Abstract
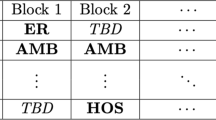
Internal Medicine residency programmes have traditionally been structured around monthly or 4-week blocks where a different rotation is assigned to each block over the year. A subset of those rotations carry the requirement of one or two half-day sessions of clinic duty per week. In the last several years, a growing number of Internal Medicine residency programmes have moved away from this traditional structure and have adopted an ‘X+Y’ template, where the resident spends X weeks on a rotation without clinic duty and then Y weeks mostly in clinic. This paper addresses the ‘4+1’ annual block scheduling problem as adopted by the Department of Medicine at the University of Texas Health Science Center in San Antonio (UTHSC-SA). We believe it is the first attempt to investigate the problem formally; specifically, we develop a series of optimization models that can be used to construct individual block schedules for the academic year and to assign clinic sessions to the residents during their ambulatory week. (At UTHSC-SA, Internal Medicine residents are divided into five groups to match the 4+1 pattern, and scheduled so only one group at a time has clinic responsibilities each of the 52 weeks.) The objective is to balance the workload during the half-day clinic sessions and to ensure that each resident receives roughly the same training experiences over their programme. Once the blocks and groups are known, a second optimization problem is solved to determine individual clinic session assignments. The basic model takes the form of a mixed-integer program but was not solvable with commercial software. After decomposing it into two parts, we were able to find optimal solutions to the original problem. Complexity results are provided for the problems solved. Compared with current practice, our decomposition approach was seen to offer improved schedules with respect to the workload balance objective for each of the five resident groups.


Similar content being viewed by others
References
Accreditation Council for Graduate Medical Education (ACGME) (2015). Common Program Requirements, https://www.acgme.org/acgmeweb/.
Alfares HK (2007). Operator staffing and scheduling for an IT-help call centre. European Journal of Industrial Engineering 1 (4): 414–430.
Aykin T (1996). Optimal shift scheduling with multiple break windows. Management Science 42 (4): 5–602.
Bard JF and Purnomo HW (2005). Preference scheduling for nurses using column generation. European Journal of Operational Research 164 (2): 510–534.
Bard JF, Shu Z and Leykum L (2013). Monthly clinic assignments for internal medicine housestaff. IIE Transactions on Healthcare Systems Engineering 3 (4): 207–239.
Bard JF, Shu Z and Leykum L (2014). A network approach for monthly scheduling of residents in primary care clinics. Operations Research for Health Care 3 (4): 200–2014.
Bard JF, Shu Z, Morrice DJ and Leykum L (2016a forthcoming). Constructing block scheduling for internal medicine residences. IIE Transactions on Healthcare Systems Engineering.
Bard JF, Shu Z, Morrice DJ, Leykum L and Poursani R (2016b forthcoming). Block scheduling for family medicine residency programs. IIE Transactions on Operations Engineering & Analytics.
Beaulieu H, Ferland J, Gendron B and Michelon P (2000). A mathematical programming approach for scheduling physicians in the emergency room. Health Care Management Science 3 (3): 193–200.
Bechtold S and Jacobs LW (1990). Implicit modeling of flexible break assignments in optimal shift scheduling. Management Science 36 (11): 1339–1351.
Beliën J and Demeulemeester E (2006). Scheduling trainees at a hospital department using a branch-and-price approach. European Journal of Operational Research 175 (1): 258–278.
Berrada I, Ferland JA and Michelon P (1996). A multi-objective approach to nurse scheduling with both hard and soft constraints. Socio-Economic Planning Sciences 30 (3): 183–193.
Brunner JO, Bard JF and Kolisch R (2009). Flexible shift scheduling of medical residents. Health Care Management Science 12 (3): 285–305.
Brusco MJ and Jacobs LW (2000). Optimal models for meal-break and start-time flexibility in continuous tour scheduling. Management Science 46 (12): 1630–1641.
Burke EK, De Causmaecker P, Berghe GV and Van Landeghem H (2004). The state of the art of nurse rostering. Journal of Scheduling 7 (6): 441–499.
