Abstract
Background
Influenza vaccination is highly recommended for nursing home residents. However, it is known that vaccination coverage is low in the general population.
Aims
We aim to find out whether influenza vaccination coverage differs for nursing home residents between the year before and after admission and factors determining the chance to receive vaccination.
Methods
Claims data of the health insurance fund DAK of at least 65-year-olds were used. The proportion of residents with influenza vaccination were compared in the year before and after the admission stratified by several covariates. A multivariate logistic regression analysis was conducted to obtain predictors for influenza vaccination after admission.
Results
Vaccination coverage was overall higher in the year after admission (53.0%) than before (38.3%). Differences in vaccination coverage between most covariates evened out after admission. Differences remained for region of residence and number of comorbidities. The strongest predictor for receiving a vaccination after admission was the vaccination status before admission (OR 3.5; 95% CI 3.3–3.6) followed by region and number of comorbidities.
Discussion
Overall, vaccination coverage of nursing home residents remains lower than recommended. Doctor–patient contacts whether due to care for comorbidities or as a continuation of the relation over the time of admission to the nursing home seem to assure vaccination for residents.
Conclusion
Clear and unambiguous evidence of vaccine safety and efficacy for different subgroups within the same age group as well as organizational efforts to increase vaccination within nursing homes would be recommended.
Similar content being viewed by others
Background
Influenza is an infectious disease caused by a family of viruses with different subtypes. Influenza viruses are highly contagious and while leading only to mild symptoms in the majority of the infected, the virus can cause severe illness with mortality rates depending on the subtype and the immune status of the host. Influenza viruses can cause seasonal epidemics with varying severity. However, vaccination against influenza infections is available [1]. Due to antigen shifts of the virus new vaccines have to be developed and reassembled annually to meet the expected epidemic situation of the season. Therefore, vaccination has to be repeated before the start of each winter season [2].
Vaccination is considered to protect against the infection with influenza, complications of influenza as pneumonia, influenza-like illnesses caused by other viruses and overall mortality [3]. The World Health Organisation recommends vaccination coverage of 75% in vulnerable population groups to reach sufficient herd immunity. Vaccination is recommended for people with chronic conditions, pregnant women, health care staff as possible transmitters and people above the age of 65 years [4]. For EU member states this vaccination recommendation is set as a policy target by the European council [5].
In Germany, it is known that vaccination rates are far from the recommended 75% coverage. Annual vaccination rates vary regionally and are as low as 50% in some of the recommended population groups. Vaccination rate increase with higher age and number of chronic conditions [6]. Vaccination policy is similar throughout the whole country since the German reunification in 1990. However, probably due to different professional traditions in the former socialist eastern part of the country with its historically mandatory vaccination regime vaccination rates are still higher than in the western part [7]. Unlike in other health care systems in Germany vaccination is carried out exclusively by medical doctors or is within a practice under doctor´s supervision delegated to physician assistants. In the community, vaccination of adults is conducted mainly by general practitioners with some other specialties involved in a smaller proportion [8]. Nursing home residents are medically treated and vaccinated by their individual GP leading to different GPs visiting the same nursing home [9]. Even though the WHO and subsequent national guidelines by the Standing Committee on Vaccination (STIKO) in Germany give clear recommendations on whom to vaccinate [10], it is known that doctors decisions to vaccinate are influenced by other factors as the perceived safety of the vaccination [11].
Living in a nursing home is associated with a worse health status than in the non-institutionalized population of the same age group [12]. German vaccination recommendations include nursing home residents, therefore, as an additional vulnerable population group [10]. Evidence from the US shows in nursing home a reduction of influenza and pneumonia caused hospital admission after influenza vaccination [13]. On the contrary, others question the overall mortality benefit of the vaccination in the elderly [14, 15]. Despite the debate of the overall benefit of the vaccination in the elderly, few studies have examined whether the vaccination rate differs between nursing home residents and the non-institutionalized population of the same age group.
