Abstract
Bushfires are increasing in frequency and severity worldwide. Bushfire smoke contains organic/inorganic compounds including aldehydes and acrolein. We described suppressive effects of tobacco smoke on the phagocytic capacity of airway macrophages, linked to secondary necrosis of uncleared apoptotic epithelial cells, persistence of non-typeable H. influenzae (NTHi), and inflammation. We hypothesised that bushfire smoke extract (BFSE) would similarly impair macrophage function. THP-1 or monocyte-derived macrophages (MDM) were exposed to 1–10% BFSE prepared from foliage of 5 common Australian native plants (genus Acacia or Eucalyptus), or 10% cigarette smoke extract (CSE). Phagocytic recognition receptors were measured by flow cytometry; pro-inflammatory cytokines and caspase 1 by immunofluorescence or cytometric bead array; viability by LDH assay; and capsase-3/PARP by western blot. BFSE significantly decreased phagocytosis of apoptotic cells or NTHi by both THP-1 macrophages and MDM vs air control, consistent with the effects of CSE. BFSE significantly decreased MDM expression of CD36, CD44, SR-A1, CD206 and TLR-2 and increased active IL-1β, caspase-1 and secreted IL-8. BFSE dose-dependently decreased THP-1 macrophage viability (5-fold increase in LDH at 10%) and significantly increased active caspase-3. BFSE impairs macrophage function to a similar extent as CSE, highlighting the need for further research, especially in patients with pre-existing lung disease.
Similar content being viewed by others
Introduction
Bushfire severity and frequency is increasing worldwide and further increases are predicted. One study comparing the incidence of major fires from 1970 to 2012 with precipitation and land-surface data confirmed an increase in bushfire activity associated with prolonged droughts1. Similar trends have been observed in Australia where average temperatures have risen by 0.9 °C since 1910 and average winter rainfall has decreased by 15–17% in southern Australia2. The increased frequency and severity of bushfires taken together with a predicted yearly occurrence of severe fire danger rated days, increasing by up to 300% by 20503, presents a greater risk of smoke exposure to the population. The United States urban interface with wildland areas increased by 52% from 1990 to 20004. This increase in bushfire frequency, coupled with global populations encroaching on forest areas, means that large communities are increasingly required to co-exist with both unplanned and prescribed wildfires5.
The interface of urban epidemiological studies have found significant associations between bushfire smoke exposure and both emergency department presentations6,7 and hospital admissions8,9 for respiratory morbidities. An Australian based study conducted by Martin et al.9,10 reported increased hospital admissions for pre-existing respiratory morbidities in association with bushfire events; 13% for chronic obstructive pulmonary disease (COPD) and 12% for asthma. This is supported by a California based study where admissions were increased by 4.8% for COPD and 6.8% for asthma8. Furthermore, healthy subjects exposed to higher levels of particulate matter (PM) during a Southeast Asian forest fire event exhibited increased systemic inflammatory responses, including increased band neutrophil counts11 and elevated cytokines in peripheral blood12. Respirable particulate matter from bushfire events in California was reported to elicit oxidative stress and inflammatory responses. Human bronchial epithelial cells exposed to PM in vitro expressed significantly more IL-8 and IL-1β13 while bronchoalveolar lavage from exposed mice contained higher levels of MIP-1α and IP-1014.
Bushfire smoke contains a range of organic and inorganic components such as respirable particulate matter, aldehydes, acrolein, and carbon monoxide15. Very little is known about its effects on airway epithelial cells and alveolar macrophages that represent the frontline immunological barrier to potentially toxic particles. One study showed that California bushfire particulate matter alone resulted in reduced number of lung macrophages in mice16 and another found increased macrophage cell death in vitro17. In contrast, the negative effects of tobacco smoke on these cell types has been well-described. We and others reported that cigarette smoke caused increased apoptosis of bronchial epithelial cells with an associated defect in the capacity of neighbouring macrophages to phagocytose these apoptotic cells (efferocytosis)18,19,20,21. Similar defects were noted in patients with chronic lung diseases including COPD, severe asthma, and childhood non-CF bronchiectasis22,23,24. This defect was associated with secondary necrosis of the uncleared material, potentially leading to release of toxic cell contents, perpetuating inflammation and further tissue damage19,25. We also found that cigarette smoke exposure inhibited the capacity of alveolar macrophages to phagocytose bacteria, including non-typeable H. influenzae (NTHi), a common coloniser of the airway in chronic lung diseases that is associated with significant morbidity. To our knowledge, the effects of bushfire smoke on macrophage phagocytic function has not been previously described. We thus hypothesised that exposure to a bushfire smoke extract (BFSE) causes defects in macrophage function that parallel our findings with cigarette smoke extract (CSE).
Results
BFSE suppressed macrophage phagocytic capacity
The capacity of THP-1 macrophages and MDM to efferocytose apoptotic HBE cells was significantly decreased after 24 h of exposure to BFSE compared to the air treated control. THP-1 macrophage efferocytosis was significantly (p = 0.012) decreased from 13.8% by control cells to 9.5% and 8.8% with 1% and 5% BFSE, respectively (Fig. 1A). MDM efferocytic capacity was decreased from 21.9% to 17.1% and 10.6% (p = 0.031), for 1% and 5% BFSE, respectively (Fig. 1B). For efferocytosis, MFI was not significantly changed by any treatment (Supplementary Fig. 1).
BFSE suppressed macrophage phagocytic capacity. THP-1 macrophage and MDM cells exposed to air control, 1% or 5% BFSE, or 10% CSE for 24 h were cultured with apoptotic epithelial cells and NTHi. Efferocytosis of apoptotic epithelial cells by THP-1 macrophage (A) and MDM (B) and phagocytosis of NTHi by THP-1 macrophage (C) and MDM (D) were assessed by flow cytometry and measured as the percentage of cells positive for internalisation of targets (THP-1 n = 4, MDM n = 6). *p < 0.05.
