinpell, R.M., Munro, C.L. and Giuliano, K.K. (2008) Targeting health care-associated infections: Evidence-based strategies. In R. G. Hughes (Ed.), Patient Safety and Quality: An Evidence-Based Handbook for Nurses. Rockville: Agency for Healthcare Research and Quality.
Percival, S.L., Suleman, L., Vuotto, C. and Donelli, G. (2015) Healthcare-associated infections, medical devices and biofilms: Risk, tolerance and control. Journal of Medical Microbiology 64: 323–334.
Zobell, C.E. and Grant, C.W. (1943) Bacterial utilization of low concentrations of organic matter. Journal of Bacteriology 45(6): 555–564.
Falkinham, J.O., 3rd, Hilborn, E.D., Arduino, M.J., Pruden, A. and Edwards, M.A. (2015) Epidemiology and Ecology of Opportunistic Premise Plumbing Pathogens: Legionella pneumophila, Mycobacterium avium, and Pseudomonas aeruginosa. Environmental Health Perspectives 123(8): 749–758.
Krageschmidt, D.A., Kubly, A.F., Browning, M.S., Wright, A.J., Lonneman, J.D., Detmer, M.J. et al (2014) A comprehensive water management program for multicampus healthcare facilities. Infection Control and Hospital Epidemiology 35(5): 556–563.
Wang, H., Edwards, M., Falkinham, J.O., 3rd and Pruden, A. (2012) Molecular survey of the occurrence of Legionella spp., Mycobacterium spp., Pseudomonas aeruginosa, and amoeba hosts in two chloraminated drinking water distribution systems. Applied and Environment Microbiology 78(17): 6285–6294.
Chui, K.K., Webb, P., Russell, R.M. and Naumova, E.N. (2009) Geographic variations and temporal trends of Salmonella-associated hospitalization in the U.S. elderly, 1991–2004: a time series analysis of the impact of HACCP regulation. BMC Public Health 9: 447.
Jagai, J. and Naumova, E.N. (2009) Clostridium difficile-associated disease in the elderly, United States. Emerging Infectious Diseases 15(2): 343–344.
Mor, S.M., DeMaria, A., Jr., Griffiths, J.K. and Naumova, E.N. (2009) Cryptosporidiosis in the elderly population of the United States. Clinical Infectious Diseases 48(6): 698–705.
Naumova, E.N., Egorov, A.I., Morris, R.D. and Griffiths, J.K. (2003) The elderly and waterborne Cryptosporidium infection: gastroenteritis hospitalizations before and during the 1993 Milwaukee outbreak. Emerging Infectious Diseases 9(4): 418–425.
Centers for Disease Control and Prevention. (2011) Association of State and Territorial Health Officials (ASTHO). Eliminating Healthcare-Associated Infections: State Policy Options. https://www.cdc.gov/hai/pdfs/toolkits/toolkit-HAI-POLICY-FINAL_01-2012.pdf.
Centers for Disease Control and Prevention. (2016) Antibiotic resistance threats in the United States, 2013. http://www.cdc.gov/drugresistance/threat-report-2013/.
Adams, D.A., Jajosky, R.A., Ajani, U., Kriseman, J., Sharp, P., Onwen, D.H. et al (2014) Summary of notifiable diseases–United States, 2012. MMWR Morbidity and Mortality Weekly Report 61(53): 1–121.
Collier, S.A., Stockman, L.J., Hicks, L.A., Garrison, L.E., Zhou, F.J. and Beach, M.J. (2012) Direct healthcare costs of selected diseases primarily or partially transmitted by water. Epidemiology and Infection 140(11): 2003–2013.
Neidell, M.J., Cohen, B., Furuya, Y., Hill, J., Jeon, C.Y., Glied, S. et al (2012) Costs of healthcare- and community-associated infections with antimicrobial-resistant versus antimicrobial-susceptible organisms. Clinical Infectious Diseases 55(6): 807–815.
Mor, S.M., Aminawung, J.A., Demaria, A., Jr. and Naumova, E.N. (2011) Pneumonia and influenza hospitalization in HIV-positive seniors. Epidemiology and Infection 9: 1317–1325.
Centers for Disease Control and Prevention. (2011) Legionellosis – United States, 2000–2009. MMWR Morbidity and Mortality Weekly Report 60(32): 1083–1086.
Scott, R.D. (2009) The direct medical costs of healthcare-associated infections in U.S. Hospitals and the benefits of prevention. http://www.cdc.gov/hai/pdfs/hai/scott_costpaper.pdf.
Behlau, I., Mukherjee, K., Todani, A., Tisdale, A.S., Cade, F., Wang, L. et al (2011) Biocompatibility and biofilm inhibition of N, N-hexyl, methyl-polyethylenimine bonded to Boston Keratoprosthesis materials. Biomaterials 32(34): 8783–8796.
Wines, M. and Schwartz, J. (2016) Unsafe lead levels in tap water not limited to flint. New York Times. http://www.nytimes.com/2016/02/09/us/regulatory-gaps-leave-unsafe-lead-levels-in-water-nationwide.html?_r=0.
Acknowledgments
The use of Centers for Medicare and Medicaid Services hospitalization records was enabled by the National Institutes of Health Grants R01-ES013171, U19-AI062627, and NO1-A150032.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Naumova, E.N., Liss, A., Jagai, J.S. et al. Hospitalizations due to selected infections caused by opportunistic premise plumbing pathogens (OPPP) and reported drug resistance in the United States older adult population in 1991–2006. J Public Health Pol 37, 500–513 (2016). https://doi.org/10.1057/s41271-016-0038-8
Published:
Issue Date:
DOI: https://doi.org/10.1057/s41271-016-0038-8