The aim of this study is to find out whether vaccination rates differ among people in the year before and after admission to a nursing home if the vaccination rate depends on the level of care, number of conditions, age and/or sex. Additionally, we want to find out if the known regional differences in vaccination rates are reproduced after the admission to the nursing home or if this finding is restricted to the non-institutionalized population.
Methods
Database and study population
Claims data of the DAK-Gesundheit, which is one of the largest German health insurance funds operating nationwide with about six million members, were used. This corresponds to about 7.5% of the German population. Data for the years 2011–2014 were used. We included all persons aged 65 years and older, which were newly admitted to a nursing home between January 1, 2012, and March 31, 2014. New admission was defined as a continuous insurance period of at least 365 days without nursing home placement. To assure a comparable time at risk, residents had to be insured at least one day in each of the four quarters after entry. This also includes persons that died during the last quarter.
Information on the date of nursing home placement was gathered from the German Long-Term Care Insurance (‘‘Gesetzliche Pflegeversicherung’’). These data also include levels of care dependency. During the years of observation, there were three care levels ranging from considerable need of care (level I) to most heavily care dependent (level III). Further information on the German long-term care system, also describing care levels in detail, can be found in Busse and Blümel [16]. German level of care regulations correlate with finer graded scales of activities of daily living, so a higher level of care can be viewed as a proxy for a greater loss of functional autonomy [17]. In principle, all residents of nursing homes are assigned to a care level on the day of admission.
We further used data on reimbursement of physicians working in ambulatory care, including both contacts in their own practice as well as visits in the corresponding nursing home. These data include diagnoses according to the German modification of the International Classification of Diseases (ICD-10 GM) as well as ambulatory procedural codes according to the uniform assessment standard (EBM). In Germany, physicians have to document diagnoses once per quarter and no specific date of diagnosis is available.
Outcome and independent variables
Our outcome of interest was influenza vaccination identified by codes of the uniform assessment standard (89004, 89111 and 89112) as done in previous studies [8].
As independent variables we assessed age (65–74, 75–84, 85–94 and 95+ years), sex (males and females), region of residence (the 16 German federal states), care levels (3 levels) and risk categories (7 diagnosis groups). Care levels were obtained on the day of nursing home placement and serve as a proxy for functional status. We used risk categories targeted for influenza vaccination as defined by Fleming and Elliot including respiratory disease, circulatory disease, diabetes and endocrine disease, disease of the liver, renal disorders, malignant neoplasms, immune compromise and others [18]. These diagnoses were assessed during the quarter of nursing home placement in ambulatory care.
Statistical analysis
We compared the proportion of residents with influenza vaccination during the year before and after nursing home admission. These analyses were stratified by age, sex, region of residence, care levels and risk categories using the above-mentioned categories. McNemar’s test for paired data was used to study differences between both periods.
To study the relation between influenza vaccination in the year after nursing home admission and further covariates, we fitted a multivariate logistic regression model. The following variables were included: age (65–74, 75–84, 85–94, 95+ years); sex (male, female); region of residence (East Germany, West Germany); level of care dependency (three categories); influenza vaccination in the years before nursing home admission (yes, no) and number of risk categories targeted for influenza vaccination (≤1, 2–3, 4+). Adjusted odds ratios (OR) with 95% confidence intervals (95% CI) were estimated.
The level of significance was 0.05. All statistical analyses were performed with SAS for Windows version 9.4 (SAS Institute Inc., Cary, North Carolina).
Results
The study population consisted of 42,068 participants of whom 77.3% were female and 22.7% male. 89.5% lived in West Germany and 10.5% in East Germany. Circulatory diseases were the most common comorbidity, followed by immune compromise, diabetes, renal disorders, respiratory diseases, neoplasms and liver disease. 48.8% of the study population was diagnosed with dementia. In terms of level of care most participants had the first level of care, followed by the second with fewest in the most severe third category (Table 1).