The capacity of THP-1 macrophages and MDM to phagocytose NTHi was also significantly reduced following 24 h exposure to BFSE. THP-1 macrophage exposure to 1% or 5% BFSE decreased phagocytosis from 12.9% to 9.9% and 9.9% respectively (p = 0.012, Fig. 1C). Exposure of MDM to 1% or 5% BFSE resulted in a decrease in phagocytosis from 20.8% to 16.2% and 13.3% (p = 0.031), respectively (Fig. 1D). Observed decreases in efferocytic and phagocytic function after 24 h exposure to 5% BFSE were to a similar extent as with 10% CSE treatment for 24 h for both THP-1 macrophage and MDM. For phagocytosis, a significant reduction in MFI was noted in the presence of both 1% and 5% BFSE (Supplementary Fig 1).
BFSE alters phagocytic recognition receptors
Effective phagocytosis of bacteria or efferocytosis by macrophages is dependent on the expression of surface recognition receptors. To investigate the effects of BFSE or cigarette smoke on the percentage of cells expressing thrombospondin receptor (CD36), hyaluronan receptor (CD44), scavenger receptor (SR)-A1 (CD204), mannose receptor (CD206) and toll-like receptors (TLR) −2/4, MDM were exposed to 1% or 5% BFSE and 10% CSE for 24 h, then receptors measured using flow cytometry. There were no significant effects of 1% BFSE on any of the receptors tested (Fig. 2). Both 5% BFSE and 10% CSE induced a significant decrease in the percentage of cells expressing CD36, CD44, CD204, CD206 and TLR-2 (Fig. 2). There was also a decrease in the MFI of staining, (Supplementary Fig. 2), indicating that the amount of receptors being expressed is being reduced, alongside the % of cells expressing the receptors. Expression of TLR-4 decreased after exposure to 5% BFSE, but was unchanged by CSE (Fig. 2).
BFSE alters phagocytic recognition receptors. MDM were exposure to air control, 1% or 5% BFSE or 10% CSE for 24 h. Cell surface markers: CD36 (A), CD44 (B), SR-A1 (C), CD206 (D), TLR-2 (E) and TLR-4 (F) were detected by immunofluorescence on a FACScanto II flow cytometer and expressed as % positive cells compared to negative controls. (n = 5) *p < 0.05.
BFSE increases intracellular pro-inflammatory mediators
The inflammatory response initiator cleaved caspase-1 was detected in the air treated control THP-1 macrophage but to a greater extent in cells exposed to 5% BFSE for 24 h (Fig. 3A). The MFI of intracellular cleaved caspase-1 in 5% BFSE treated cells was significantly (p = 0.047) higher than air treated control, 39.0 vs 24.7 (Fig. 3B).
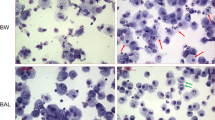
BFSE increases intracellular pro-inflammatory mediators. THP-1 macrophage cells were exposure to air control or 5% BFSE for 24 h. Active Caspase-1 (A) and; total IL-1β and active IL-1β (C) were detected by immunofluorescence. Confocal images were quantitatively measured for MFI of active Capase-1 (B) and total IL-1β (D), or the percentage of cells containing bright particulate active IL-1β (E). (n = 4) *p < 0.05 ***p < 0.001.
Increases in both precursor and cleaved IL-1β immunofluorescence were observed in 5% BFSE-treated THP-1 macrophages compared to air control (Fig. 3C). Detection of IL-1β using an antibody directed to amino acids 117–269, present in both the active and precursor IL-1β, revealed a homogenous cytoplasmic distribution which was non-significantly increased, MFI: 99.0 vs 67.2, 5% BFSE vs control (Fig. 3D). Cleaved IL-1β specific detection using an antibody reacting with the Asp 116 neoepitope on the IL-1β cleaved end but not cross-reacting with the precursor cytokine, revealed both homogenous cytoplasmic staining and accumulation in bright intracellular particles, 1–6 µm in size. The number of cells positive for cleaved IL-1β was significantly (p = 0.001) higher in the 5% BFSE treated THP-1 macrophage cells with 53.7% positive compared with 11.2% for the air treated control cells (Fig. 3E).
BFSE alters secretion of pro-inflammatory chemokines
We investigated the impact of BFSE exposure on THP-1 macrophage secretion of pro-inflammatory chemokines. Secretion of IL-8 was significantly increased from 15.7 ng/mL to 25.9 ng/mL (p < 0.05) and 28.6 ng/mL (p < 0.01) after 24 h exposure to 5% BFSE and 10% CSE, respectively (Fig. 4). Conversely, secretion of other pro-inflammatory chemokines: IP-10, MCP-1, MIP1α and MIP-1β were all significantly decreased in the supernatant of cells treated with 5% BFSE and 10% CSE (Fig. 4).
BFSE alters THP-1 macrophage chemokine secretion. THP-1 macrophage cells were exposure to air control or 1% or 5% BFSE or 10% CSE for 24 h. Supernatants were collected and assessed for IL-8 (A), IP-10 (B), MCP-1 (C), MIP-1α (D) and MIP-1β (F) by chemokine bead array and analysed by flow cytometry (n = 5). *p < 0.05 **p < 0.01 ***p < 0.001.
BFSE decreases macrophage viability
LDH release
LDH released from THP-1 macrophages increased in a dose-dependent manner after 24 h exposure to 1–10% BFSE, with mean LDH release in response to 10% BFSE increasing from 10.8% to 49.1% compared to air-treated control cells (p = 0.029). THP-1 macrophages and MDM cells treated with 5% BFSE exhibited LDH release that was consistent with exposure to 10% CSE but not significantly different from air treated control (20.5% and 16.5% vs 10.8% for THP-1, 19.3% and 17.8% vs 14.1% for MDM, respectively) (Fig. 5A).