Cabana MD and Jee SH (2004). Does continuity of care improve patient outcomes? Journal of Family Practice 53 (12): 974–980.
Carter MW and Lapierre SD (2001). Scheduling emergency room physicians. Health Care Management Science 4 (4): 347–360.
Chaudhry SI et al (2013). Moving forward in GME reform: A 4+1 model of resident ambulatory training. Journal of General Internal Medicine 28 (8): 1100–1104.
Dexter F, Wachtel RE, Epstein RH, Ledolter J and Todd MM (2010). Analysis of operating room allocations to optimize scheduling of specialty rotations for anesthesia trainees. Anesthesia & Analgesia 111 (2): 520–524.
Ernst AT, Jiang H, Krishnamoorthy M and Sier D (2004). Staff scheduling and rostering: A review of applications, methods and models. European Journal of Operational Research 153 (1): 3–27.
Franz LS and Miller JL (1993). Scheduling medical residents to rotations: Solving large-scale multiperiod staff assignment problem. Operations Research 41 (2): 269–279.
Garey MR and Johnson DS (1979). Computers and Intractability: A Guide to the Theory of NP-Completeness. W.H. Freeman: New York.
Guo J, Morrison DR, Jacobson SH and Jokela JA (2014). Complexity results for the basic residency scheduling problem. Journal of Scheduling 17 (3): 211–223.
Heist K, Guese M, Nikels M, Swigris R and Chacko K (2014). Impact of 4+1 block scheduling on patient care continuity in resident clinic. Journal of General Internal Medicine 29 (8): 1195–1199.
Kellogg DL and Walczak S (2007). Nurse scheduling: From academia to implementation or not? Interfaces 37 (4): 355–369.
Mariotti JL, Shalaby M and Fitzgibbons JP (2010). The 4:1 schedule: A novel template for internal medicine residencies. Journal of Graduate Medical Education 2 (4): 541–547.
Ovchinnikov A and Milner J (2008). Spreadsheet model helps to assign medical residents at the University of Vermont’s college of medicine. Interfaces 38 (4): 311–323.
Ozkarahan I (1994). A scheduling model for hospital residents. Journal of Medical Systems 18 (5): 251–265.
Rekik M, Cordeau J-F and Soumis F (2010). Implicit shift scheduling with multiple breaks and work stretch duration restrictions. Journal of Scheduling 13 (1): 49–75.
Rodriguez HE, Turner JP, Speicher P, Daskin MS and DaRosa DA (2010). A model for evaluating resident education with a focus on continuity of care and educational quality. Journal of Surgical Education 67 (6): 352–358.
Saultz JW and Lochner J (2005). Interpersonal continuity of care and care outcomes: A critical review. Annals of Family Medicine 3 (2): 159–166.
Sherali HD, Ramahi MH and Saifee QJ (2002). Hospital resident scheduling problem. Production Planning and Control 13 (2): 220–233.
Topaloglu S (2006). A multi-objective programming model for scheduling emergency medicine residents. Computers & Industrial Engineering 51 (3): 375–388.
Turner JP, Rodriguez HE, Daskin MS, Mehrotra S, Speicher P and DaRosa DA (2012). Overcoming obstacles to resident-patient continuity of care. Annals of Surgery 255 (4): 618–622.
Turner JP, Kim K, Mehrotra S, DaRosa DA, Daskin MS and Rodriguez HE (2013). Using optimization models to demonstrate the need for structural changes in training programs for surgical medical residents. Health Care Management Science 16 (3): 217–227.
Acknowledgements
This work was supported by grant # 153239 from the University of Texas Office of the Executive Chancellor for Health Affairs.
Author information
Authors and Affiliations
Corresponding author
Appendix
Rights and permissions
About this article
Cite this article
Bard, J., Shu, Z., Morrice, D. et al. Annual block scheduling for internal medicine residents with 4+1 templates. J Oper Res Soc 67, 911–927 (2016). https://doi.org/10.1057/jors.2015.109
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1057/jors.2015.109