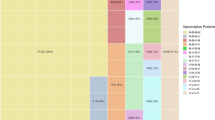
In all analyzed groups, vaccination rates were higher in the year after admission to the nursing home than in the year before (overall rate 53.0 vs. 38.3%). Before admission a clear age gradient emerged with the youngest group showing a vaccination rate of 28.5%, followed by the second youngest (38.0%) and third youngest (40.3%) while the oldest showed with 42.1% the highest rate. After admission the youngest group showed still the lowest rate (47.5%) while the age gradient in the other groups vanished with more equal rates between them (52.1–54.7%). Prior to admission, women showed a lower rate (37.4%) than men (41.2%) while after admission only a one per cent difference remained (52.7 vs. 53.8%). There were only slight differences in vaccination rates according to the dementia diagnosis both before and after admission (before 36.7 and 39.7% and after 54.7 and 51.3% residents with dementia and without). Vaccination rates were lower in West Germany both before and after admission to the nursing home (37.0 vs. 51.8%) than in the eastern part of the country (49.1 vs. 62.8%) (Table 2; Fig. 1). Prior to admission, participants in the highest level of care group showed a slightly higher vaccination rate than the other two (40.0 vs. 37.9–38.3%) while after admission no level of care gradient remained (50.4–53.2%). The vast majority was vaccinated prior and after admission to the nursing home by general practitioners (GPs) (97.2 and 98.6%). Significance tests showed for all results very strong evidence against the null hypothesis of no difference (p < 0.0001) (Table 2).
Participants with renal diseases showed before and after admission the highest vaccination rates (43.3 and 56.8%) compared to the other comorbidities. The range between different comorbidities with immune compromise showing the lowest vaccination rate (37.3%) evened out after admission (52.5–55.6%). With increasing number of comorbidities prior (32.5–44.5%) and after (48.4–57.1%) admission a clear gradient evolved (Table 3).
Results of the logistic regression analysis showed the highest chance to receive an influenza vaccination for nursing home residents in the year after admission if they were vaccinated in the year before admission, too (OR 3.45; 95%-CI 3.31–3.60). Residence in East Germany (OR 1.42; 95%-CI 1.32–1.52) and a high number of conditions (≥4) (OR 1.23; 95%-CI 1.15–1.32) were also associated with a higher chance to be vaccinated (Table 4).
Discussion
People living in nursing homes show higher vaccination rates than in the year before admission. This finding holds for all age groups, levels of care, degree of multi-morbidity and regions in Germany. In this sense vaccination recommendations are shown to have a positive effect on vaccination practice. However, neither in the overall rate nor in any of the analyzed subgroups vaccination rates reach the target of 75% in the nursing home resident population.
The age cut-off towards the young was 65 years in this study. Therefore, for all participants vaccination is recommended independent of any other additional risk factor for complicated influenza. Reasons for the low vaccination rate might be the non-mandatory vaccination policy in Germany, doctors and patients characteristics as well as features of the nursing homes. One important reason for the reluctance of doctors to vaccinate lies in the perceived risks and benefits of the vaccination, which has been shown in studies from France [19], the Netherlands [20] and Germany [11]. In our study, the clear age gradient before admission—the older the higher the vaccination rate—re-emerged as already had been shown in other studies in Germany [21]. Interestingly this age gradient—except for the youngest age group showing a lower rate—disappeared after admission. This might be due to the resident status per se associated with the additional German vaccination recommendation by the STIKO and possibly the perceived vulnerability of the patients by the GPs due to the fact that nursing home residents tend to have a worse general health status [22]. However, the level of care showed before admission only a weak association with vaccination rates and after admission no association. Again, it might be more due to the fact a level of care is assigned to a patient at all that indicates a vulnerability than the level of care itself. Before admission men showed a higher vaccination rate while after admission the rates almost evened out. Since men do have a lower life expectancy and a worse health status than women in the older age groups in Germany [23], higher vaccination rates might reflect the vulnerability as perceived by GPs while after institutionalization no difference in perception might remain.