BFSE decreases macrophage viability. THP-1 macrophage, or MDM cells, were exposure to air control or 1%, 2.5%, 5%, 10% BFSE or 10% CSE for 24 h. LDH from THP-1 macrophage or MDM cells was measured in supernatants after 24 h (n = 4) (A). THP-1 macrophage expression of Bcl-2 and PARP was assessed by western blot (B), band densitometry analysis of Bcl-2 (C) and PARP (D) was performed, data is a representation of three independent experiments, and was baselined to the air treated control sample, and normalized to β-actin expression. Error bars represent 95% confidence intervals. Representative confocal images of active caspase-3 (E) and PAR (F), in THP-1 macrophage with quantitative MFI measurement of active caspase-3 (G) and PAR (H). (n = 4) *p < 0.05, **p < 0.01.
Bcl-2, PARP and active caspase-3
Western blot analysis of protein from THP-1 macrophages exposed to 1–10% BFSE exhibited a dose-dependent decrease in the anti-apoptotic Bcl-2 and a concomitant increase in PARP cleavage compared to air treated control (Fig. 5B). The increases were confirmed using densitometry analysis (Fig. 5C,D).
Immunostaining for pro-apoptotic active caspase-3 was detected in the air treated control THP-1 macrophages and increased in cells exposed to 5% BFSE for 24 h (Fig. 5E). Image analysis of intracellular active caspase-3 revealed a significant (p = 0.021) increase in response to 5% BFSE compared to air treated control, MFI: 41.3 vs 23.0 (Fig. 5G). Immunostaining for Poly (ADP-ribose) (PAR, Fig. 5F), a polymer formed by active PARP, and an indicator of DNA damage and inducer of pro-apoptotic factor release from mitochondria26 was non-significantly (p = 0.195) increased (68.1 vs 41.7), in 5% BFSE vs control (Fig. 5H).
7AAD and Annexin V
Treatment with BFSE or CSE did not cause a significant decrease in the percentage of apoptotic/necrotic cells (which could potentially account for a decrease in phagocytosis or receptor expression), assessed by flow cytometric analysis of annexin V and 7AAD, compared to untreated cells (Supplementary Fig. 3) The percentage of total events falling in the macrophage ‘Macs” gate were not significantly affected by BFSE or CSE treatment.
Discussion
This study investigated changes to macrophage function and viability after exposure to smoke extract from common Australian flora. Previous studies have largely focused on the effects of cigarette smoke and fractions of particulate matter. However, the smoke produced from combustion of plant material also contains potentially damaging components including aldehydes, acrolein, and carbon monoxide15. To investigate the effects of BFSE we adapted our current methods used for the investigation of cigarette smoke27. The concentrations of BFSE were extrapolated from the previous findings of our group and others showing that CSE at 10% is sufficient to elicit an inflammatory response and impair macrophage function22,27,28. This concentration has been shown to be equivalent to smoking 0.5–2 packs of cigarettes per day29.
Macrophage efferocytic clearance of apoptotic cells in the airway is important to prevent secondary necrosis of the uncleared apoptotic material and a resultant progression of inflammation19,25. We have shown significantly reduced efferocytosis in the airways of patients with a range of chronic lung diseases including COPD and severe asthma18,19,22,23,30. In the present study, the capacity of THP-1 macrophages and MDM to efferocytose apoptotic bronchial epithelial cells was significantly impaired after exposure to BFSE, findings consistent with our previously reported data following CSE and E-cigarette exposure31, and with a report that acrolein, a by-product of burning wood or cigarettes, reduced the ability of macrophages to engulf erythrocytes32. Our findings may shed further light on the reported increases in COPD and asthma patient admissions associated with bushfire events8,9. As COPD patients and severe asthmatics already have compromised alveolar macrophage phagocytic function and an increased rate of lung epithelial cell apoptosis, the additional bombardment by bushfire smoke would likely compound their respiratory morbidities.
Chronic bacterial airway colonisation with potentially pathogenic bacteria including NTHi has been linked to the pathogenesis of several chronic lung diseases including COPD and severe asthma, with NTHi accounting for up to half of all isolates in COPD33. Efficient phagocytosis of this bacteria by alveolar macrophages is thus important to reduce bacterial colonisation, limit inflammation and to prevent exacerbations (in COPD, up to 80% of exacerbations are associated with this bacteria33. In the present study, BFSE significantly suppressed the capacity of THP-1 or MDM macrophages to phagocytose NTHi, again consistent with our findings with CSE and in patients with chronic lung diseases where the defective clearance was correlated with increased markers of inflammation, and potentiation of bacterial colonisation of the lower airways.
Data from BFSE-exposed THP-1 macrophages was consistent with our previous data from both CSE-exposed THP-1 macrophage cells27 and primary alveolar macrophages from heathy smokers and patients with COPD18,19,34. Nevertheless we also performed experiments using primary monocyte derived macrophages (MDM). The additional experiments with MDM showed higher initial levels of phagocytosis and more marked inhibition with BFSE and CSE, findings that are consistent with our previous studies. Consistent with the changes in percentage of cells phagocytosing, we also noted a decrease in MFI, suggesting that CSE and BFSE also affect the amount of prey being taken up. The level of inhibition induced by BFSE and CSE is likely to be physiologically relevant, as our previous studies in smoke-exposed mice treated with macrophage-targeted therapies showed an improved macrophage phagocytic capacity that significantly correlated with a reduction in inflammation.
