Abstract
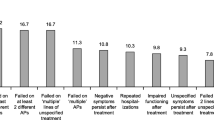
Goals: The goals of this study are 1) to determine causes and patterns of relapse for a cohort of “revolving door” schizophrenia inpatients, and 2) to assess the feasibility of starting a new psychopharmacologic intervention before discharge, either depot therapy or an atypical antipsychotic. Methods: Consecutive admissions to an acute inpatient unit in New York City were screened for “revolving door” criteria. Patients had to have a primary diagnosis of schizophrenia or schizoaffective disorder and have either 1) two hospitalizations in the last year, or 2) three hospitalizations in the last three years. Patients were then assessed for probable causes of relapse for the index and prior two hospitalizations. Treatment selection, based on this information, was trichotomized to: 1) oral conventional antipsychotic, 2) depot conventional antipsychotic (either haloperidol or fluphenazine decanoate), or 3) atypical antipsychotic (either risperidone or clozapine). Results: Sixty-three out of 131 screened admissions met the above revolving door criteria. They were indeed “revolving”, having an average of 1.3 hospitalizations per year over the last 3 years and were only out of the hospital for five months (median) before index admission. The treatment selection process was hampered by lack of information about events leading to relapse, and by the lack of outpatient participation in the medication selection process. Of the 50 patients with complete histories about precipitants for the index episode, the most common reason for rehospitalization was judged to be medication non-compliance (n = 25; 50%), followed by medication nonresponse (n = 13; 26%). Not surprisingly, medication recommendations were closely linked to the assessed reason for relapse (depot therapy [n = 27; 49%] with medication non-compliance; atypical antipsychotic [n = 20; 37%] with medication nonresponse [X2 = 26.9, p<.001]).These two recommendations were implemented before discharge for about one-half of the cases. Patient refusal was a relatively greater problem for depot recommendation while constraints in the outpatient environment were more problematic for patients recommended for atypical antipsychotics. Conclusions: Medication noncompliance and medication nonresponse, in that order, were judged to be the most common causes of relapse for “revolving door” inpatients. Both depot therapy and atypical antipsychotics were commonly recommended and ultimately accepted by about 2/3rds of patients. Choice between depot and atypical was driven by the assessed cause of relapse. In summary, it seems possible to identify “revolving door” inpatients, and to target specific medication interventions within the time frame of an acute inpatient admission.
Similar content being viewed by others
REFERENCES
Weiden P, Olfson M. Cost of relapse in schizophrenia. Schizophrenia Bulletin. 1995;21:419–428.
Redick RW, Witkin MJ, Atay JE, Manderscheid RW. Availability of psychiatric beds, United States: Selected years, 1970–1990. DHHS Publication No. (SMA) 94–3001. 1994;213:1–7.
Dickey B, Normand S-L, Norton E, Azeni H, Fisher W, Altaffer F. Managing the care of schizophrenia: Lessons from the 4-year Massachusetts Medicaid study. Archives of General Psychiatry. 1996;53:945–952.
Witkin M, Atay J, Manderscheid R. Trends in state and county mental hospitals in the U.S. from 1970 to 1992. Psychiatric Services. 1996;47:1079–1081.
Essock S. Clozapine's effectiveness: Results of a 2-year randomized trial. NCDEU. Boca Raton, FL; 1996.
Glazer W, Ereshefsky L. A pharmacoeconomic model of outpatient antipsychotic therapy in “revolving door” schizophrenic patients. Journal of Clinical Psychiatry. 1996;57:337–345.
Glazer W, Kane J. Depot neuroleptic therapy: An underutilized treatment option. J. Clin. Psychiatry. 1992;53:426–433.
Johnson DAW. Further observations on the duration of depot neuroleptic maintenance therapy in schizophrenia. British Journal of Psychiatry. 1979;135:524–530.
Kissling W. The current unsatisfactory state of relapse prevention in schizophrenic psychoses—suggestions for improvement. Clinical Neuropharmacology. 1991;14:33–44.
Munk-Jorgensen P, Lutzhoft JH, Jensen J, Stromgren E. Trends in psychiatric hospitalization in Denmark: A 10-year register-based investigation. Acta Psychiatrica Scandinavica. 1992;86:79–83.
Weiden P, Aquila R, Standard J. Atypical antipsychotic drugs and long-term outcome in schizophrenia. Journal of Clinical Psychiatry. 1996;57:53–60.
Weiden P. Using atypical antipsychotics. Journal of Practical Psychiatry and Behavioral Health. 1995;1:115–119.
Sullivan G, Wells KB, Morgenstern H, Leake B. Identifying modifiable risk factors for rehospitalization: A case-control study of seriously mentally ill persons in Mississippi. American Journal of Psychiatry. 1995;152:1749–1756.
Nageotte C, Sullivan G, Duan N, Camp P. Medication compliance among the seriously mentally ill in a public mental health system. Social Psychiatry and Psychiatric Epidemiology. 1997;32:49–56.
Mechanic D, Surles R. Challenges in state mental health policy and administration. Health Affairs 1992:34–50.
Weiden P, Olfson M, Essock S. Medication Noncompliance and Mental Health Policy. In: Blackwell B, ed. Compliance and the Treatment Alliance; 1996:35–60.
Kessler R, McGonagle K, Zhao S, et al. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States. Archives of General Psychiatry. 1994;51:8–19.
McEvoy J, Weiden P, Smith T, Carpenter D, Kahn D, Frances A. The Expert Consensus Guideline Series: Treatment of Schizophrenia. Journal of Clinical Psychiatry. 1996;(Suppl 12B).
Weiden P, Rapkin B, Zygmunt A, Mott T, Goldman A, Frances A. Postdischarge medication compliance of inpatients converted from an oral to a depot regimen. Psychiatric Services. 1995;46:1049–1054.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Weiden, P., Glazer, W. Assessment and Treatment Selection for “Revolving Door” Inpatients with Schizophrenia. Psychiatr Q 68, 377–392 (1997). https://doi.org/10.1023/A:1025499131905
Issue Date:
DOI: https://doi.org/10.1023/A:1025499131905