Different types of comorbidities showed after admission to the nursing home an alignment of vaccination rates. The exception with the highest rates before and after admission being renal diseases. Renal insufficiency requires monitoring of the patient by the GP and early specialist consultation. Renal insufficiency proves to be a problem in nursing homes for medication and other types of medical care [12].
It is known that the frequency of GP–patient contacts correlates with the vaccination rate among the elderly [24] and the most important influence on the chance to receive vaccination among elderly patients being the treating physician [25]. However, there are various reasons not to vaccinate on the physicians’ side. GPs tend to recommend vaccination more often than specialists in the US [26] and in Germany [21]. In pandemic situations, German GPs increase their vaccination efforts and serve as coordinators of vaccination programmes [27] which indicates that to those who show vaccination hesitancy, pandemic situations are considered differently to seasonal influenza. In France vaccine hesitancy among GPs is relatively common with 16–43% of GPs never recommend a vaccination to their patients. Vaccine recommendations depended on the perceived risks and benefits of the vaccine, trust in information sources and doubts in vaccine utility [19]. However, in a pandemic situation French GPs participated actively in vaccination programmes [28] and GPs who do not vaccinate in a non-pandemic situation might reconsider if the severity of the problem is perceived differently. Home visits of nursing home residents are viewed by German GPs as a core activity albeit emotionally distressing [29]. The number of chronic conditions is positively associated with the frequency of home visits by a GP while despite an aging population the overall number of home visits decreases [30]. A possible reason not to vaccinate elderly people in Germany might be that the recommendation is not a high priority in comparison to other tasks by GPs [31]. Since in nursing homes vaccination is almost entirely conducted by GPs, the strong association with vaccination in the year prior to admission indicates that continuation of care by GPs to be highly beneficial to ensure vaccination of nursing home residents.
On the patient side, acceptance of vaccination does not rely on a single argument [32], but the recommendation of the GP serves as the strongest influence [33]. In Germany, barriers against the vaccination were the fear of side effects and the perceived necessity of the vaccination all of which were lower in higher socioeconomic groups [34]. Additionally, patients choosing not to be vaccinated tend to have lesser knowledge about the causes of influenza illnesses and physicians' recommendations increase vaccination coverage [35]. Social inequalities in vaccination could be shown with international data [36] and in Germany as well [7]. It is unclear and cannot be answered with data from this study whether there are socioeconomic inequalities in the vaccination rate of the nursing home population and how actively residents of nursing homes participate in the decision to be vaccinated. Belgian data suggest influenza vaccination unlike other health care domains not to be associated with socioeconomic disparities [37].
Level of care was not associated with differentials in vaccination rates. A higher level of care corresponds with a lower degree of control and functional autonomy by the patient. Similarly, patients with a dementia diagnosis did not show relevant lower vaccination rates before and higher rates after admission to the nursing home. In US nursing homes residents with dementia had lesser use of medical services and a lower frequency of home visits than residents without [38]. In Germany, nursing home residents with dementia face a higher risk of not be adequately cared for by medical specialists [39]. Despite some evidence for a less good medical care of nursing home residents in general our data suggests the decision on influenza vaccination depend to a lesser degree on the patients’ cognitive ability or autonomy to decide. These findings are in line with French data showing only a slightly lower vaccination rate among elderly patients with a dementia diagnosis than without [40]. Results from the UK have shown differences in vaccination rates depending on dementia to rather be a problem in the community setting than in nursing homes [41]. According to our data, this does not seem to be an additional problem to the generally low rates in the community in Germany in the case of influenza vaccination.
The ongoing debate about effectiveness of influenza vaccine in the elderly [42] possibly spurred by a Cochrane meta-analysis that found no convincing evidence of the efficacy and effectiveness of the vaccination in the population above 65 years of age with the bulk of evidence being of low quality [43] might add to the uncertainty to vaccinate nursing home residents. While newer tetravalent vaccines are claimed to be more effective in the elderly [44] Japanese data show GPs to be still influenced by safety concerns [45]. Therefore, to increase vaccination rates, clear and non-ambiguous evidence about vaccine efficiency and safety would be recommended.