We also previously found that the deficiency appeared to be specific for apoptotic cells or bacteria, as tests carried out in parallel using carboxylate modified polystyrene microbeads revealed no significant difference between COPD patients and control subjects18,30. One reason for this deficiency may be defective recognition of the phagocytic target in response to cigarette or bushfire smoke, a concept that is supported by the findings in the present study and in our previous studies of cigarette smoke exposure22,34,35. The interaction between macrophages and phagocytic targets is mediated by a variety of macrophage membrane-associated proteins. We therefore applied primary MDM to investigate the effects of BFSE on several recognition molecules that can be used in both phagocytosis of bacteria and efferocytosis. BFSE, consistent with the effects of CSE, significantly decreased the percentage of MDM expressing thrombospondin receptor (CD36), class A scavenger receptors (SR-As), mannose receptor (CD206) and TLR-2 but not TLR-4. Ligation of the hyaluronan receptor (CD44) is also important for efficient clearing of excess hyaluronan and apoptotic cells that may otherwise contribute to tissue damage in COPD. We noted a significant suppression of CD44 expression by MDM in response to BFSE, consistent with our previous report of decreased expression of CD44 on alveolar macrophages from smokers with or without COPD compared with healthy never-smoker controls22. We also noted a reduction in the MFI of CD36, TLR2, TLR4 and CD44, indicating that the both the percentage of cells expressing the receptors and the amount of receptors being expressed are being reduced. This data indicates that cells that are still positive for the receptors after exposure to smoke are expressing less receptors. Taken together, this data suggests that the suppressed recognition of phagocytic targets, whether apoptotic cells or bacteria, in response to BFSE or CSE may one mechanism for the defective phagocytic clearance, contributing to bacterial persistence and increased inflammatory response. A potential limitation of our study is the effect of variable numbers of non-viable macrophages in the macrophage gate on receptor expression. We however consider this very unlikely as we used an identical protocol across multiple experiments comparing control and treatment data, and our flow cytometry gating ensured that greater than 93% of viable cells were included in the analyses.
A further pro-inflammatory effect of BFSE on THP-1 macrophages was an increase in active caspase-1 and IL-1β, two cleavage products downstream of inflammasome assembly. These data are consistent with reports that aldehydes and acrolein, components in both wood and cigarette smoke15, induced secretion of IL-8 and other inflammatory mediators from macrophages28. Interestingly, we noted a decrease in THP-1 secretion of pro-inflammatory mediators MCP-1, IP-10, MIP-1α and MIP-1β following exposure to BFSE or CSE. This was surprising given the increases in intracellular IL-1β; but consistent with the findings of many other groups. For example, decreased secretion of TNFα, IL-1β, IL-6, MIP-1α, MIP-1β, IP-10 and MCP-1 was reported in macrophages exposed to cigarette smoke or in cultured alveolar macrophages from smokers compared with non-smokers28,36,37,38,39,40,41,42,43,44,45.
Maintaining macrophage viability in the airway is important to ensure effective phagocytic function. Our dose response studies confirmed that 10% BFSE had the most cytotoxic effects on THP-1 macrophages while even 5% BFSE reduced macrophage viability to a similar extent as 10% CSE. The reduction in macrophage viability in response to 5% BFSE was accompanied by a decrease in the anti-apoptotic protein Bcl-2 and increased activation of caspase-3, suggesting that initiation of apoptosis is at least in part responsible for the decrease in macrophage survival. These findings are consistent with those of Jalava et al.46 who found an equivalent amount of apoptosis, up to 17%, in mouse macrophage RAW264.7 cells after 24 hours of exposure to particulate matter from woodland fires.
Taken together, our data shows that bushfire smoke exposure can impair macrophage function and viability and increase production of pro-inflammatory mediators, to a similar extent as CSE, and highlights the need for further research into the harmful effects of bushfire smoke, with particular relevance to patients with pre-existing lung disease.
Methods
Preparation of smoke extracts
Cigarette smoke extract (CSE)
As a known affecter of macrophage function, a single batch of 100% stock cigarette smoke extract, which was used throughout the study as a reference for the impact of bushfire smoke, was prepared as previously reported22. Briefly, the smoke from three 1R5F research-reference filtered cigarettes containing 1.67 mg of tar and 0.16 mg of nicotine (The Tobacco Research Institute, University of Kentucky, Lexington, KY) was bubbled through 30 mL RPMI 1640 medium supplemented with 10% foetal bovine serum (FBS), penicillin/gentamicin (all Thermo Fisher Scientific, MA, USA) at a speed of 5 min per cigarette using a vacuum pump. The pH was adjusted to neutrality and aliquots of the cigarette smoke extract were stored at −80 °C.
Bushfire smoke extract (BFSE)
Equal weights of the following species (indigenous or common introductions to the bushfire prone region of the Adelaide Hills, South Australia) were combined: Acacia baileyana (Cootamundra wattle) leaves and stems, Acacia melanoxylon (blackwood) leaves and stems, Acacia vestita (weeping acacia) leaves and stems, Eucalyptus camaldulensis (river red gum) leaves and Eucalyptus globulus (blue gum) leaves.
Each species was blended separately using a CG2B spice grinder (Breville, Sydney, NSW, Australia). The blended material was weighed and equal portions were mixed together, half of the mixture was frozen immediately at −80 °C (‘wet’) while the other half was dehydrated using a DT5600 food dehydrator (Sunbeam, Botany, NSW, Australia; ‘dried’) for 4 h, at setting two (approximately 55 °C) then stored in a desiccator.
To prepare the 100% stock smoke extract: smoke from 2 g of ignited foliage (1.5 g dried plus 0.5 g wet), a mass proportionate to the cigarette mass used for 100% CSE, was bubbled through 20 mL of HEPES buffered saline solution using a vacuum pump taking 15 min to burn all material. The pH was measured and adjusted to neutrality if required and aliquots were stored at −80 °C. A control solution of HEPES buffered salt solution exposed to bubbled air for 15 min and stored at −80 °C was prepared in parallel. For initial optimisation experiments, concentrations of 1–10% were investigated, and a final concentration of 5% used in all experiments. 100% BFSE was diluted into RPMI 1640 medium with 10% FBS, penicillin/gentamicin.
Preparation of Cell Lines
The monocytic cell line, THP-1 (American Type Culture Collection, Manassas, VA, USA) was maintained at 37 °C/5% CO2 in RPMI 1640 medium supplemented with 2 mM L-glutamine, 10% FBS, penicillin/gentamicin and 0.05 mM ß-mercaptoethanol (Sigma-Aldrich, MO, USA). Differentiation into macrophages was facilitated by seeding at a density of 5 × 105 cells/mL in culture medium supplemented with 50 nM phorbol 12-myristate 13-acetate (PMA; Sigma-Aldrich) for 72 h as previously described47.
The 16HBE14o- airway epithelial cell line was a generous gift from Dr Dieter C. Gruenert (University of California, San Francisco, USA). 16HBE14o- cells were maintained in MEM medium supplemented with 2 mM L-glutamine, 10% FBS, penicillin/gentamicin under humidified 37 °C/5% CO2 conditions. Cell culture materials were from Thermo Fisher Scientific unless stated otherwise.
Preparation of Monocyte Derived Macrophage (MDM)
Adult controls were recruited from our volunteer database, were non-smokers and had no history of respiratory or allergic disease. Patients were invited to participate in the study, and fully informed consent was obtained. The study protocol was approved by the Royal Adelaide Hospital Research Committee (#020811d). All research was performed in accordance with relevant guidelines and regulations. Monocytes were isolated from whole blood collected in Lithium-Heparin tubes (Greiner Bio One, Austria). Blood was diluted with 2 volumes of RPMI 1640 medium without additives and layered over LymphoprepTM (STEMCELL Technologies, BC, Canada). Peripheral blood mononuclear cells (PBMC) were isolated as per manufactures instructions. PBMC were seeded into plates at 1.4 × 106/mL in RPMI 1640 medium without additives at 37 °C/5% CO2 for 60–90 min to allow monocytes to adhere. Macrophage were derived from monocytes cultured in RPMI 1640 medium supplemented with 2 mM L-glutamine, 10% FBS, penicillin/gentamicin and 2 ng/mL granulocyte-macrophage colony-stimulating factor (GM-CSF, Sigma-Aldrich) for 12 days with full media changes at 4 and 8 days.
Phagocytosis Assays
Phagocytosis of apoptotic 16HBE14o-bronchial epithelial cells or non-typeable H. influenzae (NTHi) by differentiated THP-1 macrophages or MDM exposed to smoke extracts or control media was performed as previously reported48. Briefly, NTHi stained with Sytox Green and 16HBE14o- stained with Sytox Orange from Thermo Fisher Scientific were incubated with MDM or THP-1 macrophage cells, at a 100:1 and 5:1 ratio respectively, for 90 min before being lifted and analysed by flow cytometry on a FACSCanto II (BD Biosciences, San Diego, USA). Gating procedures have been previously published18,27,31,35.
Flow cytometry of cell surface markers
MDM cells were incubated in ice cold PBS for 15 min before lifting with a bulb pipette. Cells were washed with isoflow (BD Biosciences) containing 0.5% bovine serum albumin (Sigma-Aldrich) and pelleted. Cells were incubated with 2 µL of conjugated primary antibodies to SR-A1 (#FAB2708A; APC; R&D Systems, MN, USA); TLR-2 (#12-9024; PE) or TLR-4 (#17-9917; APC; eBiosciences, CA, USA); CD36 (#IM0766U; FITC) or CD206 (#IM2741; PE; Beckman Coulter, IN, USA); or CD44 (#555478; FITC; BD Bioscience) for 10 min in the dark, and washed. All antibodies were titrated to determine optimal antibody concentration to exclude non-specific binding. Cells were stained with isotype controls to exclude autofluorescence/non-specific binding for quadrant marker placement to include 98% of the gated cell population i.e., less than 2% positive staining35.
Fifty thousand events were collected and cell surface receptors analysed, using FACS DIVA 7.0 and expressed as % positive of cells expressing the marker. To further assess the amount of receptor being assessed and potential changes in response to BFSE and CSE, we also recorded MFI of receptor expression. Gating procedures have been previously published18,27,31,35.
Immunofluorescence and confocal microscopy
The apoptotic markers: cleaved caspase-3 and poly (ADP-ribose) (PAR, a polymer formed by active PARP (poly (ADP-ribose) polymerase)) and the inflammatory markers cleaved caspase- 1 and total/cleaved IL-1β were assessed in THP-1 macrophages exposed to 5% BFSE using a method described earlier for CSE exposure27. Briefly, cells were fixed with 2.5% formalin in phosphate-buffered saline (PBS), permeabilized with 0.1% Triton X-100 (Sigma-Aldrich) in PBS, pre-blocked with serum-free protein blocker (Dako, Glostrup, Denmark), incubated overnight at 4 °C with primary antibodies and 1 h at room temperature with secondary antibodies. Primary antibodies were rabbit polyclonal anti-cleaved caspase-3 (1/40, R&D Systems), mouse monoclonal anti-PAR (1/20, Enzo Life Sciences, NY, USA), and rabbit polyclonal anti-IL-1β (1/30, H-153) goat polyclonal anti-cleaved caspase-1 (1/20, h297) and goat polyclonal anti-cleaved IL-1β (1/20, h117) (all Santa Cruz Biotechnology). All secondary antibodies were donkey IgG F(ab’)2 fragments with Alexa Fluor (AF) conjugates from Jackson ImmunoResearch (West Grove, PA, USA); anti-rabbit IgG (AF594 or AF647), anti-goat IgG (AF488), and anti-mouse IgG (AF647). Images were captured on a LSM700 confocal microscope (Carl Zeiss Australia, NSW, Australia). For quantitative analysis, 10 serial images at a 20× objective were captured from each well of an 8-well chamber slide in a blinded manner by focusing on the DAPI channel. Measurement of mean fluorescence intensity (MFI) or percentage of brightly fluorescent cells was determined by ImageJ morphometric software (NIH, Bethesda, MA, USA).