In East Germany, higher vaccination rates in the general public than in West Germany [46] could be reproduced in our study and were continued on a higher level within nursing homes. This regional divide of vaccination practice is thought to be the result of mandatory vaccination regimes of the former German Democratic Republic. Further research has to show whether younger generations of GPs are still influenced by these traditions and how higher rates in nursing homes are to be explained.
The results of our analysis support the assumption that for many GPs the decision to conduct an influenza vaccination is not taken solely on the basis of the biological age of a patient. The German College of GPs and Family Physicians calls for an individualized approach in the non-institutionalized elderly population with a consideration of the physical fitness, personal preferences and comorbidities of the patient, while giving a clear recommendation to vaccinate the nursing home population [47]. In Germany, campaigns of the Federal Centre for Health Education to vaccinate nursing home staff are receiving little attention with a low vaccination uptake [48]. From the organizational point of view only a minority of German nursing homes are conducting organized efforts to vaccinate resulting in a need for further health education of the staff and residents [49]. These findings reinforce the need for improved organized vaccination efforts in nursing homes for both residents and staff. However, data from US suggests awareness-raising campaigns in the public are not sufficient to increase vaccination rates in nursing homes [50]. Specially organized programmes in the Netherlands involving nursing home management and staff as well as physicians and giving clear recommendations on how to assure vaccination for all residents in an institution [51] point at the importance of tailored programmes to ensure vaccination of this vulnerable population group.
Limitations
Data for this analysis stem from only one albeit large health insurance fund. The data are, therefore, not representative for the general population. Furthermore, the socioeconomic composition of the insurant population of the health insurance fund may differ from other funds. Possible differences of the socioeconomic composition might yield some different result about the magnitude of the findings but it is unlikely to come to fundamentally different results with data from another health insurance fund. Health insurance funds can encourage their insured to receive vaccination but the ultimate decision lies in the doctor–patient interaction. Since the data are derived from doctors' settlement data, reliability can be considered high since no recall bias occurred.
The study population consisted of a larger percentage of females than males. This might be due to higher life expectancy of females leading to larger representation in older age groups and the formerly female-dominated white collar employee orientation of the sickness fund. However, vaccination rates after admission differed only slightly between the genders.
Our data offered neither characteristics of the nursing homes nor of the doctors who conducted the vaccination. Further conclusions about the reasons for comparing to the national target low vaccination rate among nursing home residents remain, therefore, speculative.
The 1-year difference might not capture longer time trends. It might be equally possible that resident vaccination rates increase with length of stay or being a one-time-only increase with the tendency of decline with time.
Conclusion
In Germany, vaccination rates are higher after admission to a nursing home than for the same person group in the year before. However, in no subgroup the recommended vaccination rate of 75% is reached. Reasons for these findings might be uncertainty about efficacy and safety of the vaccination along with a general low priority on the doctor side, perceived vulnerability and little knowledge of the usefulness of the vaccination on the patient side and the absence of organized vaccination programmes in nursing homes. Higher vaccination rates in East Germany and increasing rates with the number of comorbidities indicate that traditions in professional culture and frequency of doctor patient contacts are beneficial for vaccination rates. These reasons might offer a lever to increase the vaccination rate in this vulnerable population group. Tailored recommendations according to the functional status rather than the biological age of the patient and organized campaigns involving both nursing home staff and GPs might increase vaccination efforts of GPs.
References
Ghebrehewet S, MacPherson P, Ho A (2016) Influenza. BMJ 355:i6258. doi:10.1136/bmj.i6258
WHO (2017) Global influenza surveillance and response system (GISRS): World Health Organization. http://www.who.int/influenza/gisrs_laboratory/en/. Accessed 22 Jan 2017
Beyer Walter EP, McElhaney J, Smith DJ et al (2013) Cochrane re-arranged: support for policies to vaccinate elderly people against influenza. Vaccine 31:6030–6033. doi:10.1016/j.vaccine.2013.09.063
WHO (2003) Prevention and control of influenza pandemics and annual epidemics: resolution of the World Health assembly. Resolution WHA56.19, tenth plenary meeting, 28 May 2003: World Health Organization. http://apps.who.int/gb/archive/pdf_files/WHA56/ea56r19.pdf. Accessed 8 Jan 2017
European Council (2009) Council recommendation on seasonal influenza vaccination. http://ec.europa.eu/health/ph_threats/com/Influenza/docs/seasonflu_rec2009_en.pdf. Accessed 8 Jan 2017
Wutzler P (2006) Influenza-Schutzimpfung–Wo steht Deutschland? Dtsch Med Wochenschr 131:453–457. doi:10.1055/s-2006-932543
Poethko-Müller C, Schmitz R (2013) Impfstatus von Erwachsenen in Deutschland. Bundesgesundheitsbl 56:845–857. doi:10.1007/s00103-013-1693-6
Luque Ramos A, Hoffmann F, Callhoff J et al (2016) Influenza and pneumococcal vaccination in patients with rheumatoid arthritis in comparison with age- and sex-matched controls: results of a claims data analysis. Rheumatol Int 36:1255–1263. doi:10.1007/s00296-016-3516-1
Hallauer J, Bienstein C, Lehr U et al (2005) SÄVIP—Studie zur ärztlichen Versorgung in Pflegeheimen. Vincentz Netw Market Ser
STIKO (2015) Recommendations of the standing committee on vaccination (STIKO): effective: August 2015. Epid Bull. doi:10.17886/EpiBull-2015-001.3
Böhmer MM, Walter D, Ehrhardt J et al (2014) Saisonale und pandemische Influenzaimpfung: impfquoten und Einstellung niedergelassener Ärzte in Deutschland. Gesundheitswesen 76:44–47. doi:10.1055/s-0033-1343431
Hoffmann F, Boeschen D, Dörks M et al (2016) Renal insufficiency and medication in nursing home residents. Dtsch Arztebl Int 113:92–98. doi:10.3238/arztebl.2016.0092
Pop-Vicas A, Rahman M, Gozalo PL et al (2015) Estimating the effect of influenza vaccination on nursing home residents’ morbidity and mortality. J Am Geriatr Soc 63:1798–1804. doi:10.1111/jgs.13617
Rizzo C, Viboud C, Montomoli E et al (2006) Influenza-related mortality in the Italian elderly: no decline associated with increasing vaccination coverage. Vaccine 24:6468–6475. doi:10.1016/j.vaccine.2006.06.052
Simonsen L, Taylor RJ, Viboud C et al (2007) Mortality benefits of influenza vaccination in elderly people: an ongoing controversy. Lancet Infect Dis 7:658–666. doi:10.1016/S1473-3099(07)70236-0
Busse R, Blümel M (2014) Germany: health system review. Health Syst Transit 16:1–296
Lohrmann C, Dijkstra A, Dassen T (2003) Care dependency: testing the German version of the care dependency scale in nursing homes and on geriatric wards. Scand J Caring Sci 17:51–56. doi:10.1046/j.1471-6712.2003.00117.x
Fleming DM, Elliot AJ (2006) Estimating the risk population in relation to influenza vaccination policy. Vaccine 24:4378–4385. doi:10.1016/j.vaccine.2006.02.053
Verger P, Fressard L, Collange F et al (2015) Vaccine hesitancy among general practitioners and its determinants during controversies: a national cross-sectional survey in France. EBioMed 2:891–897. doi:10.1016/j.ebiom.2015.06.018
Eilers R, Krabbe Paul FM, de Melker Hester E (2015) Attitudes of Dutch general practitioners towards vaccinating the elderly: less is more? BMC Fam Pract 16:158. doi:10.1186/s12875-015-0377-8