Cytometric Bead Array (CBA)
Supernatant from THP-1 macrophage cells exposed to smoke extracts or air control for 24 h were assessed with a human inflammatory chemokine CBA kit (BD Biosciences), as per manufacturer instructions. Chemokines: IL-8, MCP-1, IP-10, MIP-1α and MIP-1β were measured on a FACSCanto II and analysed with FCAP Array software (BD Biosciences).
Assessment of macrophage viability
LDH, an enzyme released from cells with compromised membranes was measured in supernatant from THP-1 macrophage or MDM as instructed by a cytotoxicity detection kit (Roche; Mannheim, Germany). Briefly, supernatants were centrifuge at 500 × g to remove cell debris then stored at −80 °C prior to analysis. Supernatant were added to a 96-well plate in triplicate followed by reaction mixture then incubated at room temperature in the dark for 10 min. The assay reaction was neutralised with the provided stop solution and absorbance measured at 490 nm, with a 600 nm reference wavelength, on an Epoch microplate spectrophotometer (Bio-Tek; VT, USA).
Western Analysis
For western blot analysis of the anti-apoptotic B-cell lymphoma 2 (Bcl-2) and poly-ADP ribose polymerase (PARP) cleavage, THP-1 cells were lysed using M-PER mammalian cell protein lysis reagent with Halt® protease inhibitor cocktail (Thermo Fisher Scientific). Protein samples were quantified using Bio-Rad (CA, USA) DC protein assay; 10 µg of protein (was electrophoresed on 4–12% gradient Bis-Tris gels before being transferred to nitrocellulose membrane. Membranes were blocked in 5% diploma skim milk (Fonterra, NZ) or 5% bovine serum albumin before probing with primary antibodies and corresponding horseradish peroxidase-conjugated secondary antibodies (R&D Systems). Band detection was performed using ECL Prime chemiluminescent substrate (GE Healthcare, Buckinghamshire, UK), on a LAS-4000 instrument with Multigauge software for densitometry analysis (FugiFilm, Tokyo, Japan). Primary antibodies were: PARP and Bcl-2 (rabbit polyclonal, Santa Cruz Biotechnology, CA, USA), with β-actin (mouse monoclonal, Sigma-Aldrich) used for loading correction during band analyses.
Flow cytometric analysis of 7AAD and Annexin V staining
Macrophages exposed to air control, 1% BFSE, 5% BFSE or 10% CSE for 24 h were assessed by flow cytometry for cell viability using 7AAD and Annexin V as published49,50.
Statistical analysis
Data were analysed using SPSS software (SPSS Inc. IBM Chicago, USA). Results are reported as min, max and median (q1, q3) unless otherwise indicated. Analysis was performed using the non-parametric Friedman test, with Wilcoxon signed rank tests for post-hoc pairwise comparisons. A value of p < 0.05 was considered statistically significant. Densitometry analysis of protein bands was performed using Multi Gauge software (V3.1 Fugifilm, Tokyo, Japan). Density scores were analysed by a gamma (log link) mixed model regression to allow for correlated treatment responses within each culture. Results are normalized to both β-actin and the air control; and presented as relative protein expression. Analysis was performed using R statistical software (release 3.2.3), and library lme4 (v 1.1–12)50,51.
References
Westerling, A. L. Increasing western US forest wildfire activity: sensitivity to changes in the timing of spring. Philosophical transactions of the Royal Society of London. Series B, Biological sciences 371, https://doi.org/10.1098/rstb.2015.0178 (2016).
CSIRO. Report: State of the Climate 2014 (Australian Goverment: Bureau of Meteorology and CSIRO, 2014).
Lucas, C., Hennessy, K. L., Mills, G. & Bathols, J. M. (ed. CSIRO Bureau of Meteorology, Bushfire CRC) 1–80 (Melbourne, 2007).
Theobald, D. M. & Romme, W. H. Expansion of the US wildland–urban interface. Landscape and Urban Planning 83, 340–354, https://doi.org/10.1016/j.landurbplan.2007.06.002 (2007).
Moritz, M. A. et al. Learning to coexist with wildfire. Nature 515, 58–66, https://doi.org/10.1038/nature13946 (2014).
Johnston, F. H., Kavanagh, A. M., Bowman, D. M. & Scott, R. K. Exposure to bushfire smoke and asthma: an ecological study. Med J Aust 176, 535–538 (2002).
Rappold, A. G. et al. Peat bog wildfire smoke exposure in rural North Carolina is associated with cardiopulmonary emergency department visits assessed through syndromic surveillance. Environmental health perspectives 119, 1415–1420, https://doi.org/10.1289/ehp.1003206 (2011).
Delfino, R. J. et al. The relationship of respiratory and cardiovascular hospital admissions to the southern California wildfires of 2003. Occup Environ Med 66, 189–197, https://doi.org/10.1136/oem.2008.041376 (2009).
Martin, K. L., Hanigan, I. C., Morgan, G. G., Henderson, S. B. & Johnston, F. H. Air pollution from bushfires and their association with hospital admissions in Sydney, Newcastle and Wollongong, Australia 1994–2007. Australian and New Zealand journal of public health 37, 238–243, https://doi.org/10.1111/1753-6405.12065 (2013).
Dennekamp, M. & Abramson, M. J. The effects of bushfire smoke on respiratory health. Respirology 16, 198–209, https://doi.org/10.1111/j.1440-1843.2010.01868.x (2011).
Tan, W. C. et al. The human bone marrow response to acute air pollution caused by forest fires. American journal of respiratory and critical care medicine 161, 1213–1217, https://doi.org/10.1164/ajrccm.161.4.9904084 (2000).
van Eeden, S. F. et al. Cytokines involved in the systemic inflammatory response induced by exposure to particulate matter air pollutants (PM(10)). American journal of respiratory and critical care medicine 164, 826–830, https://doi.org/10.1164/ajrccm.164.5.2010160 (2001).