Hauswaldt J, Kersting M, Hummers-Pradier E (2010) Influenza-Impfungen durch Niedersächsische Hausärzte—eine Sekundäranalyse vertragsärztlicher Versorgungsdaten aus 1995/1996, 2002/2003 und 2005/2006. Gesundheitswesen 72:332–339. doi:10.1055/s-0030-1249690
Hoffmann F, Kaduszkiewicz H, Glaeske G et al (2014) Prevalence of dementia in nursing home and community-dwelling older adults in Germany. Aging Clin Exp Res 26:555–559. doi:10.1007/s40520-014-0210-6
RKI (ed) (2015) Gesundheit in Deutschland: Gesundheitsberichterstattung des Bundes, 1. Aufl. Berlin. http://www.rki.de/EN/Content/Health_Monitoring/Health_Reporting/HealthInGermany/health_germany_node.html
Domínguez À, Soldevila N, Toledo D et al (2016) Factors associated with influenza vaccination of hospitalized elderly patients in Spain. PLoS One 11:e0147931. doi:10.1371/journal.pone.0147931
Martínez-Baz I, Aguilar I, Morán J et al (2012) Factors associated with continued adherence to influenza vaccination in the elderly. Prev Med 55:246–250. doi:10.1016/j.ypmed.2012.06.020
Nichol KL, Zimmerman R (2001) Generalist and subspecialist physicians’ knowledge, attitudes, and practices regarding influenza and pneumococcal vaccinations for elderly and other high-risk patients: a nationwide survey. Arch Intern Med 161:2702–2708. doi:10.1001/archinte.161.22.2702
Eisele M, Hansen H, Wagner H et al (2014) Epidemien und Pandemien in der hausärztlichen Praxis. Bundesgesundheitsbl 57:687–693. doi:10.1007/s00103-014-1970-z
Schwarzinger M, Verger P, Guerville M et al (2010) Positive attitudes of French general practitioners towards A/H1N1 influenza-pandemic vaccination: a missed opportunity to increase vaccination uptakes in the general public? Vaccine 28:2743–2748. doi:10.1016/j.vaccine.2010.01.027
Theile G, Kruschinski C, Buck M et al (2011) Home visits - central to primary care, tradition or an obligation? A qualitative study. BMC Fam Pract 12:24. doi:10.1186/1471-2296-12-24
Snijder EA, Kersting M, Theile G et al (2007) Hausbesuche: Versorgungsforschung mit hausärztlichen Routinedaten von 158.000 Patienten. Gesundheitswesen 69:679–685. doi:10.1055/s-2007-993181
Klett-Tammen CJ, Krause G, von Lengerke T et al (2016) Advising vaccinations for the elderly: a cross-sectional survey on differences between general practitioners and physician assistants in Germany. BMC Fam Pract 17:98. doi:10.1186/s12875-016-0502-3
Eilers R, Krabbe Paul FM, de Melker Hester E (2015) Motives of Dutch persons aged 50 years and older to accept vaccination: a qualitative study. BMC Pub Health 15:493. doi:10.1186/s12889-015-1825-z
Gulich M, Eberhardt S, Blankenhorn S et al (2006) Motivation zur Grippeimpfung bei hausärztlichen Patienten in der Saison 2005/2006. Z Allg Med 82:334–337. doi:10.1055/s-2006-942084
Böhmer MM, Walter D, Falkenhorst G et al (2012) Barriers to pandemic influenza vaccination and uptake of seasonal influenza vaccine in the post-pandemic season in Germany. BMC Pub Health 12:938. doi:10.1186/1471-2458-12-938
Bödeker B, Remschmidt C, Schmich P et al (2015) Why are older adults and individuals with underlying chronic diseases in Germany not vaccinated against flu? A population-based study. BMC Pub Health 15:618. doi:10.1186/s12889-015-1970-4
Nagata JM, Hernández-Ramos I, Kurup AS et al (2013) Social determinants of health and seasonal influenza vaccination in adults ≥65 years: a systematic review of qualitative and quantitative data. BMC Pub Health 13:388. doi:10.1186/1471-2458-13-388