Nakayama Wong, L. S., Aung, H. H., Lame, M. W., Wegesser, T. C. & Wilson, D. W. Fine particulate matter from urban ambient and wildfire sources from California’s San Joaquin Valley initiate differential inflammatory, oxidative stress, and xenobiotic responses in human bronchial epithelial cells. Toxicology in vitro: an international journal published in association with BIBRA 25, 1895–1905, https://doi.org/10.1016/j.tiv.2011.06.001 (2011).
Wegesser, T. C., Franzi, L. M., Mitloehner, F. M., Eiguren-Fernandez, A. & Last, J. A. Lung antioxidant and cytokine responses to coarse and fine particulate matter from the great California wildfires of 2008. Inhalation toxicology 22, 561–570, https://doi.org/10.3109/08958370903571849 (2010).
De Vos, A. J., Reisen, F., Cook, A., Devine, B. & Weinstein, P. Respiratory irritants in Australian bushfire smoke: air toxics sampling in a smoke chamber and during prescribed burns. Archives of environmental contamination and toxicology 56, 380–388, https://doi.org/10.1007/s00244-008-9209-3 (2009).
Wegesser, T. C., Pinkerton, K. E. & Last, J. A. California wildfires of 2008: coarse and fine particulate matter toxicity. Environmental health perspectives 117, 893–897, https://doi.org/10.1289/ehp.0800166 (2009).
Franzi, L. M., Bratt, J. M., Williams, K. M. & Last, J. A. Why is particulate matter produced by wildfires toxic to lung macrophages? Toxicology and applied pharmacology 257, 182–188, https://doi.org/10.1016/j.taap.2011.09.003 (2011).
Hodge, S., Hodge, G., Scicchitano, R., Reynolds, P. N. & Holmes, M. Alveolar macrophages from subjects with chronic obstructive pulmonary disease are deficient in their ability to phagocytose apoptotic airway epithelial cells. Immunol Cell Biol 81, 289–296, https://doi.org/10.1046/j.1440-1711.2003.t01-1-01170.x (2003).
Hodge, S., Hodge, G., Holmes, M. & Reynolds, P. N. Increased airway epithelial and T-cell apoptosis in COPD remains despite smoking cessation. The European respiratory journal 25, 447–454, https://doi.org/10.1183/09031936.05.00077604 (2005).
Berenson, C. S., Garlipp, M. A., Grove, L. J., Maloney, J. & Sethi, S. Impaired phagocytosis of nontypeable Haemophilus influenzae by human alveolar macrophages in chronic obstructive pulmonary disease. J Infect Dis 194, 1375–1384, https://doi.org/10.1086/508428 (2006).
Taylor, A. E. et al. Defective macrophage phagocytosis of bacteria in COPD. The European respiratory journal 35, 1039–1047, https://doi.org/10.1183/09031936.00036709 (2010).
Hodge, S. et al. Smoking alters alveolar macrophage recognition and phagocytic ability: implications in chronic obstructive pulmonary disease. American journal of respiratory cell and molecular biology 37, 748–755, https://doi.org/10.1165/rcmb.2007-0025OC (2007).
Simpson, J. L. et al. Impaired macrophage phagocytosis in non-eosinophilic asthma. Clin Exp Allergy 43, 29–35, https://doi.org/10.1111/j.1365-2222.2012.04075.x (2013).
Hodge, S. et al. Is Alveolar Macrophage Phagocytic Dysfunction in Children With Protracted Bacterial Bronchitis a Forerunner to Bronchiectasis? Chest 149, 508–515, https://doi.org/10.1016/j.chest.2015.10.066 (2016).
Vandivier, R. W., Henson, P. M. & Douglas, I. S. Burying the dead: the impact of failed apoptotic cell removal (efferocytosis) on chronic inflammatory lung disease. Chest 129, 1673–1682, https://doi.org/10.1378/chest.129.6.1673 (2006).
Yu, S. W. et al. Apoptosis-inducing factor mediates poly(ADP-ribose) (PAR) polymer-induced cell death. Proceedings of the National Academy of Sciences of the United States of America 103, 18314–18319, https://doi.org/10.1073/pnas.0606528103 (2006).
Tran, H. B. et al. Cigarette smoke inhibits efferocytosis via deregulation of sphingosine kinase signaling: reversal with exogenous S1P and the S1P analogue FTY720. Journal of leukocyte biology 100, 195–202, https://doi.org/10.1189/jlb.3A1015-471R (2016).
Facchinetti, F. et al. Alpha,beta-unsaturated aldehydes in cigarette smoke release inflammatory mediators from human macrophages. American journal of respiratory cell and molecular biology 37, 617–623, https://doi.org/10.1165/rcmb.2007-0130OC (2007).
Su, Y., Han, W., Giraldo, C., De Li, Y. & Block, E. R. Effect of cigarette smoke extract on nitric oxide synthase in pulmonary artery endothelial cells. American journal of respiratory cell and molecular biology 19, 819–825, https://doi.org/10.1165/ajrcmb.19.5.3091 (1998).
Hodge, S. & Reynolds, P. N. Low-dose azithromycin improves phagocytosis of bacteria by both alveolar and monocyte-derived macrophages in chronic obstructive pulmonary disease subjects. Respirology 17, 802–807, https://doi.org/10.1111/j.1440-1843.2012.02135.x (2012).
Ween, M. P., Whittall, J. J., Hamon, R., Reynolds, P. N. & Hodge, S. J. Phagocytosis and Inflammation: Exploring the effects of the components of E-cigarette vapour on macrophages. Physiological Reports [in press] (2017).