Hoeck S, van der Heyden J, Geerts J et al (2013) Preventive care use among the Belgian elderly population: does socio-economic status matter? Int J Environ Res Pub Health 11:355–372. doi:10.3390/ijerph110100355
Burton LC, German PS, Gruber-Baldini AL et al (2001) Medical care for nursing home residents: differences by dementia status. Epidemiology of dementia in nursing homes research group. J Am Geriatr Soc 49:142–147
Balzer K, Butz S, Bentzel J et al (2013) Medical specialist attendance in nursing homes. GMS Health Technol Asses. doi:10.3205/hta000108
Gallini A, Coley N, Andrieu S et al (2017) Effect of dementia on receipt of influenza vaccine: a cohort study in French older adults using administrative data: 2007–2012. Fundam Clin Pharmacol 31:471–480. doi:10.1111/fcp.12281
Shah SM, Carey IM, Harris T et al (2011) The impact of dementia on influenza vaccination uptake in community and care home residents. Age Ageing. doi:10.1093/ageing/afr135
Trucchi C, Paganino C, Orsi A et al (2015) Influenza vaccination in the elderly: why are the overall benefits still hotly debated? J Prev Med Hyg 56:E37–43
Jefferson T, Di Pietrantonj C, Al-Ansary LA et al (2010) Vaccines for preventing influenza in the elderly. Cochrane Database Syst Rev. doi:10.1002/14651858.CD004876.pub3
Wutzler P, Hardt R, Knuf M et al (2013) Targeted vaccine selection in influenza vaccination. Dtsch Arztebl Int 110:793–798. doi:10.3238/arztebl.2013.0793
Inoue Y, Matsui K (2010) Physicians’ recommendations to their patients concerning a novel pandemic vaccine: a cross-sectional survey of the 2009 influenza A/H1N1 pandemic in Japan. Environ Health Prev Med 16:320–326. doi:10.1007/s12199-010-0202-x
Reuss AM, Walter D, Feig M et al (2010) Influenza vaccination coverage in the 2004/05, 2005/06, and 2006/07 seasons. Dtsch Arztebl Int 107:845–850. doi:10.3238/arztebl.2010.0845
Ledig T (2009) Impfen um jeden Preis? Impfmüdigkeit in Deutschland? Z Allg Med 85:94–96
Bödeker B, Wichmann O, Mertens B et al (2014) Implementation of the influenza vaccination recommendation in nursing homes in Germany. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 57:1315–1321. doi:10.1007/s00103-014-2044-y
Bödeker B, Remschmidt C, Müters S et al (2015) Influenza, tetanus, and pertussis vaccination coverage among adults in Germany. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 58:174–181. doi:10.1007/s00103-014-2097-y
Cai S, Temkin-Greener H (2010) Influenza vaccination and its impact on hospitalization events in nursing homes. J Am Med Dir Assoc 12:493–498. doi:10.1016/j.jamda.2010.03.005
Cools HJM, van Essen GA (2005) Practice guideline ‘Influenza prevention in nursing homes and care homes’, issued by the Dutch society of nursing home specialists; division of tasks between nursing home specialist, general practitioner and company doctor. Ned Tijdschr Geneeskd 149:119–24 (discussion 116–8)
Acknowledgements
This study was conducted receiving no external funding. We thank the DAK-Gesundheit for providing the data.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Statement of human and animal rights
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
For this type of study formal consent is not required.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Spreckelsen, O., Luque Ramos, A., Freitag, M. et al. Influenza vaccination rates before and after admission to nursing homes in Germany. Aging Clin Exp Res 30, 609–616 (2018). https://doi.org/10.1007/s40520-017-0825-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-017-0825-5