Jakab, G. J., Risby, T. H., Sehnert, S. S., Hmieleski, R. R. & Gilmour, M. I. Suppression of alveolar macrophage membrane-receptor-mediated phagocytosis by model particle-adsorbate complexes: physicochemical moderators of uptake. Environmental health perspectives 89, 169–174 (1990).
King, P. Haemophilus influenzae and the lung (Haemophilus and the lung). Clin Transl Med 1, 10, https://doi.org/10.1186/2001-1326-1-10 (2012).
Hodge, S. et al. Azithromycin improves macrophage phagocytic function and expression of mannose receptor in chronic obstructive pulmonary disease. American journal of respiratory and critical care medicine 178, 139–148, https://doi.org/10.1164/rccm.200711-1666OC (2008).
Hodge, S. et al. Cigarette smoke-induced changes to alveolar macrophage phenotype and function are improved by treatment with procysteine. American journal of respiratory cell and molecular biology 44, 673–681, https://doi.org/10.1165/rcmb.2009-0459OC (2011).
Bardelli, C. et al. Expression of functional NK1 receptors in human alveolar macrophages: superoxide anion production, cytokine release and involvement of NF-kappaB pathway. Br J Pharmacol 145, 385–396, https://doi.org/10.1038/sj.bjp.0706198 (2005).
Birrell, M. A., Wong, S., Catley, M. C. & Belvisi, M. G. Impact of tobacco-smoke on key signaling pathways in the innate immune response in lung macrophages. J Cell Physiol 214, 27–37, https://doi.org/10.1002/jcp.21158 (2008).
Bozinovski, S. et al. Carbonylation caused by cigarette smoke extract is associated with defective macrophage immunity. American journal of respiratory cell and molecular biology 45, 229–236, https://doi.org/10.1165/rcmb.2010-0272OC (2011).
Brown, G. P., Iwamoto, G. K., Monick, M. M. & Hunninghake, G. W. Cigarette smoking decreases interleukin 1 release by human alveolar macrophages. Am J Physiol 256, C260–264, https://doi.org/10.1152/ajpcell.1989.256.2.C260 (1989).
Chen, H., Cowan, M. J., Hasday, J. D., Vogel, S. N. & Medvedev, A. E. Tobacco smoking inhibits expression of proinflammatory cytokines and activation of IL-1R-associated kinase, p38, and NF-kappaB in alveolar macrophages stimulated with TLR2 and TLR4 agonists. Journal of immunology 179, 6097–6106 (2007).
Mikuniya, T. et al. Proinflammatory or regulatory cytokines released from BALF macrophages of healthy smokers. Respiration 66, 419–426, https://doi.org/10.1159/000029425 (1999).
Nordskog, B. K., Fields, W. R. & Hellmann, G. M. Kinetic analysis of cytokine response to cigarette smoke condensate by human endothelial and monocytic cells. Toxicology 212, 87–97, https://doi.org/10.1016/j.tox.2005.04.005 (2005).
Ouyang, Y. et al. Suppression of human IL-1beta, IL-2, IFN-gamma, and TNF-alpha production by cigarette smoke extracts. J Allergy Clin Immunol 106, 280–287, https://doi.org/10.1067/mai.2000.107751 (2000).
Soliman, D. M. & Twigg, H. L. 3rd. Cigarette smoking decreases bioactive interleukin-6 secretion by alveolar macrophages. Am J Physiol 263, L471–478, https://doi.org/10.1152/ajplung.1992.263.4.L471 (1992).
Sauty, A., Mauel, J., Philippeaux, M. M. & Leuenberger, P. Cytostatic activity of alveolar macrophages from smokers and nonsmokers: role of interleukin-1 beta, interleukin-6, and tumor necrosis factor-alpha. American journal of respiratory cell and molecular biology 11, 631–637, https://doi.org/10.1165/ajrcmb.11.5.7946392 (1994).
Jalava, P. I. et al. In vitro inflammatory and cytotoxic effects of size-segregated particulate samples collected during long-range transport of wildfire smoke to Helsinki. Toxicology and applied pharmacology 215, 341–353, https://doi.org/10.1016/j.taap.2006.03.007 (2006).
Dehle, F. C. et al. Defective lung macrophage function in lung cancer+/− chronic obstructive pulmonary disease (COPD/emphysema)-mediated by cancer cell production of PGE2? PLoS One 8, e61573, https://doi.org/10.1371/journal.pone.0061573 (2013).
Ween, M. et al. A small volume technique to examine and compare alveolar macrophage phagocytosis of apoptotic cells and non typeable Haemophilus influenzae (NTHi). Journal of immunological methods 429, 7–14, https://doi.org/10.1016/j.jim.2015.12.004 (2016).
Hodge, G. L., Flower, R. & Han, P. Optimal storage conditions for preserving granulocyte viability as monitored by Annexin V binding in whole blood. Journal of immunological methods 225, 27–38 (1999).
R: A Language and Environment for Statistical Computing v. 3.2.3 (R Foundation for Statistical Computing, Vienna, Austria, 2015).
Bates, D., Mächler, M., Bolker, B. & Walker, S. Fitting Linear Mixed-Effects Models Using lme4. Journal of Statistical Software. Articles 67, 1–48, https://doi.org/10.18637/jss.v067.i01 (2015).
Author information
Authors and Affiliations
Contributions
R.H., H.T., M.W. and E.R. performed experiments; S.H. and R.H. developed study design and wrote the main manuscript text; H.J. provided clinical samples. All authors contributed to study design and approved the final manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hamon, R., Tran, H.B., Roscioli, E. et al. Bushfire smoke is pro-inflammatory and suppresses macrophage phagocytic function. Sci Rep 8, 13424 (2018). https://doi.org/10.1038/s41598-018-31459-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-31459-6
- Springer Nature Limited
This article is cited by
-
Reduction in Rubicon by cigarette smoke is associated with impaired phagocytosis and occurs through lysosomal degradation pathway
Clinical and Experimental Medicine (2023)